Pulmonary complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pulmonary complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pulmonary complications US Medical PG Question 1: Five days after being admitted to the hospital for an open cholecystectomy, a 56-year-old woman develops difficulty breathing. She also has fevers, chills, and malaise. She has a cough productive of minimal amounts of yellowish-white sputum that started two days prior. She has type 2 diabetes mellitus, hypertension, and a history of gallstones. Her current medications include metformin, lisinopril, and atorvastatin. Her temperature is 39.5°C (103.1°F), pulse is 104/minute, blood pressure is 94/68 mm Hg, and respirations are 30/minute. Pulse oximetry on 2 L of oxygen via nasal cannula shows an oxygen saturation of 92%. Examination reveals decreased breath sounds over the right lung base. Abdominal examination shows a well-healing scar without erythema or discharge in the right upper quadrant. The skin is warm and well-perfused. Her hemoglobin concentration is 10.5 g/dL, leukocyte count is 16,000/mm3, platelet count is 345,000/mm3, and creatinine is 1.5 mg/dL. She is admitted to the ICU and started on IV fluids. Blood and urine for cultures are obtained. X-ray of the chest reveals a right sided pleural effusion. Which of the following is the next best step in management?
- A. Intravenous ceftriaxone and azithromycin
- B. Intravenous dobutamine
- C. CT of the chest with contrast
- D. Intravenous vancomycin and cefepime (Correct Answer)
- E. External cooling and intravenous acetaminophen
Pulmonary complications Explanation: ***Intravenous vancomycin and cefepime***
- The patient presents with classic signs of **sepsis** and **septic shock** (fever, tachypnea, tachycardia, hypotension, elevated WBC, acute organ dysfunction with increased creatinine) following surgery, pointing to a **healthcare-associated infection (HCAI)**, likely pneumonia given the respiratory symptoms and CXR.
- **Vancomycin** provides coverage against **methicillin-resistant Staphylococcus aureus (MRSA)**, a common pathogen in HCAI, especially in patients with recent hospitalization. **Cefepime** is a broad-spectrum anti-pseudomonal beta-lactam that covers other gram-negative and gram-positive pathogens.
*Intravenous ceftriaxone and azithromycin*
- This regimen is more appropriate for **community-acquired pneumonia (CAP)**, but not for severe healthcare-associated infections due to insufficient coverage for resistant organisms, such as MRSA and *Pseudomonas*.
- The patient's recent hospitalization and surgery increase the risk for **multidrug-resistant (MDR)** organisms, which necessitate broader coverage than ceftriaxone and azithromycin.
*Intravenous dobutamine*
- **Dobutamine** is an inotropic agent used to improve cardiac contractility in **cardiogenic shock** or when cardiac output is low despite adequate fluid resuscitation.
- While the patient is hypotensive, she is in **septic shock**, and the initial management involves fluid resuscitation and broad-spectrum antibiotics, not primarily inotropes. Inotropes might be considered if hypotension persists after fluid resuscitation.
*CT of the chest with contrast*
- A chest CT may be useful for further characterization of the pleural effusion or to rule out other pathologies like pulmonary embolism if suspicion is high.
- However, given the signs of **septic shock**, initiating **empiric broad-spectrum antibiotics** is the most urgent step to stabilize the patient and treat the suspected infection. Diagnostic imaging can be pursued once the patient is stable and initial management is underway.
*External cooling and intravenous acetaminophen*
- **External cooling** and **acetaminophen** are antipyretic measures to reduce fever, which can improve patient comfort.
- While fever control is part of supportive care, it does not address the underlying **septic shock** and **infection**, which are life-threatening and require immediate aggressive antibiotic therapy and fluid resuscitation.
Pulmonary complications US Medical PG Question 2: A previously healthy 35-year-old woman is brought into the emergency department after being found unresponsive by her husband. Her husband finds an empty bottle of diazepam tablets in her pocket. She is stuporous. At the hospital, her blood pressure is 90/40 mm Hg, the pulse is 58/min, and the respirations are 6/min. The examination of the pupils shows normal size and reactivity to light. Deep tendon reflexes are 1+ bilaterally. Babinski sign is absent. All 4 extremities are hypotonic. The patient is intubated and taken to the critical care unit for mechanical ventilation and treatment. Regarding the prevention of pneumonia in this patient, which of the following strategies is most likely to achieve this goal?
