Neurological complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neurological complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neurological complications US Medical PG Question 1: A 24-year-old man presents to the emergency department after a motor vehicle collision. He was in the front seat and unrestrained driver in a head on collision. His temperature is 99.2°F (37.3°C), blood pressure is 90/65 mmHg, pulse is 152/min, respirations are 16/min, and oxygen saturation is 100% on room air. Physical exam is notable for a young man who opens his eyes spontaneously and is looking around. He answers questions with inappropriate responses but discernible words. He withdraws from pain but does not have purposeful movement. Which of the following is this patient's Glasgow coma scale?
- A. 9
- B. 15
- C. 7
- D. 11 (Correct Answer)
- E. 13
Neurological complications Explanation: ***11***
- **Eye-opening (E)**: The patient opens his eyes spontaneously, scoring **E4**.
- **Verbal response (V)**: He gives inappropriate responses but discernible words, scoring **V3**.
- **Motor response (M)**: He withdraws from pain but does not have purposeful movement, scoring **M4**.
- Therefore, the total Glasgow Coma Scale (GCS) score is **E4 + V3 + M4 = 11**.
*9*
- This score would imply a lower verbal or motor response, such as **incomprehensible sounds (V2)** or **abnormal flexion (M3)**, which is not consistent with the patient's presentation.
- For example, E4 + V2 + M3 would equal 9.
*15*
- A GCS of 15 indicates **normal neurological function**, meaning the patient would be fully oriented, obey commands, and open eyes spontaneously, which is not the case here.
- This score is for a patient who is fully conscious and responsive.
*7*
- A GCS of 7 suggests a **severe brain injury**, which would typically present with a much poorer response, such as **no verbal response (V1)** or **abnormal extension (M2)**.
- For example, E4 + V1 + M2 would equal 7.
*13*
- This score would mean a higher level of consciousness, such as **confused conversation (V4)** or **localizing pain (M5)**, which is better than the patient's described responses.
- For example, E4 + V4 + M5 would equal 13.
Neurological complications US Medical PG Question 2: A 34-year-old woman is recovering in the post-operative unit following a laparoscopic procedure for chronic endometriosis. She had initially presented with complaints of painful menstrual cramps that kept her bedridden most of the day. She also mentioned to her gynecologist that she had been diagnosed with endometriosis 4 years ago, and she could not find a medication or alternative therapeutic measure that helped. Her medical history was significant for surgery she had 6 years ago to remove tumors she had above her kidneys, after which she was prescribed hydrocortisone. An hour after the laparoscopic procedure, she calls the nurse because she is having difficulty breathing. The nurse records her vital signs include: blood pressure 85/55 mm Hg, respirations 20/min, and pulse 115/min. The patient suddenly loses consciousness. Intravenous fluids are started immediately. She gains consciousness, but her blood pressure is unchanged. Which of the following is the most likely cause of the hypotension?
- A. Bleeding profusely through the surgical site
- B. Improper supplementation of steroids (Correct Answer)
- C. Infection involving the suture line
- D. High doses of anesthetic drugs
- E. Loss of fluids during the procedure
Neurological complications Explanation: ***Improper supplementation of steroids***
- The patient's history of **bilateral adrenalectomy (tumors above kidneys)** for which she was prescribed **hydrocortisone** indicates **adrenal insufficiency**. Stressful events like surgery require an increased dose of steroids, and improper supplementation can lead to an **adrenal crisis**.
- The symptoms of **hypotension, tachycardia, and loss of consciousness** are characteristic of an **adrenal crisis (acute adrenal insufficiency)**, which occurs when the body lacks sufficient cortisol during stress.
*Bleeding profusely through the surgical site*
- While **hemorrhage** can cause hypotension and tachycardia, the patient regained consciousness with IV fluids but her **blood pressure remained unchanged**, which is less typical for isolated blood loss if volume is restored without addressing the underlying cause.
- There is no direct mention of visible bleeding, the prompt only states the patient lost consciousness and her blood pressure is unchanged.
