DVT risk assessment US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for DVT risk assessment. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
DVT risk assessment US Medical PG Question 1: A 78-year-old woman presents to the orthopedic department for an elective total left knee arthroplasty. She has had essential hypertension for 25 years and type 2 diabetes mellitus for 35 years. She has smoked 20–30 cigarettes per day for the past 40 years. The operation was uncomplicated. On day 3 post-surgery, she complains of left leg pain and swelling. On examination, her left leg appears red and edematous, and there are dilated superficial veins on the left foot. Using Wells’ criteria, the patient is diagnosed with a provoked deep venous thrombosis. Which of the following is the best initial therapy for this patient?
- A. Oral apixaban monotherapy (Correct Answer)
- B. Inferior vena cava (IVC) filter
- C. Oral dabigatran monotherapy
- D. Complete bed rest
- E. Long-term aspirin
DVT risk assessment Explanation: ***Oral apixaban monotherapy***
- **Apixaban** is a **direct oral anticoagulant** (DOAC) that offers effective and convenient treatment for DVT, particularly in postoperative settings.
- Its fixed-dose regimen, favorable safety profile (especially regarding bleeding risk), and lack of need for routine monitoring make it a preferred initial therapy for most patients with DVT.
*Inferior vena cava (IVC) filter*
- **IVC filters** are generally reserved for patients with contraindications to anticoagulation or those who experience recurrent PEs despite adequate anticoagulation.
- They do not treat the DVT itself but rather aim to prevent pulmonary emboli, and their use is associated with potential complications.
*Oral dabigatran monotherapy*
- **Dabigatran** is another direct oral anticoagulant, but its initial DVT treatment typically involves a 5-10 day bridging period with a parenteral anticoagulant (e.g., LMWH) before starting oral therapy.
- Unlike apixaban, it is not recommended as monotherapy for initial DVT treatment.
*Complete bed rest*
- **Complete bed rest** is not recommended for DVT as it can contribute to **venous stasis** and potentially worsen outcomes.
- Early ambulation, once anticoagulation is initiated, is encouraged to reduce pain and swelling and promote recovery.
*Long-term aspirin*
- **Aspirin** has a role in secondary prevention of recurrent DVT/PE in some patients after initial anticoagulant therapy.
- It is not sufficient as a primary or initial treatment for an acute DVT, as its antithrombotic effects are much weaker compared to DOACs or other anticoagulants.
DVT risk assessment US Medical PG Question 2: A 62-year-old man comes to the physician because of a 5-day history of swelling in his left arm. Two months ago, he was diagnosed with a deep venous thrombosis in the left calf. He has had a 7-kg (15-lb) weight loss in the last 3 months. He has smoked 1 pack of cigarettes daily for the past 25 years. His only medication is warfarin. Physical examination shows warm edema of the left forearm with overlying erythema and a tender, palpable cord-like structure along the medial arm. His lungs are clear to auscultation bilaterally. Duplex sonography shows thrombosis of the left basilic and external jugular veins. Which of the following is the most appropriate next step to confirm the underlying diagnosis?
- A. CT scan of the chest
- B. X-ray of the chest (Correct Answer)
- C. Transesophageal echocardiography
- D. Serum antiphospholipid antibody level
- E. Serum D-dimer level
DVT risk assessment Explanation: **X-ray of the chest**
- The patient presents with **recurrent deep venous thrombosis (DVT)**, specifically in an unusual location (upper extremity), combined with **unexplained weight loss** and a **significant smoking history**. These are strong indicators of an underlying malignancy.
- A **chest x-ray** is a readily available and cost-effective initial screening tool to evaluate for **lung cancer**, which is common in smokers and can present with paraneoplastic phenomena like hypercoagulability (Trousseau phenomenon) leading to DVT.
*CT scan of the chest*
- While a **CT scan of the chest** is more sensitive than an X-ray for detecting lung masses, an **X-ray is the more appropriate initial step** for screening given the clinical context.
- A **CT scan** would typically be performed after an abnormal chest X-ray or if clinical suspicion remains high despite a normal X-ray.
*Transesophageal echocardiography*
- **Transesophageal echocardiography (TEE)** is primarily used to evaluate **cardiac structures**, valve function, and to detect intracardiac thrombi or vegetations.
