Postoperative respiratory care US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Postoperative respiratory care. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Postoperative respiratory care US Medical PG Question 1: A 56-year-old previously healthy woman with no other past medical history is post-operative day one from an open reduction and internal fixation of a fractured right radius and ulna after a motor vehicle accident. What is one of the primary ways of preventing postoperative pneumonia in this patient?
- A. Shallow breathing exercises
- B. Incentive spirometry (Correct Answer)
- C. Outpatient oral antibiotics
- D. Hyperbaric oxygenation
- E. In-hospital intravenous antibiotics
Postoperative respiratory care Explanation: ***Incentive spirometry***
- **Incentive spirometry** is a cornerstone of postoperative care, actively encouraging patients to take slow, deep breaths. This expands the lungs and prevents the collapse of alveoli, reducing the risk of **atelectasis** and subsequent **pneumonia**.
- Its effectiveness lies in promoting lung aeration and clearing secretions, which are crucial after anesthesia and surgery, especially in patients with reduced mobility or pain.
*Shallow breathing exercises*
- **Shallow breathing** is insufficient for adequate lung expansion and can actually contribute to **atelectasis** and the pooling of secretions in the lungs.
- Effective pulmonary hygiene requires **deep breaths** to maximize alveolar recruitment and prevent respiratory complications.
*Outpatient oral antibiotics*
- **Prophylactic antibiotics** are typically given around the time of surgery to prevent surgical site infections, not primarily to prevent postoperative pneumonia in an outpatient setting.
- Administering antibiotics without a diagnosed infection can lead to **antibiotic resistance** and is not a standard practice for preventing pneumonia unless a specific risk factor or existing infection is identified.
*Hyperbaric oxygenation*
- **Hyperbaric oxygenation** involves breathing 100% oxygen in a pressurized chamber and is used for conditions like **decompression sickness**, non-healing wounds, or severe infections.
- It is not a standard or primary method for preventing postoperative pneumonia, as its mechanism of action is unrelated to common pulmonary hygiene techniques.
*In-hospital intravenous antibiotics*
- While antibiotics can treat pneumonia, their routine, **prophylactic use** intravenously in-hospital solely for preventing postoperative pneumonia is generally unwarranted and can contribute to **antibiotic resistance**.
- Antibiotics are indicated if there is evidence of an active infection, but the primary prevention of pneumonia focuses on mechanical lung expansion and airway clearance.
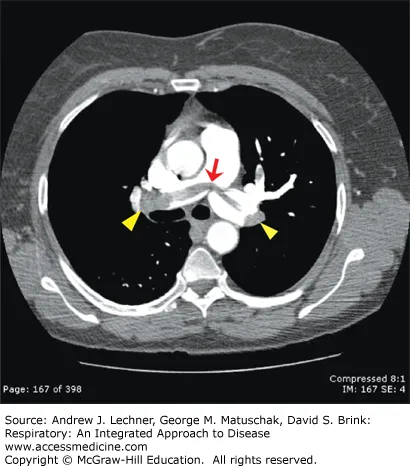
Postoperative respiratory care US Medical PG Question 2: A 36-year-old man presents to the physician with difficulty in breathing for 3 hours. There is no history of chest pain, cough or palpitation. He is a chronic smoker and underwent elective cholecystectomy one month back. There is no history of chronic or recurrent cough, wheezing or breathlessness. His temperature is 38.2°C (100.8°F), pulse is 108/min, blood pressure is 124/80 mm Hg, and respirations are 25/min. His arterial oxygen saturation is 98% in room air as shown by pulse oximetry. After a detailed physical examination, the physician orders a plasma D-dimer level, which was elevated. A contrast-enhanced computed tomography (CT) of the chest shows a filling defect in a segmental pulmonary artery on the left side. Which of the following signs is most likely to have been observed by the physician during the physical examination of this patient’s chest?
- A. Pleural friction rub
- B. Bilateral wheezing
- C. Systolic murmur at the left sternal border
- D. Localized rales (Correct Answer)
- E. S3 gallop
Postoperative respiratory care Explanation: ***Localized rales***
- The patient's presentation with **sudden onset dyspnea**, risk factors (recent surgery, smoking), elevated D-dimer, and a CT scan showing a filling defect in the pulmonary artery strongly points to a **pulmonary embolism (PE)**.
