Surgical complications

On this page
🚨 The Surgical Minefield: Navigating Post-Operative Perils
Every surgical incision opens not just tissue but a window of vulnerability where bleeding, infection, clots, and organ dysfunction lie in wait. You'll learn to anticipate these complications before they declare themselves, recognize the subtle signs that distinguish routine recovery from impending crisis, and decode overlapping symptoms when multiple systems fail simultaneously. Mastering this recognition matrix transforms you from observer to guardian, capable of intervening at the moment that separates reversible setback from irreversible harm.
📌 Remember: COMPLICATIONS - Cardiac, Organ failure, Metabolic, Pulmonary, Leak/bleeding, Infection, Clotting, Anastomotic, Thrombotic, Iatrogenic, Obstruction, Neurologic, Systemic inflammatory response
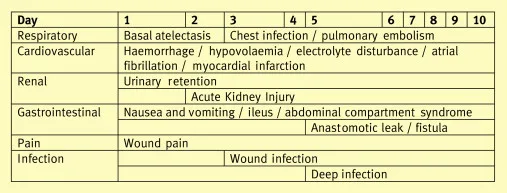
The spectrum of surgical complications follows predictable temporal patterns. Early complications (0-24 hours) include bleeding, cardiovascular instability, and immediate organ dysfunction. Intermediate complications (1-7 days) encompass infections, thromboembolism, and organ-specific failures. Late complications (>7 days) involve wound healing disorders, chronic pain syndromes, and long-term functional impairments.
| Complication Category | Timeline | Mortality Rate | Key Risk Factors | Primary Prevention |
|---|---|---|---|---|
| Hemorrhage | 0-6 hours | 2-8% | Coagulopathy, anticoagulants | Hemostasis protocols |
| Cardiac Events | 24-72 hours | 15-25% | CAD, age >70 | Beta-blockers, statins |
| Pulmonary Embolism | 3-7 days | 10-30% | Immobility, malignancy | VTE prophylaxis |
| Surgical Site Infection | 5-30 days | 1-3% | Diabetes, obesity | Antibiotic prophylaxis |
| Anastomotic Leak | 5-10 days | 20-50% | Poor perfusion, tension | Technical precision |
- Immediate Recognition Factors
- Hemodynamic instability: SBP <90 mmHg or >20% drop from baseline
- Respiratory compromise: SpO2 <92% or respiratory rate >24/min
- Neurological changes: GCS drop >2 points from baseline
- Metabolic derangements: Lactate >4 mmol/L or base deficit >-6
- Coagulation abnormalities: INR >1.5 or platelets <100,000
💡 Master This: Every complication follows the "Golden Hour" principle - early recognition within 60 minutes of onset reduces mortality by 50-70% across all complication categories.
The Clavien-Dindo Classification provides standardized severity grading: Grade I (no intervention), Grade II (pharmacological treatment), Grade III (surgical intervention), Grade IV (life-threatening), Grade V (death). This system enables objective comparison of surgical outcomes and guides quality improvement initiatives.
Understanding surgical complications transforms reactive crisis management into proactive prevention strategies, establishing the foundation for systematic complication recognition and evidence-based intervention protocols.
🚨 The Surgical Minefield: Navigating Post-Operative Perils
⚡ The Cascade Effect: When Systems Collide
📌 Remember: SHOCK progression - Systemic hypoperfusion, Hypotension, Organ dysfunction, Cellular hypoxia, Ketoacidosis/lactic acidosis
The "Three-Hit Hypothesis" explains complication development: First hit (surgical trauma), Second hit (inflammatory response), Third hit (secondary insults like infection or ischemia). Each hit amplifies the inflammatory cascade, with >3 hits associated with 60-80% mortality rates.
