Cardiac complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiac complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
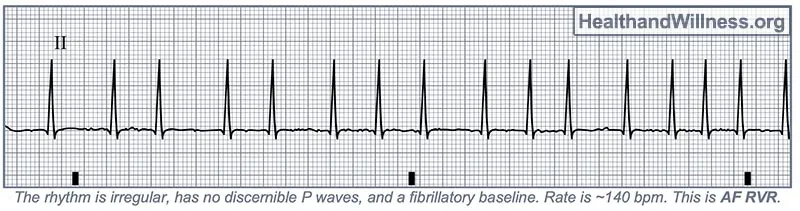
Cardiac complications US Medical PG Question 1: A 29-year-old woman with Wolff-Parkinson-White syndrome presents to her cardiologist’s office for a follow-up visit. She collapsed at her job and made a trip to the emergency department 1 week ago. At that time, she received a diagnosis of atrial fibrillation with rapid ventricular response and hemodynamic instability. While in the emergency department, she underwent direct-current cardioversion to return her heart to sinus rhythm. Her current medications include procainamide. At the cardiologist’s office, her heart rate is 61/min, respiratory rate is 16/min, the temperature is 36.5°C (97.7°F), and blood pressure is 118/60 mm Hg. Her cardiac examination reveals a regular rhythm and a I/VI systolic ejection murmur best heard at the right upper sternal border. An ECG obtained in the clinic is shown. Which of the following is the most appropriate treatment to prevent further episodes of tachyarrhythmia?
- A. Begin anticoagulation with dabigatran
- B. Add verapamil to her medication regimen
- C. Begin anticoagulation with warfarin
- D. Refer her for electrophysiology (EP) study and ablation (Correct Answer)
- E. Refer her for right heart catheterization
Cardiac complications Explanation: ***Refer her for electrophysiology (EP) study and ablation***
- This patient has **Wolff-Parkinson-White (WPW) syndrome** and experienced a life-threatening episode of **atrial fibrillation with rapid ventricular response (AFib with RVR)** and **hemodynamic instability**, indicating a high-risk accessory pathway.
- **Catheter ablation** of the accessory pathway is the definitive treatment to eliminate the re-entrant circuit and prevent future tachyarrhythmia episodes and sudden cardiac death in symptomatic WPW patients.
*Begin anticoagulation with dabigatran*
- While anticoagulation is indicated for stroke prevention in AFib, this patient's primary risk is not stroke but rather recurrent, potentially fatal, **tachyarrhythmias due to WPW**.
- Current guidelines suggest that anticoagulation is not routinely needed for AFib in the setting of WPW unless other risk factors for stroke are present (e.g., high **CHA₂DS₂-VASc score** for non-valvular AFib), which are not mentioned here for a 29-year-old.
*Add verapamil to her medication regimen*
- **Calcium channel blockers** like verapamil are contraindicated in WPW syndrome with AFib.
- They can block the normal AV nodal conduction, shunting more impulses down the **accessory pathway** and potentially accelerating the ventricular rate, leading to **ventricular fibrillation**.
*Begin anticoagulation with warfarin*
- Similar to dabigatran, anticoagulation with warfarin is primarily for **stroke prevention in AFib**, not for preventing the tachyarrhythmia itself in WPW.
- The immediate and most critical concern for this patient is the risk of recurrent, life-threatening **re-entrant tachyarrhythmias** via the accessory pathway.
*Refer her for right heart catheterization*
- A **right heart catheterization** is used to measure pressures and oxygen saturations in the right side of the heart and pulmonary arteries, typically to evaluate for conditions like pulmonary hypertension or heart failure.
- It is not indicated for the diagnosis or treatment of **supraventricular tachycardias** or **accessory pathways** like in WPW syndrome.
Cardiac complications US Medical PG Question 2: A 66-year-old man comes to the emergency department because of a 1-day history of chest pain, palpitations, and dyspnea on exertion. He had a similar episode 3 days ago and was diagnosed with an inferior wall myocardial infarction. He was admitted and a percutaneous transluminal coronary angioplasty was successfully done that day. A fractional flow reserve test during the procedure showed complete resolution of the stenosis. Laboratory tests including serum glucose, lipids, and blood count were within normal limits. He was discharged the day after the procedure on a drug regimen of aspirin, simvastatin, and isosorbide dinitrate. At the time of discharge, he had no chest pain or dyspnea. Presently, his vitals are normal and ECG at rest shows new T-wave inversion. Which of the following is the most reliable test for rapidly establishing the diagnosis in this patient?