- While PE often presents with normal lung auscultation, localized rales or crackles can be heard if there is an associated **pulmonary infarction** or local inflammation.
*Pleural friction rub*
- A **pleural friction rub** indicates inflammation of the pleura, which can occur in PE if the infarct involves the pleural surface.
- However, it is a less common finding than localized rales and is more characteristic of conditions like pleurisy or pneumonia.
*Bilateral wheezing*
- **Bilateral wheezing** is typically associated with diffuse airway obstruction, as seen in asthma or chronic obstructive pulmonary disease (COPD).
- This patient has no history of chronic respiratory conditions and the presentation is acute dyspnea, making diffuse airway obstruction less likely.
*Systolic murmur at the left sternal border*
- A **systolic murmur at the left sternal border** can be indicative of tricuspid regurgitation, often seen in the setting of **pulmonary hypertension** and right heart strain associated with a massive PE.
- However, with a stable blood pressure and moderate heart rate, severe right heart strain leading to a murmur is less likely in this scenario of a segmental PE.
*S3 gallop*
- An **S3 gallop** is a low-pitched sound heard during early diastole, often indicating **volume overload** or **ventricular dysfunction**.
- In the context of PE, an S3 often suggests significant **right ventricular dysfunction** due to acute pressure overload; this is more common with large or massive PEs causing hemodynamic instability, which is not indicated here.
Postoperative respiratory care US Medical PG Question 3: A 23-year-old woman with no significant past medical history currently on oral contraceptive pills presents to the emergency department with pleuritic chest pain. She states that it started today. Yesterday she had a trip and returned via plane. Her temperature is 98°F (36.7°C), blood pressure is 117/66 mmHg, pulse is 105/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam reveals tachycardia, a normal S1 and S2, and clear breath sounds. The patient’s lower extremities are non-tender and symmetric. Chest pain is not reproducible with position changes or palpation but is worsened with deep breaths. Which of the following is the most appropriate next test for this patient?
- A. D-dimer
- B. Ultrasound of the lower extremities
- C. Ventilation-perfusion scan
- D. CT angiogram (Correct Answer)
- E. Chest radiograph
Postoperative respiratory care Explanation: ***CT angiogram***
- This patient has **HIGH probability for pulmonary embolism (PE)** based on **Wells criteria**: oral contraceptive use (hypercoagulable state), recent long-haul flight (immobilization), pleuritic chest pain, and tachycardia (pulse 105/min).
- With a **Wells score ≥4**, the appropriate next step is **definitive imaging with CT pulmonary angiography (CTPA)**, which is the **gold standard** for diagnosing PE.
- **D-dimer should be bypassed** in high-probability cases, as a negative result would not adequately rule out PE, and a positive result (expected in high-probability patients) would require CTPA anyway.
- CTPA provides direct visualization of pulmonary arterial thrombi and can also identify alternative diagnoses.
*D-dimer*
- D-dimer is appropriate for **low to moderate probability PE** (Wells score <4) where a negative result can safely rule out PE and avoid unnecessary imaging.
- In this **high-probability case**, D-dimer is likely to be positive regardless, making it an unnecessary intermediate step that delays definitive diagnosis.
- Using D-dimer in high-probability patients can lead to false reassurance if negative or simply confirms the need for CTPA if positive.
*Ultrasound of the lower extremities*
- Lower extremity ultrasound diagnoses **deep vein thrombosis (DVT)**, not PE directly.
- While finding DVT in a patient with suspected PE would support anticoagulation, **absence of DVT does not rule out PE**, as thrombi may have already embolized.
- This would delay appropriate diagnosis and is not the most direct test for suspected PE.
*Ventilation-perfusion scan*
- V/Q scan is reserved for patients with **contraindications to CT contrast** (severe renal insufficiency, contrast allergy) or pregnant patients where radiation exposure should be minimized.
- This young patient has no mentioned contraindications to contrast-enhanced CT.
- V/Q scanning is less specific than CTPA and often yields indeterminate results.