| System | Primary Mediators | Timeline | Clinical Markers | Intervention Window |
|---|---|---|---|---|
| Cardiovascular | TNF-α, IL-1β | 0-6 hours | ↓SVR, ↑HR, ↓MAP | <2 hours |
| Respiratory | IL-6, IL-8 | 6-24 hours | ↓PaO2/FiO2, ↑PEEP | <6 hours |
| Renal | Complement C3a/C5a | 12-48 hours | ↑Creatinine, ↓UOP | <12 hours |
| Hepatic | IL-10, TGF-β | 24-72 hours | ↑Bilirubin, ↓Albumin | <24 hours |
| Neurologic | Substance P | 48-96 hours | ↓GCS, delirium | <48 hours |
- Inflammatory Cascade Checkpoints
- Complement activation: C3a/C5a levels >300 ng/mL indicate severe SIRS
- Coagulation dysfunction: D-dimer >2000 ng/mL suggests DIC development
- Endothelial dysfunction: Protein C <40% predicts capillary leak syndrome
- Metabolic acidosis: Base excess <-8 mEq/L indicates cellular dysfunction
- Cytokine storm: IL-6 >1000 pg/mL correlates with organ failure risk
💡 Master This: The "Compensatory Anti-inflammatory Response Syndrome (CARS)" follows SIRS by 12-24 hours, creating immunosuppression that increases infection risk by 300-500% - explaining why patients survive initial trauma but succumb to secondary infections.
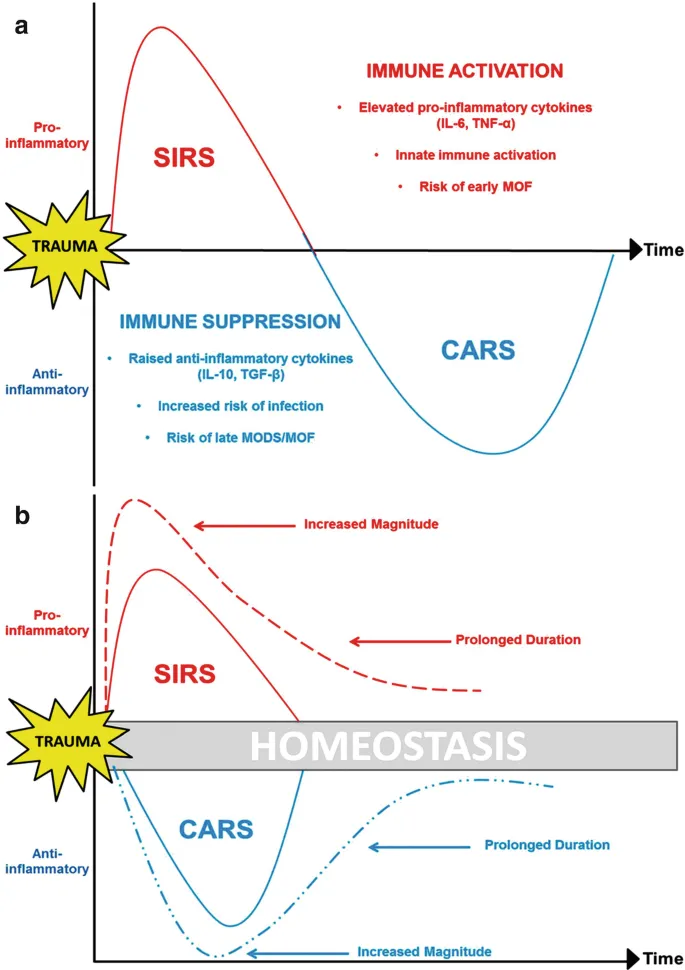
The Damage-Associated Molecular Patterns (DAMPs) released during surgery include HMGB1, heat shock proteins, and mitochondrial DNA, which activate Toll-like receptors and perpetuate inflammation. Understanding these molecular triggers enables targeted anti-inflammatory interventions during the "therapeutic window" of 6-12 hours post-surgery.
This cascade knowledge provides the mechanistic foundation for recognizing early warning signs and implementing targeted interventions before irreversible organ dysfunction develops.
⚡ The Cascade Effect: When Systems Collide
🎯 The Recognition Matrix: Spotting Trouble Before Crisis

📌 Remember: DETECT early warning signs - Deteriorating vitals, Elevated lactate, Tachycardia, Excessive bleeding, Changed mental status, Temperature instability
The Modified Early Warning Score (MEWS) provides systematic assessment using 6 physiological parameters: systolic BP, heart rate, respiratory rate, temperature, AVPU score, and urine output. Scores ≥5 require immediate physician evaluation, while scores ≥7 indicate critical illness requiring ICU consideration.
