Preoperative patient education US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Preoperative patient education. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Preoperative patient education US Medical PG Question 1: A 56-year-old previously healthy woman with no other past medical history is post-operative day one from an open reduction and internal fixation of a fractured right radius and ulna after a motor vehicle accident. What is one of the primary ways of preventing postoperative pneumonia in this patient?
- A. Shallow breathing exercises
- B. Incentive spirometry (Correct Answer)
- C. Outpatient oral antibiotics
- D. Hyperbaric oxygenation
- E. In-hospital intravenous antibiotics
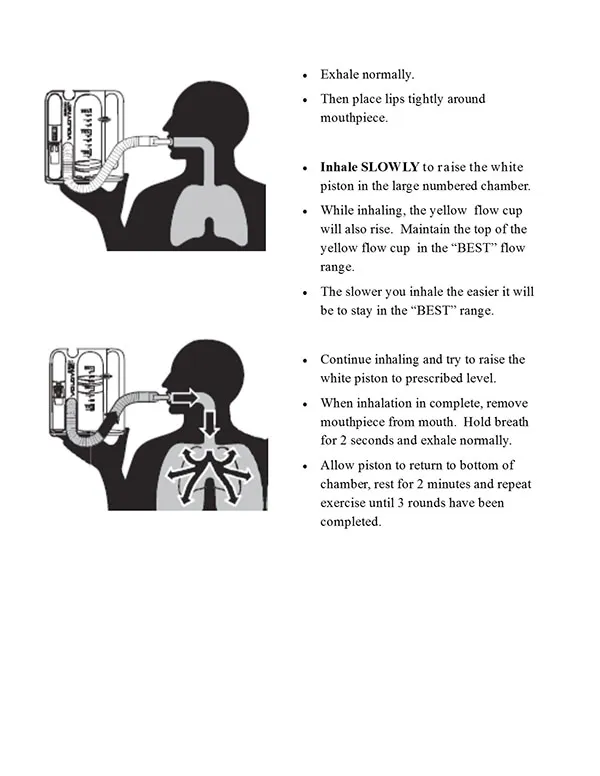
Preoperative patient education Explanation: ***Incentive spirometry***
- **Incentive spirometry** is a cornerstone of postoperative care, actively encouraging patients to take slow, deep breaths. This expands the lungs and prevents the collapse of alveoli, reducing the risk of **atelectasis** and subsequent **pneumonia**.
- Its effectiveness lies in promoting lung aeration and clearing secretions, which are crucial after anesthesia and surgery, especially in patients with reduced mobility or pain.
*Shallow breathing exercises*
- **Shallow breathing** is insufficient for adequate lung expansion and can actually contribute to **atelectasis** and the pooling of secretions in the lungs.
- Effective pulmonary hygiene requires **deep breaths** to maximize alveolar recruitment and prevent respiratory complications.
*Outpatient oral antibiotics*
- **Prophylactic antibiotics** are typically given around the time of surgery to prevent surgical site infections, not primarily to prevent postoperative pneumonia in an outpatient setting.
- Administering antibiotics without a diagnosed infection can lead to **antibiotic resistance** and is not a standard practice for preventing pneumonia unless a specific risk factor or existing infection is identified.
*Hyperbaric oxygenation*
- **Hyperbaric oxygenation** involves breathing 100% oxygen in a pressurized chamber and is used for conditions like **decompression sickness**, non-healing wounds, or severe infections.
- It is not a standard or primary method for preventing postoperative pneumonia, as its mechanism of action is unrelated to common pulmonary hygiene techniques.
*In-hospital intravenous antibiotics*
- While antibiotics can treat pneumonia, their routine, **prophylactic use** intravenously in-hospital solely for preventing postoperative pneumonia is generally unwarranted and can contribute to **antibiotic resistance**.
- Antibiotics are indicated if there is evidence of an active infection, but the primary prevention of pneumonia focuses on mechanical lung expansion and airway clearance.
