Necrotizing enterocolitis surgical management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Necrotizing enterocolitis surgical management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Necrotizing enterocolitis surgical management US Medical PG Question 1: A four-week-old female is evaluated in the neonatal intensive care unit for feeding intolerance with gastric retention of formula. She was born at 25 weeks gestation to a 32-year-old gravida 1 due to preterm premature rupture of membranes at 24 weeks gestation. The patient’s birth weight was 750 g (1 lb 10 oz). She required resuscitation with mechanical ventilation at the time of delivery, but she was subsequently extubated to continuous positive airway pressure (CPAP) and then weaned to nasal cannula. The patient was initially receiving both parenteral nutrition and enteral feeds through a nasogastric tube, but she is now receiving only continuous nasogastric formula feeds. Her feeds are being advanced to a target weight gain of 20-30 g per day. Her current weight is 1,350 g (2 lb 16 oz). The patient’s temperature is 97.2°F (36.2°C), blood pressure is 72/54 mmHg, pulse is 138/min, respirations are 26/min, and SpO2 is 96% on 4L nasal cannula. On physical exam, the patient appears lethargic. Her abdomen is soft and markedly distended. Digital rectal exam reveals stool streaked with blood in the rectal vault.
Which of the following abdominal radiographs would most likely be seen in this patient?
- A. Air in the biliary tree
- B. Normal bowel gas pattern
- C. Dilated loops of bowel
- D. Pneumoperitoneum
- E. Pneumatosis intestinalis (Correct Answer)
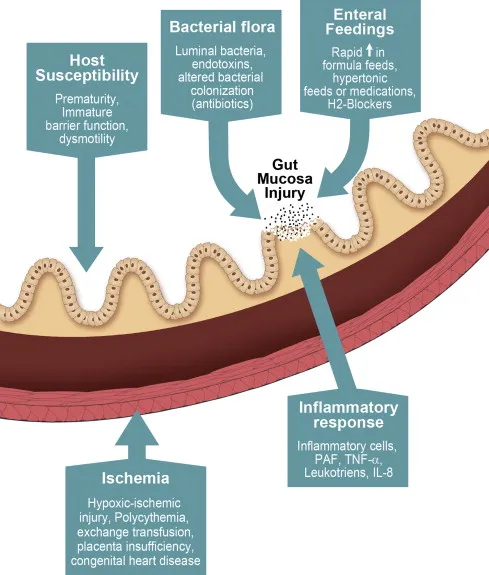
Necrotizing enterocolitis surgical management Explanation: ***Pneumatosis intestinalis***
- The patient's presentation with **feeding intolerance**, **abdominal distension**, **lethargy**, and **bloody stools** in a premature infant is highly suspicious for **necrotizing enterocolitis (NEC)**.
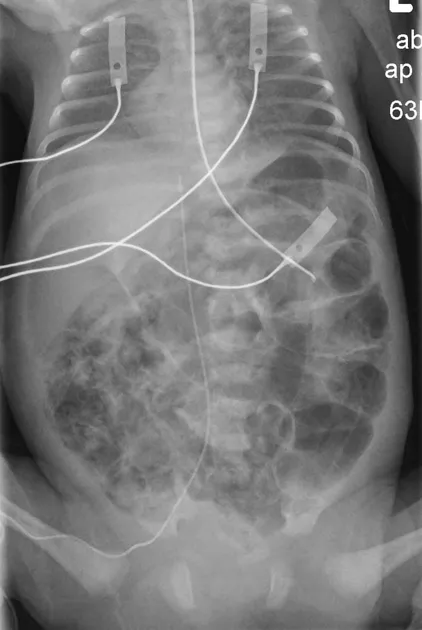
- **Pneumatosis intestinalis**, which is gas within the bowel wall, is the **pathognomonic radiographic sign of NEC**. The image clearly shows intramural gas (black arrows and white arrows with arrowheads point to gas within the bowel wall), which is indicative of this condition.
