Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pyloric stenosis diagnosis and pyloromyotomy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 1: A 23-year-old college senior visits the university health clinic after vomiting large amounts of blood. He has been vomiting for the past 36 hours after celebrating his team’s win at the national hockey championship with his varsity friends while consuming copious amounts of alcohol. His personal medical history is unremarkable. His blood pressure is 129/89 mm Hg while supine and 100/70 mm Hg while standing. His pulse is 98/min, strong and regular, with an oxygen saturation of 98%. His body temperature is 36.5°C (97.7°F), while the rest of the physical exam is normal. Which of the following is associated with this patient’s condition?
- A. Esophageal tear (Correct Answer)
- B. Portal hypertension
- C. Esophageal metaplasia
- D. Esophageal varices
- E. Esophageal perforation
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***Esophageal tear***
- This patient's presentation of **hematemesis** after prolonged, forceful vomiting, especially following substantial alcohol consumption, is highly characteristic of a **Mallory-Weiss tear**.
- A Mallory-Weiss tear is a **longitudinal mucosal laceration** at the gastroesophageal junction, caused by the sudden increase in **intra-abdominal and intra-gastric pressure** during retching or vomiting.
*Portal hypertension*
- While portal hypertension can lead to upper GI bleeding from **esophageal varices**, there is no clinical evidence of **chronic liver disease** (e.g., jaundice, ascites, spider angiomata) in this otherwise healthy young man.
- The patient's unremarkable medical history and acute onset of symptoms after an episode of severe vomiting are not typical for a new presentation of chronic **portal hypertension**.
*Esophageal metaplasia*
- **Esophageal metaplasia (Barrett's esophagus)** is a change in the lining of the esophagus from squamous to columnar epithelium, usually due to chronic gastroesophageal reflux disease (GERD).
- It is an asymptomatic precursor to adenocarcinoma and does not cause acute, massive hematemesis without associated ulceration or malignancy.
*Esophageal varices*
- **Esophageal varices** are dilated veins in the lower esophagus that can rupture and cause life-threatening bleeding, typically due to **portal hypertension** from cirrhosis or other liver diseases.
- The patient's lack of a history of liver disease and the context of excessive vomiting make variceal bleeding less likely than a Mallory-Weiss tear.
*Esophageal perforation*
- **Esophageal perforation (Boerhaave syndrome)** is a transmural tear of the esophagus, also associated with severe vomiting, but it presents with more severe symptoms.
- Key differentiating features include **severe retrosternal chest pain**, **dyspnea**, **subcutaneous emphysema**, and potentially **septic shock** due to mediastinitis, none of which are described in this patient.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 2: A 4-year-old boy presents to the emergency department after his parents found him drinking blue liquid out of an unlabeled bottle in the garage. They have no idea what was in the bottle and are concerned for his health. They have brought the bottle with them to the emergency department. The child's past medical history is not remarkable, and he is currently not taking any medications. The patient's vitals are within normal limits for his age. Physical exam reveals a crying child who is drooling. A radiograph is performed, and the child's vitals are closely monitored. It is determined that the blue liquid is a strong alkali. Which of the following is the best next step in management?
- A. Administration of a diluent
- B. Gastrografin swallow and endoscopy (Correct Answer)
- C. Administration of a weak acid
- D. Charcoal
- E. Ipecac
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***Gastrografin swallow and endoscopy***
- **Endoscopy within 12-24 hours** is the gold standard for evaluating caustic ingestions, allowing direct visualization of mucosal injury and grading of severity to guide management.
- A **Gastrografin swallow** (water-soluble contrast study) may be considered if esophageal perforation is suspected, though it is not routinely performed in all cases; CT imaging is often preferred for perforation assessment.
- The key intervention is **endoscopy**, which should not be delayed beyond 24 hours to avoid missing the optimal window for assessment before granulation tissue forms.
