Preoperative imaging selection US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Preoperative imaging selection. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
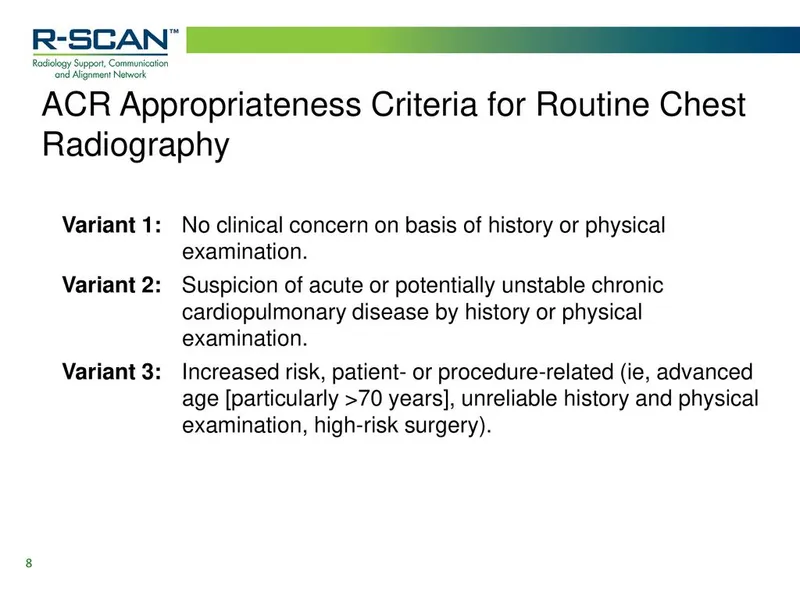
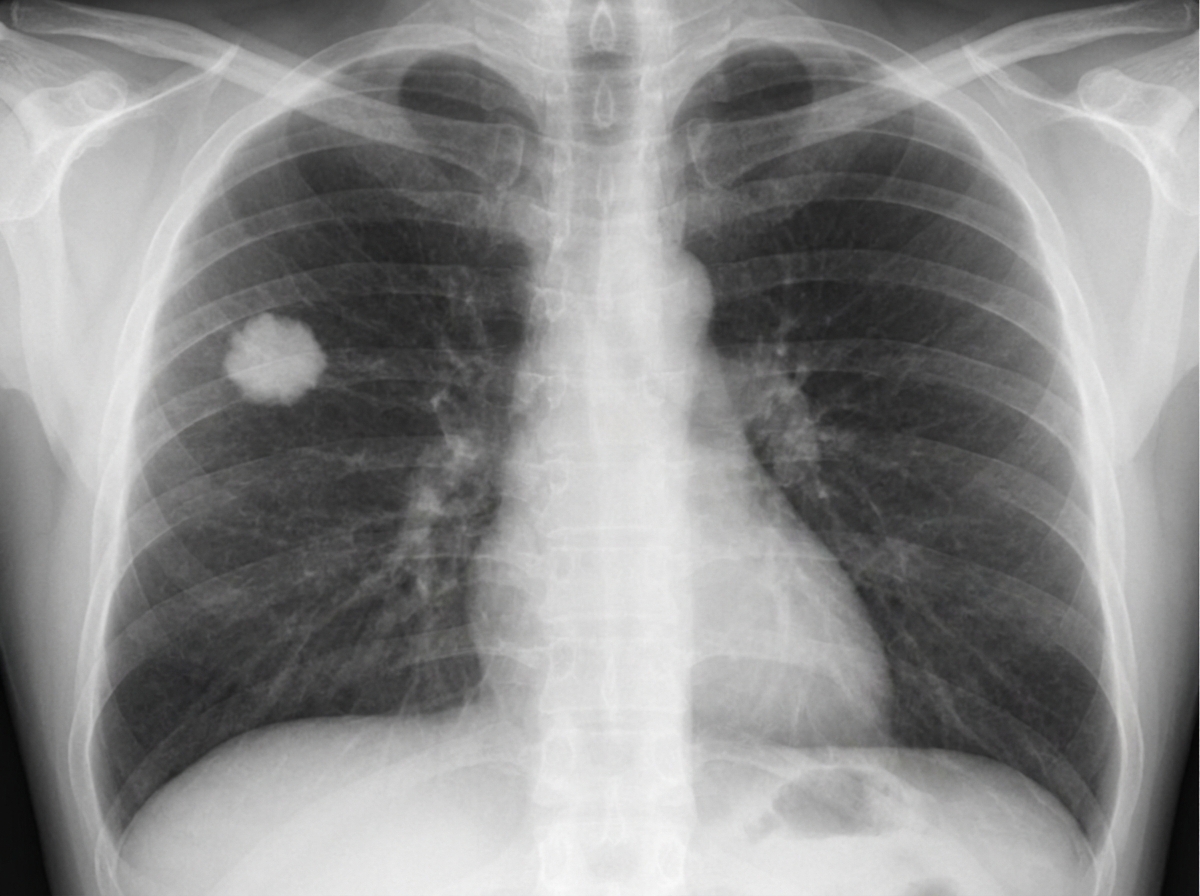
Preoperative imaging selection US Medical PG Question 1: A 60-year-old man comes to the physician for an examination prior to a scheduled cholecystectomy. He has hypertension treated with hydrochlorothiazide. His mother had chronic granulomatous disease of the lung. He works in a glass manufacturing plant. He has smoked two packs of cigarettes daily for 38 years. His vital signs are within normal limits. Examination shows no abnormalities. Laboratory studies are within the reference range. An x-ray of the chest is shown. Which of the following is the most appropriate next step in management?
- A. Perform diffusion capacity of the lung for carbon monoxide
- B. Perform arterial blood gas analysis
- C. Request previous chest x-ray (Correct Answer)
- D. Perform CT-guided biopsy
- E. Measure angiotensin-converting enzyme
Preoperative imaging selection Explanation: ***Request previous chest x-ray***
- Comparing the current chest X-ray with previous ones is crucial to determine if the findings are **new or chronic**, which significantly impacts further management.
- Given the patient's age, smoking history, and occupational exposure, a nodule or infiltrates could be present for a long time without causing symptoms, and a **stable finding** would alleviate immediate concern.
*Perform diffusion capacity of the lung for carbon monoxide*
