Recognition and management of SSIs US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Recognition and management of SSIs. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Recognition and management of SSIs US Medical PG Question 1: A 23-year-old man comes to the emergency department with an open wound on his right hand. He states that he got into a bar fight about an hour ago. He appears heavily intoxicated and does not remember the whole situation, but he does recall lying on the ground in front of the bar after the fight. He does not recall any history of injuries but does remember a tetanus shot he received 6 years ago. His temperature is 37°C (98.6°F), pulse is 77/min, and blood pressure is 132/78 mm Hg. Examination shows a soft, nontender abdomen. His joints have no bony deformities and display full range of motion. There is a 4-cm (1.6-in) lesion on his hand with the skin attached only on the ulnar side. The wound, which appears to be partly covered with soil and dirt, is irrigated and debrided by the hospital staff. Minimal erythema and no purulence is observed in the area surrounding the wound. What is the most appropriate next step in management?
- A. Apposition of wound edges under tension + rifampin
- B. Surgical treatment with skin flap + ciprofloxacin
- C. Surgical treatment with skin graft + tetanus vaccine
- D. Tension-free apposition of wound edges + sterile dressing
- E. Application of moist sterile dressing + tetanus vaccine (Correct Answer)
Recognition and management of SSIs Explanation: ***Application of moist sterile dressing + tetanus vaccine***
- This approach is appropriate for a **contaminated, high-risk avulsion wound** to prevent infection and promote healing by secondary intention.
- The patient needs an updated **tetanus vaccine** because his last one was six years ago, and he has a contaminated wound.
*Apposition of wound edges under tension + rifampin*
- **Closing a contaminated wound under tension** is contraindicated as it increases the risk of infection and necrosis.
- **Rifampin is generally not the first-line prophylactic antibiotic** for this type of wound injury and is not needed if the wound has been thoroughly cleaned.
*Surgical treatment with skin flap + ciprofloxacin*
- This is an **overly aggressive initial approach** for an acute, contaminated wound, as the priority is preventing infection before definitive closure or reconstruction.
- **Ciprofloxacin** is not typically the first-choice prophylactic antibiotic for contaminated soft tissue wounds.
*Surgical treatment with skin graft + tetanus vaccine*
- A **skin graft** is a definitive reconstructive procedure and is not indicated as the immediate next step for a fresh, contaminated avulsion wound.
- The wound first needs to be thoroughly cleaned and monitored for infection before considering graft options.
*Tension-free apposition of wound edges + sterile dressing*
- While **tension-free closure** is ideal, this wound is **heavily contaminated with soil and dirt** and has some avulsion, making primary closure risky due to a high infection rate.
- **Allowing the wound to heal by secondary intention** with a moist dressing is safer in this situation.
Recognition and management of SSIs US Medical PG Question 2: A 56-year-old previously healthy woman with no other past medical history is post-operative day one from an open reduction and internal fixation of a fractured right radius and ulna after a motor vehicle accident. What is one of the primary ways of preventing postoperative pneumonia in this patient?
- A. Shallow breathing exercises
- B. Incentive spirometry (Correct Answer)
- C. Outpatient oral antibiotics
- D. Hyperbaric oxygenation
- E. In-hospital intravenous antibiotics
Recognition and management of SSIs Explanation: ***Incentive spirometry***
- **Incentive spirometry** is a cornerstone of postoperative care, actively encouraging patients to take slow, deep breaths. This expands the lungs and prevents the collapse of alveoli, reducing the risk of **atelectasis** and subsequent **pneumonia**.
- Its effectiveness lies in promoting lung aeration and clearing secretions, which are crucial after anesthesia and surgery, especially in patients with reduced mobility or pain.
*Shallow breathing exercises*
- **Shallow breathing** is insufficient for adequate lung expansion and can actually contribute to **atelectasis** and the pooling of secretions in the lungs.
- Effective pulmonary hygiene requires **deep breaths** to maximize alveolar recruitment and prevent respiratory complications.
*Outpatient oral antibiotics*
- **Prophylactic antibiotics** are typically given around the time of surgery to prevent surgical site infections, not primarily to prevent postoperative pneumonia in an outpatient setting.
- Administering antibiotics without a diagnosed infection can lead to **antibiotic resistance** and is not a standard practice for preventing pneumonia unless a specific risk factor or existing infection is identified.