*Infection involving the suture line*
- **Surgical site infections** typically manifest several days post-op, presenting with **fever, erythema, and purulent drainage**, not acute hypotension and loss of consciousness an hour after surgery.
- The immediate post-operative timeline and systemic symptoms are not consistent with a localized wound infection as the primary cause of this acute decline.
*High doses of anesthetic drugs*
- Anesthetic drugs can cause **vasodilation and hypotension**. However, their effects are usually transient and would likely resolve more completely with IV fluids, especially an hour after a laparoscopic procedure.
- If it was due to anesthetic drugs, the patient's blood pressure would likely normalize with fluid administration once the effects of the anesthetic began to wear off, which is not the case here.
*Loss of fluids during the procedure*
- **Fluid loss** during surgery can cause hypotension, but intravenous fluids were administered, and the patient regained consciousness.
- If fluid loss were the sole cause, resolving consciousness and maintaining low blood pressure typically indicates the fluid loss was not completely compensated, but the primary cause for the persistent hypotension is not just volume.
Neurological complications US Medical PG Question 3: A 59-year-old man is brought to the emergency department by a coworker for right arm weakness and numbness. The symptoms started suddenly 2 hours ago. His coworker also noticed his face appears to droop on the right side and his speech is slurred. He has a history of hypertension, hyperlipidemia, type 2 diabetes, and peripheral arterial disease. He works as a partner at a law firm and has been under more stress than usual lately. His father died of a stroke at age 70. The patient has smoked a pack of cigarettes daily for the last 40 years. He drinks two pints (750 mL) of whiskey each week. He takes aspirin, atorvastatin, lisinopril, and metformin daily. He is 167.6 cm (5 ft 6 in) tall and weighs 104.3 kg (230 lb); BMI is 37 kg/m2. His temperature is 37.1°C (98.8°F), pulse is 92/min, respirations are 15/min, and blood pressure is 143/92 mm Hg. He is fully alert and oriented. Neurological examination shows asymmetry of the face with droop of the lips on the right. There is 3/5 strength in right wrist flexion and extension, and right finger abduction. Sensation to light touch and pinprick is reduced throughout the right arm. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Excessive alcohol intake
- B. Obesity
- C. Hypertension (Correct Answer)
- D. Increased stress
- E. Hyperlipidemia
Neurological complications Explanation: ***Hypertension***
- **Hypertension is the single most important modifiable risk factor for stroke**, accounting for approximately 50% of stroke risk in population studies
- This patient's blood pressure of **143/92 mm Hg despite being on lisinopril** indicates poorly controlled hypertension, which significantly increases stroke risk
- Hypertension directly damages blood vessels through chronic endothelial injury and accelerates **atherosclerosis**, leading to both ischemic and hemorrhagic stroke
*Excessive alcohol intake*
- Heavy alcohol consumption (>2 drinks/day) increases stroke risk, particularly hemorrhagic stroke
- This patient's intake of two pints weekly (~5 drinks) is moderate-to-heavy but not the strongest risk factor compared to poorly controlled hypertension
- The association between alcohol and stroke is less consistent than that of hypertension
*Obesity*
- **Obesity (BMI 37 kg/m²)** increases stroke risk indirectly by promoting hypertension, diabetes, and dyslipidemia
- It is an important risk factor but acts primarily through these intermediate mechanisms rather than as a direct cause
- Hypertension remains the more potent and direct predisposing factor
*Increased stress*
- Chronic stress may contribute to stroke risk through effects on blood pressure, inflammation, and health behaviors
- However, stress is a **weak and indirect risk factor** with inconsistent epidemiological evidence
- It does not compare to the well-established, quantifiable impact of hypertension
*Hyperlipidemia*
- **Hyperlipidemia** promotes atherosclerosis and is an established risk factor for ischemic stroke
- The patient is on atorvastatin, which likely provides some protection
- While significant, hypertension has consistently been shown to have the **greatest population-attributable risk for stroke** among all modifiable factors
Neurological complications US Medical PG Question 4: A 68-year-old community-dwelling woman is transported to the emergency department with decreased consciousness, headache, and nausea. The symptoms began after the patient had a syncopal episode and fell at her home. She has a history of arterial hypertension and atrial fibrillation. Her current medications include hydrochlorothiazide, lisinopril, metoprolol, and warfarin. On admission, her blood pressure is 140/90 mm Hg, heart rate is 83/min and irregular, respiratory rate is 12/min, and temperature is 36.8°C (98.4°F). She is conscious and verbally responsive, albeit confused. She is able to follow motor commands. Her pupils are round, equal, and poorly reactive to light. She is unable to abduct both eyes on an eye movement examination. She has decreased strength and increased tone (Ashworth 1/4) and reflexes (3+) in her right upper and lower extremities. Her lungs are clear to auscultation. The cardiac examination shows the presence of S3 and a pulse deficit. A head CT scan is shown in the picture. Which of the following led to the patient’s condition?