- **DLCO** measures the lung's ability to transfer gas from inhaled air to the bloodstream and is primarily used to assess **interstitial lung disease** or emphysema.
- While the patient has risk factors for lung disease (smoking, occupational exposure), without a specific indication of interstitial lung disease or significant respiratory symptoms, it is not the most immediate next step, especially before understanding the chronicity of any X-ray findings.
*Perform arterial blood gas analysis*
- **ABG analysis** assesses oxygenation, ventilation, and acid-base balance, typically performed in patients with acute respiratory distress, significant dyspnea, or to monitor severe lung pathology.
- The patient is **asymptomatic** with normal vital signs, and there is no indication that his gas exchange is compromised, making ABG analysis premature.
*Perform CT-guided biopsy*
- A **CT-guided biopsy** is an invasive procedure used to obtain tissue for histological diagnosis, typically reserved when a lesion is highly suspicious for malignancy or infection and non-invasive methods are insufficient.
- It is an aggressive initial step without first characterizing the X-ray findings further or determining if the lesion is new or chronic.
*Measure angiotensin-converting enzyme*
- **ACE levels** are primarily used in the diagnosis and monitoring of **sarcoidosis**, a granulomatous disease.
- While the patient's mother had "chronic granulomatous disease of the lung," implying a possible genetic link or predisposition to granulomatous conditions, there are no specific findings on the history or presentation to directly suggest sarcoidosis, and it would be a secondary investigation after initial X-ray comparison.
