Tracheoesophageal fistula repair US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Tracheoesophageal fistula repair. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Tracheoesophageal fistula repair US Medical PG Question 1: A 25-year-old man presents to his gastroenterologist for trouble swallowing. The patient states that whenever he eats solids, he regurgitates them back up. Given this patient's suspected diagnosis, the gastroenterologist performs a diagnostic test. Several hours later, the patient presents to the emergency department with chest pain and shortness of breath. His temperature is 99.5°F (37.5°C), blood pressure is 130/85 mmHg, pulse is 60/min, respirations are 12/min, and oxygen saturation is 99% on room air. On physical exam, the patient demonstrates a normal cardiopulmonary exam. His physical exam demonstrates no tenderness of the neck, a normal oropharynx, palpable crepitus above the clavicles, and minor lymphadenopathy. Which of the following is the best next step in management?
- A. Barium swallow
- B. Gastrografin swallow (Correct Answer)
- C. Urgent surgery
- D. Ultrasound
Tracheoesophageal fistula repair Explanation: ***Gastrografin swallow***
- This patient likely has an **esophageal perforation** following a diagnostic procedure, possibly **endoscopy or manometry** for suspected achalasia given the dysphagia, regurgitation, and subsequent symptoms.
- A **Gastrografin swallow** is the best initial diagnostic step because it is water-soluble, allowing for detection of a leak without causing severe complications if aspirated into the lungs or mediastinum.
*Barium swallow*
- This is generally not recommended for suspected esophageal perforation as **barium** is a corrosive agent that can cause a severe inflammatory reaction known as **mediastinitis** if it leaks into the mediastinum.
- While it offers superior mucosal detail, the risks associated with extravasation outweigh its benefits in this emergent setting.
*Urgent surgery*
- While **surgical repair** is the definitive treatment for significant esophageal perforations, it should only be performed after definitive diagnosis and localization of the perforation.
- Performing surgery without imaging confirmation would be inappropriate and potentially lead to unnecessary intervention or missing the actual site of injury.
*Ultrasound*
- **Ultrasound** has limited utility in diagnosing esophageal perforation due to the location of the esophagus behind the trachea and sternum, making it largely inaccessible to acoustic waves.
- It also cannot effectively detect the leakage of contrast material from the esophageal lumen.
Tracheoesophageal fistula repair US Medical PG Question 2: A new mother expresses her concerns because her 1-day-old newborn has been having feeding difficulties. The child vomits after every feeding and has had a continuous cough since shortly after birth. The mother denies any greenish coloration of the vomit and says that it is only composed of whitish milk that the baby just had. The child exhibits these coughing spells during the exam, at which time the physician notices the child’s skin becoming cyanotic. The mother states that the child was born vaginally with no complications, although her records show that she had polyhydramnios during her last ultrasound before the delivery. Which of the following is the most likely cause of the patient’s symptoms?
- A. Failure of recanalization of duodenum
- B. Obstruction due to failure of rotation of pancreatic tissue
- C. Hypertrophy of the pyloric sphincter
- D. Failure of neural crest cells to migrate into the myenteric plexus
- E. Defective formation of the esophagus with tracheoesophageal connection (Correct Answer)
Tracheoesophageal fistula repair Explanation: ***Defective formation of the esophagus with tracheoesophageal connection***
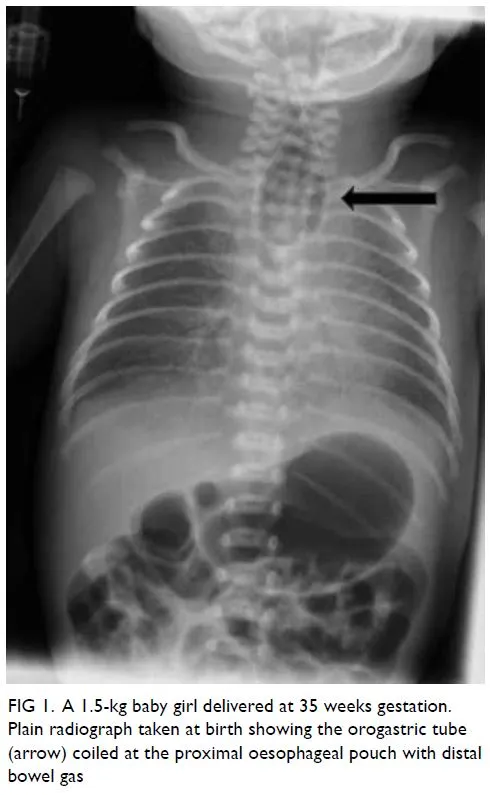
- The combination of **feeding difficulties**, vomiting of **undigested milk**, **continuous coughing**, and **cyanosis** during coughing spells in a newborn strongly suggests a **tracheoesophageal fistula (TEF)**, often with **esophageal atresia**.