- It is not indicated as a primary screening tool for an underlying malignancy or in the workup of a **venous thrombosis** not directly related to cardiac pathology.
*Serum antiphospholipid antibody level*
- **Antiphospholipid antibody syndrome** is a cause of recurrent thrombosis, but the patient's other symptoms (weight loss, smoking history, unusual DVT location) point more strongly towards an underlying malignancy.
- While it might be considered in a broader workup for hypercoagulability, it is not the most immediate next step given the constellation of findings strongly suggestive of cancer.
*Serum D-dimer level*
- A **serum D-dimer level** is a marker of fibrin degradation and is useful for **excluding DVT/PE** in low-probability patients.
- In this patient, a DVT has already been diagnosed by duplex sonography, so a D-dimer level would not provide additional diagnostic information regarding the presence of thrombosis, nor would it help in identifying the underlying cause of the recurrent thrombosis.
DVT risk assessment US Medical PG Question 3: A 68-year-old man undergoes successful mechanical prosthetic aortic valve replacement for severe aortic valve stenosis. After the procedure, he is started on an oral medication and instructed that he should take for the rest of his life and that he should avoid consuming large amounts of dark-green, leafy vegetables. Which of the following laboratory parameters should be regularly monitored to guide dosing of this drug?
- A. D-dimer
- B. Anti-factor Xa activity
- C. Activated partial thromboplastin time
- D. Prothrombin time (Correct Answer)
- E. Thrombin time
DVT risk assessment Explanation: ***Prothrombin time***
- **Warfarin** is the standard chronic anticoagulant post-mechanical valve replacement, and its dosing is monitored using the **prothrombin time (PT)**, reported as the **International Normalized Ratio (INR)**.
- The avoidance of dark-green, leafy vegetables indicates a **Vitamin K antagonist**, which is warfarin.
*D-dimer*
- **D-dimer** levels are primarily used to rule out **venous thromboembolism (VTE)** and are not used for routine monitoring of chronic anticoagulation.
- Elevated D-dimer indicates recent or ongoing **fibrinolysis**, which is not directly targeted by warfarin therapy.
*Anti-factor Xa activity*
- **Anti-factor Xa activity** is used to monitor the anticoagulant effect of **low molecular weight heparins (LMWH)** or **direct oral anticoagulants (DOACs)** like rivaroxaban or apixaban.
- This patient is on a vitamin K antagonist, not an anti-Xa inhibitor.
*Activated partial thromboplastin time*
- The **activated partial thromboplastin time (aPTT)** is used to monitor patients receiving **unfractionated heparin**, not warfarin.
- While both heparin and warfarin are anticoagulants, they act on different parts of the coagulation cascade and are monitored differently.
*Thrombin time*
- **Thrombin time (TT)** measures the time it takes for plasma to clot after adding thrombin, and it is primarily used to detect inherited or acquired **fibrinogen disorders** or to monitor **direct thrombin inhibitors**.
- It is not routinely used for monitoring warfarin therapy.
DVT risk assessment US Medical PG Question 4: A 56-year-old man comes to the emergency department because of progressive swelling and pain in his left calf for 1 day. He does not have shortness of breath or chest pain. He has hypertension and chronic kidney disease. Current medications include enalapril, aspirin, simvastatin, and vitamin D. His temperature is 100.4°F (38°C), pulse is 84/min, and blood pressure is 135/92 mm Hg. Physical examination shows tenderness and swelling of the left lower extremity. A venous Doppler ultrasonography shows a thrombus in the left popliteal vein. Treatment with unfractionated heparin is begun. Two days later, physical examination shows improvement of symptoms. Laboratory studies at admission and 2 days after admission show:
Admission Two days after admission
Hemoglobin 11.2 g/dL 11.1 g/dL
Leukocyte count 5,500/mm3 6,100/mm3
Platelet count 230,000/mm3 170,000/mm3
Serum
Prothrombin time 12 seconds 13 seconds
Partial thromboplastin time 30 seconds 55 seconds
Estimated glomerular filtration rate 29 mL/min/1.73 m2 28 mL/min/1.73 m2
Which of the following is the most appropriate next step in management?