- A. Rupture of a saccular aneurysm in the carotid circulation region
- B. Rupture of the middle meningeal artery
- C. Rupture of the cerebral bridging veins (Correct Answer)
- D. Rupture of the vein of Galen
- E. Laceration of the leptomeningeal blood vessels
Neurological complications Explanation: ***Rupture of the cerebral bridging veins***
- This patient presents with symptoms of **subdural hematoma** (decreased consciousness, headache, confusion), which is typically caused by the tearing of **bridging veins** traversing the subdural space, especially after a fall in elderly individuals due to brain atrophy.
- Her use of **warfarin** and the presence of **atrial fibrillation** significantly increase her risk of bleeding complications from trauma, making a subdural hematoma due to bridging vein rupture highly likely.
*Rupture of a saccular aneurysm in the carotid circulation region*
- A ruptured **saccular aneurysm** typically causes a **subarachnoid hemorrhage**, characterized by a "thunderclap" headache, meningismus, and rapid neurological deterioration.
- While she has a headache, the focal neurological deficits and the likely appearance of a subdural hematoma on CT (though not explicitly described, it's implied by the mechanism) are less consistent with a pure subarachnoid bleed from a saccular aneurysm alone.
*Rupture of the middle meningeal artery*
- Rupture of the **middle meningeal artery** typically causes an **epidural hematoma**, characterized by a **lucid interval** followed by rapid neurological decline and a characteristic **lenticular** (lens-shaped) lesion on CT.
- The patient's presentation with gradual symptoms and likely CT findings do not fit the typical pattern of an epidural hematoma.
*Rupture of the vein of Galen*
- **Vein of Galen malformations** are rare congenital vascular lesions usually presenting in **infancy or childhood** with heart failure or hydrocephalus.
- This is an adult patient with an acute presentation following a fall, which is inconsistent with the typical presentation or cause of a ruptured vein of Galen malformation.
*Laceration of the leptomeningeal blood vessels*
- Laceration of **leptomeningeal blood vessels** (those within the pia or arachnoid mater) would result in a **subarachnoid hemorrhage**, presenting with signs of meningeal irritation and global cerebral dysfunction.
- While a subarachnoid hemorrhage can occur, the clinical picture, particularly the emphasis on a fall and warfarin use in an elderly patient, points more strongly towards a subdural hematoma secondary to bridging vein rupture rather than isolated leptomeningeal vessel damage.
Neurological complications US Medical PG Question 5: Two hours after undergoing elective cholecystectomy with general anesthesia, a 41-year-old woman is evaluated for decreased mental status. BMI is 36.6 kg/m2. Respirations are 18/min and blood pressure is 126/73 mm Hg. Physical examination shows the endotracheal tube in normal position. She does not respond to sternal rub and gag reflex is absent. Arterial blood gas analysis on room air shows normal PO2 and PCO2 levels. Which of the following anesthetic properties is the most likely cause of these findings?
- A. Low blood solubility
- B. High lipid solubility (Correct Answer)
- C. Low brain-blood partition coefficient
- D. High minimal alveolar concentration
- E. Low cytochrome P450 activity
Neurological complications Explanation: ***High lipid solubility***
- Anesthetics with **high lipid solubility** accumulate in **adipose tissue** and are slowly released, prolonging their effect, especially in obese patients.