- A. Nasogastric tube insertion
- B. Daily evaluation for ventilator weaning
- C. Subglottic drainage of secretions (Correct Answer)
- D. Oropharynx and gut antibacterial decontamination
- E. Prone positioning during mechanical ventilation
Pulmonary complications Explanation: ***Subglottic drainage of secretions***
- This is a highly effective strategy to prevent **ventilator-associated pneumonia (VAP)** by continuously removing secretions that pool above the endotracheal tube cuff before they can be aspirated.
- Endotracheal tubes with a **subglottic secretion drainage port** reduce VAP incidence by preventing microaspiration of contaminated oropharyngeal secretions into the lower respiratory tract.
- This is a **specific mechanical intervention** that directly addresses one of the key pathogenic mechanisms of VAP.
*Nasogastric tube insertion*
- While an NG tube may be needed for feeding or gastric decompression, it does not directly prevent VAP and may **increase aspiration risk** by compromising the lower esophageal sphincter.
- NG tubes can promote gastroesophageal reflux and provide a conduit for bacterial migration.
*Daily evaluation for ventilator weaning*
- This is also a **critical component of VAP prevention** as part of the ventilator bundle, since reducing duration of mechanical ventilation is the most effective overall strategy to prevent VAP.
- However, in this question asking for a strategy to prevent pneumonia in an intubated patient, subglottic drainage is the more specific technical intervention, whereas daily weaning assessment is a broader protocol that reduces exposure time.
- Both strategies are important; subglottic drainage addresses the "how" of prevention during intubation, while weaning protocols address the "duration" of risk exposure.
*Oropharynx and gut antibacterial decontamination*
- Selective digestive decontamination (SDD) aims to reduce bacterial colonization, but evidence for routine use is mixed and raises concerns about **antimicrobial resistance**.
- Not universally recommended as a primary VAP prevention strategy in most guidelines.
*Prone positioning during mechanical ventilation*
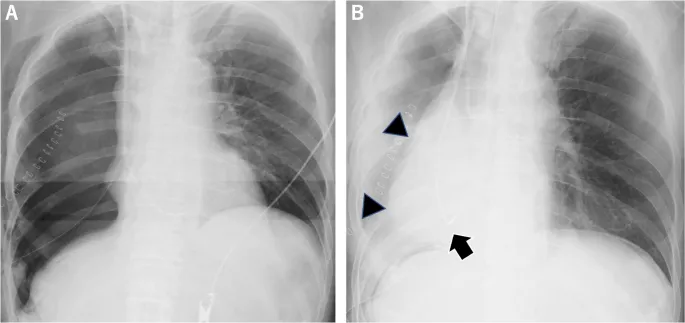
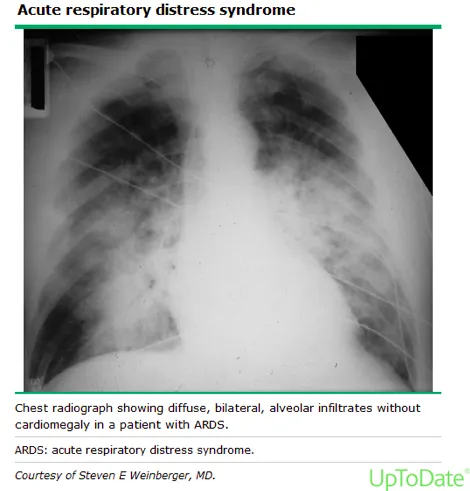
- **Prone positioning** is primarily indicated for improving oxygenation in **Acute Respiratory Distress Syndrome (ARDS)**, not for VAP prevention.
- While it may improve secretion drainage, it is not a standard VAP prevention measure and carries its own risks and logistical challenges.