*Chest radiograph*
- Chest X-ray is often **normal in PE** or shows non-specific findings (Westermark sign, Hampton's hump are rare).
- While it may help exclude alternative diagnoses like pneumothorax or pneumonia, it cannot definitively diagnose or rule out PE.
- In a patient with high clinical suspicion for PE, delaying CTPA to obtain a chest X-ray is not optimal management.
Postoperative respiratory care US Medical PG Question 4: A patient is hospitalized for pneumonia. Gram-positive cocci in clusters are seen on sputum gram stain. Which of the following clinical scenarios is most commonly associated with this form of pneumonia?
- A. Elderly patient who has trouble swallowing and poor dentition
- B. An alcoholic with evidence of empyema and "currant jelly sputum"
- C. An otherwise healthy young adult with a week of mild fatigue, chills, and cough
- D. Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness (Correct Answer)
- E. HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity
Postoperative respiratory care Explanation: ***Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness***
- Gram-positive cocci in clusters suggests **Staphylococcus aureus**, which is a common cause of secondary bacterial pneumonia, often following **viral illnesses** (e.g., influenza).
- This scenario represents a classic presentation of **secondary bacterial pneumonia**, where the initial viral infection compromises the respiratory defenses, allowing bacterial superinfection.
*Elderly patient who has trouble swallowing and poor dentition*
- This scenario points towards **aspiration pneumonia**, often caused by a **polymicrobial infection** that includes oral anaerobes, not typically dominated by Gram-positive cocci in clusters.
- While *S. aureus* can cause aspiration pneumonia, the primary concern in this context would be **anaerobic bacteria**, given the aspiration risk factors.
*An alcoholic with evidence of empyema and \"currant jelly sputum\"*
- This description is highly suggestive of **Klebsiella pneumoniae** infection, which typically presents with thick, gelatinous, and often **blood-tinged sputum**.
- **Klebsiella** is a Gram-negative rod, not Gram-positive cocci in clusters.
*An otherwise healthy young adult with a week of mild fatigue, chills, and cough*
- This presentation is more consistent with **atypical pneumonia** caused by organisms like **Mycoplasma pneumoniae** or **Chlamydophila pneumoniae**, which would not show Gram-positive cocci in clusters on sputum stain.
- **Streptococcus pneumoniae** (Gram-positive cocci in chains) can also cause community-acquired pneumonia in otherwise healthy individuals, but the "clusters" indicate **Staphylococcus aureus**.
*HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity*
- This clinical picture strongly suggests **Pneumocystis jirovecii pneumonia (PJP)**, which is common in severely immunocompromised HIV patients.
- *P. jirovecii* is a fungus and would not be seen as Gram-positive cocci in clusters on a routine Gram stain.
Postoperative respiratory care US Medical PG Question 5: A 51-year-old man presents to his physician’s office with a persistent fever that started a week ago. He says that his temperature ranges between 37.8–39.1°C (100–102.5°F). He has also had a persistent cough productive of foul-smelling sputum. There is no significant medical history to report, but he does mention that he has been suffering from dental caries for the last month. He has been meaning to see his dentist but has been too busy to do so. His blood pressure is 120/70 mm Hg, the respirations are 18/min, and the temperature is 38.5°C (101.3°F). His oxygen saturation is 90% on room air. On examination, he has decreased breath sounds in his right lung field with the presence of soft inspiratory crackles. He is sent to the laboratory for sputum analysis and chest imaging. Based on his history and physical examination, which of the following would be the next best step in the management of this patient?
- A. Bronchoscopy
- B. Surgical drainage
- C. Hospital admission (Correct Answer)
- D. Metronidazole
- E. Clindamycin
Postoperative respiratory care Explanation: ***Hospital admission***
- This patient presents with signs and symptoms suggestive of **aspiration pneumonia** with possible **lung abscess formation**, indicated by persistent fever, foul-smelling sputum, decreased breath sounds, and a history of dental caries. His **low oxygen saturation (90% on room air)** is a significant finding requiring close monitoring and immediate intervention in an inpatient setting.