- A. Switch to warfarin
- B. Obtain serum immunoassay
- C. Switch to enoxaparin
- D. Discontinue heparin and initiate argatroban (Correct Answer)
- E. Continue unfractionated heparin
DVT risk assessment Explanation: ***Discontinue heparin and initiate argatroban***
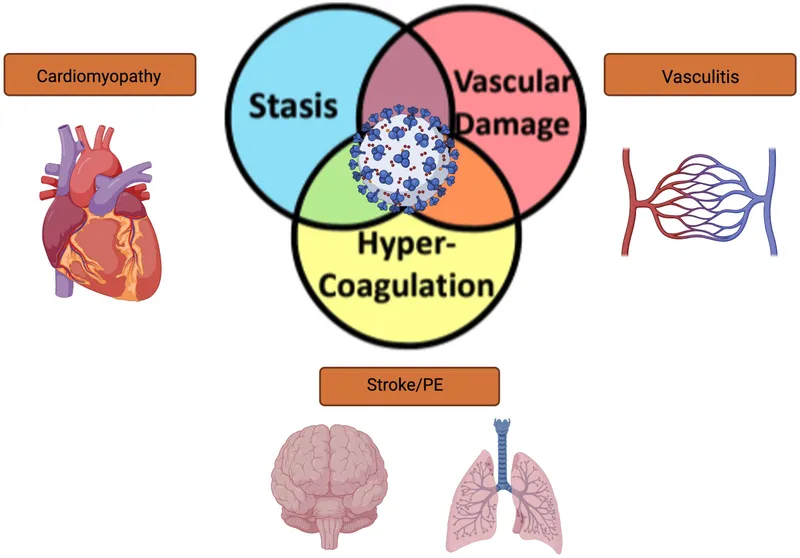
- The **26% drop in platelet count** (from 230,000 to 170,000/mm³) occurring **2 days after starting unfractionated heparin (UFH)** raises high suspicion for **heparin-induced thrombocytopenia (HIT)**.
- When HIT is suspected (intermediate to high probability by 4T score), the **most critical next step** is to **immediately discontinue all heparin products** and **start a non-heparin anticoagulant**.
- **Argatroban** is the preferred alternative in this patient with **chronic kidney disease (eGFR 28 mL/min)** as it is hepatically metabolized and safe in renal impairment.
- HIT antibody testing should be obtained concurrently, but **therapeutic anticoagulation must not be delayed** while awaiting results.
*Obtain serum immunoassay*
- While **HIT antibody testing** (heparin-PF4 immunoassay) should be obtained to confirm the diagnosis, it is **not the most appropriate next step**.
- The priority is to **stop heparin exposure immediately** and provide alternative anticoagulation to prevent thrombotic complications.
- Testing can and should be done concurrently with changing anticoagulation.
*Switch to warfarin*
- Initiating **warfarin alone** in suspected or confirmed HIT is **contraindicated** and can cause **venous limb gangrene** due to rapid depletion of protein C before clotting factors.
- Warfarin should only be started after platelet count recovery (>150,000/mm³) and after at least 5 days of therapeutic non-heparin anticoagulation.
*Switch to enoxaparin*
- **Enoxaparin** (low-molecular-weight heparin) has **>90% cross-reactivity** with HIT antibodies.
- Switching to LMWH in suspected HIT is **contraindicated** as it will perpetuate platelet activation and thrombosis.
*Continue unfractionated heparin*
- Continuing UFH with a significant **platelet drop** is dangerous and will worsen **HIT**, leading to life-threatening **arterial and venous thrombosis**.
- Immediate discontinuation is imperative.