*Hyperbaric oxygenation*
- **Hyperbaric oxygenation** involves breathing 100% oxygen in a pressurized chamber and is used for conditions like **decompression sickness**, non-healing wounds, or severe infections.
- It is not a standard or primary method for preventing postoperative pneumonia, as its mechanism of action is unrelated to common pulmonary hygiene techniques.
*In-hospital intravenous antibiotics*
- While antibiotics can treat pneumonia, their routine, **prophylactic use** intravenously in-hospital solely for preventing postoperative pneumonia is generally unwarranted and can contribute to **antibiotic resistance**.
- Antibiotics are indicated if there is evidence of an active infection, but the primary prevention of pneumonia focuses on mechanical lung expansion and airway clearance.
Recognition and management of SSIs US Medical PG Question 3: Three days after undergoing coronary bypass surgery, a 67-year-old man becomes unresponsive and hypotensive. He is intubated, mechanically ventilated, and a central line is inserted. Vasopressin and noradrenaline infusions are begun. A Foley catheter is placed. Six days later, he has high unrelenting fevers. He is currently receiving noradrenaline via an infusion pump. His temperature is 39.6°C (102.3°F), pulse is 113/min, and blood pressure is 90/50 mm Hg. Examination shows a sternal wound with surrounding erythema; there is no discharge from the wound. Crackles are heard at both lung bases. Cardiac examination shows an S3 gallop. Abdominal examination shows no abnormalities. A Foley catheter is present. His hemoglobin concentration is 10.8 g/dL, leukocyte count is 21,700/mm3, and platelet count is 165,000/mm3. Samples for blood culture are drawn simultaneously from the central line and peripheral IV line. Blood cultures from the central line show coagulase-negative cocci in clusters on the 8th postoperative day, and those from the peripheral venous line show coagulase-negative cocci in clusters on the 10th postoperative day. Which of the following is the most likely diagnosis in this patient?
- A. Central line-associated blood stream infection (Correct Answer)
- B. Catheter-associated urinary tract infection
- C. Surgical site infection
- D. Bowel ischemia
- E. Ventilator-associated pneumonia
Recognition and management of SSIs Explanation: ***Central line-associated blood stream infection***
- The patient exhibits signs of **sepsis** (fever, hypotension, tachycardia) following central line insertion, and **coagulase-negative cocci** (e.g., *Staphylococcus epidermidis*) were isolated from both central and peripheral blood cultures with differential times to positivity, indicating a central line origin.
- The organism isolated, **coagulase-negative cocci**, is a common cause of **central line-associated bloodstream infections** (CLABSI).
*Catheter-associated urinary tract infection*
- While a **Foley catheter** is present, there are no specific signs or symptoms of a **urinary tract infection**, such as dysuria, frequency, or hematuria.
- The microbiology results (coagulase-negative cocci in blood, not urine) do not support a urinary source for the infection.
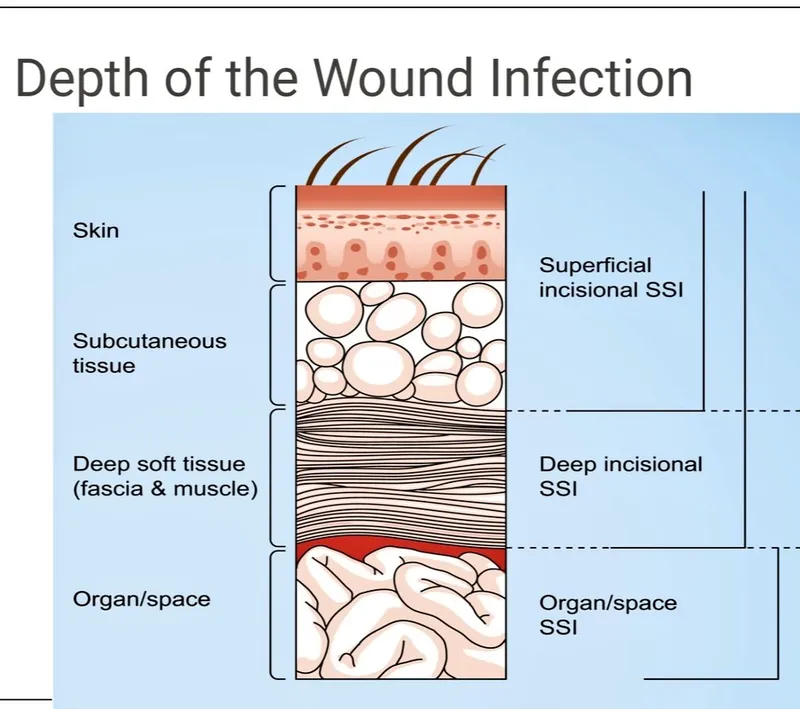
*Surgical site infection*
- There is **erythema** around the sternal wound, suggesting a superficial infection, but no **discharge** or deepening wound involvement is noted.