Pulmonary complications US Medical PG Question 3: Three days after undergoing coronary artery bypass surgery, a 72-year-old man has severe right upper quadrant pain, fever, nausea, and vomiting. He has type 2 diabetes mellitus, benign prostatic hyperplasia, peripheral vascular disease, and chronic mesenteric ischemia. He had smoked one pack of cigarettes daily for 30 years but quit 10 years ago. He drinks 8 cans of beer a week. His preoperative medications include metformin, aspirin, simvastatin, and finasteride. His temperature is 38.9°C (102°F), pulse is 102/min, respirations are 18/min, and blood pressure is 110/60 mmHg. Auscultation of the lungs shows bilateral inspiratory crackles. Cardiac examination shows no murmurs, rubs or gallops. Abdominal examination shows soft abdomen with tenderness and sudden inspiratory arrest upon palpation in the right upper quadrant. There is no rebound tenderness or guarding. Laboratory studies show the following:
Hemoglobin 13.1 g/dL
Hematocrit 42%
Leukocyte count 15,700/mm3
Segmented neutrophils 65%
Bands 10%
Lymphocytes 20%
Monocytes 3%
Eosinophils 1%
Basophils 0.5%
AST 40 U/L
ALT 100 U/L
Alkaline phosphatase 85 U/L
Total bilirubin 1.5 mg/dL
Direct 0.9 mg/dL
Amylase 90 U/L
Abdominal ultrasonography shows a distended gallbladder, thickened gallbladder wall with pericholecystic fluid, and no stones. Which of the following is the most appropriate next step in management?
- A. Intravenous heparin therapy followed by embolectomy
- B. Careful observation with serial abdominal examinations
- C. Endoscopic retrograde cholangiopancreatography with papillotomy
- D. Intravenous piperacillin-tazobactam therapy and percutaneous cholecystostomy (Correct Answer)
- E. Immediate cholecystectomy
Pulmonary complications Explanation: ***Intravenous piperacillin-tazobactam therapy and percutaneous cholecystostomy***
- The patient presents with **acalculous cholecystitis**, characterized by severe RUQ pain, fever, leukocytosis, elevated transaminases, and ultrasonographic findings of a distended gallbladder with a thickened wall and pericholecystic fluid, but no stones.
- Given his comorbid conditions (diabetes, PVD, recent CABG) and the severity of his illness, empirical **broad-spectrum antibiotics** (like piperacillin-tazobactam) along with image-guided **percutaneous cholecystostomy** for gallbladder decompression are the most appropriate management, avoiding the high risks of immediate surgery.
*Intravenous heparin therapy followed by embolectomy*
- This approach is indicated for **acute mesenteric ischemia with embolism**, which can present with severe abdominal pain and signs of hypoperfusion.
- While the patient has chronic mesenteric ischemia, his current symptoms and imaging findings are more consistent with cholecystitis, and there is no clear evidence of acute embolic event requiring embolectomy.
*Careful observation with serial abdominal examinations*
- This patient exhibits signs of a severe inflammatory process (fever, leukocytosis, RUQ tenderness, elevated LFTs, and sonographic findings of severe inflammation) and systemic illness, making **conservative observation insufficient** and potentially dangerous.
- **Acalculous cholecystitis** is a serious condition with a high risk of complications like perforation and sepsis, especially in critically ill patients, and requires prompt intervention.
*Endoscopic retrograde cholangiopancreatography with papillotomy*
- **ERCP with papillotomy** is indicated for conditions like **choledocholithiasis** (common bile duct stones) or **cholangitis**, which cause biliary obstruction.
- The ultrasound shows **no stones** and features specific to cholecystitis rather than common bile duct obstruction, making ERCP inappropriate as an initial step.
*Immediate cholecystectomy*
- While cholecystectomy is the definitive treatment for cholecystitis, immediate open or laparoscopic cholecystectomy in a critically ill patient with **acalculous cholecystitis** after recent CABG carries a **very high morbidity and mortality risk**.
- **Percutaneous cholecystostomy** offers a safer, less invasive alternative for source control and stabilizes the patient before potential delayed definitive surgery if needed, once the patient's condition improves.
Pulmonary complications US Medical PG Question 4: A 52-year-old man presents to the emergency department with sudden-onset dyspnea, tachypnea, and chest pain. He works as a long-haul truck driver, and he informs you that he recently returned to the west coast from a trip to Tennessee. His medical history is significant for gout, hypertension, hypercholesterolemia, diabetes mellitus type 2, and mild intellectual disability. He currently smokes 2 packs of cigarettes/day, drinks a 6-pack of beer/day, and he endorses a past history of injection drug use but currently denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 23/min. His physical examination shows minimal bibasilar rales, but otherwise clear lungs on auscultation, grade 2/6 holosystolic murmur, and a benign abdominal physical examination. A computed tomography angiography (CTA) demonstrates a segmental pulmonary embolism (PE). Which of the following is the most appropriate treatment plan for this patient?