- A. Creatine kinase MB
- B. Lactate dehydrogenase
- C. Copeptin
- D. Aspartate aminotransferase
- E. Cardiac troponin T (Correct Answer)
Cardiac complications Explanation: ***Cardiac troponin T***
- **Cardiac troponin T** is a highly sensitive and specific biomarker for **myocardial injury**, making it the most reliable test for rapidly diagnosing acute coronary syndrome or re-infarction.
- Its elevation indicates ongoing **myocardial necrosis**, even after a recent MI, and is crucial for guiding immediate management.
*Creatine kinase MB*
- While CK-MB is used for diagnosing myocardial infarction, its levels can also be elevated in cases of **skeletal muscle injury** or **after cardiac procedures**, reducing its specificity in this context.
- CK-MB also has a **shorter window of elevation** compared to troponins, potentially missing later presentations of myocardial injury.
*Lactate dehydrogenase*
- **LDH** is a relatively **nonspecific marker** that can elevate due to various conditions affecting different organs (e.g., liver disease, hemolysis, renal injury).
- Its elevation onset is **slower** and its diagnostic window is longer, making it less suitable for rapid diagnosis of acute myocardial injury.
*Copeptin*
- **Copeptin** is a marker of **endogenous stress** and is often used in conjunction with troponins to rule out NSTEMI, especially at early presentation.
- However, it is not a direct marker of myocardial necrosis itself and is **not as specific** as troponin for diagnosing a re-infarction.
*Aspartate aminotransferase*
- **AST** is a **nonspecific enzyme** found in various tissues, including the liver, skeletal muscle, and heart.
- Elevated AST levels are frequently seen in **liver damage** and are not a primary biomarker for diagnosing acute myocardial infarction or re-infarction.
Cardiac complications US Medical PG Question 3: A 65-year-old man presents to his primary care physician for a pre-operative evaluation. He is scheduled for cataract surgery in 3 weeks. His past medical history is notable for diabetes, hypertension, and severe osteoarthritis of the right knee. His medications include metformin, hydrochlorothiazide, lisinopril, and aspirin. His surgeon ordered blood work 1 month ago, which showed a hemoglobin of 14.2 g/dL, INR of 1.2, and a hemoglobin A1c of 6.9%. His vital signs at the time of the visit show BP: 130/70 mmHg, Pulse: 80, RR: 12, and T: 37.2 C. He has no current complaints and is eager for his surgery. Which of the following is the most appropriate course of action for this patient at this time?
- A. Tell the patient he will have to delay his surgery for at least 1 year
- B. Medically clear the patient for surgery (Correct Answer)
- C. Repeat the patient's CBC and coagulation studies
- D. Schedule the patient for a stress test and ask him to delay surgery for at least 6 months
- E. Perform an EKG
Cardiac complications Explanation: **Medically clear the patient for surgery**
- The patient's **blood pressure is well-controlled** (130/70 mmHg), and his **hemoglobin A1c of 6.9%** indicates good glycemic control, both of which are favorable for elective surgery.
- He is currently on **aspirin**, which, for cataract surgery (a low-risk bleeding procedure), can generally be continued, and his **INR of 1.2 is within a safe range** for surgery.
*Tell the patient he will have to delay his surgery for at least 1 year*
- There are **no indications for such a prolonged delay** based on the provided clinical information.
- His chronic conditions (diabetes, hypertension) are **adequately managed**, and his lab values are acceptable.
*Repeat the patient's CBC and coagulation studies*
- The **existing blood work from 1 month ago is recent enough** for a pre-operative evaluation for cataract surgery, especially with no new symptoms.
- Repeating these tests without a clinical indication would be **unnecessary and inefficient**.
*Schedule the patient for a stress test and ask him to delay surgery for at least 6 months*
- The patient has **no active cardiac symptoms** (e.g., chest pain, shortness of breath), and his well-controlled hypertension does not automatically warrant a stress test for low-risk surgery.
- A stress test and a **6-month delay are not indicated** for a low-risk procedure like cataract surgery in an asymptomatic patient.