- A surgical site infection would typically manifest with more prominent localized signs and would be less likely to cause a systemic bloodstream infection with coagulase-negative cocci detected *before* peripheral line cultures.
*Bowel ischemia*
- This condition is often associated with **abdominal pain**, distension, and signs of organ dysfunction.
- The abdominal examination is explicitly stated as normal, making bowel ischemia unlikely.
*Ventilator-associated pneumonia*
- The patient has crackles at lung bases and is mechanically ventilated, but there are no specific findings like new infiltrates on chest imaging or purulent sputum that would strongly indicate **pneumonia**.
- The isolated organism in the blood (coagulase-negative cocci) is not a typical pathogen for ventilator-associated pneumonia, which usually involves Gram-negative rods or *Staphylococcus aureus*.
Recognition and management of SSIs US Medical PG Question 4: A 38-year-old female presents to the emergency room with fevers, fatigue, and anorexia for over a month. Past medical history includes mild mitral valve prolapse. She underwent an uncomplicated tooth extraction approximately 6 weeks ago. Her vital signs include a temperature of 100.8 F, pulse of 83, blood pressure of 110/77, and SpO2 of 97% on room air. On exam, you note a grade III/VI holosystolic murmur at the apex radiating to the axilla as well as several red, painful nodules on her fingers. Which of the following is the next best course of action?
- A. Blood cultures are not needed. Start empiric antibiotics
- B. Start anticoagulation with heparin
- C. Consult cardiothoracic surgery for mitral valve replacement
- D. Obtain blood cultures x3 sites over 24 hours and start antibiotics after culture results are available
- E. Obtain blood cultures x3 sites over 1 hour and start empiric antibiotics (Correct Answer)
Recognition and management of SSIs Explanation: ***Obtain blood cultures x3 sites over 1 hour and start empiric antibiotics***
- The patient's presentation with **fever, fatigue, anorexia, new murmur, and painful finger nodules (Osler's nodes)** after a recent dental procedure strongly suggests **infective endocarditis**. Prompt initiation of **empiric antibiotics** after obtaining adequate blood cultures is crucial to improve outcomes and prevent further complications like septic emboli or valvular damage.
- Obtaining **multiple blood cultures rapidly (e.g., three sets over 1 hour)** from different sites maximizes the chance of isolating the causative organism before antibiotics are given, enabling targeted therapy later, while minimizing delay to treatment.
*Blood cultures are not needed. Start empiric antibiotics*
- **Blood cultures are essential** for diagnosing infective endocarditis, identifying the causative organism, and guiding appropriate antibiotic therapy. Skipping blood cultures could lead to inappropriate antibiotic selection and treatment failure.
- While empiric antibiotics are warranted, they should always be initiated **after blood cultures** have been drawn to avoid sterilizing the blood and making microbial identification difficult.
*Start anticoagulation with heparin*
- **Anticoagulation is generally contraindicated** in infective endocarditis due to the increased risk of hemorrhagic complications, especially in cases of septic emboli to the brain.
- While patients with endocarditis can form vegetations that may embolize, the risks of **bleeding outweigh the benefits** of routine anticoagulation.
*Consult cardiothoracic surgery for mitral valve replacement*
- While **mitral valve prolapse** is a risk factor for endocarditis and severe valvular damage may eventually require surgery, primary management involves **antibiotic therapy**.
- Surgical intervention is typically reserved for cases with **severe valvular regurgitation/stenosis leading to heart failure**, uncontrolled infection despite antibiotics, or recurrent emboli, and is not the immediate next step.
*Obtain blood cultures x3 sites over 24 hours and start antibiotics after culture results are available*
- Waiting for **24 hours to collect blood cultures** would significantly delay the initiation of antibiotics, which is dangerous in a potentially life-threatening infection like endocarditis.
- Delaying antibiotics until **culture results are available** could take several days, leading to worsening infection, organ damage, and increased mortality. **Empiric antibiotics** must be started promptly after initial blood collection.