- **Polyhydramnios** during pregnancy is a classic prenatal sign due to the fetal inability to swallow amniotic fluid.
*Failure of recanalization of duodenum*
- This condition, known as **duodenal atresia**, typically presents with **bilious vomiting** if the obstruction is distal to the ampulla of Vater, or non-bilious if proximal, but typically does not cause continuous coughing or cyanosis during feeds.
- While it causes vomiting, it primarily affects digestion and nutrient absorption, and **polyhydramnios** can also be present due to impaired fetal swallowing.
*Obstruction due to failure of rotation of pancreatic tissue*
- This describes **annular pancreas**, where pancreatic tissue encircles the duodenum, causing obstruction and **vomiting** (often bilious).
- Like duodenal atresia, it doesn't explain the characteristic **coughing and cyanosis** with feeds seen in this case.
*Hypertrophy of the pyloric sphincter*
- **Pyloric stenosis** typically presents later (2-8 weeks of age) with **projectile non-bilious vomiting**, and an **olive-shaped mass** may be palpable in the abdomen.
- It does not cause coughing or cyanosis that correlates directly with feeding in a 1-day-old.
*Failure of neural crest cells to migrate into the myenteric plexus*
- This describes **Hirschsprung disease**, which primarily affects the colon and presents with symptoms of **intestinal obstruction** (e.g., abdominal distension, failure to pass meconium, bilious vomiting if severe).
- It is not associated with feeding difficulties, coughing, or cyanosis in the manner described.
Tracheoesophageal fistula repair US Medical PG Question 3: A previously healthy 55-year-old man comes to the physician because of a 5-month history of progressively worsening substernal chest pain after meals. The pain occurs almost daily, is worst after eating spicy food or drinking coffee, and often wakes him up from sleep at night. He has not had any weight loss. He has smoked 1 pack of cigarettes daily for 35 years and he drinks 1 to 2 glasses of wine daily with dinner. Physical examination is unremarkable. Esophagogastroduodenoscopy shows erythema of the distal esophagus with two small mucosal erosions. Biopsy specimens obtained from the esophagus show no evidence of metaplasia. Without treatment, this patient is at greatest risk for which of the following complications?
- A. Esophageal squamous cell carcinoma
- B. Esophageal adenocarcinoma
- C. Esophageal stricture (Correct Answer)
- D. Sliding hiatal hernia
- E. Pyloric stenosis
Tracheoesophageal fistula repair Explanation: ***Esophageal stricture***
- Chronic inflammation from **gastroesophageal reflux disease (GERD)** can lead to **fibrosis and scar tissue formation** in the esophagus, resulting in the narrowing of the esophageal lumen.
- While not immediately life-threatening, **esophageal strictures** can cause **dysphagia** and require endoscopic dilation.
*Esophageal squamous cell carcinoma*
- This type of cancer is more commonly associated with **tobacco and alcohol use**, but generally does not directly result from GERD.
- There is no mention of **dysphagia to solids** or other typical symptoms of esophageal cancer.
*Esophageal adenocarcinoma*
- This complication is typically preceded by **Barrett's esophagus**, which involves **intestinal metaplasia** of the esophageal lining.
- The biopsy results explicitly state **no evidence of metaplasia**, making this an unlikely immediate risk.
*Sliding hiatal hernia*
- A **sliding hiatal hernia** is a common anatomical predisposition for GERD, and it may contribute to the patient's symptoms but is not a complication *of* GERD itself.
- It involves the **protrusion of the stomach into the chest cavity** through the diaphragm.
*Pyloric stenosis*
- **Pyloric stenosis** affects the **pylorus**, the opening between the stomach and the small intestine, and is not a direct complication of esophageal reflux disease.
- It usually presents with **projectile vomiting** and typically occurs in infants or, less commonly, in adults due to other causes like chronic ulcers or tumors.