*Administration of a diluent*
- Administering a diluent is **contraindicated** when there are signs of esophageal injury such as drooling, as it can worsen inflammation, induce vomiting, or lead to perforation.
- Dilution may also cause vomiting which re-exposes the esophagus to the caustic substance, causing additional injury.
*Administration of a weak acid*
- Neutralizing a strong alkali with a weak acid is **not recommended** due to the exothermic reaction this causes, generating heat and worsening tissue damage.
- The precise amount of acid needed for safe neutralization cannot be reliably determined, making this approach dangerous.
*Charcoal*
- **Activated charcoal** does not bind to strong alkalis or acids and is therefore not indicated for caustic ingestions.
- It may also impede endoscopic visualization, delaying definitive diagnosis and management.
*Ipecac*
- **Syrup of ipecac** induces vomiting and is **contraindicated** in caustic ingestions because it causes re-exposure of the esophagus to the corrosive substance, increasing mucosal damage.
- Vomiting also carries significant risk of aspiration into the lungs, which can cause severe respiratory complications.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 3: A 48-year-old woman is transferred from her primary care physician's office to the emergency department for further evaluation of hypokalemia to 2.5 mEq/L. She was recently diagnosed with hypertension 2 weeks ago and started on medical therapy. The patient said that she enjoys all kinds of food and exercises regularly, but has not been able to complete her workouts as she usually does. Her temperature is 97.7°F (36.5°C), blood pressure is 107/74 mmHg, pulse is 80/min, respirations are 15/min, and SpO2 is 94% on room air. Her physical exam is unremarkable. Peripheral intravenous (IV) access is obtained. Her basic metabolic panel is obtained below.
Serum:
Na+: 135 mEq/L
Cl-: 89 mEq/L
K+: 2.2 mEq/L
HCO3-: 33 mEq/L
BUN: 44 mg/dL
Glucose: 147 mg/dL
Creatinine: 2.3 mg/dL
Magnesium: 2.0 mEq/L
What is the next best step in management?
- A. Obtain an electrocardiogram (Correct Answer)
- B. Obtain urine sodium and creatinine
- C. Administer isotonic saline 1 liter via peripheral IV
- D. Administer potassium chloride 40mEq via peripheral IV
- E. Administer potassium bicarbonate 50mEq per oral
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***Obtain an electrocardiogram***
- The patient has severe **hypokalemia** (K+ 2.2 mEq/L), which requires urgent assessment for cardiac complications before initiating treatment.
- An **ECG is the mandatory first step** in severe hypokalemia (K+ <2.5 mEq/L) to evaluate for life-threatening arrhythmias and ECG changes including U waves, T wave flattening, ST depression, and QT prolongation.
- The patient is **hemodynamically stable** with only mild symptoms (exercise intolerance), so immediate potassium administration is not required before obtaining an ECG.
- ECG findings will guide the urgency and route of potassium repletion and determine the need for cardiac monitoring during treatment.
*Administer potassium chloride 40mEq via peripheral IV*
- While **IV potassium chloride** will be needed for repletion, it should be administered after ECG assessment in a stable patient.
- IV potassium administration carries risks including phlebitis, infiltration, and potential cardiac complications if given too rapidly without monitoring.
- In severe hypokalemia without cardiac arrest or documented life-threatening arrhythmias, obtaining an ECG first is standard practice.
*Obtain urine sodium and creatinine*
- Measuring **urine electrolytes** helps identify the cause of hypokalemia (likely diuretic-induced given recent hypertension treatment with metabolic alkalosis and hypochloremia).
- However, this diagnostic workup should follow the immediate assessment and treatment of severe hypokalemia.
- While useful for long-term management, it does not take priority over assessing cardiac risk with an ECG.
*Administer potassium bicarbonate 50mEq per oral*
- **Potassium bicarbonate** is contraindicated in this patient with **metabolic alkalosis** (HCO3- 33 mEq/L), as it would worsen the alkalosis.