- The patient's **obesity (BMI 36.6 kg/m2)** contributes to a larger reservoir for lipid-soluble drugs, leading to delayed recovery and decreased mental status.
*Low blood solubility*
- **Low blood solubility** implies a rapid equilibrium between the lungs and the blood, leading to a **faster onset and offset** of anesthetic action.
- This property would result in a quicker recovery from anesthesia, which contradicts the patient's prolonged unconsciousness.
*Low brain-blood partition coefficient*
- A **low brain-blood partition coefficient** means the anesthetic does not accumulate significantly in brain tissue relative to blood.
- Agents with this property equilibrate quickly and leave the brain rapidly upon discontinuation, resulting in **fast recovery**, which is inconsistent with the patient's persistent decreased mental status.
*High minimal alveolar concentration*
- **High minimal alveolar concentration (MAC)** means that a higher concentration of the anesthetic gas is required to produce immobility in 50% of patients.
- A high MAC describes the **potency** of an anesthetic and does not directly explain prolonged recovery or decreased mental status in an obese patient, but rather indicates that a larger dose or concentration was needed to achieve anesthesia.
*Low cytochrome P450 activity*
- **Low cytochrome P450 activity** would lead to slower metabolism of drugs that are primarily cleared by this system, potentially prolonging their effects.
- While relevant for some drugs, the primary issue for inhaled anesthetics is their **physical distribution and elimination**, not typically metabolic clearance via Cytochrome P450 enzymes.
Neurological complications US Medical PG Question 6: An 88-year-old woman with no significant medical history is brought to the emergency room by her daughter after a fall, where the woman lightly hit her head against a wall. The patient is lucid and complains of a mild headache. The daughter indicates that her mother did not lose consciousness after the fall. On exam, there are no focal neurological deficits, but you decide to perform a CT scan to be sure there is no intracranial bleeding. The CT scan is within normal limits and head MRI is performed (shown). Which of the following conditions has the most similar risk factor to this patient's condition?
- A. Pulmonary embolism
- B. Raynaud's phenomenon
- C. Prinzmetal's angina
- D. Abdominal aortic aneurysm
- E. Thoracic aortic aneurysm (Correct Answer)
Neurological complications Explanation: ***Thoracic aortic aneurysm***
- The MRI images show numerous **microhemorrhages** (dark spots on the GRE/SWI sequences), indicative of **cerebral amyloid angiopathy (CAA)**, a common cause of lobar intracerebral hemorrhage in the elderly.
- CAA is most strongly associated with **advanced age** (the primary risk factor), and both CAA and **thoracic aortic aneurysm (TAA)** can be associated with **underlying connective tissue abnormalities** and vascular wall weakening processes.
- While the exact pathophysiology differs, both conditions involve progressive vascular wall degeneration that increases with age.
*Abdominal aortic aneurysm*
- While AAA is strongly associated with **advanced age**, **hypertension**, and **smoking**, it is primarily driven by **atherosclerotic degeneration** rather than the amyloid deposition seen in CAA.
- AAA has a particularly strong association with smoking (the most important modifiable risk factor), which is not characteristic of CAA.
*Pulmonary embolism*
- Primarily caused by **venous thromboembolism** (VTE) due to factors like immobility, surgery, cancer, and hypercoagulable states, which are distinct from CAA risk factors.
- While age is a risk factor for PE, the underlying mechanisms (thrombosis vs. vascular wall amyloid deposition) differ fundamentally.
*Raynaud's phenomenon*
- Characterized by **vasospasm** of small arteries and arterioles, typically triggered by cold or stress, and is often associated with connective tissue diseases.
- Its pathophysiology is unrelated to the progressive vascular wall degeneration and amyloid deposition seen in CAA.
*Prinzmetal's angina*
- Caused by **coronary artery spasm**, leading to transient myocardial ischemia, often occurring at rest and typically not associated with age-related vascular degeneration.
- The mechanism is localized vascular spasm rather than widespread degenerative arterial disease or amyloid deposition.