*Air in the biliary tree*
- Air in the biliary tree (pneumobilia) is typically associated with conditions such as a **gallstone ileus**, surgical anastomosis (e.g., choledochojejunostomy), or an incompetent sphincter of Oddi, none of which are indicated by the patient's symptoms or risk factors.
- While it's an abnormal finding, it does not directly explain the clinical picture of a premature infant with feeding intolerance and bloody stools, which strongly points to NEC.
*Normal bowel gas pattern*
- The patient presents with significant symptoms including **marked abdominal distension**, **lethargy**, **feeding intolerance**, and **bloody stools**. A normal bowel gas pattern would be inconsistent with these severe clinical signs.
- In a premature infant with suspected NEC, a normal study is possible early in the disease but usually progresses to show signs of bowel pathology.
*Dilated loops of bowel*
- While **dilated bowel loops** can be seen in NEC, they are a non-specific finding and can occur in various conditions causing **bowel obstruction** or ileus.
- **Pneumatosis intestinalis** is a more specific and advanced radiographic sign of NEC, indicating gas produced by bacteria invading the bowel wall, and is therefore a more definitive finding for this condition.
*Pneumoperitoneum*
- **Pneumoperitoneum**, or free air in the abdomen, indicates **bowel perforation**, which is a severe complication of necrotizing enterocolitis.
- While NEC can lead to pneumoperitoneum, the image provided shows gas *within* the bowel wall (pneumatosis), not free air *outside* the bowel. Pneumoperitoneum would typically manifest as air under the diaphragm on an upright film or a Football sign on a supine film.
Necrotizing enterocolitis surgical management US Medical PG Question 2: A 32-year-old man comes to the emergency department because of recurrent episodes of vomiting for 1 day. He has had over 15 episodes of bilious vomiting. During this period he has had cramping abdominal pain but has not had a bowel movement or passed flatus. He does not have fever or diarrhea. He was diagnosed with Crohn disease at the age of 28 years which has been well controlled with oral mesalamine. He underwent a partial small bowel resection for midgut volvulus at birth. His other medications include vitamin B12, folic acid, loperamide, ferrous sulfate, and vitamin D3. He appears uncomfortable and his lips are parched. His temperature is 37.1°C (99.3°F), pulse is 103/min, and blood pressure is 104/70 mm Hg. The abdomen is distended, tympanitic, and tender to palpation over the periumbilical area and the right lower quadrant. Rectal examination is unremarkable. A CT scan of the abdomen shows multiple dilated loops of small bowel with a transition zone in the mid to distal ileum. After 24 hours of conservative management with IV fluid resuscitation, nasogastric bowel decompression, promethazine, and analgesia, his condition does not improve and a laparotomy is scheduled. During the laparotomy, two discrete strictures are noted in the mid-ileum, around 20 cm apart. Which of the following is the most appropriate next step in management?
- A. Small bowel resection with ileostomy
- B. Abdominal closure and start palliative care
- C. Small bowel resection and primary anastomosis
- D. Strictureplasty of individual strictures (Correct Answer)
- E. Ileocolectomy
Necrotizing enterocolitis surgical management Explanation: ***Strictureplasty of individual strictures***
- This patient presents with **multiple strictures** in the mid-ileum causing a small bowel obstruction in the setting of **Crohn's disease**. Strictureplasty is the preferred surgical approach for *short, multiple (up to four), or recurrent Crohn's disease strictures* as it preserves bowel length.
- While small bowel resection is an option, **strictureplasty** is favored in Crohn's disease to *avoid short bowel syndrome*, especially if multiple strictures are present, as seen here.
*Small bowel resection with ileostomy*
- An ileostomy is typically created when a primary anastomosis is not safe due to high risk of leak (e.g., severe inflammation, peritonitis, patient instability) or when there is extensive disease not amenable to strictureplasty with primary anastomosis.
- Performing an ileostomy when primary anastomosis is possible unnecessarily creates a stoma, which can lead to complications and impact quality of life.
*Abdominal closure and start palliative care*
- This patient, while acutely unwell, has a surgically correctable cause for his obstruction and is not described as having an incurable or end-stage condition necessitating only palliative care.