Tracheoesophageal fistula repair US Medical PG Question 4: A 35-year-old man is admitted with an acute onset of dysphagia, odynophagia, slight retrosternal chest pain, hypersalivation, and bloody sputum. These symptoms appeared 3 hours ago during a meal when the patient ate fish. The patient’s past medical history is significant for repair of a traumatic esophageal rupture 5 years ago.
The patient’s vital signs are as follows: blood pressure 140/90 mm Hg, heart rate 87/min, respiratory rate 16/min, and temperature 36.8℃ (98.2℉). On exam, the patient is pale and breathing deeply. The oral cavity appears normal. The pharynx is erythematous but with no visible lesions. Lungs are clear to auscultation. Cardiovascular examination shows no abnormalities. The abdomen is nondistended and nontender. Which of the following interventions are indicated in this patient?
- A. Foley catheter removal
- B. Removal with Magill forceps
- C. Bougienage
- D. Emergency endoscopy (Correct Answer)
- E. IV administration of glucagon
Tracheoesophageal fistula repair Explanation: ***Emergency endoscopy***
- This patient presents with **acute dysphagia**, **odynophagia**, and **bloody sputum** after ingesting fish, strongly suggesting an esophageal foreign body, possibly with esophageal injury or perforation given his history of esophageal repair.
- **Emergency endoscopy** is the most appropriate intervention to directly visualize, retrieve the foreign body, assess the extent of injury, and manage potential complications like perforation.
*Foley catheter removal*
- The patient's presentation does not provide any information or indication for the presence of a **Foley catheter**, which is typically used for urinary drainage.
- Removing a Foley catheter would not address the patient's acute esophageal symptoms or potential foreign body.
*Removal with Magill forceps*
- While Magill forceps can be used to remove foreign bodies from the **oropharynx or hypopharynx**, they are generally not suitable for deep esophageal foreign bodies.
- This method risks blindly pushing the object further or causing additional trauma to the esophagus, especially in a patient with a history of esophageal repair.
*Bougienage*
- **Bougienage** (esophageal dilation) is contraindicated in the presence of an esophageal foreign body or suspected perforation.
- Attempting bougienage could worsen esophageal injury, push the foreign body into deeper structures, or exacerbate an existing perforation.
*IV administration of glucagon*
- **Glucagon** is sometimes used to relax the smooth muscle of the esophagus in cases of food impaction without sharp objects, to facilitate passage.
- However, it is **contraindicated** if there is suspicion of a sharp foreign body, severe esophageal injury, or perforation, as seen in this patient with bloody sputum and a history of esophageal rupture.
Tracheoesophageal fistula repair US Medical PG Question 5: A 2600-g (5-lb 8-oz) male newborn is delivered at 34 weeks' gestation to a 22-year-old woman. The mother did not have prenatal care. Upon examination in the delivery room, the newborn's skin appears blue. He is gasping and breathing irregularly. The ears are low-set with broad auricles, and the nasal tip is flattened. The lower jaw is small and displaced backward. The right foot is clubbed. Which of the following is the most likely underlying cause of this patient's condition?
- A. Pulmonary hypoplasia
- B. Posterior urethral valves (Correct Answer)
- C. Fetal anemia
- D. Anencephaly
- E. Esophageal atresia
Tracheoesophageal fistula repair Explanation: ***Posterior urethral valves***
- The combination of **respiratory distress** and distinctive craniofacial and limb abnormalities (low-set ears, broad auricles, flattened nasal tip, micrognathia, club foot) in a premature infant suggests **Potter sequence**, which is usually caused by **severe oligohydramnios**.
- **Posterior urethral valves** are the most common cause of lower urinary tract obstruction in male infants, leading to **oligohydramnios** and subsequent Potter sequence.
*Pulmonary hypoplasia*
- While present in this case due to Potter sequence, **pulmonary hypoplasia** is a consequence, not the underlying cause.
- It results from the lung compression due to **oligohydramnios**, preventing normal lung development.
*Fetal anemia*
- Fetal anemia typically manifests as **hydrops fetalis**, characterized by severe edema, ascites, and pleural effusions, which are not described here.
- It does not directly lead to the specific constellation of craniofacial and limb anomalies seen in this patient.
*Anencephaly*
- **Anencephaly** is a severe form of neural tube defect involving absence of a major portion of the brain and skull.