Recognition and management of SSIs US Medical PG Question 5: A 63-year-old female recovering from a total shoulder arthroplasty completed 6 days ago presents complaining of joint pain in her repaired shoulder. Temperature is 39 degrees Celsius. Physical examination demonstrates erythema and significant tenderness around the incision site. Wound cultures reveal Gram-positive cocci that are resistant to nafcillin. Which of the following organisms is the most likely cause of this patient's condition?
- A. Streptococcus pyogenes
- B. Escherichia coli
- C. Streptococcus viridans
- D. Staphylococcus epidermidis
- E. Staphylococcus aureus (Correct Answer)
Recognition and management of SSIs Explanation: ***Staphylococcus aureus***
- The combination of **post-surgical infection**, **erythema**, and fever with **Gram-positive cocci** that are **nafcillin-resistant** is highly indicative of **Methicillin-Resistant Staphylococcus aureus (MRSA)**.
- *S. aureus* is a common cause of **surgical site infections**, and its resistance to nafcillin implies it is MRSA, a significant clinical concern for its difficulty in treatment.
*Streptococcus pyogenes*
- While *S. pyogenes* is a Gram-positive coccus that can cause skin and soft tissue infections, it is typically **susceptible to penicillin** and related antibiotics like nafcillin, unlike the organism described.
- It is more commonly associated with **streptococcal pharyngitis** or **cellulitis**, and while it can cause severe disease, its resistance profile doesn't match the clinical picture.
*Escherichia coli*
- *E. coli* is a **Gram-negative rod**, not a Gram-positive coccus.
- It is a common cause of **urinary tract infections** and **gastrointestinal infections**, making it an unlikely pathogen for a post-surgical joint infection unless contaminated from a visceral source.
*Streptococcus viridans*
- **Viridans streptococci** are Gram-positive cocci but are typically associated with **endocarditis** or dental infections, especially after poor dental hygiene or procedures.
- They are usually **susceptible to penicillin** and do not typically exhibit nafcillin resistance as the primary feature in a post-arthroplasty infection.
*Staphylococcus epidermidis*
- *S. epidermidis* is a **coagulase-negative Staphylococcus** known for forming **biofilms on prosthetic devices**, leading to chronic, low-grade infections.
- While it can be nafcillin-resistant, the **acute presentation** with fever and significant inflammation suggests a more virulent pathogen like *S. aureus*, as *S. epidermidis* infections are typically indolent.
Recognition and management of SSIs US Medical PG Question 6: A 32-year-old woman is supposed to undergo tooth extraction surgery. Physical examination is unremarkable, and she has a blood pressure of 126/84 mm Hg and regular pulse of 72/min. She takes no medications. Which of the following cardiac conditions would warrant antibiotic prophylaxis to prevent infective endocarditis in this patient?
- A. Hypertrophic obstructive cardiomyopathy (HOCM)
- B. Mitral regurgitation
- C. Past history of infective endocarditis (Correct Answer)
- D. Ventricular septal defect (VSD)
- E. Implantable cardioverter defibrillator (ICD)
Recognition and management of SSIs Explanation: ***Past history of infective endocarditis***
- A **history of infective endocarditis** is a definite indication for **antibiotic prophylaxis** before dental procedures that involve manipulation of gingival tissue, periapical region of teeth, or perforation of the oral mucosa due to the high risk of recurrence.
- This condition creates a predisposition to subsequent episodes of endocarditis, even with minor bacteremia.
*Hypertrophic obstructive cardiomyopathy (HOCM)*
- While HOCM is a significant cardiac condition, it is **no longer an indication** for routine infective endocarditis prophylaxis in the absence of other high-risk features like a prosthetic valve.
- Current guidelines have narrowed the criteria for prophylaxis due to the low absolute risk and potential for side effects from antibiotics.
*Mitral regurgitation*
- **Mitral valve regurgitation**, in the absence of a prosthetic valve or a previous history of endocarditis, generally **does not warrant antibiotic prophylaxis** for routine dental procedures.
- Only specific types of valvular heart disease with high risk (e.g., prosthetic valves, certain congenital heart diseases) require prophylaxis.
*Ventricular septal defect (VSD)*
- **Most ventricular septal defects do not require prophylaxis**. Only **unrepaired cyanotic VSD** or **repaired VSD with residual defects adjacent to prosthetic material** would warrant prophylaxis.
