DVT prophylaxis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for DVT prophylaxis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
DVT prophylaxis US Medical PG Question 1: A 26-year-old man presents with a 2-day history of worsening right lower leg pain. He states that he believes his right leg is swollen when compared to his left leg. Past medical history is significant for generalized anxiety disorder, managed effectively with psychotherapy. He smokes a pack of cigarettes daily but denies alcohol and illicit drug use. His father died of a pulmonary embolism at the age of 43. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, respiratory rate 14/min. On physical examination, the right lower leg is warmer than the left, and dorsiflexion of the right foot produces pain. Which of the following conditions is most likely responsible for this patient’s presentation?
- A. Vitamin K deficiency
- B. Hemophilia A
- C. von Willebrand disease
- D. Factor V Leiden (Correct Answer)
- E. Factor XI deficiency
DVT prophylaxis Explanation: ***Factor V Leiden***
- The patient presents with classic symptoms of a **deep vein thrombosis (DVT)** in the right lower leg: pain, swelling, warmth, and pain on dorsiflexion (**Homans' sign**). His history of smoking and a family history of **pulmonary embolism (PE)** in a young father strongly suggest an underlying **thrombophilia**.
- **Factor V Leiden** is the most common inherited thrombophilia, predisposing individuals to venous thromboembolism. The constellation of symptoms and risk factors points directly to this condition.
*Vitamin K deficiency*
- **Vitamin K deficiency** primarily leads to impaired production of clotting factors II, VII, IX, and X, resulting in a **bleeding diathesis**, not thrombotic events.
- Patients would typically present with **bruising, petechiae, gastrointestinal bleeding, or hematuria**, which are not seen here.
*Hemophilia A*
- **Hemophilia A** is an X-linked recessive disorder characterized by a deficiency of **Factor VIII**, leading to severe **bleeding**.
- Symptoms include **spontaneous or prolonged bleeding** into joints (hemarthrosis), muscles, or following trauma, which is the opposite of the patient's presentation.
*von Willebrand disease*
- **Von Willebrand disease (vWD)** is the most common inherited bleeding disorder, caused by a deficiency or defect in **von Willebrand factor**.
- It primarily causes **mucocutaneous bleeding**, such as epistaxis, menorrhagia, and easy bruising, not thrombotic episodes.
*Factor XI deficiency*
- **Factor XI deficiency** is a rare inherited bleeding disorder that typically causes **mild to moderate bleeding**, often associated with trauma or surgery.
- It is not associated with an increased risk of thrombosis and would present with bleeding, not a DVT.
DVT prophylaxis US Medical PG Question 2: A 62-year-old man comes to the physician because of a 5-day history of swelling in his left arm. Two months ago, he was diagnosed with a deep venous thrombosis in the left calf. He has had a 7-kg (15-lb) weight loss in the last 3 months. He has smoked 1 pack of cigarettes daily for the past 25 years. His only medication is warfarin. Physical examination shows warm edema of the left forearm with overlying erythema and a tender, palpable cord-like structure along the medial arm. His lungs are clear to auscultation bilaterally. Duplex sonography shows thrombosis of the left basilic and external jugular veins. Which of the following is the most appropriate next step to confirm the underlying diagnosis?
- A. CT scan of the chest
- B. X-ray of the chest (Correct Answer)
- C. Transesophageal echocardiography
- D. Serum antiphospholipid antibody level
- E. Serum D-dimer level
DVT prophylaxis Explanation: **X-ray of the chest**
- The patient presents with **recurrent deep venous thrombosis (DVT)**, specifically in an unusual location (upper extremity), combined with **unexplained weight loss** and a **significant smoking history**. These are strong indicators of an underlying malignancy.
- A **chest x-ray** is a readily available and cost-effective initial screening tool to evaluate for **lung cancer**, which is common in smokers and can present with paraneoplastic phenomena like hypercoagulability (Trousseau phenomenon) leading to DVT.
*CT scan of the chest*
- While a **CT scan of the chest** is more sensitive than an X-ray for detecting lung masses, an **X-ray is the more appropriate initial step** for screening given the clinical context.
- A **CT scan** would typically be performed after an abnormal chest X-ray or if clinical suspicion remains high despite a normal X-ray.
*Transesophageal echocardiography*
- **Transesophageal echocardiography (TEE)** is primarily used to evaluate **cardiac structures**, valve function, and to detect intracardiac thrombi or vegetations.