- Palliative care would be considered for patients with widespread untreatable disease or severe comorbidities, which is not indicated here given the localized, treatable strictures.
*Small bowel resection and primary anastomosis*
- While small bowel resection is a valid treatment for isolated, non-recurrent strictures, strictureplasty is generally preferred in Crohn's disease when multiple strictures are present.
- **Resection of multiple segments** can lead to significant **short bowel syndrome**, especially in a patient with a history of prior small bowel resection, making strictureplasty a more bowel-sparing and appropriate choice.
*Ileocolectomy*
- **Ileocolectomy** involves resection of the terminal ileum and a portion of the colon. This would be indicated if the disease involves the *ileocecal valve region* or the *colon*, which is not the case in this patient, whose strictures are in the mid-ileum.
- This procedure is excessive for mid-ileal strictures and would result in unnecessary removal of healthy bowel given the location of the strictures.
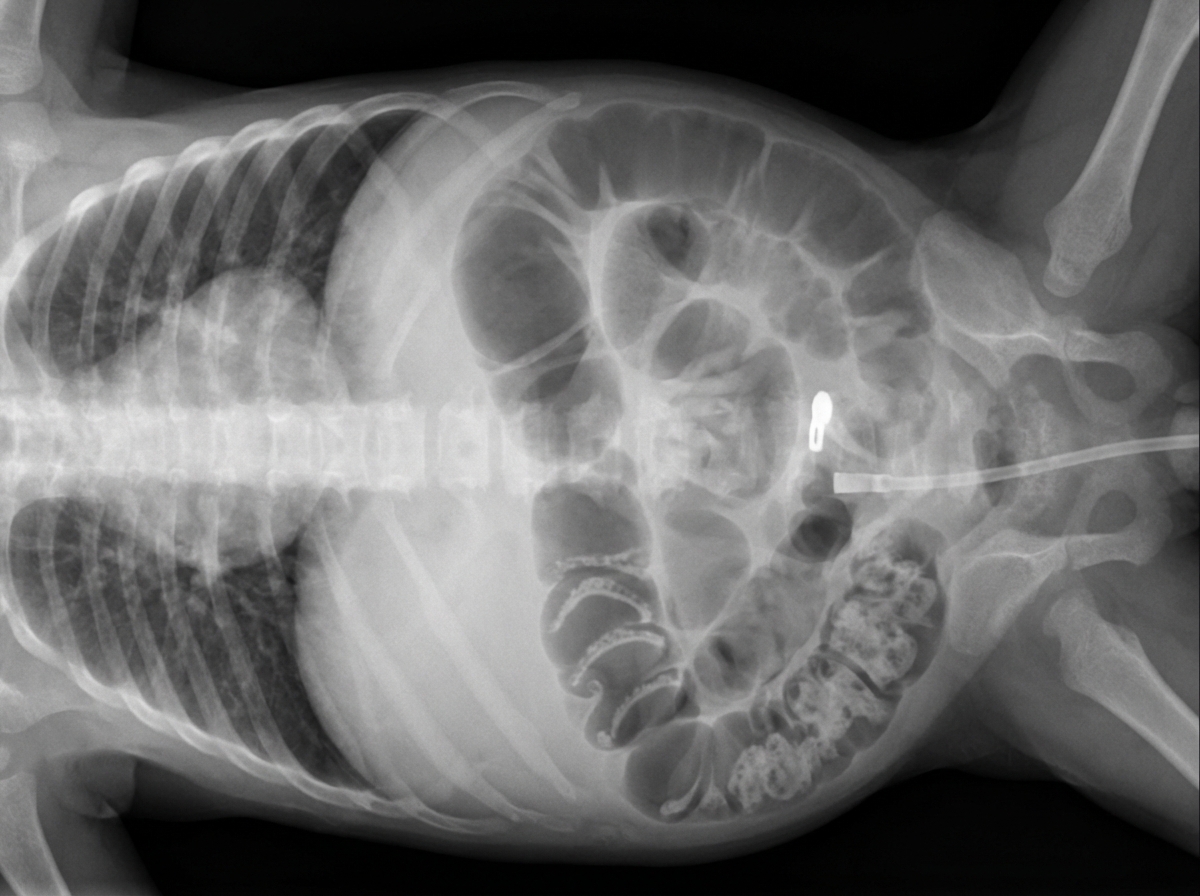
Necrotizing enterocolitis surgical management US Medical PG Question 3: An institutionalized 65-year-old man is brought to the emergency department because of abdominal pain and distension for 12 hours. The pain was acute in onset and is a cramping-type pain associated with nausea, vomiting, and constipation. He has a history of chronic constipation and has used laxatives for years. There is no history of inflammatory bowel disease in his family. He has not been hospitalized recently. There is no recent history of weight loss or change in bowel habits. On physical examination, the patient appears ill. The abdomen is distended with tenderness mainly in the left lower quadrant and is tympanic on percussion. The blood pressure is 110/79 mm Hg, heart rate is 100/min, the respiratory rate is 20/min, and the temperature is 37.2°C (99.0°F). The CBC shows an elevated white blood cell count. The plain abdominal X-ray is shown in the accompanying image. What is the most likely cause of his condition?
- A. Sigmoid volvulus (Correct Answer)
- B. Intussusception
- C. Acute diverticulitis
- D. Toxic megacolon
- E. Colon cancer
Necrotizing enterocolitis surgical management Explanation: ***Sigmoid volvulus***
- The patient’s symptoms of acute **abdominal pain**, distension, and cramping strongly indicate **sigmoid volvulus**, often seen in chronic constipation and institutionalized patients.
- Physical examination revealing **tenderness in the left lower quadrant** and a tympanic abdomen supports the diagnosis of bowel obstruction typically caused by **volvulus**.