- A. Consult interventional radiologist (IR) for IVC filter placement
- B. Initiate heparin
- C. Tissue plasminogen activator (tPA)
- D. Initiate heparin with a bridge to warfarin (Correct Answer)
- E. Initiate warfarin anticoagulation
Pulmonary complications Explanation: ***Initiate heparin with a bridge to warfarin***
- This patient presents with a **segmental pulmonary embolism (PE)** and is hemodynamically stable (BP 126/74 mmHg, HR 87/min), making initial anticoagulation with **heparin** followed by a bridge to **warfarin** the most appropriate treatment.
- Heparin provides rapid anticoagulation, while warfarin is initiated concurrently and takes several days to reach therapeutic levels, requiring overlap until the **International Normalized Ratio (INR)** is within the therapeutic range (2.0-3.0).
*Consult interventional radiologist (IR) for IVC filter placement*
- **Inferior vena cava (IVC) filters** are typically reserved for patients with a **contraindication to anticoagulation** or those who experience **recurrent PE despite adequate anticoagulation**.
- This patient has no stated contraindications to anticoagulation and has not failed initial therapy, so an IVC filter is not indicated at this time.
*Initiate heparin*
- While initiating **heparin** is the correct first step, it is incomplete as a long-term treatment strategy for PE.
- Patients with PE require **long-term anticoagulation** (typically 3-6 months or longer), for which warfarin or novel oral anticoagulants (NOACs) are used, following an initial period of rapid-acting anticoagulation.
*Tissue plasminogen activator (tPA)*
- **Thrombolytic therapy with tPA** is indicated for patients with **massive PE** who are **hemodynamically unstable** (e.g., hypotension, shock).
- This patient is hemodynamically stable, and his PE is segmental, so thrombolysis carries a higher risk of bleeding complications than benefits in this case.
*Initiate warfarin anticoagulation*
- **Warfarin** has a slow onset of action (3-5 days to achieve therapeutic INR) and therefore should not be used as monotherapy for initial management of acute PE.
- Initial management requires a **rapid-acting anticoagulant** like heparin or low molecular weight heparin (LMWH) to prevent further clot propagation and embolization.
Pulmonary complications US Medical PG Question 5: A 43-year-old woman presents to her primary care physician with complaints of mild shortness of breath and right-sided chest pain for three days. She reports that lately she has had a nagging nonproductive cough and low-grade fevers. On examination, her vital signs are: temperature 99.1 deg F (37.3 deg C), blood pressure is 115/70 mmHg, pulse is 91/min, respirations are 17/min, and oxygen saturation 97% on room air. She is well-appearing, with normal work of breathing, and no leg swelling. She is otherwise healthy, with no prior medical or surgical history, currently taking no medications. The attending has a low suspicion for the most concerning diagnosis and would like to exclude it with a very sensitive though non-specific test. Which of the following should this physician order?
- A. Obtain chest radiograph
- B. Obtain spiral CT chest with IV contrast
- C. Order a lower extremity ultrasound
- D. Order a D-dimer (Correct Answer)
- E. Obtain ventilation-perfusion scan
Pulmonary complications Explanation: ***Order a D-dimer***
- The physician has a **low suspicion based on clinical assessment** and wants to **exclude** a concerning diagnosis (likely **pulmonary embolism** or PE) using a **sensitive test**. A negative D-dimer test can effectively rule out PE in patients with a low pre-test probability.
- The D-dimer is a product of **fibrin degradation** and its elevation indicates recent or ongoing **thrombus formation** and lysis. It is highly sensitive for PE but has low specificity.
*Obtain chest radiograph*
- A chest radiograph is often **normal in pulmonary embolism** or may show non-specific findings, making it unsuitable for ruling out PE.
- While useful for diagnosing other conditions like pneumonia or pleural effusions, it is **not sensitive enough to exclude PE**.
*Obtain spiral CT chest with IV contrast*
- A **spiral CT chest with IV contrast (CT pulmonary angiography)** is the gold standard for diagnosing PE, but it is **not a sensitive rule-out test** for low-probability cases.
- It involves **radiation exposure** and **contrast administration**, which are generally avoided if a less invasive, equally effective rule-out test is available for low-risk patients.
*Order a lower extremity ultrasound*
- Lower extremity ultrasound is used to diagnose **deep vein thrombosis (DVT)**, which is a common source of PE.