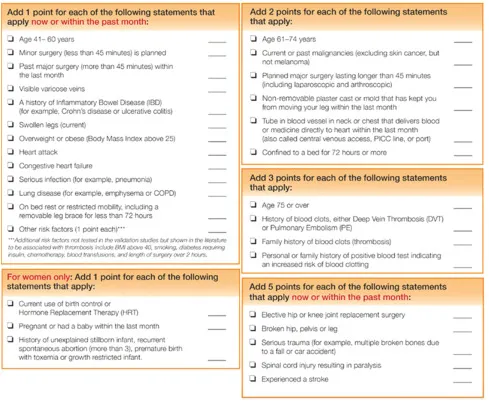
DVT risk assessment US Medical PG Question 5: A 28-year-old woman presents to the emergency department with fever, cough, and difficulty in breathing for the last 6 hours. She also mentions that she noticed some blood in her sputum an hour ago. She denies nasal congestion or discharge, sneezing, wheezing, chest pain, or palpitation. Her past history does not suggest any chronic medical condition, including respiratory disease, cardiovascular disease, or cancer. There is no history of pulmonary embolism or deep vein thrombosis in the past. Her temperature is 38.3°C (101.0°F), the pulse is 108/min, the blood pressure is 116/80 mm Hg, and the respirations are 28/min. Auscultation of her lungs reveals the presence of localized crackles over the right inframammary region. Edema is present over her left leg and tenderness is present over her left calf region. When her left foot is dorsiflexed, she complains of calf pain. The emergency department protocol mandates the use of a modified Wells scoring system in all patients presenting with the first episode of breathlessness when there is no history of a cardiorespiratory disorder in the past. According to the modified Wells scoring system, which of the following risk factors, if present, would contribute the most points toward a high clinical probability of pulmonary embolism?
- A. History of surgery within the last 30 days (Correct Answer)
- B. Use of oral contraceptives within last 90 days
- C. Intravenous drug use within last 14 days
- D. History of travel of 2 hours in 30 days
- E. History of smoking for more than 1 year
DVT risk assessment Explanation: ***History of surgery within the last 30 days***
- Recent surgery (within the previous 4 weeks) is a significant **risk factor for venous thromboembolism (VTE)** due to immobility, endothelial damage, and hypercoagulability, and contributes **1.5 points** in the modified Wells score.
- Among the options listed, this is the **only risk factor that actually contributes points** to the modified Wells score, making it the correct answer for the highest individual contribution.
- In this scoring system, scores are categorized as: ≤1 point (low probability), 2-6 points (moderate probability), and ≥7 points (high probability).
*Use of oral contraceptives within last 90 days*
- While **oral contraceptives** are a known risk factor for VTE in epidemiological studies, they are **not included as a scored component** in the modified Wells criteria for pulmonary embolism.
- The Wells score focuses on acute clinical factors rather than chronic predisposing conditions like hormonal contraception.
*Intravenous drug use within last 14 days*
- **Intravenous drug use** is not a component of the modified Wells score for pulmonary embolism.
- It may lead to other complications (such as septic emboli or endocarditis) but does not directly increase the score for PE risk in this specific diagnostic tool.
*History of travel of 2 hours in 30 days*
- **Prolonged immobilization** (≥3 days of bed rest or travel exceeding 4-6 hours) is a risk factor for VTE and would contribute **1.5 points** as part of the immobilization criterion.
- However, travel of only **2 hours** does not meet the threshold for significant immobilization and would **not contribute points** to the modified Wells score.
*History of smoking for more than 1 year*
- **Smoking** is a general risk factor for various cardiovascular and pulmonary diseases but is **not a component** of the modified Wells score for assessing the acute probability of pulmonary embolism.
- While it contributes to overall cardiovascular risk, it does not add points in this specific diagnostic tool for PE.
DVT risk assessment US Medical PG Question 6: A 52-year-old woman presents to the emergency room complaining of chest pain. She reports a 4-hour history of dull substernal pain radiating to her jaw. Her history is notable for hypertension, diabetes mellitus, and alcohol abuse. She has a 30 pack-year smoking history and takes lisinopril and metformin but has an allergy to aspirin. Her temperature is 99.1°F (37.3°C), blood pressure is 150/90 mmHg, pulse is 120/min, and respirations are 22/min. Physical examination reveals a diaphoretic and distressed woman. An electrocardiogram reveals ST elevations in leads I, aVL, and V5-6. She is admitted with plans for immediate transport to the catheterization lab for stent placement. What is the mechanism of the next medication that should be given to this patient?