- The correct form for repletion in metabolic alkalosis is **potassium chloride**, which addresses both the hypokalemia and hypochloremia.
- Oral repletion is also too slow for severe hypokalemia and may cause gastrointestinal side effects.
*Administer isotonic saline 1 liter via peripheral IV*
- While the patient shows signs of volume depletion (elevated BUN/Cr ratio, likely prerenal azotemia from diuretic use), the immediate priority is assessing the cardiac impact of severe hypokalemia.
- **Isotonic saline** without potassium supplementation could potentially worsen hypokalemia through dilution and increased renal potassium excretion.
- Volume resuscitation should be considered after ECG assessment and in conjunction with potassium repletion.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 4: A 3-week-old firstborn baby girl is brought to the pediatric emergency room with projectile vomiting. She started vomiting while feeding 12 hours ago and has been unable to keep anything down since then. After vomiting, she appears well and hungry, attempting to feed again. The vomitus has been non-bloody and non-bilious. The last wet diaper was 10 hours ago. The child was born at 40 weeks gestation to a healthy mother. On examination, the child appears sleepy but has a healthy cry during the exam. The child has dry mucous membranes and delayed capillary refill. There is a palpable olive-shaped epigastric mass on palpation. Which of the following is the most likely cause of this patient's condition?
- A. Failure of neural crest cell migration into the rectum
- B. Telescoping of the small bowel into the large bowel
- C. Hypertrophic muscularis externa (Correct Answer)
- D. Patent tract between the trachea and esophagus
- E. Failure of duodenal lumen recanalization
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***Hypertrophic muscularis externa***
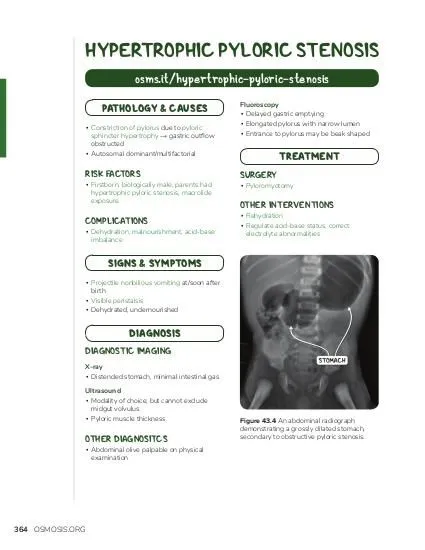
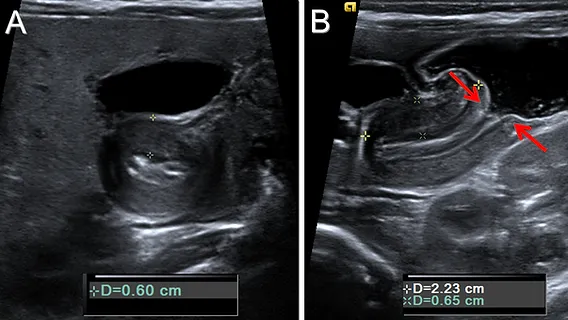
- The presented symptoms, including **projectile vomiting** in a 3-week-old, **non-bilious** emesis, post-vomiting **hunger**, and a **palpable olive-shaped mass** in the epigastrium, are classic signs of **pyloric stenosis**. This condition is caused by the **hypertrophy of the pyloric sphincter's muscularis externa**.
- Pyloric stenosis commonly presents between **2-8 weeks of age** and leads to an obstruction of gastric outflow, causing the characteristic vomiting and signs of dehydration like **dry mucous membranes** and **delayed capillary refill**.
*Failure of neural crest cell migration into the rectum*
- This describes **Hirschsprung disease**, which typically presents with **constipation**, **abdominal distension**, and a **failure to pass meconium** in the neonatal period.
- While it involves GI obstruction, its symptoms and location of obstruction are distinctly different from the projectile vomiting seen in this case.