- It is not indicated as a primary screening tool for an underlying malignancy or in the workup of a **venous thrombosis** not directly related to cardiac pathology.
*Serum antiphospholipid antibody level*
- **Antiphospholipid antibody syndrome** is a cause of recurrent thrombosis, but the patient's other symptoms (weight loss, smoking history, unusual DVT location) point more strongly towards an underlying malignancy.
- While it might be considered in a broader workup for hypercoagulability, it is not the most immediate next step given the constellation of findings strongly suggestive of cancer.
*Serum D-dimer level*
- A **serum D-dimer level** is a marker of fibrin degradation and is useful for **excluding DVT/PE** in low-probability patients.
- In this patient, a DVT has already been diagnosed by duplex sonography, so a D-dimer level would not provide additional diagnostic information regarding the presence of thrombosis, nor would it help in identifying the underlying cause of the recurrent thrombosis.
DVT prophylaxis US Medical PG Question 3: A 59-year-old woman comes to the physician because of left leg swelling that started after a transcontinental flight. A duplex ultrasound of the left leg shows a noncompressible popliteal vein. A drug is prescribed that inhibits the coagulation cascade. Two weeks later, laboratory studies show:
Platelet count 210,000/mm3
Partial thromboplastin time 28 seconds (normal: 25-35)
Prothrombin time 12 seconds (normal: 11-13)
Thrombin time 15 seconds (control: 15 seconds)
Which of the following drugs was most likely prescribed?
- A. Unfractionated heparin
- B. Apixaban
- C. Aspirin
- D. Warfarin
- E. Low molecular weight heparin (Correct Answer)
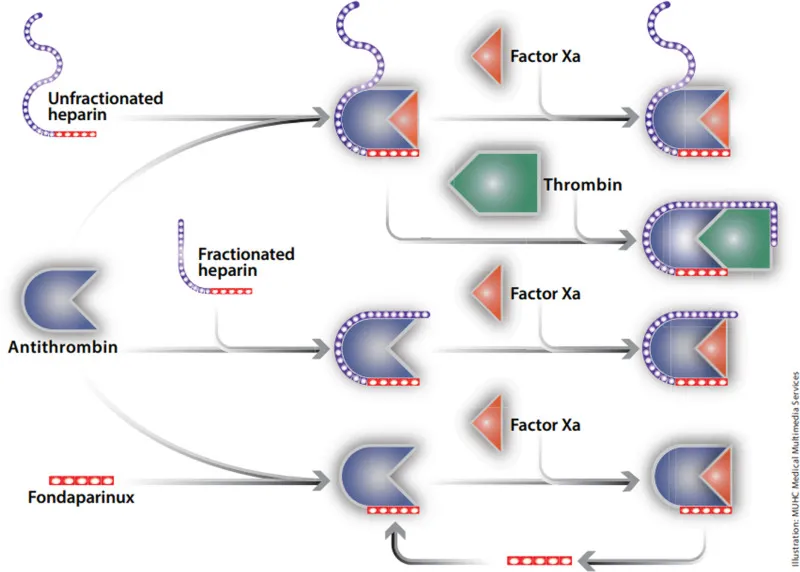
DVT prophylaxis Explanation: ***Low molecular weight heparin***
- **LMWH (e.g., enoxaparin) is the first-line treatment for acute DVT** in ambulatory patients and is the most likely drug prescribed in this outpatient scenario
- LMWH enhances **antithrombin activity primarily against Factor Xa** (more than Factor IIa/thrombin), which is why it has **minimal effect on routine coagulation tests** (PT, PTT, TT)
- **Monitoring of LMWH is done via anti-Xa levels**, not PTT, PT, or TT, explaining why all these values remain normal two weeks after initiation
- The normal coagulation studies are **expected and consistent** with therapeutic LMWH use
*Unfractionated heparin*
- Unfractionated heparin (UFH) acts by enhancing **antithrombin activity against both Factor Xa and Factor IIa (thrombin)**, which significantly **prolongs PTT** (typically 1.5-2x control when therapeutic)
- UFH requires **IV administration and hospital monitoring**, making it unlikely for this ambulatory post-flight DVT patient
- If the patient were currently on UFH, the **PTT would be prolonged** (not normal as shown); if discontinued, this wouldn't be "the drug prescribed" for ongoing DVT treatment
*Apixaban*
- Apixaban is a **direct Factor Xa inhibitor** that would cause **mild prolongation of PT** and possibly PTT at therapeutic levels
- While it's a reasonable outpatient DVT treatment, the completely normal PT argues against current apixaban use
- Apixaban doesn't require routine monitoring, but when measured, coagulation times would typically show some abnormality
*Warfarin*
- Warfarin is a **vitamin K antagonist** that inhibits synthesis of factors II, VII, IX, and X, causing **significant PT/INR prolongation** (target INR 2-3 for DVT)
- The **normal PT (12 seconds) excludes warfarin** as the current medication