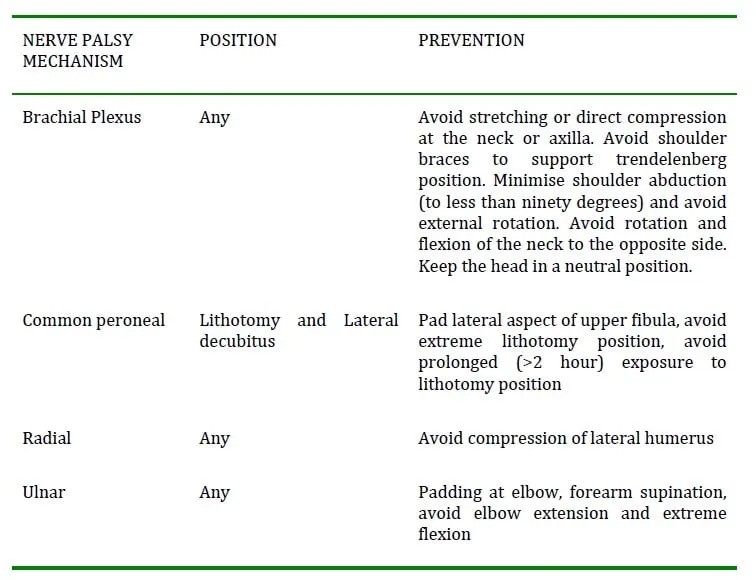
Neurological complications US Medical PG Question 7: A 23-year-old college student was playing basketball when he fell directly onto his left elbow. He had sudden, intense pain and was unable to move his elbow. He was taken immediately to the emergency room by his teammates. He has no prior history of trauma or any chronic medical conditions. His blood pressure is 128/84 mm Hg, the heart rate is 92/min, and the respiratory rate is 14/min. He is in moderate distress and is holding onto his left elbow. On physical examination, pinprick sensation is absent in the left 5th digit and the medial aspect of the left 4th digit. Which of the following is the most likely etiology of this patient’s condition?
- A. Axillary neuropathy
- B. Median neuropathy
- C. Radial neuropathy
- D. Musculocutaneous neuropathy
- E. Ulnar neuropathy (Correct Answer)
Neurological complications Explanation: ***Ulnar neuropathy***
- Direct trauma to the elbow, combined with **pinprick sensation loss** in the **5th digit** and the **medial aspect of the 4th digit**, is highly indicative of **ulnar nerve injury**.
- The ulnar nerve passes through the **cubital tunnel** at the elbow, making it vulnerable to compression or trauma from direct falls.
*Axillary neuropathy*
- An **axillary nerve injury** typically presents with weakness in **shoulder abduction** (deltoid muscle) and sensory loss over the **lateral aspect of the shoulder**.
- This clinical picture does not match the patient's sensory deficits in the fingers.
*Median neuropathy*
- **Median nerve injury** at the elbow would typically cause sensory loss in the **first three fingers and the lateral half of the fourth finger**, along with **weakness in thumb opposition** and **flexion of the index and middle fingers**.
- The sensory loss described in the patient does not align with median nerve distribution.
*Radial neuropathy*
- **Radial nerve injury** at the elbow level would primarily result in **wrist drop** and sensory loss over the **dorsal aspect of the hand**, particularly the **first three and a half digits**.
- These are not the clinical findings presented by the patient.
*Musculocutaneous neuropathy*
- **Musculocutaneous nerve injury** would cause weakness in **elbow flexion** (biceps and brachialis muscles) and sensory loss over the **lateral forearm**.
- The patient's reported sensory loss is in a different distribution and no specific motor deficits of elbow flexion are mentioned.
Neurological complications US Medical PG Question 8: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Neurological complications Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
Neurological complications US Medical PG Question 9: A 24-year-old woman at 36 weeks pregnant presents to the emergency department with a headache and abdominal pain. The woman has no known past medical history and has inconsistently followed up with an obstetrician for prenatal care. Her temperature is 98.5°F (36.9°C), blood pressure is 163/101 mmHg, pulse is 90/min, respirations are 16/min, and oxygen saturation is 97% on room air. Prior to performing the physical exam, the patient experiences a seizure, which resolves after 60 seconds. Which of the following is the best management for this patient?