*Perform an EKG*
- While an EKG might be considered in some pre-operative evaluations for patients with cardiac risk factors, there are **no specific symptoms or significant new risk factors** presented that necessitate an EKG for this low-risk cataract surgery.
- Given his stable condition and controlled hypertension, an EKG is **not a mandatory part of medical clearance** for this procedure.
Cardiac complications US Medical PG Question 4: A 67-year-old man presents to the emergency department for squeezing and substernal chest pain. He states that he was at home eating dinner when his symptoms began. The patient has a past medical history of diabetes, hypertension, and dyslipidemia. He is currently taking atorvastatin, lisinopril, insulin, metformin, metoprolol, and aspirin. Six days ago he underwent percutaneous coronary intervention. His temperature is 99.5°F (37.5°C), blood pressure is 197/118 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam reveals an uncomfortable elderly man who is sweating. An ECG is ordered. Which of the following is the best next step in management for this patient?
- A. Stress testing
- B. Angiography (Correct Answer)
- C. Cardiac troponins
- D. Creatine kinase-MB
- E. Myoglobin
Cardiac complications Explanation: ***Correct: Angiography***
- This patient presenting with **acute chest pain 6 days post-PCI** is at high risk for **stent thrombosis or acute in-stent restenosis**, which represents a life-threatening emergency.
- Given the **clinical instability** (severe hypertension 197/118, tachycardia 120/min, diaphoresis) and classic ACS symptoms in the immediate post-PCI period, **urgent coronary angiography** is the best next step in management.
- While ECG and troponins are important diagnostic tools, this patient requires **immediate intervention** to evaluate the recent PCI site and potentially perform emergent revascularization.
- In the setting of suspected **acute stent thrombosis**, time to reperfusion is critical, and angiography allows both diagnosis and treatment.
*Incorrect: Cardiac troponins*
- While troponins are essential biomarkers for myocardial injury and should be obtained, they are a **diagnostic test** rather than definitive management.
- Waiting for troponin results would delay definitive management in a patient with clear clinical evidence of ACS.
- In this high-risk post-PCI patient with active symptoms, management should not wait for biomarker confirmation.
*Incorrect: Stress testing*
- Stress testing is **absolutely contraindicated** in patients with active chest pain and suspected acute MI.
- It could precipitate further myocardial ischemia, arrhythmias, or cardiac arrest.
- Stress testing is reserved for risk stratification in stable patients or after ACS has been ruled out.
*Incorrect: Creatine kinase-MB*
- CK-MB is less sensitive and specific than troponins for myocardial injury, as it can be elevated in skeletal muscle conditions.
- It has a shorter elevation window and has largely been replaced by troponins in modern practice.
- Like troponins, it would not change the immediate management need in this clinically unstable patient.
*Incorrect: Myoglobin*
- Myoglobin lacks cardiac specificity (present in both cardiac and skeletal muscle) and has poor diagnostic accuracy for MI.
- Its rapid rise and fall make it unreliable, and it generates many false positives.
- It has no role in guiding management decisions in suspected ACS.
Cardiac complications US Medical PG Question 5: A 70-year-old male presents for an annual exam. His past medical history is notable for shortness of breath when he sleeps, and upon exertion. Recently he has experienced dyspnea and lower extremity edema that seems to be worsening. Both of these symptoms have resolved since he was started on several medications and instructed to weigh himself daily. Which of the following is most likely a component of his medical management?
- A. Lidocaine
- B. Verapamil
- C. Carvedilol (Correct Answer)
- D. Aspirin
- E. Ibutilide
Cardiac complications Explanation: ***Carvedilol***
- The patient exhibits classic symptoms of **heart failure**, such as **dyspnea on exertion**, **orthopnea** (shortness of breath when he sleeps), and **lower extremity edema**.
- **Beta-blockers** like carvedilol are essential for managing **chronic heart failure** by reducing myocardial oxygen demand and improving cardiac function.
*Lidocaine*
- **Lidocaine** is primarily an **antiarrhythmic drug** used for acute treatment of **ventricular arrhythmias**, not for chronic heart failure management.
- It works by blocking sodium channels and has no direct benefit in addressing the underlying pathophysiology of heart failure.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** typically used for hypertension, angina, and supraventricular tachyarrhythmias.
- It can have **negative inotropic effects**, which are generally contraindicated or used with extreme caution in patients with **systolic heart failure** due to its potential to worsen cardiac function.