- Completely repaired VSDs without residual defects do not require prophylaxis after the initial 6 months post-repair.
- In this case, with an unremarkable physical examination and normal vital signs, there is no indication of cyanotic heart disease.
*Implantable cardioverter defibrillator (ICD)*
- An **implantable cardioverter defibrillator (ICD)** itself is a device and does not inherently increase the risk for infective endocarditis to warrant prophylaxis for dental procedures.
- The risk of infection is primarily associated with the device insertion procedure itself, not with subsequent dental interventions.
Recognition and management of SSIs US Medical PG Question 7: Three days after being admitted to the hospital because of a fall from the roof of a two-story building, a 27-year-old man is being monitored in the intensive care unit. On arrival, the patient was somnolent and not oriented to person, place, or time. A CT scan of the head showed an epidural hemorrhage that was 45 cm3 in size and a midline shift of 7 mm. Emergency surgery was performed with craniotomy and hematoma evacuation on the day of admission. Perioperatively, a bleeding vessel was identified and ligated. Postoperatively, the patient was transferred to the intensive care unit and placed on a ventilator. His temperature is 37°C (98.6°F), pulse is 67/min, and blood pressure is 117/78 mm Hg. The ventilator is set at a FiO2 of 55%, tidal volume of 520 mL, and positive end-expiratory pressure of 5.0 cm H2O. In addition to intravenous administration of fluids, which of the following is the most appropriate next step in managing this patient's nutrition?
- A. Enteral feeding via nasogastric tube (Correct Answer)
- B. Oral feeding
- C. Keep patient NPO
- D. Total parenteral nutrition
- E. Enteral feeding using a percutaneous endoscopic gastrostomy (PEG) tube
Recognition and management of SSIs Explanation: ***Enteral feeding via nasogastric tube***
- This patient has been **somnolent** and on a ventilator for 3 days after a significant head injury, indicating a prolonged period without oral intake and an inability to protect his airway for oral feeding. **Early enteral nutrition** via a nasogastric tube is preferred in critically ill patients, especially those with head injuries, as it helps maintain gut integrity and reduces complications compared to parenteral nutrition.
- The patient's **hemodynamic stability** (blood pressure and pulse are within a reasonable range for a ventilated patient) suggests he can tolerate enteral feeding, and there are no signs of gut ischemia or ileus that would contraindicate it.
*Enteral feeding using a percutaneous endoscopic gastrostomy (PEG) tube*
- While a PEG tube provides enteral nutrition, it is typically reserved for patients requiring **long-term enteral support** (usually more than 4-6 weeks) or those who cannot tolerate a nasogastric tube.
- Given that it has only been 3 days post-injury, a **less invasive method** like a nasogastric tube is initially preferred.
*Oral feeding*
- The patient is described as **somnolent** and on a ventilator, meaning he is not awake enough or able to protect his airway to safely receive oral feeding.
- Attempting oral feeding in this state carries a high risk of **aspiration pneumonia**.
*Keep patient NPO*
- Keeping the patient NPO (nil per os) for an extended period in critical illness is associated with several negative outcomes, including **gut mucosal atrophy, increased infection risk**, and poorer clinical outcomes.
- After 3 days, initiating nutritional support is crucial to prevent these complications.
*Total parenteral nutrition*
- **Total parenteral nutrition (TPN)** is generally considered a last resort when the gastrointestinal tract is non-functional or enteral feeding is contraindicated.
- TPN is associated with a **higher risk of complications**, such as central line infections, liver dysfunction, and metabolic disturbances, compared to enteral feeding.
Recognition and management of SSIs US Medical PG Question 8: A 65-year-old woman comes to the physician because of progressive weight loss for 3 months. Physical examination shows jaundice and a nontender, palpable gallbladder. A CT scan of the abdomen shows an ill-defined mass in the pancreatic head. She is scheduled for surgery to resect the pancreatic head, distal stomach, duodenum, early jejunum, gallbladder, and common bile duct and anastomose the jejunum to the remaining stomach, pancreas, and bile duct. Following surgery, this patient is at the greatest risk for which of the following?