Preoperative imaging selection US Medical PG Question 2: A 41-year-old man is admitted to the emergency room after being struck in the abdomen by a large cement plate while transporting it. On initial assessment by paramedics at the scene, his blood pressure was 110/80 mm Hg, heart rate 85/min, with no signs of respiratory distress. On admission, the patient is alert but in distress. He complains of severe, diffuse, abdominal pain and severe weakness. Vital signs are now: blood pressure 90/50 mm Hg, heart rate 96/min, respiratory rate 19/min, temperature 37.4℃ (99.3℉), and oxygen saturation of 95% on room air. His lungs are clear on auscultation. The cardiac exam is significant for a narrow pulse pressure. Abdominal examination reveals a large bruise over the epigastric and periumbilical regions. The abdomen is distended and there is diffuse tenderness to palpation with rebound and guarding, worst in the epigastric region. There is hyperresonance to percussion in the epigastric region and absence of hepatic dullness in the right upper quadrant. Aspiration of the nasogastric tube reveals bloody contents. Focused assessment with sonography for trauma (FAST) shows free fluid in the pelvic region. Evaluation of the perisplenic and perihepatic regions is impossible due to the presence of free air. Aggressive intravenous fluid resuscitation is administered but fails to improve upon the patient’s hemodynamics. Which of the following is the next best step in management?
- A. Emergency laparoscopy
- B. Abdominal ultrasound
- C. Diagnostic peritoneal lavage (DPL)
- D. Emergency laparotomy (Correct Answer)
- E. CT scan
Preoperative imaging selection Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** unresponsive to fluid resuscitation, coupled with clear signs of **perforation** (hyperresonance, absent hepatic dullness, free air on FAST limited view). This clinical picture is a direct indication for immediate surgical intervention.
- The presence of bloody nasogastric tube contents, diffuse tenderness with rebound and guarding, and a history of significant blunt trauma further support the need for urgent exploratory **laparotomy** to identify and repair the source of injury.
*Emergency laparoscopy*
- While laparoscopy can be used for abdominal exploration, it is **contraindicated in hemodynamically unstable patients** due to the need for pneumoperitoneum, which can further compromise cardiovascular stability.
- In cases of suspected visceral perforation with extensive free air and massive bleeding, **laparoscopy may be technically challenging** and less efficient than open laparotomy for rapid control of hemorrhage and contamination.
*Abdominal ultrasound*
- An abdominal ultrasound (**FAST exam**) has already been partially performed, revealing free fluid and raising suspicion of free air, making further ultrasound redundant.
- While useful for initial trauma assessment, an ultrasound **cannot definitively rule out all abdominal injuries**, especially hollow viscus perforations or retroperitoneal hematomas, and is insufficient for unstable patients with clear signs of peritonitis.
*Diagnostic peritoneal lavage (DPL)*
- **DPL is largely replaced by FAST and CT scans** in most trauma centers, especially given the availability of imaging.
- Although it can detect intraperitoneal bleeding or perforation, it is an **invasive procedure** with potential complications and would only confirm what is already strongly suspected clinically; it does not address the need for immediate therapeutic intervention in an unstable patient.
*CT scan*
- A CT scan would be the imaging modality of choice for a **hemodynamically stable** patient with blunt abdominal trauma.
- However, performing a CT scan on an **unstable patient** would unnecessarily delay definitive surgical management, which is critical given the signs of ongoing internal bleeding and likely perforation.
Preoperative imaging selection US Medical PG Question 3: A 37-year-old woman presents to the Emergency Department after 8 hours of left sided flank pain that radiates to her groin and pelvic pain while urinating. Her medical history is relevant for multiple episodes of urinary tract infections, some requiring hospitalization, and intravenous antibiotics. In the hospital, her blood pressure is 125/83 mm Hg, pulse of 88/min, a respiratory rate of 28/min, and a body temperature of 36.5°C (97.7°F). On physical examination, she has left costovertebral tenderness and lower abdominal pain. Laboratory studies include a negative pregnancy test, mild azotemia, and a urinary dipstick that is positive for blood. Which of the following initial tests would be most useful in the diagnosis of this case?