*Aspirin*
- **Aspirin** is an **antiplatelet agent** used for primary or secondary prevention of **atherosclerotic cardiovascular disease** (e.g., in patients with coronary artery disease).
- It does not directly manage the symptoms or pathophysiology of **heart failure** unless there is a coexisting ischemic etiology.
*Ibutilide*
- **Ibutilide** is an **antiarrhythmic drug** specifically used for the rapid conversion of **atrial flutter and atrial fibrillation** of recent onset to sinus rhythm.
- It is not a medication used for the long-term management of **heart failure** symptoms described in the patient.
Cardiac complications US Medical PG Question 6: A 59-year-old woman comes to the physician for a 3-month history of progressively worsening shortness of breath on exertion and swelling of her legs. She has a history of breast cancer, which was treated with surgery followed by therapy with doxorubicin and trastuzumab 4 years ago. Cardiac examination shows an S3 gallop; there are no murmurs or rubs. Examination of the lower extremities shows pitting edema below the knees. Echocardiography is most likely to show which of the following sets of changes in this patient?
$$$ Ventricular wall thickness %%% Ventricular cavity size %%% Diastolic function %%% Aorto-ventricular pressure gradient $$$
- A. ↓ ↑ normal normal (Correct Answer)
- B. Normal normal ↓ normal
- C. ↑ ↓ ↓ normal
- D. ↑ ↓ ↓ ↑
- E. ↓ ↑ ↓ normal
Cardiac complications Explanation: ***↓ ↑ normal normal***
- Doxorubicin is an **anthracycline** known to cause **dilated cardiomyopathy**, characterized by **decreased ventricular wall thickness**, **increased ventricular cavity size**, and **preserved diastolic function**.
- The S3 gallop and pitting edema indicate **heart failure with reduced ejection fraction (HFrEF)**, consistent with dilated cardiomyopathy.
*Normal normal ↓ normal*
- This option suggests a primary issue with **diastolic function**, which is not the typical presentation of doxorubicin-induced cardiomyopathy.
- While diastolic dysfunction can occur, doxorubicin characteristically causes **systolic dysfunction** manifesting as chamber dilation and wall thinning.
*↑ ↓ ↓ normal*
- This pattern of **increased wall thickness** and **decreased cavity size** is characteristic of **hypertrophic cardiomyopathy** or **restrictive cardiomyopathy**, which are generally not caused by doxorubicin.
- Doxorubicin typically causes **cardiac muscle fiber damage** leading to thinning and dilation.
*↑ ↓ ↓ ↑*
- This option also suggests **increased wall thickness** and **decreased cavity size**, inconsistent with doxorubicin's effects on the heart.
- The **elevated aorto-ventricular pressure gradient** might indicate outflow tract obstruction or significant aortic stenosis, which are not typical sequelae of doxorubicin.
*↓ ↑ ↓ normal*
- While doxorubicin leads to **decreased wall thickness** and **increased cavity size**, the diastolic function is usually preserved early on, not decreased.
- A decrease in diastolic function might occur in later stages, but the primary and most characteristic feature due to doxorubicin is **systolic dysfunction** and chamber remodeling.
Cardiac complications US Medical PG Question 7: A 72-year-old female presents to the emergency department following a syncopal episode while walking down several flights of stairs. The patient has not seen a doctor in several years and does not take any medications. Your work-up demonstrates that she has symptoms of angina and congestive heart failure. Temperature is 36.8 degrees Celsius, blood pressure is 160/80 mmHg, heart rate is 81/min, and respiratory rate is 20/min. Physical examination is notable for a 3/6 crescendo-decrescendo systolic murmur present at the right upper sternal border with radiation to the carotid arteries. Random blood glucose is 205 mg/dL. Which of the following portends the worst prognosis in this patient?
- A. Hypertension
- B. Angina
- C. Diabetes
- D. Syncope
- E. Congestive heart failure (CHF) (Correct Answer)
Cardiac complications Explanation: ***Congestive heart failure (CHF)***
- Once **congestive heart failure** symptoms develop in severe aortic stenosis, the prognosis is very poor, with an average survival of 1.5-2 years if untreated.
- This indicates significant myocardial dysfunction and increased risk of sudden cardiac death.
*Syncope*
- **Syncope** in aortic stenosis, while serious and indicating reduced cerebral perfusion, has a slightly better prognosis than CHF, with an average survival of 2-3 years untreated.