*Telescoping of the small bowel into the large bowel*
- This is known as **intussusception**, which usually presents with **intermittent, colicky abdominal pain**, **"currant jelly" stools** (due to blood and mucus), and a sausage-shaped abdominal mass, typically in older infants (3 months to 3 years).
- The type of vomiting (often bilious) and stool characteristics are different from the patient's presentation.
*Patent tract between the trachea and esophagus*
- This describes a **tracheoesophageal fistula (TEF)**, often associated with esophageal atresia. Infants with TEF typically present with **choking, coughing, and cyanosis** during feeds, as well as aspiration, due to misdirection of fluid into the lungs.
- The symptoms are immediate and severe with initial feeds and do not typically involve progressive projectile vomiting after several weeks of life.
*Failure of duodenal lumen recanalization*
- This leads to **duodenal atresia**, which typically presents with **bilious vomiting** within the first 24-48 hours of life, and the classic "double bubble" sign on X-ray.
- The vomiting in this case is **non-bilious** and started later, which rules out duodenal atresia.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 5: A 5-week-old infant boy presents to the pediatrician with intermittent vomiting for the last 2 weeks. The mother reports that the vomiting is non-bilious and immediately follows feeding. After vomiting, the baby is hungry and wants to feed again. The frequency of vomiting has been increasing progressively over 2 weeks. The vital signs are within normal limits. The examination of the abdomen reveals the presence of a firm mass of approx. 2 cm in length, above and to the right of the umbilicus. The mass is movable, olive-shaped, and hard on palpation. Which of the following is the most likely surgical treatment for this infant’s condition?
- A. Duodenoduodenostomy
- B. Pyloromyotomy (Correct Answer)
- C. Surgical ligation of the fistula and primary end-to-end anastomosis of the esophagus
- D. Diverticulectomy
- E. Endorectal pull-through procedure
Pyloric stenosis diagnosis and pyloromyotomy Explanation: **Pyloromyotomy**
- The clinical presentation of **non-bilious projectile vomiting** in an infant, immediately after feeding, with persistent hunger, and a palpable **olive-shaped mass** in the epigastrium, is classic for **hypertrophic pyloric stenosis**.
- **Pyloromyotomy (Ramstedt procedure)** is the definitive surgical treatment, which involves incising the hypertrophied muscle of the pylorus while leaving the mucosa intact, thereby relieving the obstruction.
*Duodenoduodenostomy*
- This procedure is typically performed to correct **duodenal atresia**, an anatomical blockage of the duodenum and presents from birth.
- Duodenal atresia usually causes **bilious vomiting** and is not associated with a palpable epigastric mass.
*Surgical ligation of the fistula and primary end-to-end anastomosis of the esophagus*
- This is the surgical treatment for **esophageal atresia with tracheoesophageal fistula**, which would present as choking, coughing, and respiratory distress during feeding from birth.
- It does not involve a palpable abdominal mass or progressive non-bilious vomiting.
*Diverticulectomy*
- This procedure is performed to remove a **Meckel's diverticulum**, which may present with painless rectal bleeding or intussusception, but not typically with projectile non-bilious vomiting or a palpable olive-shaped mass.
- Meckel's diverticulum is a congenital abnormality that is usually asymptomatic.
*Endorectal pull-through procedure*
- This is the standard surgical treatment for **Hirschsprung disease**, a condition characterized by the absence of ganglion cells in the distal colon, leading to functional obstruction.
