Pre-operative evaluation

On this page
🎯 The Pre-Operative Command Center: Surgical Success Starts Here
Every surgical procedure begins long before the first incision-in the pre-operative evaluation where you'll identify hidden risks, optimize medical conditions, and transform uncertainty into calculated safety. You'll master cardiac and pulmonary risk stratification, learn which lab tests actually matter, navigate the complex decisions around continuing or holding medications, and understand how anesthesiologists assess patient readiness. This systematic approach doesn't just check boxes; it prevents complications, reduces mortality, and ensures your patients reach the operating room in their best possible condition.
📌 Remember: PREPARE - Pulmonary assessment, Renal function, Endocrine status, Pharmacology review, Airway evaluation, Risk stratification, Education and consent
The systematic approach to pre-operative evaluation follows evidence-based protocols that reduce surgical mortality by 40% when properly implemented. Understanding this framework enables prediction of surgical outcomes before the first incision.
- Risk Stratification Categories
- Low Risk (<1% mortality): Superficial procedures, cataract surgery
- ASA Class I-II patients
- Procedures <30 minutes duration
- Minimal physiologic stress
- Intermediate Risk (1-5% mortality): Intraperitoneal surgery, carotid endarterectomy
- ASA Class III patients
- Procedures 30-180 minutes
- Moderate physiologic stress
- High Risk (>5% mortality): Aortic surgery, major emergency procedures
- ASA Class IV-V patients
- Procedures >180 minutes
- Major physiologic stress
- Low Risk (<1% mortality): Superficial procedures, cataract surgery
| Risk Factor | Low Risk | Intermediate Risk | High Risk | Mortality Impact | Intervention Threshold |
|---|---|---|---|---|---|
| Cardiac | No CAD | Stable angina | Unstable angina | 3-fold increase | RCRI ≥2 |
| Pulmonary | Normal PFTs | Mild COPD | FEV1 <40% | 2.5-fold increase | PFTs indicated |
| Renal | Cr <1.2 | Cr 1.2-2.0 | Cr >2.0 | 4-fold increase | eGFR <60 |
| Hepatic | Normal LFTs | Child-Pugh A | Child-Pugh B/C | 5-fold increase | MELD >15 |
| Age | <65 years | 65-80 years | >80 years | 1.5-fold per decade | Frailty assessment |
💡 Master This: Pre-operative evaluation reduces surgical complications by 35-50% through systematic identification and optimization of modifiable risk factors before physiologic stress occurs.
The foundation of surgical safety depends on understanding that every patient carries unique risk profiles requiring individualized assessment strategies. Connect this systematic approach through cardiac risk stratification to understand how specific organ systems determine surgical outcomes.
🎯 The Pre-Operative Command Center: Surgical Success Starts Here
⚡ Cardiac Risk Stratification: The Heart of Surgical Safety
📌 Remember: CRIMES - Cerebrovascular disease, Renal dysfunction (Cr >2.0), Ischemic heart disease, Major surgery, Endocrine (diabetes), Supraventricular surgery
The RCRI score directly correlates with perioperative cardiac event rates, enabling precise risk quantification and management decisions. Each additional risk factor exponentially increases cardiac complications.
- RCRI Risk Stratification
- 0 Risk Factors: 0.4% cardiac event rate
- Proceed to surgery without delay
- Standard perioperative monitoring
- No additional cardiac testing required
- 1 Risk Factor: 0.9% cardiac event rate
- Consider functional capacity assessment
- Optimize medical therapy
- Standard monitoring adequate
- 2 Risk Factors: 7% cardiac event rate
- Cardiology consultation recommended
- Stress testing if poor functional capacity
- Enhanced perioperative monitoring
- ≥3 Risk Factors: 11% cardiac event rate
- Mandatory cardiology evaluation
- Stress testing or coronary angiography
- Consider surgery delay for optimization
- 0 Risk Factors: 0.4% cardiac event rate
| Surgery Type | Cardiac Risk | 30-Day MI Rate | Mortality Rate | Monitoring Level | Assessment Required |
|---|---|---|---|---|---|
| Superficial | <1% | 0.1% | <0.5% | Standard | Basic history/exam |
| Intermediate | 1-5% | 0.5-1.5% | 0.5-1.5% | Enhanced | RCRI + functional capacity |
| Vascular | >5% | 2-5% | 2-5% | Intensive | Full cardiac evaluation |
| Emergency | Variable | 3-15% | 5-25% | Maximum | Risk vs benefit analysis |
| Aortic | >10% | 5-15% | 5-15% | Maximum | Mandatory optimization |
The 4-MET threshold represents the critical functional capacity dividing line for cardiac risk assessment. Patients unable to achieve 4 METs during daily activities require enhanced cardiac evaluation regardless of RCRI score.