- Given the severity of his respiratory distress and the potential for rapid deterioration, **hospital admission** is necessary for intravenous antibiotics, respiratory support, and further diagnostic workup, such as a chest CT scan to confirm a lung abscess.
*Bronchoscopy*
- While bronchoscopy can be used for diagnosis and drainage of a lung abscess, it is typically performed *after* initial stabilization and empiric antibiotic therapy in a hospitalized patient.
- It is not the *immediate* next best step given the patient's acute respiratory compromise.
*Surgical drainage*
- Surgical drainage is a more invasive procedure and is reserved for cases where medical management with antibiotics fails, or when there is a very large or complicated abscess.
- It is not the initial treatment strategy for a suspected lung abscess.
*Metronidazole*
- Metronidazole is an antibiotic that covers anaerobic bacteria, which are commonly implicated in aspiration pneumonia and lung abscesses.
- However, it is usually used in combination with other antibiotics (e.g., a beta-lactam) and would be initiated *after* hospital admission and establishment of IV access.
*Clindamycin*
- Clindamycin is an effective antibiotic against anaerobic bacteria and is a common choice for lung abscesses.
- Similar to metronidazole, it would be administered *after* hospital admission as part of the treatment regimen, not as the immediate next step in management.
Postoperative respiratory care US Medical PG Question 6: A 63-year-old man undergoes workup for nocturnal dyspnea and what he describes as a "choking" sensation while sleeping. He also endorses fatigue and dyspnea on exertion. Physical exam reveals a normal S1, loud P2, and a neck circumference of 17 inches (43 cm) (normal < 14 inches (< 35 cm)). His temperature is 98.8°F (37°C), blood pressure is 128/82 mmHg, pulse is 86/min, and respirations are 19/min. He undergoes spirometry, which is unrevealing, and polysomnography, which shows 16 hypopneic and apneic events per hour. Mean pulmonary arterial pressure is 30 mmHg. Which of the following complications is this patient most at risk for?
- A. Left ventricular failure
- B. Right ventricular failure (Correct Answer)
- C. Pulmonary embolism
- D. Aspiration pneumonia
- E. Chronic obstructive pulmonary disease
Postoperative respiratory care Explanation: ***Right ventricular failure***
- The patient's symptoms (nocturnal dyspnea, choking sensation, fatigue, exertional dyspnea), risk factors (large neck circumference), and polysomnography results (16 hypopneic/apneic events/hour) are consistent with **obstructive sleep apnea (OSA)**.
- OSA leads to **chronic intermittent hypoxia** and hypercapnia, causing **pulmonary vasoconstriction** and increased pulmonary arterial pressure (mean PAP 30 mmHg), which can result in **pulmonary hypertension** and eventually **right ventricular failure**.
*Left ventricular failure*
- While OSA can exacerbate cardiovascular conditions, the primary cardiac complication directly resulting from ongoing pulmonary hypertension due to OSA is typically right-sided, not primarily left-sided, failure.
- There are no specific findings in the description (e.g., S3 gallop, crackles) that strongly point to left ventricular dysfunction as the most immediate and direct complication.
*Pulmonary embolism*
- Although obesity (suggested by large neck circumference) is a risk factor for pulmonary embolism, there are no acute symptoms (e.g., sudden onset dyspnea, pleuritic chest pain, hemoptysis) or signs (e.g., tachycardia, hypoxemia) to suggest a pulmonary embolism.
- The patient's symptoms are chronic and related to sleep-disordered breathing and pulmonary hypertension.
*Aspiration pneumonia*
- While a "choking" sensation could potentially lead to aspiration, there's no evidence of infection (e.g., fever, productive cough, crackles) or recurrent aspiration events.
- The primary respiratory pathology is clearly defined by the polysomnography and elevated pulmonary pressures.
*Chronic obstructive pulmonary disease*
- Spirometry was reported as "unrevealing," which rules out significant airflow limitation characteristic of COPD.
- The patient's symptoms are more indicative of sleep-disordered breathing and its cardiovascular consequences rather than an intrinsic obstructive lung disease like COPD.