- While DVT can lead to PE, a negative lower extremity ultrasound **does not rule out PE** itself, as the clot may have already embolized or originated from elsewhere.
*Obtain ventilation-perfusion scan*
- A **ventilation-perfusion (V/Q) scan** is an alternative to CT angiography for diagnosing PE, particularly in patients with contraindications to contrast.
- However, it is **less definitive than CTPA** and is typically used when suspicion for PE is moderate or higher, rather than as a primary rule-out test for low-probability patients.
Pulmonary complications US Medical PG Question 6: A 68-year-old woman presents to the hospital for an elective right hemicolectomy. She is independently mobile and does her own shopping. She has had type 2 diabetes mellitus for 20 years, essential hypertension for 15 years, and angina on exertion for 6 years. She has a 30-pack-year history of smoking. The operation was uncomplicated. On post-op day 5, she becomes confused. She has a temperature of 38.5°C (101.3°F), respiratory rate of 28/min, and oxygen saturation of 92% on 2 L of oxygen. She is tachycardic at 118/min and her blood pressure is 110/65 mm Hg. On chest auscultation, she has coarse crackles in the right lung base. Her surgical wound appears to be healing well, and her abdomen is soft and nontender. Which of the following is the most likely diagnosis?
- A. Malignant hyperthermia
- B. Drug-induced fever
- C. Multiple organ dysfunction syndrome
- D. Sepsis (Correct Answer)
- E. Non-infectious systemic inflammatory response syndrome (SIRS)
Pulmonary complications Explanation: ***Sepsis***
- The patient exhibits several signs of **systemic inflammatory response syndrome (SIRS)** (fever, tachycardia, tachypnea) coupled with evidence of infection (coarse crackles in the lung base suggests **pneumonia**).
- The combination of **SIRS criteria** and a likely infection source in a postoperative patient strongly points to sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection.
*Malignant hyperthermia*
- This is a rare, life-threatening condition typically triggered by **volatile anesthetic agents** or **succinylcholine** during surgery.
- It usually presents **intraoperatively or immediately postoperatively** with rapid onset of hyperthermia, muscle rigidity, and metabolic acidosis, which is not consistent with a presentation on post-op day 5.
*Drug-induced fever*
- While drug-induced fever is possible, particularly in polymedicated patients, it would be a **diagnosis of exclusion** when other more likely causes of fever, such as infection, are present.
- There are no specific clinical features in this case that strongly suggest a drug as the singular cause of fever and the systemic inflammatory response.
*Multiple organ dysfunction syndrome*
- **MODS** is the progressive failure of two or more organ systems and is often a **complication of severe sepsis or septic shock**, rather than an initial diagnosis.
- While the patient is unwell, her current presentation describes a potential precursor (sepsis) rather than established multi-organ dysfunction.
*Non-infectious systemic inflammatory response syndrome (SIRS)*
- SIRS caused by non-infectious etiologies (e.g., pancreatitis, trauma, burns) can occur, but the presence of **localized lung crackles** and a **postoperative fever** makes an infectious etiology much more likely.
- Postoperative SIRS can occur due to surgical stress, but the signs of infection (especially respiratory) shift the diagnosis towards sepsis.
Pulmonary complications US Medical PG Question 7: Five minutes after arriving in the postoperative care unit following total knee replacement under general anesthesia, a 55-year-old woman is acutely short of breath. The procedure was uncomplicated. Postoperatively, prophylactic treatment with cefazolin was begun and the patient received morphine and ketorolac for pain management. She has generalized anxiety disorder. Her only other medication is escitalopram. She has smoked one pack of cigarettes daily for 25 years. Her temperature is 37°C (98.6°F), pulse is 108/min, respirations are 26/min, and blood pressure is 95/52 mm Hg. A flow-volume loop obtained via pulmonary function testing is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Decreased central respiratory drive
- B. Neuromuscular blockade
- C. Bronchial hyperresponsiveness
- D. Rupture of an alveolar bleb
- E. Type I hypersensitivity reaction (Correct Answer)
Pulmonary complications Explanation: ***Type I hypersensitivity reaction***
- The patient's acute shortness of breath, **tachycardia (pulse 108/min)**, **hypotension (95/52 mm Hg)**, and tachypnea (respirations 26/min) immediately post-surgery are highly suggestive of **anaphylaxis**, which is a severe, systemic type I hypersensitivity reaction.