- While associated with **polyhydramnios** (due to impaired fetal swallowing), it does not cause the specific features of Potter sequence.
*Esophageal atresia*
- **Esophageal atresia** often presents with **polyhydramnios** due to the inability of the fetus to swallow amniotic fluid.
- The primary clinical sign after birth is excessive salivation and inability to pass a feeding tube, not the craniofacial and limb anomalies described.
Tracheoesophageal fistula repair US Medical PG Question 6: A 68-year-old woman comes to the physician with dysphagia and halitosis for several months. She feels food sticking to her throat immediately after swallowing. Occasionally, she regurgitates undigested food hours after eating. She has no history of any serious illness and takes no medications. Her vital signs are within normal limits. Physical examination including the oral cavity, throat, and neck shows no abnormalities. Which of the following is the most appropriate diagnostic study at this time?
- A. Cervical magnetic resonance imaging
- B. Upper gastrointestinal series
- C. Chest computed tomography scan
- D. Barium swallow with video fluoroscopy (Correct Answer)
- E. Chest X-ray
Tracheoesophageal fistula repair Explanation: ***Barium swallow with video fluoroscopy***
- This is the most appropriate initial diagnostic step to visualize the act of swallowing and identify structural abnormalities in the esophagus and pharynx, such as a **Zenker's diverticulum** (which is strongly suggested by symptoms of dysphagia, halitosis, and regurgitation of undigested food hours after eating).
- It allows for the detection of **motility disorders**, strictures, or outpouchings that can cause the described symptoms.
*Upper gastrointestinal series*
- While it uses barium, an upper GI series focuses more on the **stomach and duodenum** rather than the pharynx and esophagus in dynamic motion during swallowing.
- It is less effective in evaluating the **pharyngeal phase of swallowing** and subtle motility issues compared to a dedicated barium swallow with fluoroscopy.
*Cervical magnetic resonance imaging*
- MRI is excellent for soft tissue evaluation but is not the first-line investigation for **dysphagia caused by structural or motility issues** in the pharynx or esophagus.
- It does not provide real-time functional assessment of swallowing and may not clearly visualize the mucosal details or a small diverticulum.
*Chest computed tomography scan*
- A chest CT scan is primarily used to evaluate structures within the **chest cavity**, including the lungs, mediastinum, and large vessels.
- It is generally not the initial diagnostic tool for evaluating **oropharyngeal or esophageal dysphagia** as it offers limited dynamic information about swallowing mechanics.
*Chest X-ray*
- A chest X-ray provides a static image of the chest and is mainly used to assess cardiopulmonary pathology.
- It has **limited utility** in evaluating the esophagus or pharynx for the causes of dysphagia and regurgitation, as it cannot visualize soft tissue details or dynamic swallowing processes.
Tracheoesophageal fistula repair US Medical PG Question 7: A baby is born after the 32nd gestational week by cesarean delivery. The mother suffered from gestational diabetes; however, she had no other pregnancy-related diseases and was otherwise healthy. The baby has a blood pressure of 100/58 mm Hg, heart rate of 104/min, and oxygen saturation of 88%. The child has tachypnea, subcostal and intercostal retractions, nasal flaring, and cyanosis. The cyanosis is responding well to initial administration of oxygen. The nasogastric tube was positioned without problems. Which of the following is the most likely diagnosis?
- A. Tracheoesophageal fistula
- B. Pneumonia
- C. Neonatal respiratory distress syndrome (NRDS) (Correct Answer)
- D. Sepsis
- E. Congenital heart anomaly with right-to-left shunt
Tracheoesophageal fistula repair Explanation: ***Neonatal respiratory distress syndrome (NRDS)***
- The premature birth (32nd week), presence of **tachypnea**, **retractions**, **nasal flaring**, **cyanosis** responding to oxygen, and maternal **gestational diabetes** are all highly suggestive of NRDS.
- Maternal gestational diabetes can delay fetal lung maturity, increasing the risk of **surfactant deficiency**, which is the primary cause of NRDS.
*Tracheoesophageal fistula*
- This condition typically presents with **choking**, **coughing**, and **regurgitation** during feeding, often with inability to pass a nasogastric tube into the stomach.
- The successful positioning of the **nasogastric tube** makes this diagnosis less likely.