Postoperative respiratory care US Medical PG Question 7: A 68-year-old man is brought to the emergency department because of fever, progressive weakness, and cough for the past five days. He experienced a similar episode 2 months ago, for which he was hospitalized for 10 days while visiting his son in Russia. He states that he has never fully recovered from that episode. He felt much better after being treated with antibiotics, but he still coughs often during meals. He sometimes also coughs up undigested food after eating. For the last 5 days, his coughing has become more frequent and productive of yellowish-green sputum. He takes hydrochlorothiazide for hypertension and pantoprazole for the retrosternal discomfort that he often experiences while eating. He has smoked half a pack of cigarettes daily for the last 30 years and drinks one shot of vodka every day. The patient appears thin. His temperature is 40.1°C (104.2°F), pulse is 118/min, respirations are 22/min, and blood pressure is 125/90 mm Hg. Auscultation of the lungs shows right basal crackles. There is dullness on percussion at the right lung base. The remainder of the physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 15.4 g/dL
Leukocyte count 17,000/mm3
Platelet count 350,000/mm3
Na+ 139 mEq/L
K+
4.6 mEq/L
Cl- 102 mEq/L
HCO3- 25 mEq/L
Urea Nitrogen 16 mg/dL
Creatinine 1.3 mg/dL
An x-ray of the chest shows a right lower lobe infiltrate. Which of the following is the most likely explanation for this patient's symptoms?
- A. Weak tone of the lower esophageal sphincter
- B. Unrestricted growth of pneumocytes with invasion of the surrounding tissue
- C. Uncoordinated contractions of the esophagus
- D. Formation of a tissue cavity containing necrotic debris
- E. Outpouching of the hypopharynx (Correct Answer)
Postoperative respiratory care Explanation: ***Outpouching of the hypopharynx***
- The patient's history of coughing up undigested food and coughing during meals suggests **dysphagia** and potential **aspiration**, which can be caused by a **Zenker's diverticulum** (an outpouching of the hypopharynx).
- This condition creates a pouch that can trap food, leading to regurgitation and repeated aspiration pneumonia, as evidenced by his recurrent pneumonia and current symptoms.
- Zenker's diverticulum is the **underlying explanation** that accounts for *all* of this patient's symptoms: the regurgitation of undigested food, dysphagia, and recurrent aspiration pneumonia.
*Weak tone of the lower esophageal sphincter*
- A weak lower esophageal sphincter (LES) primarily causes **gastroesophageal reflux disease (GERD)**, often associated with heartburn and regurgitation of stomach contents, not undigested food.
- While GERD can cause aspiration, the coughing up of *undigested food* is more indicative of a proximal esophageal issue or pharyngeal problem.
*Unrestricted growth of pneumocytes with invasion of the surrounding tissue*
- This describes **lung cancer**, which can present with cough, weight loss, and recurrent pneumonia due to bronchial obstruction.
- However, the symptom of coughing up *undigested food* is not typical of primary lung malignancy, and the history strongly points to a swallowing disorder.
*Uncoordinated contractions of the esophagus*
- This refers to esophageal motility disorders like **achalasia** or **diffuse esophageal spasm**, which can cause dysphagia and regurgitation.
- While these can lead to aspiration, the specific complaint of coughing up *undigested food* *after eating* is more characteristic of a pharyngeal pouch (Zenker's diverticulum) rather than general esophageal dysmotility.
*Formation of a tissue cavity containing necrotic debris*
- This describes a **lung abscess**, which is a possible *complication* of aspiration pneumonia, accounting for the fever, productive cough, and infiltrate.
- However, the question asks for the **most likely explanation** for this patient's symptoms—a lung abscess is a *sequela* of aspiration, not the *underlying cause* of the repeated aspiration events.
- It does not explain the pathognomonic finding of coughing up undigested food after eating, which points to Zenker's diverticulum as the root cause.