- A. Urine osmolality
- B. Fractional excretion of sodium (FeNa+)
- C. Renal ultrasonography (Correct Answer)
- D. Contrast abdominal computed tomography
- E. Blood urea nitrogen (BUN): serum creatinine (SCr) ratio
Preoperative imaging selection Explanation: ***Renal ultrasonography***
- This is the most appropriate initial imaging test to evaluate for **kidney stones** (given the flank pain radiating to groin and hematuria) and **hydronephrosis** (which can indicate obstruction) and assess for signs of **pyelonephritis** (given the history of recurrent UTIs and CVA tenderness).
- It is **non-invasive**, readily available, and avoids radiation exposure, making it suitable as a first-line diagnostic tool in this setting.
*Urine osmolality*
- This test primarily assesses the kidney's ability to **concentrate urine**, which is more relevant for evaluating fluid balance, diabetes insipidus, or other renal tubular disorders.
- It would not directly diagnose the cause of acute flank pain or urinary tract obstruction.
*Fractional excretion of sodium (FeNa+)*
- FeNa+ is used to differentiate between **prerenal azotemia** and **acute tubular necrosis**, indicating the kidney's response to hypoperfusion.
- While the patient has mild azotemia, FeNa+ would not identify the underlying cause of the flank pain, hematuria, or potential obstruction.
*Contrast abdominal computed tomography*
- While highly sensitive for diagnosing kidney stones and other renal pathologies, **contrast CT** exposes the patient to **ionizing radiation** and risks associated with contrast agents (e.g., contrast-induced nephropathy), especially with pre-existing azotemia.
- It is often reserved for cases where ultrasound is inconclusive or more detailed anatomical information is needed.
*Blood urea nitrogen (BUN): serum creatinine (SCr) ratio*
- This ratio is primarily used to differentiate between **prerenal** causes of acute kidney injury (high ratio, e.g., >20:1) and **intrinsic renal** causes (lower ratio, e.g., <15:1).
- While it can provide insight into the etiology of azotemia, it does not directly identify the cause of the patient's acute flank pain or potential urinary tract obstruction.
Preoperative imaging selection US Medical PG Question 4: A 45-year-old man presents for a follow-up visit as part of his immigration requirements into the United States. Earlier this week, he was administered the Mantoux tuberculin skin test (TST). Today’s reading, 3 days after being administered the test, he shows an induration of 10 mm. Given his recent immigration from a country with a high prevalence of tuberculosis, he is requested to obtain a radiograph of the chest, which is shown in the image. Which of the following is true regarding this patient’s chest radiograph (CXR)?
- A. Posterior ribs 9 and 10 are visible only in an expiratory film.
- B. The right lower boundary of the mediastinal silhouette belongs to the right ventricle.
- C. If the spinous process is not in-between the two clavicular heads, the image is repeated. (Correct Answer)
- D. The film is taken in a supine position.
- E. The view is anteroposterior (AP).
Preoperative imaging selection Explanation: ***If the spinous process is not in-between the two clavicular heads, the image is repeated.***
- Proper patient positioning is crucial for an accurate chest X-ray; **rotation of the patient** can distort the appearance of the heart and lungs, simulating pathology or obscuring real findings.
- Symmetrical positioning, indicated by the **spinous process being equidistant from the medial ends of the clavicles**, ensures an ideal posteroanterior (PA) view for interpretation.
*Posterior ribs 9 and 10 are visible only in an expiratory film.*
- In a properly **inspired chest X-ray**, at least 9 or 10 posterior ribs (or 5-6 anterior ribs) should be visible above the diaphragm.
- If fewer ribs are visible on a standard PA film, it indicates a **poor inspiratory effort**, which can compress lung fields and mimic pathology.
*The right lower boundary of the mediastinal silhouette belongs to the right ventricle.*
- The **right lower boundary of the mediastinal silhouette** is formed by the right atrium, not the right ventricle.