- The sudden onset shortly after general anesthesia and initiation of prophylactic cefazolin points to a potential allergic reaction to a medication administered during this period (e.g., **antibiotics**, **neuromuscular blockers**, anesthetics).
*Decreased central respiratory drive*
- This would typically lead to **bradypnea** or hypopnea rather than the tachypnea seen in this patient.
- While opioids like morphine can depress respiratory drive, the patient's respiratory rate of 26/min indicates an *increased* drive.
*Neuromuscular blockade*
- Residual neuromuscular blockade would cause respiratory muscle weakness, leading to **shallow breathing** and potentially hypoventilation, but not typically the acute onset of shortness of breath with tachypnea and systemic hemodynamic instability observed here.
- The immediate onset of symptoms also points away from persistent effects of intraoperative neuromuscular blockers, which are usually reversed before emergence.
*Bronchial hyperresponsiveness*
- While the patient is a smoker, which can predispose to respiratory issues, **bronchial hyperresponsiveness** (e.g., asthma exacerbation) typically presents with **wheezing**, prolonged expiration, and often hypoxemia, which are not described.
- The severe hypotension and acute onset of systemic symptoms are not typical features of an isolated asthma flare-up.
*Rupture of an alveolar bleb*
- A ruptured bleb can cause a **pneumothorax**, leading to sudden shortness of breath and chest pain.
- However, it would not typically cause **systemic hypotension** or tachycardia to this degree without other signs of tension pneumothorax (e.g., tracheal deviation, absent breath sounds).
Pulmonary complications US Medical PG Question 8: A 55-year-old man presents to his primary care physician for a wellness checkup. The patient has a past medical history of alcohol abuse and is currently attending alcoholics anonymous with little success. He is currently drinking roughly 1L of hard alcohol every day and does not take his disulfiram anymore. Which of the following findings is most likely to also be found in this patient?
- A. Dysdiadochokinesia (Correct Answer)
- B. Microcytic anemia
- C. Constipation
- D. Decreased CNS NMDA activity
- E. Increased transketolase activity
Pulmonary complications Explanation: ***Dysdiadochokinesia***
- Chronic **alcohol abuse** can lead to cerebellar degeneration, a condition characterized by damage to the **cerebellum**.
- **Dysdiadochokinesia**, the impaired ability to perform rapidly alternating movements, is a classic sign of **cerebellar dysfunction**.
*Microcytic anemia*
- **Chronic alcohol abuse** typically causes **macrocytic anemia** due to folate deficiency, or less commonly, iron deficiency anemia from gastrointestinal bleeding.
- **Microcytic anemia** is usually associated with **iron deficiency** (often due to chronic blood loss) or **thalassemia**, neither of which are suggested here.
*Constipation*
- While various factors can cause constipation, **chronic alcohol abuse** is more commonly associated with **diarrhea** due to alterations in gut motility and malabsorption.
- Constipation is not a direct or prominent feature of **alcoholism**.
*Decreased CNS NMDA activity*
- **Chronic alcohol abuse** leads to an **upregulation of NMDA receptors** in the brain as a compensatory mechanism against alcohol's inhibitory effects on the central nervous system.
- When alcohol consumption ceases, this upregulated NMDA activity contributes to the **excitatory symptoms of alcohol withdrawal**, such as seizures and delirium tremens.
*Increased transketolase activity*
- **Transketolase activity** is usually **decreased** in chronic alcoholics due to **thiamine deficiency**, as thiamine (vitamin B1) is a critical cofactor for this enzyme.
- A **decrease** in transketolase activity is a key diagnostic indicator for thiamine deficiency, which contributes to conditions like **Wernicke-Korsakoff syndrome**.
Pulmonary complications US Medical PG Question 9: A 5-year-old child is brought to a pediatric clinic by his mother for a rash that started a few days ago. The mother adds that her son has also had a fever and sore throat since last week. His immunizations are up to date. On examination, a rash is present over the trunk and upper extremities and feels like sandpaper to touch. An oropharyngeal examination is suggestive of exudative pharyngitis with a white coat over the tongue. The physician swabs the throat and uses the swab in a rapid antigen detection test kit. He also sends the sample for microbiological culture. The physician then recommends empiric antibiotic therapy and tells the mother that if the boy is left untreated, the likelihood of developing a complication later in life is very high. Which of the following best explains the mechanism underlying the development of the complication the physician is talking about?