- A. Wide-based gait
- B. Calcium oxalate kidney stones
- C. Microcytic anemia (Correct Answer)
- D. Increased bile production
- E. Hypercoagulable state
Recognition and management of SSIs Explanation: ***Microcytic anemia***
- The surgical procedure described is a **Whipple procedure**, which involves partial gastrectomy and duodenectomy. This significant alteration to the upper GI tract can lead to **iron malabsorption**, as iron is primarily absorbed in the duodenum and proximal jejunum, and gastric acid is crucial for converting dietary iron to its absorbable ferrous form.
- **Iron deficiency** is the most common cause of **microcytic anemia**, characterized by small, pale red blood cells, due to impaired hemoglobin synthesis as a result of insufficient iron availability for the heme component.
*Wide-based gait*
- A **wide-based gait** is typically associated with **ataxia** or conditions affecting cerebellar function or proprioception, which are not direct complications of a Whipple procedure.
- While nutritional deficiencies can occur post-surgery, a wide-based gait specifically points to neurological impairment rather than postsurgical metabolic issues.
*Calcium oxalate kidney stones*
- **Calcium oxalate kidney stones** are often associated with conditions causing **hypercalciuria** or malabsorption of fat, which leads to increased oxalate absorption in the colon. While fat malabsorption can occur after a Whipple due to pancreatic insufficiency, dietary oxalate intake and hydration status are generally more significant determinants of stone formation.
- The surgery itself does not directly increase the risk for calcium oxalate kidney stones more than other listed complications.
*Increased bile production*
- A Whipple procedure involves the removal of the **gallbladder** and rerouting of the **bile duct** directly into the jejunum. This does not lead to increased bile production, but rather a different regulation and flow of bile.
- In fact, the absence of the gallbladder means there is no storage for bile, leading to a continuous, unregulated flow of bile into the small intestine, potentially contributing to maldigestion or diarrhea, but not "increased production."
*Hypercoagulable state*
- While surgery, including a Whipple procedure, can transiently increase the risk of a **hypercoagulable state** (e.g., deep vein thrombosis, pulmonary embolism) in the immediate postoperative period due to immobility and tissue injury, this risk is generally mitigated with prophylactic anticoagulation.
- The question asks about the **greatest risk** post-surgery, and long-term complications related to altered anatomy and malabsorption, such as microcytic anemia, are more direct and sustained consequences unique to the extent of the resection.
Recognition and management of SSIs US Medical PG Question 9: A 55-year-old woman is brought to the emergency department due to sudden onset retrosternal chest pain. An ECG shows ST-segment elevation. A diagnosis of myocardial infarction is made and later confirmed by elevated levels of troponin I. The patient is sent to the cardiac catheter laboratory where she undergoes percutaneous catheterization. She has 2 occluded vessels in the heart and undergoes a percutaneous coronary intervention to place 2 stents in her coronary arteries. Blood flow is successfully restored in the affected arteries. The patient complains of flank pain on post-procedure evaluation a few hours later. A significant drop in hematocrit is observed, as well as a drop in her blood pressure to 90/60 mm Hg. Physical examination reveals extensive ecchymoses in the flanks and loin as seen in the provided image. Which of the following conditions is this patient most likely experiencing?
- A. Retroperitoneal hemorrhage (Correct Answer)
- B. Fat embolism
- C. Adrenal hemorrhage
- D. Patent ductus arteriosus
- E. Ventricular septal defect
Recognition and management of SSIs Explanation: ***Retroperitoneal hemorrhage***
- The sudden onset of **flank pain**, significant drop in **hematocrit** and **blood pressure**, and the presence of **extensive ecchymoses in the flanks and loin (Grey Turner's sign)** following a cardiac catheterization via femoral artery access are highly suggestive of a **retroperitoneal hemorrhage**.
- **Retroperitoneal hemorrhage** is a known complication of femoral artery puncture, where the puncture site bleeds into the retroperitoneal space, causing symptoms like pain, hypovolemia, and the characteristic flank ecchymoses.
- This is an acute post-procedural complication that requires immediate recognition and management.
*Fat embolism*
- Fat embolism syndrome typically presents with a **triad of respiratory distress**, **neurological symptoms**, and a **petechial rash**, which are not described in this patient.
- While it can occur after trauma or orthopedic procedures, it is not a direct complication of cardiac catheterization and stent placement in this manner.
*Adrenal hemorrhage*
- Adrenal hemorrhage can cause flank pain and hypovolemia, but it is typically associated with **severe stress, sepsis, or anticoagulant use**, and usually presents with symptoms of **adrenal insufficiency**.