Preoperative patient education US Medical PG Question 2: A 63-year-old woman is brought to the emergency department because of severe abdominal pain and vomiting for 3 hours. She had previous episodes of abdominal pain that lasted for 10–15 minutes and resolved with antacids. She lives with her daughter and grandchildren. She divorced her husband last year. She is alert and oriented. Her temperature is 37.3°C (99.1°F), pulse is 134/min, and blood pressure is 90/70 mm Hg. The abdomen is rigid and diffusely tender. Guarding and rebound tenderness are present. Rectal examination shows a collapsed rectum. Infusion of 0.9% saline is begun and a CT of the abdomen shows intestinal perforation. The surgeon discusses the need for emergent exploratory laparotomy with the patient and she agrees to it. Written informed consent is obtained. While in the holding area awaiting emergent transport to the operating room, she calls for the surgeon and informs him that she no longer wants the surgery. He explains the risks of not performing the surgery to her and she indicates she understands but is adamant about not proceeding with surgery. Which of the following is the most appropriate next step in management?
- A. Consult hospital ethics committee
- B. Obtain consent from the patient's daughter
- C. Obtain consent from the patient's ex-husband
- D. Continue with emergency life-saving surgery
- E. Cancel the surgery (Correct Answer)
Preoperative patient education Explanation: ***Cancel the surgery***
- The patient is **alert and oriented** and has indicated she understands the risks of refusing surgery, demonstrating **decision-making capacity**. An adult with intact capacity has the right to refuse medical treatment, even if it is life-saving.
- While the decision may seem medically unwise, **patient autonomy** is a fundamental ethical principle that must be respected once capacity is confirmed.
*Consult hospital ethics committee*
- An ethics committee consultation is typically reserved for situations where there is **uncertainty about a patient's capacity**, a conflict among healthcare providers, or a difficult ethical dilemma where principles of patient care are in clear conflict.
- In this case, the patient's capacity seems clear, and her refusal is unequivocal.
*Obtain consent from the patient's daughter*
- The patient's daughter cannot provide consent for her mother if the mother is **competent and able to make her own decisions**. **Surrogate decision-makers** are only legally authorized when the patient lacks capacity.
- The patient's expressed wishes directly override any potential preferences of her next-of-kin.
*Obtain consent from the patient's ex-husband*
- As the patient is divorced, her ex-husband has **no legal standing** to make medical decisions on her behalf.
- Even if they were still married, a spouse can only act as a surrogate if the patient lacks decision-making capacity.
*Continue with emergency life-saving surgery*
- Performing surgery against a **competent patient's explicit refusal** would be an act of **battery** and a violation of her **autonomy**.
- Even in life-threatening situations, a patient with capacity has the right to refuse treatment.
Preoperative patient education US Medical PG Question 3: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
Preoperative patient education Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
Preoperative patient education US Medical PG Question 4: A 65-year-old man presents to his primary care physician for a pre-operative evaluation. He is scheduled for cataract surgery in 3 weeks. His past medical history is notable for diabetes, hypertension, and severe osteoarthritis of the right knee. His medications include metformin, hydrochlorothiazide, lisinopril, and aspirin. His surgeon ordered blood work 1 month ago, which showed a hemoglobin of 14.2 g/dL, INR of 1.2, and a hemoglobin A1c of 6.9%. His vital signs at the time of the visit show BP: 130/70 mmHg, Pulse: 80, RR: 12, and T: 37.2 C. He has no current complaints and is eager for his surgery. Which of the following is the most appropriate course of action for this patient at this time?
- A. Tell the patient he will have to delay his surgery for at least 1 year
- B. Medically clear the patient for surgery (Correct Answer)
- C. Repeat the patient's CBC and coagulation studies
- D. Schedule the patient for a stress test and ask him to delay surgery for at least 6 months
- E. Perform an EKG
Preoperative patient education Explanation: **Medically clear the patient for surgery**
- The patient's **blood pressure is well-controlled** (130/70 mmHg), and his **hemoglobin A1c of 6.9%** indicates good glycemic control, both of which are favorable for elective surgery.