- Functional Capacity Assessment
- Excellent (>10 METs): Run 8 mph, carry 80 lbs upstairs
- Proceed to surgery without cardiac testing
- Risk equivalent to healthy population
- Standard perioperative care adequate
- Good (7-10 METs): Heavy housework, climb 2 flights rapidly
- Low cardiac risk regardless of RCRI
- Consider optimization of medical therapy
- Enhanced monitoring for high-risk surgery
- Moderate (4-7 METs): Walk 4 mph on level ground
- Intermediate risk requiring RCRI assessment
- Stress testing if ≥2 risk factors
- Cardiology consultation recommended
- Poor (<4 METs): Cannot walk 2 blocks or climb 1 flight
- High risk requiring comprehensive evaluation
- Stress testing or angiography indicated
- Mandatory optimization before surgery
- Excellent (>10 METs): Run 8 mph, carry 80 lbs upstairs
💡 Master This: Cardiac risk stratification combines objective RCRI scoring with functional capacity assessment to predict perioperative events with 85% accuracy, enabling evidence-based surgical decision-making.
Understanding cardiac risk assessment provides the foundation for comprehensive evaluation. Connect this systematic approach through pulmonary risk evaluation to understand how respiratory function impacts surgical outcomes.
⚡ Cardiac Risk Stratification: The Heart of Surgical Safety
🫁 Pulmonary Risk Assessment: Breathing Life into Surgical Safety
📌 Remember: COPD RISK - Chronic lung disease, Obesity (BMI >30), Poor functional status, Dyspnea at rest, Recent respiratory infection, Immobility, Smoking history, Kidney disease
The pulmonary risk assessment integrates clinical factors with objective testing to predict respiratory complications. Each risk factor contributes additively to overall pulmonary morbidity.
- Pulmonary Risk Factors
- Patient Factors (Non-modifiable)
- Age >70 years: 2-fold increased risk
- COPD with FEV1 <50%: 4-fold increased risk
- Congestive heart failure: 3-fold increased risk
- Procedure Factors (Non-modifiable)
- Upper abdominal surgery: 6-fold increased risk
- Thoracic surgery: 8-fold increased risk
- Surgery duration >3 hours: 2-fold increased risk
- Modifiable Factors
- Active smoking: 3-fold increased risk
- Obesity BMI >35: 2.5-fold increased risk
- Poor nutritional status: 2-fold increased risk
- Patient Factors (Non-modifiable)
| Risk Category | PFT Criteria | Complication Rate | Mortality Risk | Intervention Strategy | Optimization Time |
|---|---|---|---|---|---|
| Low Risk | FEV1 >80% | 2-5% | <1% | Standard care | None required |
| Moderate Risk | FEV1 50-80% | 10-20% | 1-3% | Bronchodilators + PT | 2-4 weeks |
| High Risk | FEV1 30-50% | 25-40% | 3-8% | Pulmonary rehabilitation | 6-8 weeks |
| Prohibitive | FEV1 <30% | >50% | >15% | Consider alternatives | 3-6 months |
| Emergency | Any level | Variable | 5-25% | Risk vs benefit | Immediate |
Pulmonary function testing provides objective risk stratification for patients with known or suspected lung disease. The FEV1 represents the most predictive single parameter for respiratory complications.