*Pneumonia*
- While pneumonia can cause respiratory distress, the **early onset** in a premature infant with maternal gestational diabetes points more strongly towards **NRDS**.
- Pneumonia would typically have signs of **infection** such as fever, though early neonatal pneumonia can be atypical.
*Sepsis*
- Sepsis can cause respiratory distress, but it's usually accompanied by other signs of systemic infection, such as **fever or hypothermia**, **lethargy**, and poor feeding and often signs of **circulatory compromise**.
- The clinical picture provided primarily points towards a respiratory rather than a systemic infectious cause primarily.
*Congenital heart anomaly with right-to-left shunt*
- While this can cause **cyanosis** and respiratory distress, the prompt response to oxygen management makes a significant right-to-left shunt less likely.
- A significant right-to-left shunt would typically cause **cyanosis** that is refractory to oxygen administration.
Tracheoesophageal fistula repair US Medical PG Question 8: A 5-year-old girl is brought to the emergency department after drinking a bottle of drain cleaner. It is unknown how much the child drank. She has a past medical history of Down syndrome and obesity. The patient's vitals are unremarkable. Physical exam is notable for a child in no acute distress. She is tolerating her oral secretions and interactive. Inspection of the oropharynx is unremarkable. Which of the following is appropriate management of this patient?
- A. Dilute hydrochloric acid
- B. Polyethylene glycol
- C. Observation
- D. Intubation
- E. Endoscopy (Correct Answer)
Tracheoesophageal fistula repair Explanation: ***Endoscopy***
- Due to the **inherent danger of caustic ingestion**, regardless of initial symptoms, **esophagogastroduodenoscopy (EGD)** is the gold standard for assessing the extent and severity of injury to the upper gastrointestinal tract. This procedure is crucial within the first 12-24 hours to guide further management.
- While the patient is asymptomatic, **caustic injuries** can progress and develop into strictures or perforations even without immediate obvious symptoms, making direct visualization essential.
*Dilute hydrochloric acid*
- **Neutralizing alkalis with acids** (or vice-versa) is contraindicated as it can cause an **exothermic reaction**, leading to further thermal injury and worsening the damage.
- Chemical neutralization can also produce gas, which increases the **risk of esophageal perforation**.
*Polyethylene glycol*
- **Polyethylene glycol (PEG)** is an osmotic laxative used for **bowel preparation** or as a treatment for constipation but has no role in the management of caustic ingestion.
- It would not remove the caustic substance from the esophagus or stomach, nor would it mitigate the chemical damage.
*Observation*
- Despite being asymptomatic initially, **caustic ingestions** can lead to delayed and severe complications such as **stricture formation**, perforation, and mediastinitis.
- **Asymptomatic presentation** does not rule out significant internal injury, particularly because the full extent of the ingestion is unknown, making observation alone an unsafe approach.
*Intubation*
- While airway compromise is a potential complication of caustic ingestion, the patient is currently in no acute distress and is tolerating oral secretions, indicating a **patent airway**.
- **Prophylactic intubation** is not indicated at this stage unless there are signs of respiratory distress, stridor, or significant oropharyngeal edema.
Tracheoesophageal fistula repair US Medical PG Question 9: A 25-year-old woman gives birth to a male child at 30 weeks of gestation. Pregnancy was complicated by polyhydramnios diagnosed on ultrasonography at 26 weeks of gestation. The baby is born vaginally weighing 1.2 kg (2.64 lb). Because he does not cry immediately after birth, endotracheal intubation is attempted to secure the airway. However, the vocal cords cannot be visualized because there is only a single opening corresponding to the esophagus. He is transferred to the NICU under bag and mask ventilation, where intubation is attempted once again by passing the endotracheal tube in the visualized opening, after which his oxygen saturation begins to improve. His temperature is 37.0ºC (98.6°F), pulse is 120/min, and respiratory rate is 42/min. On physical examination, no abnormalities are noted. Chest radiography is suggestive of respiratory distress syndrome. Which of the following most likely failed to develop in this patient?