- He is currently on **aspirin**, which, for cataract surgery (a low-risk bleeding procedure), can generally be continued, and his **INR of 1.2 is within a safe range** for surgery.
*Tell the patient he will have to delay his surgery for at least 1 year*
- There are **no indications for such a prolonged delay** based on the provided clinical information.
- His chronic conditions (diabetes, hypertension) are **adequately managed**, and his lab values are acceptable.
*Repeat the patient's CBC and coagulation studies*
- The **existing blood work from 1 month ago is recent enough** for a pre-operative evaluation for cataract surgery, especially with no new symptoms.
- Repeating these tests without a clinical indication would be **unnecessary and inefficient**.
*Schedule the patient for a stress test and ask him to delay surgery for at least 6 months*
- The patient has **no active cardiac symptoms** (e.g., chest pain, shortness of breath), and his well-controlled hypertension does not automatically warrant a stress test for low-risk surgery.
- A stress test and a **6-month delay are not indicated** for a low-risk procedure like cataract surgery in an asymptomatic patient.
*Perform an EKG*
- While an EKG might be considered in some pre-operative evaluations for patients with cardiac risk factors, there are **no specific symptoms or significant new risk factors** presented that necessitate an EKG for this low-risk cataract surgery.
- Given his stable condition and controlled hypertension, an EKG is **not a mandatory part of medical clearance** for this procedure.
Preoperative patient education US Medical PG Question 5: A psychiatrist receives a call from a patient who expresses thoughts of harming his ex-girlfriend. The patient describes a detailed plan to attack her at her workplace. Which of the following represents the psychiatrist's most appropriate legal obligation?
- A. Warn the ex-girlfriend and notify law enforcement (Correct Answer)
- B. Only notify the patient's family
- C. Warn only law enforcement
- D. Maintain patient confidentiality
Preoperative patient education Explanation: ***Warn the ex-girlfriend and notify law enforcement***
- This scenario directly triggers the **"duty to warn"** and **"duty to protect"** principles, primarily stemming from the **Tarasoff v. Regents of the University of California** case.
- The psychiatrist has a legal obligation to take reasonable steps to protect the identifiable victim, which includes directly warning the intended victim and informing law enforcement.
*Only notify the patient's family*
- Notifying the patient's family alone does not fulfill the **legal obligation to protect** an identifiable third party from a serious threat of harm.
- While family involvement might be part of a comprehensive safety plan, it is insufficient as the sole action in this critical situation.
*Warn only law enforcement*
- While notifying law enforcement is a crucial step, the **Tarasoff duty** specifically mandates warning the **intended victim** directly (or those who can reasonably be expected to notify the victim).
- Relying solely on law enforcement might not ensure the immediate safety of the ex-girlfriend, especially if there's a delay in their response or ability to locate her.
*Maintain patient confidentiality*
- Patient confidentiality is a cornerstone of psychiatric practice, but it is **not absolute** when there is a serious and imminent threat of harm to an identifiable individual.
- The **duty to protect** a potential victim *outweighs* the duty to maintain confidentiality in such extreme circumstances.
Preoperative patient education US Medical PG Question 6: A 65-year-old man is admitted to the hospital because of a 1-month history of fatigue, intermittent fever, and weakness. Results from a peripheral blood smear taken during his evaluation are indicative of possible acute myeloid leukemia. Bone marrow aspiration and subsequent cytogenetic studies confirm the diagnosis. The physician sets aside an appointed time-slot and arranges a meeting in a quiet office to inform him about the diagnosis and discuss his options. He has been encouraged to bring someone along to the appointment if he wanted. He comes to your office at the appointed time with his daughter. He appears relaxed, with a full range of affect. Which of the following is the most appropriate opening statement in this situation?
- A. Your lab reports show that you have an acute myeloid leukemia
- B. What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies? (Correct Answer)
- C. You must be curious and maybe even anxious about the results of your tests.