- Warfarin requires regular INR monitoring and would not show normal values at therapeutic doses
*Aspirin*
- Aspirin is an **antiplatelet agent** (COX-1 inhibitor) that affects platelet aggregation, **not the coagulation cascade**
- It has **no effect on PT, PTT, or TT** and is **inadequate monotherapy for DVT treatment**
- While it may have a role in extended VTE prevention, it would not be the primary drug prescribed for acute DVT
DVT prophylaxis US Medical PG Question 4: An epidemiologist is evaluating the efficacy of Noxbinle in preventing HCC deaths at the population level. A clinical trial shows that over 5 years, the mortality rate from HCC was 25% in the control group and 15% in patients treated with Noxbinle 100 mg daily. Based on this data, how many patients need to be treated with Noxbinle 100 mg to prevent, on average, one death from HCC?
- A. 20
- B. 73
- C. 10 (Correct Answer)
- D. 50
- E. 100
DVT prophylaxis Explanation: ***10***
- The **number needed to treat (NNT)** is calculated by first finding the **absolute risk reduction (ARR)**.
- **ARR** = Risk in control group - Risk in treatment group = 25% - 15% = **10%** (or 0.10).
- **NNT = 1 / ARR** = 1 / 0.10 = **10 patients**.
- This means that **10 patients must be treated with Noxbinle to prevent one death from HCC** over 5 years.
*20*
- This would result from an ARR of 5% (1/0.05 = 20), which is not supported by the data.
- May arise from miscalculating the risk difference or incorrectly halving the actual ARR.
*73*
- This value does not correspond to any standard calculation of NNT from the given mortality rates.
- May result from confusion with other epidemiological measures or calculation error.
*50*
- This would correspond to an ARR of 2% (1/0.02 = 50), which significantly underestimates the actual risk reduction.
- Could result from incorrectly calculating the difference as a proportion rather than absolute percentage points.
*100*
- This would correspond to an ARR of 1% (1/0.01 = 100), grossly underestimating the treatment benefit.
- May result from confusing ARR with relative risk reduction or other calculation errors.
DVT prophylaxis US Medical PG Question 5: A 74-year-old man presents to the emergency department by paramedics for slurred speech and weakness in the left arm and leg for 1 hour. The patient was playing with his grandson when the symptoms started and his wife immediately called an ambulance. There is no history of head trauma or recent surgery. The patient takes captopril for hypertension. The vital signs include: pulse 110/min, respiratory rate 22/min, and blood pressure 200/105 mm Hg. The physical examination shows that the patient is alert and conscious, but speech is impaired. Muscle strength is 0/5 in the left arm and leg and 5/5 in the right arm and leg. A non-contrast CT of the head shows no evidence of intracranial bleeding. The lab results are as follows:
Serum glucose 90 mg/dL
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Serum creatinine 1.3 mg/dL
Blood urea nitrogen 20 mg/dL
Cholesterol, total 240 mg/dL
HDL-cholesterol 38 mg/dL
LDL-cholesterol 100 mg/dL
Triglycerides 190 mg/dL
Hemoglobin (Hb%) 15.3 g/dL
Mean corpuscular volume (MCV) 83 fL
Reticulocyte count 0.8%
Erythrocyte count 5.3 million/mm3
Platelet count 130,000/mm3
Partial thromboplastin time (aPTT) 30 sec
Prothrombin time (PT) 12 sec
Although he is within the time frame for the standard therapy of the most likely condition, the treatment cannot be started because of which of the following contraindications?