- It often reflects a critical reduction in cardiac output, but the heart muscle itself may still have some compensatory capacity.
*Angina*
- **Angina** is a common symptom of aortic stenosis, reflecting increased myocardial oxygen demand or reduced coronary perfusion.
- Untreated, patients with angina in aortic stenosis have an average survival of 3-5 years, which is better than syncope or CHF.
*Hypertension*
- While **hypertension** is a risk factor for aortic stenosis and can exacerbate symptoms, it is not a direct symptom of severe aortic stenosis itself but rather a co-morbidity.
- Its presence doesn't inherently portend a worse prognosis for aortic stenosis than the severe symptomatic manifestations like syncope or CHF.
*Diabetes*
- **Diabetes** is a systemic disease that can accelerate atherosclerosis and increase cardiovascular risk, but it is a chronic condition rather than an acute symptom of severe aortic stenosis.
- While it complicates management and overall prognosis, its impact is not as immediate or as severe as the development of CHF directly attributable to the aortic stenosis itself.
Cardiac complications US Medical PG Question 8: A 60-year-old man presents to the emergency department with progressive dyspnea for the last 3 weeks. He complains of shortness of breath while lying flat and reports nighttime awakenings due to shortness of breath for the same duration. The patient has been a smoker for the last 30 years. Past medical history is significant for myocardial infarction 7 months ago. Current medications include metoprolol, aspirin, and rosuvastatin, but the patient is noncompliant with his medications. His temperature is 37.2°C (98.9°F), the blood pressure is 150/115 mm Hg, the pulse is 110/min, and the respiratory rate is 24/min. Oxygen saturation on room air is 88%. Chest auscultation reveals bilateral crackles and an S3 gallop. On physical examination, the cardiac apex is palpated in left 6th intercostal space. Bilateral pitting edema is present, and the patient is in moderate distress. Which of the following is the best next step in the management of the patient?
- A. Intravenous beta blockers
- B. Intravenous diuretics (Correct Answer)
- C. Echocardiography
- D. Cardiac stress testing
- E. Intravenous inotropes
Cardiac complications Explanation: ***Intravenous diuretics***
- The patient presents with classic signs and symptoms of **acute decompensated heart failure**, such as progressive dyspnea, orthopnea, paroxysmal nocturnal dyspnea, bilateral crackles, S3 gallop, pitting edema, and elevated blood pressure with elevated heart rate due to fluid overload.
- **Intravenous loop diuretics** (e.g., furosemide) are the most appropriate initial therapy to reduce preload, alleviate pulmonary and systemic congestion, and improve oxygenation.
*Intravenous beta blockers*
- While beta-blockers are a cornerstone of chronic heart failure management, **starting or acutely increasing beta-blocker dosage in acute decompensated heart failure** can worsen cardiac output and lead to symptomatic hypotension or cardiogenic shock.
- Beta-blockers should generally be withheld or reduced during acute exacerbations and reinstituted once the patient is stable.
*Echocardiography*
- While an **echocardiogram** is essential for diagnosing the underlying cause and assessing cardiac function in heart failure, it is not the *best next step* in a patient presenting with acute, severe symptoms requiring immediate stabilization.
- The patient's acute respiratory distress and hypoxemia necessitate immediate medical intervention to reduce fluid overload before detailed diagnostic imaging.
*Cardiac stress testing*
- **Cardiac stress testing** is used to evaluate for inducible ischemia in stable patients and is not appropriate in the setting of acute decompensated heart failure.
- Performing a stress test on a patient with signs of fluid overload and respiratory distress would be dangerous and could exacerbate their condition.
*Intravenous inotropes*
- **Intravenous inotropes** (e.g., dobutamine, milrinone) are typically reserved for patients with evidence of **cardiogenic shock** or severe heart failure with persistent hypoperfusion despite optimal fluid management and diuretic therapy.
- This patient, while acutely ill, primarily exhibits signs of fluid overload without clear evidence of severe hypoperfusion compromising end-organ function.