- A. Second branchial arch
- B. Mesonephric duct
- C. Fourth and sixth branchial arches (Correct Answer)
- D. First branchial arch
- E. Third branchial arch
Tracheoesophageal fistula repair Explanation: ***Fourth and sixth branchial arches***
- The clinical presentation of **inability to visualize the vocal cords** and the presence of only a **single opening** suggests **laryngeal atresia** or severe laryngotracheal malformation. While the laryngotracheal structures primarily develop from the laryngotracheal diverticulum (an outgrowth of the foregut), the **fourth and sixth pharyngeal arches** are critical for the development of **laryngeal cartilages** and **innervation**:
- **Fourth arch**: Contributes to the thyroid cartilage, cricothyroid muscle, and superior laryngeal nerve
- **Sixth arch**: Forms the cricoid cartilage, arytenoid cartilages, and provides the recurrent laryngeal nerve (innervating all intrinsic laryngeal muscles except cricothyroid)
- Failure of proper development of these arches results in **absence or malformation of the larynx**, preventing normal vocal cord formation and airway development.
- The **polyhydramnios** occurs because the fetus cannot swallow amniotic fluid effectively due to airway obstruction.
*Second branchial arch*
- The **second branchial arch** (hyoid arch) contributes to the **stapes**, styloid process, stylohyoid ligament, lesser horn and upper body of the hyoid bone, and muscles of facial expression (via facial nerve).
- Defects in this arch typically lead to conditions like **Treacher Collins syndrome** or hemifacial microsomia, not laryngeal agenesis.
*Mesonephric duct*
- The **mesonephric duct (Wolffian duct)** is an embryonic structure crucial for the development of male internal reproductive organs including the **epididymis**, vas deferens, seminal vesicles, and ejaculatory duct.
- Failure of this duct to develop would result in male reproductive anomalies, not respiratory tract malformations.
*First branchial arch*
- The **first branchial arch** (mandibular arch) gives rise to the **maxilla, mandible, malleus, incus**, muscles of mastication, and trigeminal nerve branches.
- Malformations of this arch are associated with conditions like **Pierre Robin sequence** or mandibulofacial dysostosis, presenting with micrognathia and facial abnormalities, which are not described in this case.
*Third branchial arch*
- The **third branchial arch** forms the **greater horn and lower body of the hyoid bone**, stylopharyngeus muscle, and glossopharyngeal nerve.
- Anomalies of this arch may present with swallowing difficulties or glossopharyngeal nerve deficits, but do not cause the complete absence of laryngeal structures described in this scenario.
Tracheoesophageal fistula repair US Medical PG Question 10: A 56-year-old man presents to the emergency department with severe chest pain and a burning sensation. He accidentally drank a cup of fluid at his construction site 2 hours ago. The liquid was later found to contain lye. On physical examination, his blood pressure is 100/57 mm Hg, respiratory rate is 21/min, pulse is 84/min, and temperature is 37.7°C (99.9°F). The patient is sent immediately to the radiology department. The CT scan shows air in the mediastinum, and a contrast swallow study confirms the likely diagnosis. Which of the following is the best next step in the management of this patient’s condition?
- A. Ceftriaxone
- B. Oral antidote
- C. Dexamethasone
- D. Surgical repair (Correct Answer)
- E. Nasogastric lavage
Tracheoesophageal fistula repair Explanation: ***Surgical repair***
- The presence of **mediastinal air** on CT scan and confirmation of **esophageal perforation** by contrast swallow study indicate a surgical emergency.
- **Emergency surgical repair** is crucial to prevent widespread mediastinitis, sepsis, and potential mortality from corrosive ingestion.
*Ceftriaxone*
- While **antibiotics** like Ceftriaxone might be used as adjuncts to prevent infection, they are not the primary treatment for an established esophageal perforation.
- Antibiotics alone will not address the structural defect or contain the leakage of corrosive material into the mediastinum.
*Oral antidote*
- For corrosive ingestions, administering an **oral antidote** is contraindicated as it can worsen tissue damage or induce vomiting, leading to further esophageal injury.
- The immediate priority is managing the perforation, not neutralizing the corrosive agent internally.
*Dexamethasone*
- **Corticosteroids** like dexamethasone are sometimes considered in the management of corrosive ingestions to reduce stricture formation, but their role is controversial and they are not the initial treatment for an acute perforation.
- In an active perforation, corticosteroids would not address the immediate life-threatening issue of mediastinal contamination.
*Nasogastric lavage*
- **Nasogastric lavage** is contraindicated in corrosive ingestions, especially with suspected or confirmed perforation.
- Passing a tube could further injure the already damaged tissue and increase the risk of perforation or exacerbate an existing one.
More Tracheoesophageal fistula repair US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.