- A. A platelet count of 130,000/mm3
- B. Age of 74 years
- C. Cholesterol level of 240 mg/dL
- D. Creatinine level of 1.3 mg/dL
- E. Systolic blood pressure of 200 mm Hg (Correct Answer)
DVT prophylaxis Explanation: ***Systolic blood pressure of 200 mm Hg***
- The patient presents with symptoms highly suggestive of an **acute ischemic stroke**, including **slurred speech** and **left-sided weakness**.
- For patients with acute ischemic stroke who are candidates for **thrombolytic therapy (e.g., alteplase)**, a **systolic blood pressure consistently >185 mm Hg or diastolic >110 mm Hg is a contraindication** due to increased risk of hemorrhagic transformation.
*A platelet count of 130,000/mm3*
- A platelet count of 130,000/mm³ is above the **contraindication threshold for thrombolytic therapy**, which is typically <100,000/mm³.
- Therefore, this platelet count would **not prevent** the initiation of tPA.
*Age of 74 years*
- While older age was once considered a relative contraindication, current guidelines **do not consider age alone (including 74 years old) as an absolute contraindication** for thrombolytic therapy in acute ischemic stroke.
- Eligibility is determined by a comprehensive risk-benefit assessment, not solely by age.
*Cholesterol level of 240 mg/dL*
- An elevated **cholesterol level** is a **risk factor for atherosclerosis** and ischemic stroke, but it is **not a contraindication for acute thrombolytic therapy**.
- It relates to the underlying cause of the stroke rather than the immediate treatment decision.
*Creatinine level of 1.3 mg/dL*
- A **creatinine level of 1.3 mg/dL** indicates **mild renal impairment**, but it is **not a contraindication for thrombolytic therapy**.
- Renal function more significantly impacts the use of certain anticoagulants, but not typically alteplase in the acute setting.
DVT prophylaxis US Medical PG Question 6: A 25-year-old man presents to the emergency department with pain in his leg. He states that the pain was sudden and that his leg feels very tender. This has happened before, but symptoms resolved a few days later with acetaminophen. His temperature is 98.5°F (36.9°C), blood pressure is 129/88 mmHg, pulse is 90/min, respirations are 12/min, and oxygen saturation is 98% on room air. Physical exam reveals clear breath sounds bilaterally and a normal S1 and S2. The patient’s right leg is red, inflamed, and tender to palpation inferior to the popliteal fossa. Which of the following is the best treatment for this patient?
- A. Heparin (Correct Answer)
- B. Aspirin
- C. Ibuprofen and rest
- D. Clindamycin
- E. Warfarin
DVT prophylaxis Explanation: ***Heparin***
- The sudden onset of leg pain, tenderness, and inflammation, especially with a history of recurrent episodes, is highly suggestive of a **deep vein thrombosis (DVT)**. The location inferior to the popliteal fossa is a common site for calf vein DVTs.
- **Heparin** (either unfractionated or low molecular weight) is the first-line treatment for acute DVT to prevent clot propagation, pulmonary embolism, and post-thrombotic syndrome.
*Aspirin*
- **Aspirin** is an antiplatelet agent used for arterial thrombosis and cardiovascular event prevention, not effective for treating acute venous thromboembolism like DVT.
- Its mechanism primarily involves inhibiting cyclooxygenase to reduce thromboxane A2, which is less relevant in the coagulation cascade implicated in DVT.
*Ibuprofen and rest*
- **Ibuprofen** is an NSAID that can reduce pain and inflammation but does not address the underlying **thrombotic process** and will not prevent complications like pulmonary embolism.
- While rest might alleviate discomfort, it is not a primary treatment for DVT and prolonged immobility can actually worsen venous stasis.
*Clindamycin*
- **Clindamycin** is an antibiotic used to treat bacterial infections; it has no role in the management of DVT, which is a vascular condition.
- There are no signs of infection in the patient's presentation that would warrant antibiotic therapy.
*Warfarin*
- **Warfarin** is an oral anticoagulant used for long-term management of DVT and other thrombotic conditions, but it has a **delayed onset of action** (several days) due to its mechanism of inhibiting vitamin K-dependent clotting factors.
- It is typically initiated concurrently with a rapid-acting anticoagulant like heparin, which provides immediate anticoagulation until warfarin reaches therapeutic levels.