- PFT Interpretation for Surgical Risk
- FEV1 >80% predicted: Proceed without pulmonary optimization
- Standard perioperative care adequate
- Early mobilization and incentive spirometry
- Monitor for standard complications
- FEV1 50-80% predicted: Optimize bronchodilator therapy
- Inhaled β2-agonists and anticholinergics
- Consider systemic corticosteroids
- Enhanced respiratory monitoring
- FEV1 30-50% predicted: Comprehensive pulmonary rehabilitation
- 6-8 weeks pre-operative conditioning
- Nutritional optimization and weight loss
- Smoking cessation mandatory
- FEV1 <30% predicted: Consider non-surgical alternatives
- Prohibitive risk for elective procedures
- Multidisciplinary team evaluation
- Palliative care consultation if appropriate
- FEV1 >80% predicted: Proceed without pulmonary optimization
💡 Master This: Pulmonary risk assessment combines clinical risk factors with objective PFT values to predict respiratory complications with 80% accuracy, enabling targeted interventions that reduce morbidity by 40%.
Pulmonary assessment integrates with overall risk stratification to optimize surgical outcomes. Connect this respiratory evaluation through laboratory testing strategies to understand how biochemical markers guide perioperative management.
🫁 Pulmonary Risk Assessment: Breathing Life into Surgical Safety
🔬 Laboratory Testing Strategy: The Biochemical Blueprint
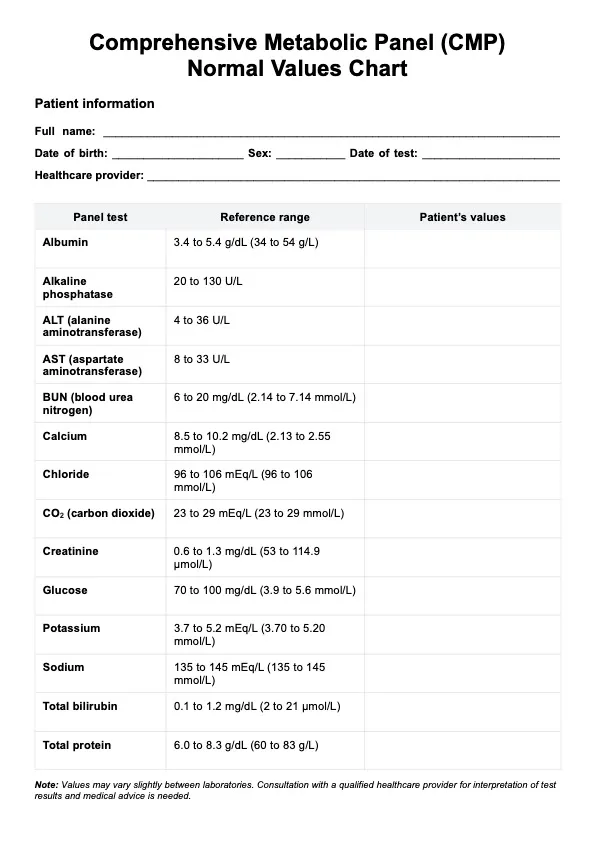
📌 Remember: LABS WISE - Liver function, Anemia assessment, Bleeding studies, Sugar control, White count, Ions and kidney, Specific indications, Electrolytes
Laboratory testing should follow indication-based protocols rather than routine screening approaches. Each test must have specific clinical justification and potential to change perioperative management.