- The right ventricle forms part of the **anterior cardiac border** and is typically not seen as a distinct border on a standard PA chest X-ray.
*The film is taken in a supine position.*
- The presence of the **gastric bubble visible below the left hemidiaphragm** confirms an upright position, as gas rises in the stomach.
- A supine film would typically result in a **magnified cardiac silhouette** and less prominent gastric air.
*The view is anteroposterior (AP).*
- In an AP view, the **medial ends of the clavicles overlay the lung apices**, and the scapulae are often within the lung fields; this image shows the scapulae largely clear of the lung fields, consistent with a PA view.
- AP films also tend to **magnify the heart shadow** due to the divergent X-ray beam, which is not evident here.
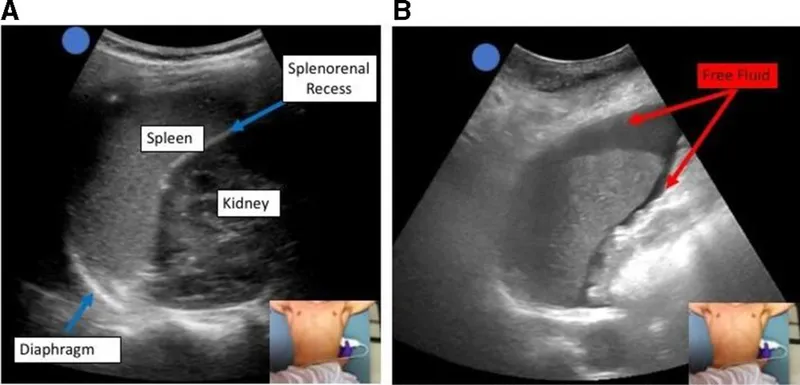
Preoperative imaging selection US Medical PG Question 5: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Preoperative imaging selection Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
Preoperative imaging selection US Medical PG Question 6: A 24-year-old woman presents to the emergency department for evaluation of lower abdominal pain. She endorses 6 hours of progressively worsening pain. She denies any significant past medical history and her physical examination is positive for non-specific, diffuse pelvic discomfort. She denies the possibility of pregnancy given her consistent use of condoms with her partner. The vital signs are: blood pressure, 111/68 mm Hg; pulse, 71/min; and respiratory rate, 15/min. She is afebrile. Which of the following is the next best step in her management?
- A. Surgical consultation
- B. Admission and observation
- C. Obtain a pelvic ultrasound
- D. Serum hCG (Correct Answer)
- E. Abdominal CT scan
Preoperative imaging selection Explanation: ***Serum hCG***
- Despite the patient's claim of consistent condom use, **pregnancy must be ruled out** in any woman of reproductive age presenting with lower abdominal pain. **Ectopic pregnancy** is a life-threatening condition that can present this way.
- A **serum hCG** is more sensitive than a urine test and can detect very early pregnancies, which is crucial for prompt diagnosis and management.
*Surgical consultation*
- Surgical consultation would be premature without a definitive diagnosis or clear signs of an acute surgical abdomen, such as peritonitis or hemodynamic instability.
- Initial diagnostic steps are necessary to identify the cause of the pain before considering surgical intervention.
*Admission and observation*
- While observation might be necessary, it's not the immediate next best step. Without a diagnosis, observation alone may delay critical interventions for conditions like ectopic pregnancy.
- Admission for observation typically follows initial diagnostic workup when the diagnosis is uncertain but not immediately life-threatening.
*Obtain a pelvic ultrasound*
- A pelvic ultrasound is an important diagnostic tool for evaluating pelvic pain, but it should be performed only **after pregnancy has been ruled out** or confirmed.
- If the patient is pregnant, a pelvic ultrasound would be used to assess for intrauterine or ectopic pregnancy. If she is not pregnant, the ultrasound would help identify other gynecological causes of pain.
*Abdominal CT scan*
- An abdominal CT scan is less specific for gynecological causes of pain and exposes the patient to **ionizing radiation**, making it a less ideal initial step compared to ruling out pregnancy.