DVT prophylaxis US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
DVT prophylaxis Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
DVT prophylaxis US Medical PG Question 8: A 62-year-old Nigerian woman arrived 2 days ago to the US to visit her adult children from Nigeria. She is now brought to an urgent care center by her daughter for leg pain. Her right leg has been painful for 24 hours and is now causing her to limp. She denies any fevers, chills, or sweats and does not remember injuring her leg. She tells you she takes medications for hypertension and diabetes and occasionally for exertional chest pain. She has not had any recent chest pain. The right leg is swollen and tender. Flexion of the right ankle causes a worsening of the pain. Doppler ultrasonography reveals a large clot in a deep vein. Which of the following is the most appropriate course of action?
- A. Direct oral anticoagulant (DOAC) therapy (Correct Answer)
- B. Initiation of heparin followed by bridge to warfarin
- C. Initiation of heparin
- D. Initiation of warfarin
- E. Treatment with tissue plasminogen activator
DVT prophylaxis Explanation: ***Direct oral anticoagulant (DOAC) therapy***
- **DOACs are the first-line treatment** for acute DVT in most patients according to current guidelines (ACCP, ASH, ESC 2023-2024).
- Options include **rivaroxaban, apixaban, edoxaban, or dabigatran**, which provide rapid anticoagulation without the need for bridging therapy or routine INR monitoring.
- This patient has **provoked DVT** (recent long-distance travel from Nigeria), standard cardiovascular risk factors, and no contraindications to DOACs.
- DOACs offer **comparable efficacy** to warfarin with **lower risk of major bleeding** and greater convenience for patients.
*Initiation of heparin followed by bridge to warfarin*
- The **heparin-warfarin bridge** was standard therapy in the past but is now considered **second-line** for most patients.
- This approach is now **reserved for specific situations**: severe renal impairment (CrCl <30 mL/min), antiphospholipid syndrome, mechanical heart valves, or when DOACs are contraindicated or unavailable.
- The patient has **exertional chest pain** (angina), which is related to coronary artery disease and does **not** constitute a contraindication to DOACs or an indication for warfarin.
- The heparin bridge adds complexity, requires hospitalization or close monitoring, and delays transition to oral therapy.
*Initiation of heparin*
- **Heparin monotherapy** is insufficient for long-term DVT management and is only used as a bridge to oral anticoagulation in specific scenarios.
- While it provides immediate anticoagulation, discontinuing heparin without oral anticoagulant coverage leads to high recurrence risk.
- Modern practice favors **direct initiation of DOACs**, eliminating the need for parenteral therapy in most cases.
*Initiation of warfarin*
- **Warfarin monotherapy** at initiation is contraindicated because warfarin has a **delayed onset of action** (5-7 days) due to its mechanism of depleting vitamin K-dependent clotting factors.
- Starting warfarin alone creates a paradoxical **prothrombotic state** in the first 24-48 hours (due to rapid depletion of protein C) and leaves the patient unprotected from clot propagation.
- Warfarin requires **bridging with heparin** if used, but DOACs are preferred in current practice.
*Treatment with tissue plasminogen activator*
- **Thrombolytic therapy** (tPA, catheter-directed thrombolysis) is reserved for **life- or limb-threatening DVT** such as phlegmasia cerulea dolens or massive pulmonary embolism with hemodynamic instability.
- This patient has **uncomplicated DVT** without signs of limb-threatening ischemia, making anticoagulation the appropriate first-line therapy.
- Thrombolysis carries significant **bleeding risk** and is not indicated for routine DVT management.
DVT prophylaxis US Medical PG Question 9: A 45-year-old man presents to the emergency department because of fever and scrotal pain for 2 days. Medical history includes diabetes mellitus and morbid obesity. His temperature is 40.0°C (104.0°F), the pulse is 130/min, the respirations are 35/min, and the blood pressure is 90/68 mm Hg. Physical examination shows a large area of ecchymosis, edema, and crepitus in his perineal area. Fournier gangrene is suspected. A right internal jugular central venous catheter is placed without complication under ultrasound guidance for vascular access in preparation for the administration of vasopressors. Which of the following is the most appropriate next step?
- A. Confirm line placement by ultrasound
- B. Begin to use the line after documenting the return of dark, non-pulsatile blood from all ports
- C. Begin infusion of normal saline through a central line
- D. Obtain an immediate portable chest radiograph to evaluate line placement (Correct Answer)
- E. Begin infusion of norepinephrine to maintain systolic blood pressure over 90 mm Hg
DVT prophylaxis Explanation: **Obtain an immediate portable chest radiograph to evaluate line placement**
- The most appropriate next step after central venous catheter placement is to **confirm its correct position** and rule out complications like **pneumothorax** via imaging.