- Cardiovascular Warning Patterns
- Compensated shock: HR >100 bpm with normal BP (early sign)
- Decompensated shock: SBP <90 mmHg or >20% drop from baseline
- Cardiogenic patterns: ↑CVP, ↓CO, cool extremities, oliguria <0.5 mL/kg/hr
- Distributive patterns: ↓SVR, warm extremities, wide pulse pressure
- Hypovolemic patterns: ↓CVP, ↓PCWP, narrow pulse pressure, tachycardia
| Warning Sign | Normal Range | Mild Concern | Moderate Risk | Critical Alert |
|---|---|---|---|---|
| Heart Rate | 60-100 bpm | 101-110 bpm | 111-130 bpm | >130 bpm |
| Systolic BP | 110-140 mmHg | 100-109 mmHg | 90-99 mmHg | <90 mmHg |
| Respiratory Rate | 12-20/min | 21-24/min | 25-29/min | >30/min |
| Temperature | 36.1-37.2°C | 35.1-36°C | 38.1-39°C | <35°C or >39°C |
| Urine Output | >0.5 mL/kg/hr | 0.3-0.5 mL/kg/hr | 0.1-0.3 mL/kg/hr | <0.1 mL/kg/hr |
💡 Master This: The "Golden Triad" of surgical deterioration - tachycardia >110 bpm, oliguria <0.5 mL/kg/hr, and lactate >2.5 mmol/L - predicts major complications with 92% sensitivity when all three are present.
- Laboratory Pattern Recognition
- Infection patterns: WBC >12,000 or <4,000, bandemia >10%, procalcitonin >2 ng/mL
- Bleeding patterns: Hgb drop >2 g/dL, platelet count <100,000, INR >1.5
- Organ dysfunction: Creatinine ↑ >0.5 mg/dL, bilirubin >2 mg/dL, ALT >2x normal
- Metabolic stress: Glucose >180 mg/dL, albumin <3 g/dL, phosphorus <2.5 mg/dL
The "Rapid Response Team (RRT)" activation criteria include: systolic BP <90 mmHg, HR >130 bpm, RR >28/min, O2 sat <90%, acute mental status change, or staff concern. RRT activation reduces cardiac arrests by 50% and mortality by 15-20%.
This recognition framework transforms subjective clinical concern into objective, actionable assessment tools that enable proactive intervention before complications become irreversible.
🎯 The Recognition Matrix: Spotting Trouble Before Crisis
🔬 The Differential Decoder: Separating Signal from Noise
📌 Remember: VINDICATE differential framework - Vascular, Infectious, Neoplastic, Degenerative, Iatrogenic, Congenital, Autoimmune, Traumatic, Endocrine/metabolic
The "Rule of Threes" for surgical complications: 3 most common causes account for 80% of presentations, next 3 account for 15%, and remaining causes account for 5%. This distribution guides diagnostic workup prioritization and resource allocation.
| Clinical Presentation | Most Common (80%) | Moderately Common (15%) | Rare Causes (5%) | Key Discriminators |
|---|---|---|---|---|
| Postop Hypotension | Hypovolemia, bleeding, sepsis | Cardiogenic shock, PE, pneumothorax | Adrenal crisis, anaphylaxis, fat embolism | CVP, lactate, echo |
| Postop Fever | SSI, pneumonia, UTI | DVT/PE, drug fever, atelectasis | Malignant hyperthermia, thyroid storm | WBC, cultures, imaging |
| Postop Tachycardia | Pain, hypovolemia, fever | PE, MI, sepsis | Hyperthyroidism, withdrawal, fat embolism | ECG, D-dimer, echo |
| Postop Oliguria | Hypovolemia, hypotension, drugs | AKI, obstruction, sepsis | Rhabdomyolysis, HUS, cort |
🔬 The Differential Decoder: Separating Signal from Noise
Practice Questions: Surgical complications
Test your understanding with these related questions
A 52-year-old man comes to the physician because of a 3-week history of a cough and hoarseness. He reports that the cough is worse when he lies down after lunch. His temperature is 37.5°C (99.5°F); the remainder of his vital signs are within normal limits. Because the physician has recently been seeing several patients with the common cold, the diagnosis of a viral upper respiratory tract infection readily comes to mind. The physician fails to consider the diagnosis of gastroesophageal reflux disease, which the patient is later found to have. Which of the following most accurately describes the cognitive bias that the physician had?