- The context of a recent femoral artery puncture and the characteristic ecchymoses point away from isolated adrenal hemorrhage as the primary cause.
*Patent ductus arteriosus*
- **Patent ductus arteriosus (PDA)** is a congenital heart defect characterized by a persistent connection between the aorta and pulmonary artery, leading to a **left-to-right shunt**. It is *not* an acute complication of cardiac catheterization in an adult.
- Symptoms of PDA in adults typically include **dyspnea, fatigue, and a continuous murmur**, none of which are presented in this acute post-procedural scenario.
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** is a **hole in the septum** separating the ventricles, often congenital, and can cause a shunt and heart failure. It is *not* an acute complication of cardiac catheterization and stent placement.
- A VSD would typically present with a **loud harsh holosystolic murmur** and signs of heart failure (if significant), which are not discussed in this acute post-procedure presentation following a chest pain event.
Recognition and management of SSIs US Medical PG Question 10: Twelve days after undergoing total pancreatectomy for chronic pancreatitis, a 62-year-old woman notices oozing from her abdominal wound. She first noticed fluid draining 8 hours ago. Her postoperative course has been complicated by persistent hypotension requiring intravenous fluids and decreased ability to tolerate food. She has type 1 diabetes mellitus and glaucoma. The patient smoked one pack of cigarettes daily for 30 years, but quit 2 years ago. She drank a pint of vodka every day starting at age 20 and quit when she was 35 years old. Her current medications include subcutaneous insulin and timolol eye drops. She appears comfortable. Her temperature is 37°C (98.6°F), pulse is 95/min, and blood pressure is 104/78 mm Hg. The abdomen is soft and mildly tender to palpation. There is a 12-cm vertical wound beginning in the epigastrium and extending caudally. 25 mL of a viscous, dark green substance is draining from the middle of the wound. There is a small amount of dried fluid on the patient's hospital gown. The wound edges are nonerythematous. There is no pus draining from the wound. Laboratory studies show:
Hematocrit 38%
Leukocyte count 8,000/mm3
Serum
Na+ 135 mEq/L
Cl- 100 mEq/L
K+ 3.4 mEq/L
HCO3- 23 mEq/L
Urea nitrogen 13 mg/dL
Creatinine 1.1 mg/dL
Glucose 190 mg/dL
Which of the following is the most appropriate next step in management?
- A. Intravenous antibiotic therapy
- B. Surgical exploration of the abdomen
- C. Total parenteral nutrition and ostomy pouch (Correct Answer)
- D. Wound debridement and irrigation
- E. Oral food intake and intravenous fluid administration
Recognition and management of SSIs Explanation: ***Total parenteral nutrition and ostomy pouch***
- The patient, having undergone total pancreatectomy, is experiencing an **enterocutaneous fistula** from an anastomotic leak (e.g., gastrojejunostomy or choledochojejunostomy), presenting as viscid, dark green drainage from the wound.
- An **ostomy pouch** will protect the skin from digestive enzymes and allow quantification of output, while **total parenteral nutrition (TPN)** provides bowel rest, promoting spontaneous healing of the fistula.
- This conservative approach is appropriate given the patient's **hemodynamic stability** and **absence of signs of sepsis or peritonitis**.
*Intravenous antibiotic therapy*
- While infection is a concern, there are **no clear signs of systemic infection** (e.g., fever, leukocytosis, erythema, purulent drainage) in this patient.
- **Antibiotics alone** would not address the underlying anatomical leak and its resulting drainage.
*Surgical exploration of the abdomen*
- **Surgical exploration** is typically reserved for cases with signs of **sepsis**, **peritonitis**, **uncontrolled leak**, or failure of conservative management.
- Given the patient is hemodynamically stable without signs of severe infection or acute abdomen, a **conservative approach** is preferred initially.
*Wound debridement and irrigation*
- **Wound care** is important, but debridement and irrigation alone will **not stop the internal leakage** of enteric content from the gastrointestinal tract.
- The primary issue is an internal fistula, not a localized wound infection requiring debridement.
*Oral food intake and intravenous fluid administration*
- **Oral food intake** would exacerbate the fistula by stimulating digestive secretions and increasing enteric output, hindering natural healing.
- While **intravenous fluids** are used for hydration and electrolyte balance, they do not address the fistula, and **bowel rest is crucial** for spontaneous closure.
More Recognition and management of SSIs US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.