- A. Antigenic shift
- B. Bacterial tissue invasion
- C. Toxin-mediated cellular damage
- D. Molecular mimicry (Correct Answer)
- E. Genetic drift
Pulmonary complications Explanation: ***Molecular mimicry***
- The clinical presentation suggests **streptococcal pharyngitis** (sore throat, fever, sandpaper rash, exudative pharyngitis), which, if untreated, can lead to **rheumatic fever**.
- **Molecular mimicry** occurs when antibodies produced against streptococcal M protein cross-react with self-antigens in the heart, joints, and brain, causing auto-immune damage characteristic of rheumatic fever.
*Antigenic shift*
- This mechanism involves **major genetic re-assortment** in viruses (e.g., influenza A) leading to new strains, which is not relevant to complications from bacterial infections like strep throat.
- It results in pandemics due to a lack of pre-existing immunity in the population, unlike the autoimmune sequelae of bacterial infections.
*Bacterial tissue invasion*
- While bacteria can invade tissues, the serious long-term complications of streptococcal pharyngitis (like rheumatic fever) are not primarily due to **direct tissue invasion** by the bacteria themselves.
- Instead, the tissue damage results from a **post-infectious autoimmune response**.
*Toxin-mediated cellular damage*
- **Streptococcal toxins** (e.g., erythrogenic toxins) are responsible for the rash (scarlatiniform rash or scarlet fever) but not for the specific long-term autoimmune complications like rheumatic fever.
- Toxin-mediated damage occurs acutely during the infection, whereas rheumatic fever is a delayed immune-mediated sequela.
*Genetic drift*
- This mechanism describes **minor genetic mutations** that accumulate over time in viruses (e.g., influenza), leading to seasonal epidemics.
- It does not explain the autoimmune complications associated with bacterial infections such as those caused by *Streptococcus pyogenes*.
Pulmonary complications US Medical PG Question 10: A 31-year-old woman is brought to the emergency department 25 minutes after sustaining a gunshot wound to the neck. She did not lose consciousness. On arrival, she has severe neck pain. She appears anxious. Her temperature is 37°C (98.6°F), pulse is 105/min, respirations are 25/min, and blood pressure is 100/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. She is oriented to person, place, and time. Examination shows a bullet entrance wound in the right posterior cervical region of the neck. There is no exit wound. Carotid pulses are palpable bilaterally. There are no carotid bruits. Sensation to pinprick and light touch is normal. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. In addition to intravenous fluid resuscitation, which of the following is the most appropriate next step in the management of this patient?
- A. Laryngoscopy
- B. Surgical exploration
- C. Barium swallow
- D. CT angiography (Correct Answer)
- E. Esophagoscopy
Pulmonary complications Explanation: ***CT angiography***
- This patient has a **penetrating neck injury** with significant concern for vascular compromise given the mechanism (gunshot wound) and location (posterior cervical region).
- **CT angiography** is the most appropriate initial imaging study to evaluate for **vascular injury** (e.g., artery dissection, pseudoaneurysm, active bleeding) and often provides information about potential airway or esophageal damage.
*Laryngoscopy*
- While airway injury is a concern with neck trauma, this patient has a **stable airway** (oxygen saturation 96%, no stridor, clear lungs).
- Laryngoscopy is more indicated for direct evaluation of the **larynx and pharynx** if there are signs of airway compromise or difficulty breathing.
*Surgical exploration*
- **Surgical exploration** is typically reserved for patients with clear signs of **hemodynamic instability** or definitive evidence of significant injury (e.g., expanding hematoma, pulsatile bleeding) after initial imaging.
- Given the patient's relative stability, a less invasive diagnostic approach is warranted first.
*Barium swallow*
- A **barium swallow** (esophagography) is used to evaluate for **esophageal injury**.
- While esophageal damage is possible with a gunshot wound to the neck, CTA can often provide indirect evidence and is generally performed first due to the higher index of suspicion for vascular injury.
*Esophagoscopy*
- **Esophagoscopy** is a more invasive procedure for directly visualizing the esophagus.
- It would be considered if there is suspicion for esophageal injury, especially after initial imaging, but **CTA is preferred first** for broader assessment of vascular and other structures.
More Pulmonary complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.