Postoperative respiratory care US Medical PG Question 8: A 19-year-old man is brought to the emergency department 35 minutes after being involved in a high-speed motor vehicle collision. On arrival, he is alert, has mild chest pain, and minimal shortness of breath. He has one episode of vomiting in the hospital. His temperature is 37.3°C (99.1°F), pulse is 108/min, respirations are 23/min, and blood pressure is 90/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. Examination shows multiple abrasions over his trunk and right upper extremity. There are coarse breath sounds over the right lung base. Cardiac examination shows no murmurs, rubs, or gallop. Infusion of 0.9% saline is begun. He subsequently develops increasing shortness of breath. Arterial blood gas analysis on 60% oxygen shows:
pH 7.36
pCO2 39 mm Hg
pO2 68 mm Hg
HCO3- 18 mEq/L
O2 saturation 81%
An x-ray of the chest shows patchy, irregular infiltrates over the right lung fields. Which of the following is the most likely diagnosis?
- A. Pneumothorax
- B. Pulmonary contusion (Correct Answer)
- C. Aspiration pneumonia
- D. Acute respiratory distress syndrome
- E. Pulmonary embolism
Postoperative respiratory care Explanation: ***Pulmonary contusion***
- The patient's presentation with **hypoxia**, increasing shortness of breath after a high-speed motor vehicle collision, and **patchy, irregular infiltrates** on chest x-ray despite initial hydration, are highly suggestive of **pulmonary contusion**.
- The coarse breath sounds over the right lung base further support the presence of parenchymal injury and hemorrhage in the lung tissue.
*Pneumothorax*
- While a pneumothorax is common after trauma, the chest x-ray would typically show a **collapsed lung** and **absence of lung markings** in the affected area, which is not described.
- The presence of coarse breath sounds suggests air entry, not a complete absence due to collapsed lung.
*Aspiration pneumonia*
- Although the patient had one episode of vomiting, **aspiration pneumonia** typically develops hours to days after aspiration, presenting with fever and signs of infection.
- The acute onset of symptoms within minutes of trauma and the lack of fever make aspiration pneumonia less likely as the primary diagnosis immediately following the accident.
*Acute respiratory distress syndrome*
- **Acute respiratory distress syndrome (ARDS)** is a severe inflammatory lung injury that typically develops **24 to 72 hours** after an initial insult, not immediately.
- While the patient has hypoxia, the diffuse bilateral infiltrates characteristic of ARDS are not seen, and his symptoms are too acute for ARDS to be the primary cause at 35 minutes post-injury.
*Pulmonary embolism*
- A **pulmonary embolism** would typically present with sudden onset of shortness of breath and pleuritic chest pain, often without significant findings on chest x-ray or presenting with a **wedge-shaped infiltrate**.
- Given the direct chest trauma and immediate onset of respiratory compromise, a pulmonary contusion is a more direct and acute consequence.
Postoperative respiratory care US Medical PG Question 9: A 32-year-old man is brought to the emergency department 15 minutes after falling 7 feet onto a flat-top wooden post. On arrival, he is in severe pain and breathing rapidly. His pulse is 135/min, respirations are 30/min, and blood pressure is 80/40 mm Hg. There is an impact wound in the left fourth intercostal space at the midaxillary line. Auscultation shows tracheal deviation to the right and absent breath sounds over the left lung. There is dullness to percussion over the left chest. Neck veins are flat. Cardiac examination shows no abnormalities. Two large-bore intravenous catheters are placed and intravenous fluid resuscitation is begun. Which of the following is the most likely diagnosis?
- A. Bronchial rupture
- B. Cardiac tamponade
- C. Flail chest
- D. Hemothorax (Correct Answer)
- E. Tension pneumothorax
Postoperative respiratory care Explanation: ***Hemothorax***
- The combination of **absent breath sounds**, **dullness to percussion** on the left, and **hypotension with flat neck veins** following trauma strongly suggests a massive hemothorax causing **hypovolemic shock** from significant blood loss into the pleural space.
- The injury site at the **left fourth intercostal space** (midaxillary line) is a common location for vascular injury. Dullness to percussion indicates fluid (blood) accumulation, not air.
- **Flat neck veins** are the key finding distinguishing hypovolemic shock (blood loss) from obstructive shock (tension pneumothorax or tamponade would cause distended neck veins).
- Tracheal deviation away from the affected side can occur with massive hemothorax due to mediastinal shift from fluid accumulation.
*Bronchial rupture*
- While possible with severe trauma, bronchial rupture typically presents with significant **air leak**, leading to subcutaneous emphysema and persistent pneumothorax, rather than **dullness to percussion** (which indicates fluid, not air).