- Hirschsprung disease typically presents with **constipation**, abdominal distension, and failure to pass meconium, not early-onset projectile vomiting or a palpable olive mass.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 6: A 42-year-old woman is brought to the emergency department because of a 5-day history of epigastric pain, fever, nausea, and malaise. Five weeks ago she had acute biliary pancreatitis and was treated with endoscopic retrograde cholangiopancreatography and subsequent cholecystectomy. Her maternal grandfather died of pancreatic cancer. She does not smoke. She drinks 1–2 beers daily. Her temperature is 38.7°C (101.7°F), respirations are 18/min, pulse is 120/min, and blood pressure is 100/70 mm Hg. Abdominal examination shows epigastric tenderness and three well-healed laparoscopy scars. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10 g/dL
Leukocyte count 15,800/mm3
Serum
Na+ 140 mEq/L
Cl− 103 mEq/L
K+ 4.5 mEq/L
HCO3- 25 mEq/L
Urea nitrogen 18 mg/dL
Creatinine 1.0 mg/dL
Alkaline phosphatase 70 U/L
Aspartate aminotransferase (AST, GOT) 22 U/L
Alanine aminotransferase (ALT, GPT) 19 U/L
γ-Glutamyltransferase (GGT) 55 U/L (N = 5–50)
Bilirubin 1 mg/dl
Glucose 105 mg/dL
Amylase 220 U/L
Lipase 365 U/L (N = 14–280)
Abdominal ultrasound shows a complex cystic fluid collection with irregular walls and septations in the pancreas. Which of the following is the most likely diagnosis?
- A. Pancreatic cancer
- B. Acute cholangitis
- C. Pancreatic abscess (Correct Answer)
- D. Pancreatic pseudocyst
- E. ERCP-induced pancreatitis
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***Pancreatic abscess***
- The presence of fever, leukocytosis (WBC 15,800/mm³), and a complex, septated fluid collection seen on ultrasound, following acute pancreatitis, is highly suggestive of a **pancreatic abscess**.
- **Pancreatic abscesses** develop as a complication of acute pancreatitis, typically resulting from infected pancreatic necrosis and often present with persistent symptoms of infection.
*Pancreatic cancer*
- While there is a family history of pancreatic cancer, her acute presentation with **fever, leukocytosis**, and a tender, complex fluid collection is **not typical** for initial pancreatic cancer presentation.
- Pancreatic cancer typically presents with **jaundice, weight loss**, and chronic abdominal pain rather than acute infectious symptoms and a fluid collection after pancreatitis.
*Acute cholangitis*
- Acute cholangitis is characterized by **Charcot's triad** (fever, jaundice, right upper quadrant pain) or **Reynold's pentad** (Charcot's triad plus altered mental status and hypotension).
- The patient's **normal bilirubin level** (1 mg/dL), absence of jaundice, and epigastric pain (not right upper quadrant specific) make acute cholangitis less likely, especially with a history of cholecystectomy.
*Pancreatic pseudocyst*
- A pancreatic pseudocyst is a **sterile** fluid collection without signs of active infection (e.g., fever, leukocytosis) and typically has well-defined, smooth walls rather than irregular walls or septations.
- While she has a fluid collection from pancreatitis, the **fever, leukocytosis, and irregular/septated walls** on ultrasound point away from a simple pseudocyst and towards an infected collection.
*ERCP-induced pancreatitis*
- ERCP-induced pancreatitis would have occurred **immediately after the procedure**, which was five weeks ago. The current symptoms occurring five weeks later suggest a complication of the initial pancreatitis, not a new induction.
- While ERCP can cause pancreatitis, this diagnosis refers to the initial event, not a **secondary infectious complication** manifesting weeks later.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 7: A 37-year-old man presents to the physician. He has been overweight since childhood. He has not succeeded in losing weight despite following different diet and exercise programs over the past several years. He has had diabetes mellitus for 2 years and severe gastroesophageal reflux disease for 9 years. His medications include metformin, aspirin, and pantoprazole. His blood pressure is 142/94 mm Hg, pulse is 76/min, and respiratory rate is 14/min. His BMI is 36.5 kg/m2. Laboratory studies show:
Hemoglobin A1C 6.6%
Serum
Fasting glucose 132 mg/dL
Which of the following is the most appropriate surgical management?