*Intussusception*
- Generally presents with **currant jelly stools** and is more common in children; the acute symptoms here are less typical.
- It often involves a **lead point** or associated conditions like **polyps** or tumors, which are not indicated in this case.
*Acute diverticulitis*
- Usually associated with **localized pain** in the left lower quadrant but would present with fever and changes in bowel habits, which the patient lacks.
- Typically shows **peritoneal signs** and may have complications like abscess or perforation, not indicated here.
*Toxic megacolon*
- Commonly associated with underlying **inflammatory bowel disease** or infections, not indicated in this patient with no recent history of **IBD**.
- Symptoms would include severe **diarrhea** and abdominal pain, which do not fit the current acute cramping and constipation pattern.
*Colon cancer*
- While it can cause abdominal symptoms, it presents more insidiously with **weight loss** or **change in bowel habits**, none of which are reported here.
- The acute presentation and findings do not align with a malignancy, which would often be chronic in nature.
Necrotizing enterocolitis surgical management US Medical PG Question 4: A 13-year-old boy is brought to the emergency department by his mother because of vomiting and severe testicular pain for 3 hours. The boy has had 4–5 episodes of vomiting during this period. He has never had a similar episode in the past and takes no medications. His father died of testicular cancer at the age of 50. His immunizations are up-to-date. He appears anxious and uncomfortable. His temperature is 37°C (98.6°F), pulse is 90/min, respirations are 14/min, and blood pressure is 100/60 mm Hg. Cardiopulmonary examination shows no abnormalities The abdomen is soft and nondistended. The left scrotum is firm, erythematous, and swollen. There is severe tenderness on palpation of the scrotum that persists on elevation of the testes. Stroking the inner side of the left thigh fails to elicit elevation of the scrotum. Which of the following is the most appropriate next step in management?
- A. Urine dipstick
- B. Ceftriaxone and doxycycline therapy
- C. Close observation
- D. CT scan of the abdomen and pelvis
- E. Surgical exploration of the scrotum (Correct Answer)
Necrotizing enterocolitis surgical management Explanation: ***Surgical exploration of the scrotum***
- The sudden onset of severe testicular pain, vomiting, an **absent cremasteric reflex**, and testicular tenderness that **persists on elevation (negative Prehn's sign)** are highly suggestive of **testicular torsion**.