- Usually causes **hyperresonance** on percussion, not dullness. Does not typically cause immediate massive hypovolemic shock with flat neck veins.
*Cardiac tamponade*
- Characterized by **Beck's triad**: hypotension, muffled heart sounds, and **distended neck veins** (due to impaired venous return).
- This patient has **flat neck veins**, which rules out tamponade. Additionally, cardiac examination shows no abnormalities (would expect muffled heart sounds in tamponade).
*Flail chest*
- Involves **paradoxical chest wall movement** due to multiple rib fractures creating a free-floating segment. While it causes pain and respiratory distress, it does not explain absent breath sounds, dullness to percussion, tracheal deviation, or hypovolemic shock.
- The primary issue is usually underlying pulmonary contusion, not massive blood loss into the pleural space.
*Tension pneumothorax*
- Classic presentation includes **absent breath sounds**, **hyperresonance to percussion** (air accumulation), **tracheal deviation** away from affected side, and **distended neck veins** (obstructive shock).
- This patient has **dullness to percussion** (fluid, not air) and **flat neck veins** (hypovolemic, not obstructive shock), making tension pneumothorax incompatible with the clinical picture.
Postoperative respiratory care US Medical PG Question 10: A 47-year-old man is brought to the emergency room by his wife. She states that they were having dinner at a restaurant when the patient suddenly became out of breath. His past medical history is irrelevant but has a 20-year pack smoking history. On evaluation, the patient is alert and verbally responsive but in moderate respiratory distress. His temperature is 37°C (98.6°F), blood pressure is 85/56 mm Hg, pulse is 102/min, and respirations are 20/min. His oxygen saturation is 88% on 2L nasal cannula. An oropharyngeal examination is unremarkable. The trachea is deviated to the left. Cardiopulmonary examination reveals decreased breath sounds on the right lower lung field with nondistended neck veins. Which of the following is the next best step in the management of this patient?
- A. Urgent needle decompression (Correct Answer)
- B. D-dimer levels
- C. Nebulization with albuterol
- D. Chest X-ray
- E. Heimlich maneuver
Postoperative respiratory care Explanation: ***Urgent needle decompression***
- The patient presents with sudden onset **respiratory distress**, **tracheal deviation** to the left (away from the affected right side), **decreased breath sounds** on the right, and **hypotension** with **tachycardia**. These are classic signs of a **tension pneumothorax**, which requires immediate needle decompression.
- This is a life-threatening emergency where air accumulates in the pleural space under positive pressure, collapsing the lung and shifting mediastinal structures, compromising venous return to the heart.
*D-dimer levels*
- While helpful in the workup for pulmonary embolism, **D-dimer levels** are not relevant as the immediate next step for a patient in acute respiratory distress with clear signs of tracheal deviation and decreased breath sounds, which points toward a mechanical lung issue.
- The patient's presentation with acute, severe respiratory symptoms and hemodynamic instability mandates immediate life-saving intervention.
*Nebulization with albuterol*
- **Albuterol** is used for bronchospasm, as seen in asthma or COPD exacerbations. This patient's symptoms are sudden and severe, with clear signs of a **tension pneumothorax**, which would not respond to bronchodilators.
- There is no indication of wheezing or a history of reactive airway disease to suggest this as a primary treatment.
*Chest X-ray*
- A **chest X-ray** would confirm the diagnosis of tension pneumothorax. However, given the patient's severe respiratory distress, hypotension, and classic physical findings (tracheal deviation, absent breath sounds), performing an X-ray would delay life-saving intervention.
- In a true tension pneumothorax, diagnosis is clinical, and immediate intervention takes precedence over imaging.
*Heimlich maneuver*
- The **Heimlich maneuver** is indicated for foreign body airway obstruction. The patient is verbally responsive, which indicates a patent airway, and there are no direct signs of choking on food.
- Although the patient was having dinner, the distinct clinical signs of **tracheal deviation** and unilateral decreased breath sounds do not support an airway obstruction requiring the Heimlich maneuver.
More Postoperative respiratory care US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.