- It might be considered if the initial workup for gynecological causes is negative or if there are concerns for other intra-abdominal pathology.
Preoperative imaging selection US Medical PG Question 7: A 32-year-old man is brought to the emergency department after a skiing accident. The patient had been skiing down the mountain when he collided with another skier who had stopped suddenly in front of him. He is alert but complaining of pain in his chest and abdomen. He has a past medical history of intravenous drug use and peptic ulcer disease. He is a current smoker. His temperature is 97.4°F (36.3°C), blood pressure is 77/53 mmHg, pulse is 127/min, and respirations are 13/min. He has a GCS of 15 and bilateral shallow breath sounds. His abdomen is soft and distended with bruising over the epigastrium. He is moving all four extremities and has scattered lacerations on his face. His skin is cool and delayed capillary refill is present. Two large-bore IVs are placed in his antecubital fossa, and he is given 2L of normal saline. His FAST exam reveals fluid in Morison's pouch. Following the 2L normal saline, his temperature is 97.5°F (36.4°C), blood pressure is 97/62 mmHg, pulse is 115/min, and respirations are 12/min.
Which of the following is the best next step in management?
- A. Diagnostic peritoneal lavage
- B. Emergency laparotomy (Correct Answer)
- C. Upper gastrointestinal endoscopy
- D. Close observation
- E. Diagnostic laparoscopy
Preoperative imaging selection Explanation: ***Emergency laparotomy***
- The patient remains **hemodynamically unstable** (BP 97/62 mmHg, HR 115/min after 2L IV fluids) with evidence of **intra-abdominal fluid on FAST exam** (fluid in Morison's pouch).
- This clinical picture indicates active intra-abdominal hemorrhage requiring **immediate surgical intervention** to identify and control the source of bleeding.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has largely been replaced by the focused abdominal sonography for trauma (FAST) exam and CT scans.
- While it can detect intra-abdominal bleeding, it is **invasive** and would delay definitive treatment in a hemodynamically unstable patient with positive FAST.
*Upper gastrointestinal endoscopy*
- This procedure is primarily for diagnosing and treating **upper gastrointestinal bleeding** or mucosal abnormalities.
- It is **not indicated** for evaluating traumatic intra-abdominal hemorrhage or hemodynamic instability following blunt abdominal trauma.
*Close observation*
- Close observation is appropriate for **hemodynamically stable patients** with blunt abdominal trauma and minor injuries or equivocal findings.
- This patient's persistent hypotension, tachycardia, and positive FAST findings rule out observation as a safe or appropriate next step.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a minimally invasive surgical procedure used to evaluate the abdominal cavity.
- While it can be diagnostic, it is generally **contraindicated in hemodynamically unstable patients** as it can prolong the time to definitive hemorrhage control if a major injury is found.
Preoperative imaging selection US Medical PG Question 8: A 43-year-old man presents with acute-onset left flank pain for the past 6 hours. He describes the pain as severe, intermittent, colicky, and “coming in waves”, and he points to the area of the left costovertebral angle (CVA). He says he recently has been restricting oral liquid intake to only 2 glasses of water per day based on the advice of his healer. He also reports nausea and vomiting. The patient has a history of hypertension, gout, and type 2 diabetes mellitus. He is afebrile, and his vital signs are within normal limits. On physical examination, he is writhing in pain and moaning. There is exquisite left CVA tenderness. A urinalysis shows gross hematuria. Which of the following is the next best step in the management of this patient?
- A. Non-contrast CT of the abdomen
- B. Contrast CT of the abdomen and pelvis
- C. Supine abdominal radiograph
- D. Renal ultrasound
- E. Non-contrast CT of the abdomen and pelvis (Correct Answer)
Preoperative imaging selection Explanation: **Non-contrast CT of the abdomen and pelvis**
- **Non-contrast CT of the abdomen and pelvis** is the gold standard for diagnosing urolithiasis, providing high sensitivity and specificity for detecting stones, identifying their size and location, and assessing for hydronephrosis.