- A. No surgical management at this time
- B. Laparoscopic adjustable gastric banding
- C. Biliopancreatic diversion and duodenal switch (BPD-DS)
- D. Laparoscopic sleeve gastrectomy
- E. Laparoscopic Roux-en-Y gastric bypass (Correct Answer)
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***Laparoscopic Roux-en-Y gastric bypass***
- This patient meets criteria for bariatric surgery with a **BMI of 36.5 kg/m2** along with significant **comorbidities** such as **type 2 diabetes** and **severe GERD**.
- Roux-en-Y gastric bypass is particularly effective for **diabetes remission** and is the most effective bariatric procedure for **resolving GERD**, making it the most appropriate choice given his symptoms.
*No surgical management at this time*
- The patient has a high BMI (36.5 kg/m2) with multiple obesity-related comorbidities including **diabetes mellitus** and **severe GERD** that have not improved with lifestyle changes and medication.
- Delaying surgical management would allow his obesity and related conditions to potentially worsen, despite his efforts to lose weight through diet and exercise.
*Laparoscopic adjustable gastric banding*
- This procedure typically results in **less weight loss** compared to other bariatric surgeries and is less effective at resolving comorbidities like diabetes and GERD.
- It carries a higher rate of **long-term complications** such as band erosion or slippage, and would not address the patient's severe GERD effectively.
*Biliopancreatic diversion and duodenal switch (BPD-DS)*
- While BPD-DS leads to the most significant weight loss and diabetes remission, it is associated with a **higher risk of surgical complications** and **severe nutritional deficiencies**.
- Given the patient's BMI and comorbidities, a less aggressive procedure like Roux-en-Y gastric bypass offers a better risk-benefit profile, especially for GERD.
*Laparoscopic sleeve gastrectomy*
- Sleeve gastrectomy is an effective weight-loss procedure, but it can **worsen or induce GERD** in some patients due to changes in gastric anatomy and pressure.
- As the patient has severe GERD, this procedure would not be the optimal choice and could exacerbate his symptoms.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 8: A 6-year-old baby is brought to the hospital by her parents complaining about right upper quadrant pain. On examination the baby is found to have jaundice and palpable abdominal mass. USG of the baby is shown below. What is the most likely cause?
- A. Pseudo pancreatic cyst
- B. Hydatid cyst
- C. Choledochal cyst (Correct Answer)
- D. Amoebic liver abscess
- E. Biliary atresia
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***Choledochal cyst***
- The classic triad of **abdominal pain**, **jaundice**, and a **palpable right upper quadrant mass** in a child is highly suggestive of a choledochal cyst.
- The ultrasound image shows a **cystic dilatation of the common bile duct** (labeled X), which is the hallmark of a choledochal cyst.
*Pseudo pancreatic cyst*
- Pancreatic pseudocysts usually develop after **pancreatitis** or pancreatic trauma, and are typically located in the **epigastric region**.
- They are not directly associated with jaundice related to biliary obstruction, though large cysts can cause obstruction via compression.
*Hydatid cyst*
- Hydatid cysts are typically seen in the **liver** and are caused by *Echinococcus granulosus*, often presenting with a **multiloculated appearance** and daughter cysts.
- While they can cause hepatomegaly and pain, jaundice and a palpable mass, they do not typically manifest as a primary dilatation of the bile duct.
*Amoebic liver abscess*
- An amoebic liver abscess is caused by *Entamoeba histolytica* and typically presents with **fever**, **right upper quadrant pain**, and sometimes hepatomegaly.
- While it can cause biliary obstruction in rare cases, the ultrasound appearance is usually that of a **hypoechoic lesion** within the liver parenchyma, not a distinct cystic dilatation of the bile duct.
*Biliary atresia*
- Biliary atresia typically presents in **early infancy** (first 2-3 months of life) with progressive jaundice and acholic stools.