- Evidence-Based Testing Indications
- Complete Blood Count
- Age >65 years or cardiovascular disease
- History of anemia, bleeding, or hematologic disorders
- Major surgery with expected blood loss >500 mL
- Malignancy or chemotherapy history
- Basic Metabolic Panel
- Diabetes mellitus or endocrine disorders
- Hypertension or cardiovascular disease
- Renal disease or nephrotoxic medications
- Age >70 years for intermediate/high-risk surgery
- Coagulation Studies
- Anticoagulant or antiplatelet therapy
- Liver disease or bleeding history
- Family history of bleeding disorders
- Surgery with high bleeding risk
- Complete Blood Count
| Test Category | Clinical Indication | Abnormal Threshold | Management Impact | Cost per Test | Yield Rate |
|---|---|---|---|---|---|
| CBC | Age >65, bleeding history | Hgb <10 g/dL | Transfusion planning | $25 | 15% |
| BMP | DM, HTN, renal disease | Cr >1.5 mg/dL | Nephrotoxin avoidance | $30 | 20% |
| PT/INR | Anticoagulation, liver disease | INR >1.5 | Reversal strategy | $20 | 25% |
| LFTs | Liver disease, alcohol use | ALT >2x normal | Anesthesia modification | $40 | 10% |
| HbA1c | Diabetes mellitus | >8% | Glucose optimization | $35 | 30% |
Specific laboratory abnormalities require targeted interventions before surgery to optimize outcomes. Understanding normal values and intervention thresholds enables evidence-based decision-making.
- Critical Laboratory Thresholds
- Hemoglobin Optimization
- >10 g/dL: Proceed to surgery without intervention
- 8-10 g/dL: Consider iron supplementation or EPO
- <8 g/dL: Investigate cause and optimize before elective surgery
- <7 g/dL: Transfusion indicated for symptomatic anemia
- Renal Function Assessment
- eGFR >60: Normal perioperative management
- eGFR 30-60: Nephrotoxin avoidance and hydration
- eGFR 15-30: Nephrology consultation recommended
- eGFR <15: Dialysis coordination required
- Glucose Control Targets
- HbA1c <7%: Optimal glycemic control
- HbA1c 7-8%: Acceptable for surgery
- HbA1c 8-10%: Consider optimization delay
- HbA1c >10%: Mandatory endocrine consultation
- Hemoglobin Optimization
💡 Master This: Evidence-based laboratory testing reduces unnecessary costs by 60% while identifying clinically significant abnormalities in 15-25% of appropriately selected patients, optimizing both safety and resource utilization.
Laboratory assessment provides biochemical foundation for surgical planning. Connect this systematic testing approach through medication management strategies to understand how pharmacologic interventions impact perioperative care.
🔬 Laboratory Testing Strategy: The Biochemical Blueprint
💊 Perioperative Medication Management: The Pharmacologic Balancing Act
📌 Remember: MEDS STOP - Metformin, Enoxaparin, Diuretics, Statins (continue), Steroids (stress dose), Thyroid (continue), Opioids (taper), Platelet inhibitors
Perioperative medication management requires balancing therapeutic benefits against surgical risks. Each medication class demands specific timing and modification strategies based on pharmacokinetics and surgical requirements.
- Anticoagulation Management
- Warfarin (INR target <1.5)
- Discontinue 5 days before surgery
- Bridge with LMWH if high thrombotic risk
- Resume 12-24 hours post-operatively
- Direct Oral Anticoagulants
- Stop 24-48 hours before surgery (CrCl dependent)
- No routine bridging required
- Resume when hemostasis achieved
- Antiplatelet Therapy
- Aspirin: Continue for cardiac stents, stop 7 days for bleeding risk
- Clopidogrel: Stop 5 days before surgery
- Dual therapy: Cardiology consultation required
- Warfarin (INR target <1.5)
| Medication Class | Action Required | Timing | Rationale | Monitoring | Restart Protocol |
|---|---|---|---|---|---|
| ACE Inhibitors | Hold morning of surgery | Day of surgery | Hypotension risk | BP monitoring | POD 1-2 |
| Metformin | Stop 48h before | 2 days prior | Lactic acidosis | Renal function | When eating |
| Insulin | Reduce by 50% | Night before | Hypoglycemia | Glucose q2h | Sliding scale |
| Steroids | Stress dose | Day of surgery | Adrenal insufficiency | Electrolytes | Taper schedule |
| Statins | Continue | No interruption | Pleiotropic benefits | LFTs if indicated | No change |
Specific medication classes require individualized management strategies based on half-life, mechanism of action, and surgical bleeding risk. Understanding pharmacokinetics enables optimal timing decisions.