- D. I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.
- E. Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?
Preoperative patient education Explanation: ***"What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies?"***
- This **open-ended question** allows the patient to express their current knowledge and perceptions, which helps the physician tailor the discussion.
- It establishes a **patient-centered approach**, respecting the patient's existing understanding and preparing them for further information.
*"You must be curious and maybe even anxious about the results of your tests."*
- While empathic, this statement makes an **assumption about the patient's feelings** rather than inviting them to share their own.
- It is often better to ask directly or use more open-ended questions that allow the patient to express their true emotions, especially given their **relaxed demeanor**.
*"I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.”"*
- This statement immediately introduces **overwhelming and potentially alarming information** (referral, chemotherapy, radiotherapy) without first establishing the diagnosis or assessing the patient's readiness to receive it.
- It prematurely jumps to treatment and logistics, potentially causing **unnecessary distress** before the patient has processed the core diagnosis.
*"Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?""*
- While it attempts to assess the patient's preference for information, this question is a **closed-ended "either/or" choice** that might limit the patient's ability to express nuanced needs.
- It also prematurely introduces the idea of "options" without first explaining the diagnosis in an understandable context.
*"Your lab reports show that you have an acute myeloid leukemia"*
- This is a **direct and blunt delivery of a serious diagnosis** without any preparatory context or assessment of the patient's existing knowledge or emotional state.
- Delivering such news abruptly can be shocking and overwhelming, potentially **hindering effective communication** and rapport building.
Preoperative patient education US Medical PG Question 7: A 32-year-old male asks his physician for information regarding a vasectomy. On further questioning, you learn that he and his wife have just had their second child and he asserts that they no longer wish to have additional pregnancies. You ask him if he has discussed a vasectomy with his wife to which he replies, "Well, not yet, but I'm sure she'll agree." What is the next appropriate step prior to scheduling the patient's vasectomy?
- A. Insist that the patient first discuss this procedure with his wife
- B. Telephone the patient's wife to inform her of the plan
- C. Refuse to perform the vasectomy
- D. Explain the risks and benefits of the procedure and request signed consent from the patient and his wife
- E. Explain the risks and benefits of the procedure and request signed consent from the patient (Correct Answer)
Preoperative patient education Explanation: ***Explain the risks and benefits of the procedure and request signed consent from the patient***
- A patient has the **right to make autonomous decisions** about their own medical care, including reproductive choices, regardless of their marital status or spousal approval.
- The physician's role is to ensure the patient is fully informed and provides **voluntary, uncoerced consent** after understanding the risks, benefits, and alternatives of the procedure.
*Insist that the patient first discuss this procedure with his wife*
- This option would be a **violation of patient autonomy** and confidentiality, as a married person has the right to make independent medical decisions.
- Requiring spousal consent for a procedure performed solely on one individual is not ethically or legally mandated and could be considered discriminatory.
*Telephone the patient's wife to inform her of the plan*
- This action would be a **breach of patient confidentiality**, as the patient's medical information, including his intent to have a vasectomy, cannot be shared with a third party, even a spouse, without explicit permission.
- Informing the wife without the husband's consent also undermines the patient's autonomy and right to privacy regarding his healthcare decisions.
*Refuse to perform the vasectomy*
- Refusing to perform the procedure simply because the patient has not discussed it with his wife would be **unethical and inconsistent with medical professionalism**, assuming the patient is competent and fully informed.
- A physician should not deny medically appropriate care based on a patient's marital dynamics or the presumed wishes of a spouse, as long as the patient's consent is valid.
*Explain the risks and benefits of the procedure and request signed consent from the patient and his wife*
- While it is advisable for a patient to discuss major life decisions with their spouse, requiring **spousal consent for a patient's own medical procedure** is not legally or ethically mandated for competent adults.
- Obtaining consent from both individuals is typically reserved for procedures affecting both parties directly or for those involving a surrogate decision-maker, not for an autonomous adult's personal medical choice.