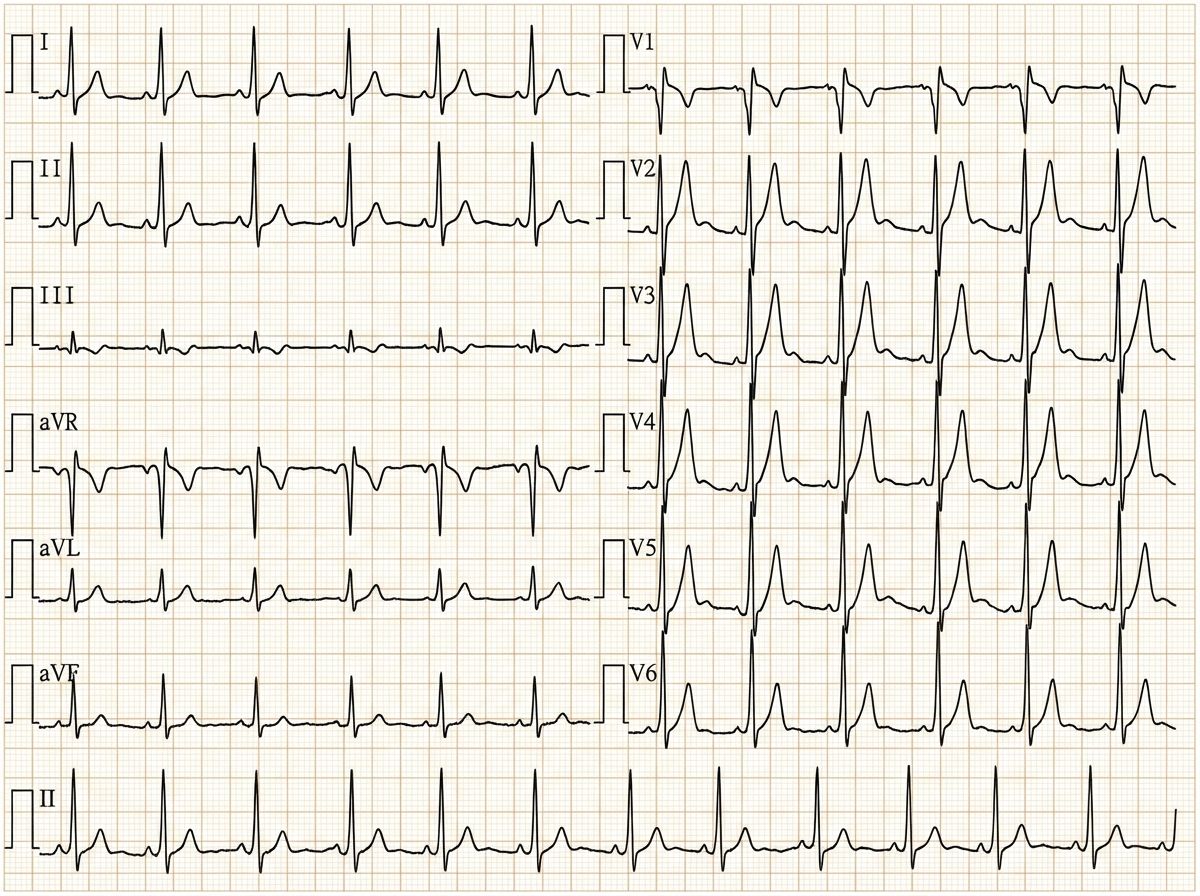
Cardiac complications US Medical PG Question 9: A 62-year-old woman presents to the emergency department complaining of fever, worsening fatigue, and muscle weakness for the previous 48 hours. The patient describes her muscle weakness as symmetric and worse in the upper limbs. Her past medical history is significant for long-standing diabetes type 2 complicated by stage 5 chronic kidney disease (CKD) on hemodialysis. She takes lisinopril, verapamil, metformin, and glargine. Today, the patient’s vital signs include: temperature 38.6°C (101.5°F), pulse 80/min, blood pressure 155/89 mm Hg, respirations 24/min, and 95% oxygen saturation on room air. The cardiac and pulmonary exams are unremarkable. The abdomen is soft and non-tender. Her strength is 3/5 in the upper extremities and 4/5 in the lower extremities and her sensation is intact. Deep tendon reflexes are absent in both the upper and lower limbs. A 12-lead electrocardiogram (ECG) is shown in the image below. Blood work is drawn and the patient is admitted and started on continuous cardiac monitoring. Based on the available information, what is the next best step in managing this patient?