- The patient's presentation with **acute-onset, severe, colicky flank pain**, nausea, vomiting, gross hematuria, and CVA tenderness is highly suggestive of **renal colic due to a kidney stone**.
*Non-contrast CT of the abdomen*
- This option is **insufficient** as kidney stones can be located in the ureters within the pelvis; a scan of the abdomen alone might miss stones in the distal ureter.
- While a non-contrast CT is appropriate, the scope of only the abdomen is **incomplete** for evaluating the entire urinary tract that might be affected by stones.
*Contrast CT of the abdomen and pelvis*
- **Contrast-enhanced CT is generally not indicated** for the initial evaluation of suspected renal colic due to urolithiasis because it can obscure the visualization of urinary stones.
- The use of contrast also carries risks such as **allergic reaction** and **contrast-induced nephropathy**, which are unnecessary in this acute, non-complicated setting.
*Supine abdominal radiograph*
- A supine abdominal radiograph (KUB) has **limited sensitivity** for detecting kidney stones, especially radiolucent stones (e.g., uric acid stones) or small stones.
- It also provides **poor anatomical detail** and cannot assess for hydronephrosis or other complications as effectively as CT.
*Renal ultrasound*
- Renal ultrasound can detect **hydronephrosis** and some kidney stones but is less sensitive than CT for visualizing smaller stones, especially in the ureters.
- Its diagnostic utility can be **limited by body habitus** and operator dependence, making it less reliable as a primary diagnostic tool for acute renal colic.
Preoperative imaging selection US Medical PG Question 9: A 69-year-old man is scheduled to undergo radical retropubic prostatectomy for prostate cancer in 2 weeks. He had a myocardial infarction at the age of 54 years. He has a history of GERD, unstable angina, hyperlipidemia, and severe osteoarthritis in the left hip. He is unable to climb up stairs or walk fast because of pain in his left hip. He had smoked one pack of cigarettes daily for 30 years but quit 25 years ago. He drinks one glass of wine daily. Current medications include aspirin, metoprolol, lisinopril, rosuvastatin, omeprazole, and ibuprofen as needed. His temperature is 36.4°C (97.5°F), pulse is 90/min, and blood pressure is 136/88 mm Hg. Physical examination shows no abnormalities. A 12-lead ECG shows Q waves and inverted T waves in leads II, III, and aVF. His B-type natriuretic protein is 84 pg/mL (N < 125). Which of the following is the most appropriate next step in management to assess this patient's perioperative cardiac risk?
- A. No further testing
- B. 24-hour ambulatory ECG monitoring
- C. Radionuclide myocardial perfusion imaging (Correct Answer)
- D. Treadmill stress test
- E. Resting echocardiography
Preoperative imaging selection Explanation: ***Radionuclide myocardial perfusion imaging***
- This patient requires **perioperative cardiac risk assessment** before intermediate-risk surgery (radical prostatectomy).
- Key factors include: history of **myocardial infarction**, current cardiac risk factors, and **inability to exercise** due to severe osteoarthritis.
- Since he cannot perform exercise stress testing, **pharmacologic stress testing** with radionuclide myocardial perfusion imaging (using agents like adenosine, dipyridamole, or regadenoson) is the most appropriate test to assess for **inducible myocardial ischemia**.
- This provides functional assessment of coronary perfusion under pharmacologic stress, helping guide perioperative risk stratification and management.
- *Note: The presence of unstable angina would typically require cardiac stabilization first; this question focuses on selecting the appropriate stress test modality for a patient unable to exercise.*
*No further testing*
- This patient has significant cardiac risk factors including **prior MI**, ongoing cardiac medications, and ECG changes suggesting old infarction.
- Proceeding directly to surgery without functional cardiac assessment would be **inappropriate** given his risk profile and the intermediate-risk nature of the planned surgery.