Preoperative patient education US Medical PG Question 8: A 37-year-old man presents to his primary care physician because he has been experiencing episodes where he wakes up at night gasping for breath. His past medical history is significant for morbid obesity as well as hypertension for which he takes lisinopril. He is diagnosed with sleep apnea and prescribed a continuous positive airway pressure apparatus. In addition, the physician discusses making lifestyle and behavioral changes such as dietary modifications and exercise. The patient agrees to attempt these behavioral changes. Which of the following is most likely to result in improving patient adherence to this plan?
- A. Refer the patient to a peer support group addressing lifestyle changes
- B. Ask the patient to bring a family member to next appointment
- C. Provide follow-up appointments to assess progress in attaining goals (Correct Answer)
- D. Provide appropriate publications for the patient's educational level
- E. Inform the patient of the health consequences of not intervening
Preoperative patient education Explanation: ***Provide follow-up appointments to assess progress in attaining goals***
- **Regular follow-up appointments** provide accountability and opportunities to discuss progress, troubleshoot challenges, and reinforce motivation for lifestyle changes
- This approach fosters a **patient-centered relationship** where the physician actively participates in the patient's journey, increasing adherence
- Evidence supports that scheduled follow-up is one of the most effective interventions for improving adherence to chronic disease management plans
*Refer the patient to a peer support group addressing lifestyle changes*
- While peer support can be beneficial for some patients, it is **not universally effective** and might not be suitable for all patients, especially as a primary strategy for adherence
- The effectiveness of such groups varies widely based on the patient's personality and group dynamics, potentially leading to **inconsistent adherence**
*Ask the patient to bring a family member to next appointment*
- Involving family can be supportive, but it may not always be appropriate or desired by the patient and doesn't directly address the patient's individual motivation or challenges
- While family support can enhance adherence, this approach is supplementary rather than primary in effectiveness
*Provide appropriate publications for the patient's educational level*
- Providing educational materials is a good initial step, but information alone is often **insufficient to sustain long-term behavioral changes**
- Without active follow-up and personalized guidance, written materials can be easily forgotten or not fully implemented into daily life
*Inform the patient of the health consequences of not intervening*
- While explaining risks is crucial for informed consent and awareness, relying solely on **fear-based motivation** often has limited long-term effectiveness in promoting sustained behavioral change
- Patients are often aware of potential negative consequences, but this knowledge alone does not provide the practical support or strategies needed for adherence
Preoperative patient education US Medical PG Question 9: An 8-year-old boy and his 26-year-old babysitter are brought into the emergency department with severe injuries caused by a motor vehicle accident. The child is wheeled to the pediatric intensive care unit with a severe injury to his right arm, as well as other external and internal injuries. He is hemorrhaging and found to be hemodynamically unstable. He subsequently requires transfusion and surgery, and he is currently unconscious. The pediatric trauma surgeon evaluates the child’s arm and realizes it will need to be amputated at the elbow. Which of the following is the most appropriate course of action to take with regards to the amputation?
- A. Obtain an emergency court order from a judge to obtain consent to amputate the child’s arm
- B. Find the child’s parents to obtain consent to amputate the child’s arm
- C. Amputate the child’s arm at the elbow joint (Correct Answer)
- D. Wait for the child’s babysitter to recover from her injuries to obtain her consent to amputate the child’s arm
- E. Wait for the child to gain consciousness to obtain his consent to amputate his arm
Preoperative patient education Explanation: ***Amputate the child’s arm at the elbow joint***
- In an emergency situation where a child's life is at risk and a procedure is immediately necessary to save their life or prevent significant harm, **implied consent** allows for medical intervention without explicit parental consent. The child's **hemodynamic instability** and **severe hemorrhage** indicate an immediate threat to life.
- The decision to amputate to save the child's life is a **medically necessary emergency intervention**. Waiting for consent would cause a dangerous delay.