- High-Risk Medication Categories
- Anticoagulants and Antiplatelets
- Warfarin: 5-day washout period for INR normalization
- Rivaroxaban: 24-hour washout (normal renal function)
- Apixaban: 48-hour washout (CrCl <50)
- Clopidogrel: 5-day washout for platelet recovery
- Cardiovascular Medications
- ACE inhibitors: Hold morning of surgery (hypotension risk)
- Beta-blockers: Continue perioperatively (withdrawal syndrome)
- Diuretics: Hold morning of surgery (volume depletion)
- Statins: Continue throughout (anti-inflammatory benefits)
- Endocrine Medications
- Metformin: Stop 48 hours before (lactic acidosis risk)
- Insulin: Reduce basal by 50% night before
- Oral hypoglycemics: Hold morning of surgery
- Thyroid hormone: Continue without interruption
- Anticoagulants and Antiplatelets
💡 Master This: Systematic medication management reduces perioperative complications by 30% through evidence-based protocols that balance therapeutic benefits against surgical risks, optimizing both safety and efficacy.
Medication management integrates with comprehensive risk assessment to ensure surgical safety. Connect this pharmacologic approach through anesthesia evaluation to understand how perioperative care coordination optimizes outcomes.
💊 Perioperative Medication Management: The Pharmacologic Balancing Act
🎭 Anesthesia Evaluation: The Perioperative Safety Net
📌 Remember: AIRWAY SAFE - Anatomy assessment, Intubation history, Range of motion, Weight/BMI, Apnea history, Youth vs elderly, Surgery type, Allergies, Fasting status, Emergency vs elective
The ASA Physical Status Classification provides standardized risk stratification that correlates directly with perioperative morbidity and mortality. Each ASA class represents exponentially increasing risk levels.
- ASA Classification System
- ASA I: Healthy patient without systemic disease
- Mortality risk: 0.05%
- Standard monitoring adequate
- Minimal perioperative complications
- ASA II: Mild systemic disease without functional limitation
- Mortality risk: 0.2%
- Enhanced monitoring recommended
- Controlled hypertension, diabetes, obesity
- ASA III: Severe systemic disease with functional limitation
- Mortality risk: 1.8%
- Intensive monitoring required
- Unstable angina, COPD with dyspnea, dialysis
- ASA IV: Severe disease that is constant threat to life
- Mortality risk: 7.8%
- Maximum monitoring and support
- Recent MI, severe heart failure, sepsis
- ASA I: Healthy patient without systemic disease
| Airway Assessment | Normal Finding | Concerning Finding | Intubation Difficulty | Management Strategy | Success Rate |
|---|---|---|---|---|---|
| Mallampati | Class I-II | Class III-IV | 5-fold increase | Video laryngoscopy | 95% vs 75% |
| Thyromental Distance | >6 cm | <6 cm | 3-fold increase | Awake intubation | 98% vs 85% |
| Neck Extension | >35 degrees | <35 degrees | 4-fold increase | Flexible bronchoscopy | 99% vs 80% |
| Mouth Opening | >3 cm | <3 cm | 6-fold increase | Surgical airway | 95% vs 60% |
| BMI | <30 | >40 | 2-fold increase | Ramped positioning | 90% vs 75% |
Airway assessment represents the most critical component of anesthesia evaluation, as airway complications can rapidly become life-threatening. Systematic evaluation identifies high-risk patients requiring specialized management.