- A. Cyclooxygenase activator
- B. ADP receptor inhibitor (Correct Answer)
- C. Phosphodiesterase activator
- D. Thrombin inhibitor
- E. Vitamin K epoxide reductase inhibitor
DVT risk assessment Explanation: ***ADP receptor inhibitor***
- This patient is experiencing an **ST-elevation myocardial infarction (STEMI)** as evidenced by ST elevations in leads I, aVL, and V5-6 (lateral wall infarction)
- **Dual antiplatelet therapy** is the standard of care for STEMI, typically consisting of aspirin plus a P2Y12 inhibitor (ADP receptor inhibitor)
- Since this patient has an **aspirin allergy**, an ADP receptor inhibitor such as **clopidogrel, ticagrelor, or prasugrel** becomes the critical next antiplatelet medication
- These agents **irreversibly or reversibly block the P2Y12 receptor** on platelets, preventing ADP-mediated platelet activation and aggregation
- This is essential for preventing further thrombotic complications during and after percutaneous coronary intervention (PCI)
*Cyclooxygenase activator*
- No cyclooxygenase activator exists in clinical practice for cardiovascular disease
- Aspirin works as a **cyclooxygenase inhibitor**, blocking COX-1 to prevent thromboxane A2 synthesis, but the patient is allergic to aspirin
- "Activating" cyclooxygenase would promote platelet aggregation, which is counterproductive in acute MI
*Phosphodiesterase activator*
- Phosphodiesterase activation would decrease cAMP/cGMP levels, which is not therapeutically beneficial
- **Phosphodiesterase inhibitors** (such as cilostazol or dipyridamole) can have antiplatelet effects by increasing cAMP, but they are not first-line agents for acute STEMI
- An activator would have the opposite and undesirable effect
*Thrombin inhibitor*
- Thrombin inhibitors (e.g., **bivalirudin, heparin**) are anticoagulants that prevent conversion of fibrinogen to fibrin
- While **anticoagulation is important in STEMI management**, it is used as adjunctive therapy alongside antiplatelet agents
- Given the aspirin allergy, the immediate priority is **antiplatelet therapy with an ADP receptor inhibitor**
- Anticoagulation would typically be given concurrently but is not "the next" critical medication in this specific context
*Vitamin K epoxide reductase inhibitor*
- Warfarin is a vitamin K epoxide reductase inhibitor used for chronic anticoagulation
- It has a **slow onset of action** (days) and is inappropriate for acute STEMI management
- It is used for long-term anticoagulation in conditions like atrial fibrillation or mechanical heart valves, not for acute coronary syndromes requiring rapid platelet inhibition
DVT risk assessment US Medical PG Question 7: A 38-year-old male is brought to the emergency department by ambulance after a motor vehicle collision. He is found to have a broken femur and multiple soft tissue injuries and is admitted to the hospital. During the hospital course, he is found to have lower extremity swelling, redness, and pain, so he is given an infusion of a medication. The intravenous medication is discontinued in favor of an oral medication in preparation for discharge; however, the patient leaves against medical advice prior to receiving the full set of instructions. The next day, the patient is found to have black lesions on his trunk and his leg. The protein involved in this patient's underlying abnormality most likely affects the function of which of the following factors?
- A. Factor II only
- B. Factors II, VII, IX, and X
- C. Factors II and X
- D. Factors V and VIII (Correct Answer)
- E. Factor V only
DVT risk assessment Explanation: ***Factors V and VIII***
- The patient's initial presentation of **lower extremity swelling, redness, and pain** after trauma and immobilization is highly suggestive of **deep vein thrombosis (DVT)**, for which he received IV anticoagulation. The subsequent development of **black lesions on his trunk and leg** after switching to an oral anticoagulant and leaving against medical advice points to **warfarin-induced skin necrosis (WISN)**.
- **Warfarin-induced skin necrosis** develops in patients with a congenital deficiency of **protein C** or, less commonly, **protein S**. Protein C, in its activated form (APC), functions to inactivate **Factor V (Va)** and **Factor VIII (VIIIa)**, which are crucial cofactors in the coagulation cascade. A deficiency means these factors remain active, leading to a **procoagulant state**.
*Factor II only*
- **Factor II (prothrombin)** is inactivated by protein C, but a deficiency in protein C primarily affects the inactivation of **Factors V and VIII**, which are the specific targets of activated protein C.
- While factor II is part of the coagulation cascade, its regulation is not the primary mechanism by which protein C deficiency leads to the hypercoagulable state seen in WISN.