- A **chest radiograph** is the standard and immediate method to confirm proper placement of the tip in the lower superior vena cava and rule out pneumothorax, especially given the patient's critical condition.
*Confirm line placement by ultrasound*
- While ultrasound is used during placement to visualize the vessel and guide needle insertion, it is **not sufficient for confirming the final tip position** of the catheter or for ruling out pneumothorax.
- Ultrasound confirmation usually involves visualizing a **saline flush** in the right atrium, but a chest X-ray is still required for comprehensive evaluation.
*Begin to use the line after documenting the return of dark, non-pulsatile blood from all ports*
- Documenting blood return confirms that the catheter is in a vein but does not confirm **optimal tip placement** or exclude potential complications like **pneumothorax**.
- Using the line without radiological confirmation can lead to administering medications into incorrect locations (e.g., subclavian artery) or exacerbating unnoticed complications.
*Begin infusion of normal saline through a central line*
- Administering fluids before confirming proper line placement carries the risk of **extravasation** or infusing into an artery or other unintended space, which could worsen the patient's condition.
- Although IV fluids are needed in this septic patient, **confirmation of line placement** is a higher priority before commencing infusions.
*Begin infusion of norepinephrine to maintain systolic blood pressure over 90 mm Hg*
- While norepinephrine is crucial for managing septic shock and **hypotension** in this patient, starting it before confirming central line placement is dangerous.
- **Vasopressors require a secure central line** to prevent severe local tissue damage if extravasation occurs.
DVT prophylaxis US Medical PG Question 10: Five days after undergoing right knee arthroplasty for osteoarthritis, a 68-year-old man has severe pain in his right knee preventing him from participating in physical therapy. On the third postoperative day when the dressing was changed, the surgical wound appeared to be intact, slightly swollen, and had a clear secretion. He has a history of diabetes, hyperlipidemia, and hypertension. Current medications include metformin, enalapril, and simvastatin. His temperature is 37.3°C (99.1°F), pulse is 94/min, and blood pressure is 130/88 mm Hg. His right knee is swollen, erythematous, and tender to palpation. There is pain on movement of the joint. The medial parapatellar skin incision appears superficially opened in its proximal and distal part with yellow-green discharge. There is blackening of the skin on both sides of the incision. Which of the following is the next best step in the management of this patient?
- A. Vacuum dressing
- B. Antiseptic dressing
- C. Nafcillin therapy
- D. Removal of prostheses
- E. Surgical debridement (Correct Answer)
DVT prophylaxis Explanation: ***Surgical debridement***
- The patient presents with classic signs of **necrotizing fasciitis** or a severe wound infection: rapidly worsening pain, erythema, swelling, **yellow-green discharge**, and crucially, **blackening of the skin** (indicating tissue necrosis).
- Immediate **surgical debridement** is critical for source control, removal of necrotic tissue, and preventing further spread of infection, which can be life-threatening.
*Vacuum dressing*
- A vacuum-assisted closure (VAC) dressing is used for wound management after adequate debridement or for wounds without signs of aggressive infection to promote healing.
- Applying a VAC dressing to a wound with widespread necrosis and active infection, especially necrotizing fasciitis, without prior debridement would be ineffective and potentially harmful.
*Antiseptic dressing*
- While antiseptic dressings can help reduce bacterial load in some superficial wounds, they are entirely insufficient for deep-seated, rapidly spreading infections with tissue necrosis.
- This approach fails to address the underlying necrotic tissue and the extent of the infection, leading to rapid deterioration.
*Nafcillin therapy*
- **Antibiotic therapy** is essential for treating severe infections; however, it must be combined with source control, especially when necrosis is present.
- Giving antibiotics alone without **surgical debridement** in cases of necrotizing fasciitis is inadequate and will not prevent progression of the infection or improve patient outcomes.
*Removal of prostheses*
- While **prosthesis removal** may be necessary in some cases of established periprosthetic joint infection, it is a definitive and often late measure.
- The immediate priority in a rapidly progressing, necrotic wound infection is **surgical debridement** to remove devitalized tissue and control the local infection, prior to considering implant removal unless the infection is directly on the implant.
More DVT prophylaxis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.