*Obtain an emergency court order from a judge to obtain consent to amputate the child’s arm*
- While court orders can be used in cases of parental refusal or unavailability for non-emergency procedures, the **urgent nature** of this life-threatening situation precludes waiting for a court order.
- The delay in obtaining a court order could significantly worsen the child's prognosis or lead to death.
*Find the child’s parents to obtain consent to amputate the child’s arm*
- Although parental consent is generally required for minors, the child's **critical condition** and **hemodynamic instability** mean delaying life-saving treatment to locate parents would be medically irresponsible.
- The principle of **beneficence** (acting in the best interest of the patient) and avoiding harm takes precedence in this emergency.
*Wait for the child’s babysitter to recover from her injuries to obtain her consent to amputate the child’s arm*
- A babysitter is generally not legally authorized to provide consent for major medical procedures for a child, especially an amputation.
- Even if the babysitter had some form of temporary custody, her own injury makes her an unreliable source of consent, and the delay would be critical.
*Wait for the child to gain consciousness to obtain his consent to amputate his arm*
- An 8-year-old child is generally not considered mature enough to provide **informed consent** for such a major medical decision.
- The child is **unconscious and hemodynamically unstable**, making it impossible to obtain consent and dangerously delaying a life-saving procedure.
Preoperative patient education US Medical PG Question 10: A 66-year-old man with severe aortic stenosis (valve area 0.7 cm², mean gradient 55 mmHg) and Class III heart failure requires emergent hemicolectomy for perforated diverticulitis with peritonitis. He is hemodynamically stable on pressors. Cardiology states he is high-risk for valve replacement but could undergo TAVR in 2-3 weeks. The surgeon believes he needs surgery within 6-8 hours. Evaluate the management approach.
- A. Delay surgery, perform urgent TAVR, then colectomy in 2-3 weeks
- B. Proceed with colectomy under invasive monitoring with cardiology backup (Correct Answer)
- C. Perform colostomy only under local anesthesia, defer resection
- D. Medical management of perforation with antibiotics pending TAVR
- E. Simultaneous TAVR and emergency colectomy in hybrid OR
Preoperative patient education Explanation: ***Proceed with colectomy under invasive monitoring with cardiology backup***
- Perforated diverticulitis with **peritonitis** is an immediate surgical emergency requiring intervention within hours to prevent **sepsis** and death.
- Management of **severe aortic stenosis** in non-cardiac emergencies involves **invasive hemodynamic monitoring** to maintain a fixed cardiac output, adequate **preload**, and stable **systemic vascular resistance**.
*Delay surgery, perform urgent TAVR, then colectomy in 2-3 weeks*
- Waiting 2-3 weeks for a **TAVR** is not feasible for a patient with **peritonitis**, as the risk of mortality from untreated perforation is nearly 100%.
- **TAVR** requires a recovery period and often **antiplatelet therapy**, which would further complicate and delay the necessary abdominal surgery.
*Perform colostomy only under local anesthesia, defer resection*
- **Local anesthesia** is insufficient for managing generalized **peritonitis** and would not allow for the necessary thorough abdominal washout and source control.
- A simple colostomy without **resection** of the perforated segment fails to eliminate the source of **fecal contamination**, leading to persistent sepsis.
*Medical management of perforation with antibiotics pending TAVR*
- Antibiotics alone are inadequate for **Hinchey III/IV peritonitis**; the lack of **source control** results in high mortality regardless of cardiac status.
- The patient is already on **pressors**, indicating that the septic process is advanced and requires mechanical/surgical correction rather than conservative medical therapy.
*Simultaneous TAVR and emergency colectomy in hybrid OR*
- Combining a **clean-contaminated** or dirty surgery (colectomy) with a sterile cardiac procedure (TAVR) carries an unacceptable risk of **prosthetic valve infection**.
- The physiological stress of both procedures simultaneously would likely exceed the patient's **hemodynamic compensatory** mechanisms in the setting of acute sepsis.
More Preoperative patient education US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.