*Factors II, VII, IX, and X*
- These factors are **vitamin K-dependent coagulation factors**, which are inhibited by warfarin. While a deficiency in protein C can lead to an initial hypercoagulable state when warfarin is started (due to the faster drop in protein C levels compared to these factors), the primary function of protein C is to inactivate **Factors V and VIII**.
- The problem described is a **protein C deficiency**, which specifically impacts the inactivation of factors V and VIII, not directly these other vitamin K-dependent factors.
*Factors II and X*
- Similar to Factor II only, these are **vitamin K-dependent factors** inhibited by warfarin. The core issue in warfarin-induced skin necrosis is a deficiency in protein C, which normally inactivates **Factors V and VIII**, leading to a transient prothrombotic state.
- While Factor X is affected by warfarin, the direct regulatory role of protein C is predominantly on factors V and VIII.
*Factor V only*
- While **Factor V** is indeed a target of activated protein C inactivation, **Factor VIII** is also a critical target. Inactivating both **Factor V** and **Factor VIII** is essential for effective anticoagulation by protein C.
- A deficiency in protein C affects both of these crucial cofactors, making the combined option more accurate.
DVT risk assessment US Medical PG Question 8: Three days after undergoing laparoscopic colectomy, a 67-year-old man reports swelling and pain in his right leg. He was diagnosed with colon cancer 1 month ago. His temperature is 38.5°C (101.3°F). Physical examination shows swelling of the right leg from the ankle to the thigh. There is no erythema or rash. Which of the following is likely to be most helpful in establishing the diagnosis?
- A. D-dimer level
- B. Compression ultrasonography (Correct Answer)
- C. CT pulmonary angiography
- D. Transthoracic echocardiography
- E. Blood cultures
DVT risk assessment Explanation: ***Compression ultrasonography***
- This patient's presentation with **unilateral leg swelling and pain** after surgery, especially given his recent **colon cancer diagnosis** (a hypercoagulable state), is highly suspicious for a **deep vein thrombosis (DVT)**.
- **Compression ultrasonography** is the gold standard, non-invasive imaging modality for diagnosing DVT, allowing direct visualization of thrombi and assessing venous compressibility.
*D-dimer level*
- While a **positive D-dimer** indicates recent or ongoing clot formation, it is **non-specific** and can be elevated in many conditions, including surgery, cancer, and infection.
- A normal D-dimer can rule out DVT in low-probability patients, but a high D-dimer in a high-probability patient (like this case) requires further imaging for confirmation, making it less definitive than ultrasound.
*CT pulmonary angiography*
- This imaging is used to diagnose a **pulmonary embolism (PE)**, which is a complication of DVT, but the primary symptoms here are localized to the leg.
- While PE is a concern, diagnosing the source (DVT) in the leg is the immediate priority for treatment and prevention of future complications.
*Transthoracic echocardiography*
- **Echocardiography** evaluates cardiac structure and function and can sometimes detect large clots in the right heart leading to PE, but it is not the primary diagnostic tool for DVT in the leg.
- It would be done if signs of cardiac strain or shunting associated with acute PE were prominent, which is not the case here.
*Blood cultures*
- **Blood cultures** are used to diagnose **bacteremia or sepsis**, which might explain a fever, but the prominent, unilateral leg swelling and pain are not typical for a primary infectious cause in the leg without local signs of cellulitis or abscess.
- While a low-grade fever is present, the absence of erythema or rash makes a primary infectious etiology less likely than DVT given the risk factors.
DVT risk assessment US Medical PG Question 9: A 45-year-old man presents to the emergency department because of fever and scrotal pain for 2 days. Medical history includes diabetes mellitus and morbid obesity. His temperature is 40.0°C (104.0°F), the pulse is 130/min, the respirations are 35/min, and the blood pressure is 90/68 mm Hg. Physical examination shows a large area of ecchymosis, edema, and crepitus in his perineal area. Fournier gangrene is suspected. A right internal jugular central venous catheter is placed without complication under ultrasound guidance for vascular access in preparation for the administration of vasopressors. Which of the following is the most appropriate next step?