- A. Diazepam, magnesium, and continuous monitoring
- B. Magnesium and continuous monitoring
- C. Nifedipine and cesarean section
- D. Magnesium and cesarean section (Correct Answer)
- E. Magnesium and labetalol
Neurological complications Explanation: **Magnesium and cesarean section**
- The patient's presentation with **headache**, **abdominal pain**, and **hypertension** followed by a **seizure** is classic for **eclampsia**, a severe complication of pre-eclampsia.
- **Magnesium sulfate** is the first-line treatment for seizure control and prevention in eclampsia, while **delivery (cesarean section)** is the definitive treatment since it removes the source of the disease (the placenta).
*Diazepam, magnesium, and continuous monitoring*
- While **magnesium** is correct for seizure management, **diazepam** is typically reserved as a second-line agent if magnesium is ineffective or contraindicated.
- The definitive management of eclampsia is delivery; continuous monitoring alone is insufficient without plans for delivery.
*Magnesium and continuous monitoring*
- **Magnesium** is indeed the critical first step for seizure management in eclampsia.
- However, continuous monitoring without addressing the underlying cause via **delivery** is not sufficient definitive management for eclampsia.
*Nifedipine and cesarean section*
- **Nifedipine** is an antihypertensive and can be used to manage severe hypertension in pregnancy, but it is not the primary treatment for active seizures or seizure prevention in eclampsia.
- While a **cesarean section** is appropriate for delivery, **magnesium** is crucial for immediate seizure control.
*Magnesium and labetalol*
- **Magnesium** is appropriate for seizure management.
- **Labetalol** is an antihypertensive agent used for severe hypertension in pregnancy, but it does not treat the seizure or the underlying eclampsia definitively; delivery is still required.
Neurological complications US Medical PG Question 10: A 55-year-old man presents to his primary care physician for a wellness checkup. The patient has a past medical history of alcohol abuse and is currently attending alcoholics anonymous with little success. He is currently drinking roughly 1L of hard alcohol every day and does not take his disulfiram anymore. Which of the following findings is most likely to also be found in this patient?
- A. Dysdiadochokinesia (Correct Answer)
- B. Microcytic anemia
- C. Constipation
- D. Decreased CNS NMDA activity
- E. Increased transketolase activity
Neurological complications Explanation: ***Dysdiadochokinesia***
- Chronic **alcohol abuse** can lead to cerebellar degeneration, a condition characterized by damage to the **cerebellum**.
- **Dysdiadochokinesia**, the impaired ability to perform rapidly alternating movements, is a classic sign of **cerebellar dysfunction**.
*Microcytic anemia*
- **Chronic alcohol abuse** typically causes **macrocytic anemia** due to folate deficiency, or less commonly, iron deficiency anemia from gastrointestinal bleeding.
- **Microcytic anemia** is usually associated with **iron deficiency** (often due to chronic blood loss) or **thalassemia**, neither of which are suggested here.
*Constipation*
- While various factors can cause constipation, **chronic alcohol abuse** is more commonly associated with **diarrhea** due to alterations in gut motility and malabsorption.
- Constipation is not a direct or prominent feature of **alcoholism**.
*Decreased CNS NMDA activity*
- **Chronic alcohol abuse** leads to an **upregulation of NMDA receptors** in the brain as a compensatory mechanism against alcohol's inhibitory effects on the central nervous system.
- When alcohol consumption ceases, this upregulated NMDA activity contributes to the **excitatory symptoms of alcohol withdrawal**, such as seizures and delirium tremens.
*Increased transketolase activity*
- **Transketolase activity** is usually **decreased** in chronic alcoholics due to **thiamine deficiency**, as thiamine (vitamin B1) is a critical cofactor for this enzyme.
- A **decrease** in transketolase activity is a key diagnostic indicator for thiamine deficiency, which contributes to conditions like **Wernicke-Korsakoff syndrome**.
More Neurological complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.