*24-hour ambulatory ECG monitoring*
- Holter monitoring detects arrhythmias and silent ischemic episodes but does not provide **functional capacity assessment** or evaluation of inducible ischemia under stress conditions.
- It is not the primary tool for **perioperative cardiac risk stratification** before major surgery.
*Treadmill stress test*
- The patient's **severe osteoarthritis** prevents him from climbing stairs or walking fast, making him unable to achieve adequate exercise workload for a treadmill stress test.
- This functional limitation makes **exercise stress testing contraindicated**; pharmacologic stress testing is required instead.
*Resting echocardiography*
- Resting echocardiography assesses **baseline left ventricular function**, wall motion abnormalities from prior infarction, and valvular disease.
- While useful for structural assessment, it does **not evaluate for exercise-induced or stress-induced ischemia**, which is critical for perioperative risk assessment in patients with coronary artery disease.
- His normal BNP (84 pg/mL) suggests adequate baseline ventricular function, making functional ischemia assessment more relevant than structural evaluation alone.
Preoperative imaging selection US Medical PG Question 10: A 56-year-old man is brought to the emergency department 25 minutes after he was involved in a high-speed motor vehicle collision where he was the unrestrained passenger. He has severe lower abdominal and pelvic pain. On arrival, he is alert and oriented. His pulse is 95/min, respirations are 22/min, and blood pressure is 106/62 mm Hg. Examination shows severe tenderness to palpation over the lower abdomen and over the left anterior superior iliac spine. There is no limb length discrepancy. Application of downward pressure over the pelvis shows no springy resistance or instability. Rectal examination is unremarkable. A focused assessment with sonography shows no free fluid in the abdomen. There is no blood at the urethral meatus. Placement of a Foley catheter shows gross hematuria. An x-ray of the pelvis shows a fracture of the left pelvic edge. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. External fixation of the pelvis
- C. Cystoscopy
- D. Retrograde urethrography
- E. Retrograde cystography (Correct Answer)
Preoperative imaging selection Explanation: ***Retrograde cystography***
- The presence of **gross hematuria** in a patient with a **pelvic fracture** necessitates ruling out **bladder injury**. A retrograde cystography directly visualizes the bladder and can detect extravasation of contrast if a bladder rupture is present.
- This imaging study specifically investigates the bladder using retrograde contrast filling, which is crucial for diagnosing **intraperitoneal** or **extraperitoneal bladder rupture**.
*Intravenous pyelography*
- This study evaluates the **kidneys** and **ureters** for injury, but the primary concern with gross hematuria and pelvic fracture is the bladder.
- An IV pyelogram provides less detailed imaging of the bladder compared to a retrograde cystogram and is less effective for detecting bladder rupture.
*External fixation of the pelvis*
- While the patient has a pelvic fracture, the immediate priority in a hemodynamically stable patient with gross hematuria is to identify and manage potential **life-threatening urologic injuries** before definitive orthopedic repair.
- **Pelvic external fixation** is primarily indicated for **unstable pelvic fractures** or those causing significant hemorrhage, neither of which is explicitly described as an immediate concern requiring intervention before urologic evaluation.
*Cystoscopy*
- **Cystoscopy** is an endoscopic procedure that allows direct visualization of the bladder's interior. While it can identify bladder injuries, it is generally considered after imaging studies like **retrograde cystography** to confirm findings or address specific issues like clot evacuation or stent placement.
- The initial diagnostic step should focus on assessing for rupture via contrast study, which is often less invasive than a direct endoscopic procedure in the acute trauma setting.
*Retrograde urethrography*
- **Retrograde urethrography (RUG)** is used to evaluate for **urethral injury**, especially when there is blood at the urethral meatus, a high-riding prostate, or an inability to pass a Foley catheter.
- The patient's Foley catheter was successfully placed, and there was **no blood at the urethral meatus**, making urethral injury less likely and thus RUG a lower priority as the initial step compared to assessing for bladder injury.
More Preoperative imaging selection US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.