- A. Confirm line placement by ultrasound
- B. Begin to use the line after documenting the return of dark, non-pulsatile blood from all ports
- C. Begin infusion of normal saline through a central line
- D. Obtain an immediate portable chest radiograph to evaluate line placement (Correct Answer)
- E. Begin infusion of norepinephrine to maintain systolic blood pressure over 90 mm Hg
DVT risk assessment Explanation: **Obtain an immediate portable chest radiograph to evaluate line placement**
- The most appropriate next step after central venous catheter placement is to **confirm its correct position** and rule out complications like **pneumothorax** via imaging.
- A **chest radiograph** is the standard and immediate method to confirm proper placement of the tip in the lower superior vena cava and rule out pneumothorax, especially given the patient's critical condition.
*Confirm line placement by ultrasound*
- While ultrasound is used during placement to visualize the vessel and guide needle insertion, it is **not sufficient for confirming the final tip position** of the catheter or for ruling out pneumothorax.
- Ultrasound confirmation usually involves visualizing a **saline flush** in the right atrium, but a chest X-ray is still required for comprehensive evaluation.
*Begin to use the line after documenting the return of dark, non-pulsatile blood from all ports*
- Documenting blood return confirms that the catheter is in a vein but does not confirm **optimal tip placement** or exclude potential complications like **pneumothorax**.
- Using the line without radiological confirmation can lead to administering medications into incorrect locations (e.g., subclavian artery) or exacerbating unnoticed complications.
*Begin infusion of normal saline through a central line*
- Administering fluids before confirming proper line placement carries the risk of **extravasation** or infusing into an artery or other unintended space, which could worsen the patient's condition.
- Although IV fluids are needed in this septic patient, **confirmation of line placement** is a higher priority before commencing infusions.
*Begin infusion of norepinephrine to maintain systolic blood pressure over 90 mm Hg*
- While norepinephrine is crucial for managing septic shock and **hypotension** in this patient, starting it before confirming central line placement is dangerous.
- **Vasopressors require a secure central line** to prevent severe local tissue damage if extravasation occurs.
DVT risk assessment US Medical PG Question 10: A 30-year-old male gang member is brought to the emergency room with a gunshot wound to the abdomen. The patient was intubated and taken for an exploratory laparotomy, which found peritoneal hemorrhage and injury to the small bowel. He required 5 units of blood during this procedure. Following the operation, the patient was sedated and remained on a ventilator in the surgical intensive care unit (SICU). The next day, a central line is placed and the patient is started on total parenteral nutrition. Which of the following complications is most likely in this patient?
- A. Mesenteric ischemia
- B. Hypocalcemia
- C. Refeeding syndrome
- D. Sepsis (Correct Answer)
- E. Cholelithiasis
DVT risk assessment Explanation: ***Sepsis***
- This patient has undergone **major abdominal surgery** after a **gunshot wound**, which carries a high risk of **peritoneal contamination** and subsequent infection.
- He also has several risk factors for sepsis, including **intubation**, central line placement, and possibly prolonged ventilation, all of which increase the risk of nosocomial infections and subsequent sepsis.
*Mesenteric ischemia*
- While possible in critically ill patients, there is no direct evidence such as advanced age, atherosclerosis, or specific signs of **bowel ischemia** (e.g., severe abdominal pain disproportionate to exam, bloody diarrhea) presenting in this case.
- The initial injury was to the small bowel, but the current context points more to systemic complications rather than a focal vascular event.
*Hypocalcemia*
- Hypocalcemia can occur in critically ill patients due to various reasons, but it is not the *most likely* complication given the patient's presentation primarily focused on surgical trauma and subsequent interventions.
- Dilutional effects from massive transfusions or **citrate toxicity** could contribute to temporary hypocalcemia, but sepsis poses a more immediate and widespread threat.
*Refeeding syndrome*
- Refeeding syndrome occurs when severely malnourished patients are rapidly refed, leading to shifts in **electrolytes** (especially **phosphate**, potassium, magnesium).
- Although the patient is starting **total parenteral nutrition (TPN)**, there's no indication of prior severe malnutrition, making sepsis a more prominent immediate concern due to the gunshot wound and surgery.
*Cholelithiasis*
- **Cholelithiasis** (gallstones) can be a long-term complication of total parenteral nutrition (TPN) due to gallbladder stasis.
- However, it is unlikely to develop so acutely within a day of starting TPN and is thus not the most immediate or likely complication for this patient's acute critical state.
More DVT risk assessment US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.