- While it causes biliary obstruction, the ultrasound findings show **absent or atretic bile ducts** rather than cystic dilatation, and the age of presentation (6 years) makes this diagnosis unlikely.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 9: A 12-year-old patient with esophageal varices is managed by the procedure shown in the image. All of the following statements regarding this condition are true except:
- A. Sengstaken-Blakemore tube
- B. Gastric balloon is inflated with 400 mL of air
- C. Esophageal balloon is inflated with 40 mm Hg pressure of air
- D. This is the definitive treatment (Correct Answer)
- E. Should be kept inflated for a maximum of 24-48 hours
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***This is the definitive treatment***
- The image shows a **Sengstaken-Blakemore tube** being used, which is a temporary measure for controlling **bleeding esophageal varices**.
- It is an emergency treatment used for stabilization and does not address the underlying cause of varices or prevent future bleeding.
- **Definitive treatments** include endoscopic variceal ligation (EVL), sclerotherapy, or TIPS procedure.
*Sengstaken-Blakemore tube*
- The device shown in the image, with balloons and multiple lumens, is indeed a **Sengstaken-Blakemore tube**, used for **tamponade of actively bleeding esophageal varices**.
- This tube features a gastric balloon and an esophageal balloon, along with lumens for suction, designed to exert pressure on the bleeding varices.
*Gastric balloon is inflated with 400 mL of air*
- The **gastric balloon** of a Sengstaken-Blakemore tube is typically inflated with **200-500 mL of air** (often around 250-300 ml in adults, 150 ml in children) to anchor the tube and compress gastric varices.
- While 400 mL is within the general range, the exact volume can vary based on patient size and clinical protocol.
*Esophageal balloon is inflated with 40 mm Hg pressure of air*
- The **esophageal balloon** is indeed inflated to a pressure of **20-45 mmHg (typically 30-45 mmHg)** to compress esophageal varices.
- This pressure application is critical for achieving local hemostasis in acute bleeding episodes.
*Should be kept inflated for a maximum of 24-48 hours*
- The balloons should be deflated after **24-48 hours maximum** to prevent complications such as **esophageal necrosis, ulceration, or perforation**.
- Prolonged inflation can cause pressure necrosis of the esophageal or gastric mucosa.
Pyloric stenosis diagnosis and pyloromyotomy US Medical PG Question 10: What does the intraoperative image shown below depict?
- A. Transverse colon volvulus
- B. Meckel's diverticulum
- C. Intussusception (Correct Answer)
- D. Intestinal duplication cyst
- E. Malrotation with midgut volvulus
Pyloric stenosis diagnosis and pyloromyotomy Explanation: ***Intussusception***
- The image clearly shows a segment of bowel telescoping into an adjacent segment, characteristic of **intussusception**
- This condition involves the invagination of one part of the intestine into another, often presenting clinically with abdominal pain, vomiting, and **"red jelly" stools**
- The classic intraoperative finding is the appearance of bowel within bowel, creating a sausage-shaped mass
*Transverse colon volvulus*
- **Transverse colon volvulus** involves the twisting of the transverse colon around its mesentery, which would appear as a dilated, twisted loop of bowel
- The image does not show the characteristic twisting or significant dilation associated with a volvulus
*Meckel's diverticulum*
- A **Meckel's diverticulum** is a true diverticulum, a remnant of the vitelline duct, which appears as a small pouch or bulge on the wall of the small intestine
- The image depicts a larger-scale bowel obstruction caused by one segment of bowel entering another, not an abnormal outpouching
*Intestinal duplication cyst*
- **Intestinal duplication cysts** are spherical or tubular structures that share a common wall with the bowel and are lined with gastrointestinal mucosa
- These appear as separate cystic masses adjacent to the bowel, not as telescoping segments
*Malrotation with midgut volvulus*
- **Malrotation with midgut volvulus** presents with twisting of the small bowel around the superior mesenteric artery, creating a characteristic "whirlpool" or "corkscrew" appearance
- The image shows telescoping of bowel segments rather than the rotational twisting pattern seen in volvulus
More Pyloric stenosis diagnosis and pyloromyotomy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.