- A. Order a stat serum potassium level
- B. Administer IV calcium gluconate (Correct Answer)
- C. Emergency dialysis
- D. Administer IV sodium bicarbonate
- E. Administer regular insulin and 50% dextrose in water
Cardiac complications Explanation: ***Administer IV calcium gluconate***
- The patient's presentation with **symmetrical muscle weakness** (worse in upper limbs), **absent deep tendon reflexes**, and characteristic ECG changes (peaked T waves, prolonged PR interval, wide QRS) in the context of **end-stage renal disease** and hemodialysis strongly suggests **severe hyperkalemia**.
- **Intravenous calcium gluconate** is the first-line treatment for clinically significant hyperkalemia with ECG changes, as it directly antagonizes the cardiac membrane effects of potassium and helps to stabilize the myocardium.
*Order a stat serum potassium level*
- While it is crucial to confirm hyperkalemia with a **stat serum potassium level**, the clinical picture (CKD, hemodialysis, muscle weakness, absent reflexes, and ECG changes) is emergent and highly suggestive of severe hyperkalemia.
- Waiting for laboratory confirmation before administering calcium gluconate can delay life-saving treatment and is not the "next best step" when ECG changes are evident.
*Emergency dialysis*
- **Emergency dialysis** is an effective way to remove potassium from the body and is often needed in severe hyperkalemia, especially in ESRD patients.
- However, **calcium gluconate** should be administered *immediately* to stabilize the cardiac membrane and prevent life-threatening arrhythmias, even before preparing for dialysis.
*Administer IV sodium bicarbonate*
- **Sodium bicarbonate** can shift potassium intracellularly, particularly in the setting of metabolic acidosis, but its effect is slower and less reliable than calcium in stabilizing cardiac membranes.
- It is often used as an adjunct but not as the initial, most critical intervention for immediate cardiac stabilization in severe hyperkalemia.
*Administer regular insulin and 50% dextrose in water*
- **Insulin and dextrose** shift potassium into cells, thereby lowering serum potassium levels. This is an important step in managing hyperkalemia.
- However, similar to sodium bicarbonate, its effect on serum potassium is not immediate enough to counteract the acute cardiotoxic effects, making **calcium gluconate** the priority for cardiac stabilization.
Cardiac complications US Medical PG Question 10: A 55-year-old man presents to his primary care physician for a wellness checkup. The patient has a past medical history of alcohol abuse and is currently attending alcoholics anonymous with little success. He is currently drinking roughly 1L of hard alcohol every day and does not take his disulfiram anymore. Which of the following findings is most likely to also be found in this patient?
- A. Dysdiadochokinesia (Correct Answer)
- B. Microcytic anemia
- C. Constipation
- D. Decreased CNS NMDA activity
- E. Increased transketolase activity
Cardiac complications Explanation: ***Dysdiadochokinesia***
- Chronic **alcohol abuse** can lead to cerebellar degeneration, a condition characterized by damage to the **cerebellum**.
- **Dysdiadochokinesia**, the impaired ability to perform rapidly alternating movements, is a classic sign of **cerebellar dysfunction**.
*Microcytic anemia*
- **Chronic alcohol abuse** typically causes **macrocytic anemia** due to folate deficiency, or less commonly, iron deficiency anemia from gastrointestinal bleeding.
- **Microcytic anemia** is usually associated with **iron deficiency** (often due to chronic blood loss) or **thalassemia**, neither of which are suggested here.
*Constipation*
- While various factors can cause constipation, **chronic alcohol abuse** is more commonly associated with **diarrhea** due to alterations in gut motility and malabsorption.
- Constipation is not a direct or prominent feature of **alcoholism**.
*Decreased CNS NMDA activity*
- **Chronic alcohol abuse** leads to an **upregulation of NMDA receptors** in the brain as a compensatory mechanism against alcohol's inhibitory effects on the central nervous system.
- When alcohol consumption ceases, this upregulated NMDA activity contributes to the **excitatory symptoms of alcohol withdrawal**, such as seizures and delirium tremens.
*Increased transketolase activity*
- **Transketolase activity** is usually **decreased** in chronic alcoholics due to **thiamine deficiency**, as thiamine (vitamin B1) is a critical cofactor for this enzyme.
- A **decrease** in transketolase activity is a key diagnostic indicator for thiamine deficiency, which contributes to conditions like **Wernicke-Korsakoff syndrome**.
More Cardiac complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.