- Comprehensive Airway Assessment
- Anatomical Factors
- Mallampati Class III-IV: Tongue obscures pharyngeal structures
- Short thyromental distance (<6 cm): Limited laryngeal exposure
- Reduced neck extension (<35 degrees): Difficult laryngoscopy
- Limited mouth opening (<3 cm): Inadequate visualization
- Historical Factors
- Previous difficult intubation: 10-fold increased risk
- Sleep apnea: 3-fold increased risk
- Radiation therapy: 5-fold increased risk
- Facial trauma: 8-fold increased risk
- Physiological Factors
- BMI >40: 2-fold increased difficulty
- Pregnancy: 8-fold increased aspiration risk
- Emergency surgery: 4-fold increased complications
- Full stomach: 6-fold increased aspiration risk
- Anatomical Factors
💡 Master This: Anesthesia evaluation combines ASA risk stratification with systematic airway assessment to predict perioperative complications with 90% accuracy, enabling proactive management strategies that reduce morbidity by 40%.
Anesthesia assessment completes the comprehensive pre-operative evaluation framework. Connect this systematic approach through rapid mastery tools to synthesize all components into practical clinical decision-making frameworks.
🎭 Anesthesia Evaluation: The Perioperative Safety Net
🚀 Pre-Operative Mastery Arsenal: Your Clinical Command Center
📌 Remember: SURGICAL SUCCESS - Systematic assessment, Understand risks, Risk stratification, Guideline adherence, Individualized care, Communication, Airway evaluation, Lab optimization, Safety protocols, Unified approach, Comprehensive planning, Continuous monitoring, Evidence-based decisions, Standard protocols, Safety first
The Essential Numbers Arsenal provides rapid reference for critical thresholds that determine surgical safety and timing decisions.
- Critical Threshold Quick Reference
- Cardiac Risk: RCRI ≥2 = cardiology consult, <4 METs = stress test
- Pulmonary Risk: FEV1 <50% = optimization, <30% = prohibitive
- Renal Function: eGFR <60 = nephrotoxin avoidance, <30 = nephrology
- Anemia: Hgb <10 = investigate, <8 = optimize, <7 = transfuse
- Anticoagulation: Stop warfarin 5 days, DOAC 24-48 hours, clopidogrel 5 days
- Diabetes: HbA1c >8% = optimize, >10% = endocrine consult
- Airway: ≥3 predictors = awake intubation, Mallampati III-IV = video laryngoscopy
| Risk Category | Assessment Tool | Low Risk Action | High Risk Action | Optimization Time | Success Metric |
|---|---|---|---|---|---|
| Cardiac | RCRI + METs | Standard care | Stress test + optimization | 4-6 weeks | Event rate <2% |
| Pulmonary | PFTs + clinical | Incentive spirometry | Pulmonary rehab | 6-8 weeks | Complication <10% |
| Renal | eGFR + proteinuria | Standard hydration | Nephrology consult | 2-4 weeks | AKI rate <5% |
| Nutritional | Albumin + BMI | Standard diet | Nutrition support | 2-4 weeks | Wound healing >90% |
| Functional | Frailty assessment | Early mobilization | Prehabilitation | 4-8 weeks | Independence >80% |
💡 Master This: Pre-operative evaluation excellence combines systematic risk assessment, evidence-based optimization, and multidisciplinary coordination to transform surgical outcomes through proactive identification and management of modifiable risk factors.
🚀 Pre-Operative Mastery Arsenal: Your Clinical Command Center
Practice Questions: Pre-operative evaluation
Test your understanding with these related questions
A 36-year-old woman is brought to the emergency department 20 minutes after being involved in a high-speed motor vehicle collision. On arrival, she is unconscious. Her pulse is 140/min, respirations are 12/min and shallow, and blood pressure is 76/55 mm Hg. 0.9% saline infusion is begun. A focused assessment with sonography shows blood in the left upper quadrant of the abdomen. Her hemoglobin concentration is 7.6 g/dL and hematocrit is 22%. The surgeon decided to move the patient to the operating room for an emergent explorative laparotomy. Packed red blood cell transfusion is ordered prior to surgery. However, a friend of the patient asks for the transfusion to be held as the patient is a Jehovah's Witness. The patient has no advance directive and there is no documentation showing her refusal of blood transfusions. The patient's husband and children cannot be contacted. Which of the following is the most appropriate next best step in management?