- **Testicular torsion** is a surgical emergency requiring immediate exploration to salvage the testis; delaying surgery beyond 6-8 hours significantly increases the risk of **testicular ischemia** and necrosis.
*Urine dipstick*
- While a **urine dipstick** can help rule out a **urinary tract infection** or **epididymitis**, these conditions typically present with more gradual pain and often have associated urinary symptoms, which are not the primary concern here.
- Delaying definitive treatment for a suspected **testicular torsion** by performing non-urgent diagnostic tests can lead to irreversible damage to the testis.
*Ceftriaxone and doxycycline therapy*
- This antibiotic regimen is typically used to treat **epididymitis** or **orchitis**, especially in sexually active adolescents, or cases suspected of bacterial infection.
- The acute, severe nature of the pain and the absence of fever or urinary symptoms make **bacterial epididymitis** less likely, and administering antibiotics would delay the critical intervention needed for **testicular torsion**.
*Close observation*
- **Close observation** is inappropriate given the highly suspicious symptoms of **testicular torsion**, which is a time-sensitive emergency.
- Delaying intervention can result in irreversible **ischemic damage** to the testicle, leading to its loss.
*CT scan of the abdomen and pelvis*
- A **CT scan** is not the appropriate initial diagnostic step for acute scrotal pain; it exposes the patient to radiation and would delay definitive diagnosis and treatment.
- While it could identify other sources of abdominal pain, the clinical presentation is characteristic of a local scrotal pathology, and **ultrasound with Doppler** is preferred if imaging is needed to confirm **testicular torsion**, though clinical suspicion often warrants direct surgical exploration.
Necrotizing enterocolitis surgical management US Medical PG Question 5: A 27-year-old man is brought to the emergency department by ambulance following a motor vehicle accident 1 hour prior. He appears agitated. His blood pressure is 85/60 mm Hg, the pulse is 110/min, and the respiratory rate is 19/min. Physical examination shows bruising of the left flank and fracture of the left lower thoracic bones. Strict bed rest and monitoring with intravenous fluids is initiated. Urinalysis shows numerous RBCs. A contrast-enhanced CT scan shows normal enhancement of the right kidney. The left renal artery is only visible in the proximal section with a small amount of extravasated blood around the left kidney. The left kidney shows no enhancement. Imaging of the spleen shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Immediate surgical exploration (Correct Answer)
- B. Observation with delayed repair
- C. Conservative management
- D. Renal artery embolization
- E. Renal artery embolization with delayed nephrectomy
Necrotizing enterocolitis surgical management Explanation: ***Immediate surgical exploration***
- The patient presents with signs of **hemodynamic instability** (BP 85/60, pulse 110/min, agitation) and imaging findings consistent with **left renal artery avulsion** and devascularization (no enhancement of the left kidney, visible only proximally, extravasated blood). These findings necessitate immediate surgical intervention to control hemorrhage and assess kidney viability.
- The goal is to revascularize the kidney if possible, perform a nephrectomy if the kidney is unsalvageable, and manage hemorrhage to stabilize the patient.
*Observation with delayed repair*
- This approach is typically reserved for **hemodynamically stable** patients with renal injuries, especially lower-grade injuries that do not involve complete vessel avulsion or ongoing significant hemorrhage.
- Delaying intervention in a hemodynamically unstable patient with a presumed renal artery avulsion can lead to further decompensation, irreversible kidney damage, and increased mortality.
*Conservative management*
- **Conservative management** is appropriate for hemodynamically stable patients with minor renal injuries, such as contusions or small lacerations, or for very selected cases of more severe injuries that have spontaneously tamponaded and are not causing significant clinical compromise.
- The patient's **hemodynamic instability** and direct evidence of renal artery injury preclude conservative management in this case.
*Renal artery embolization*
- **Renal artery embolization** is a highly effective, minimally invasive technique for controlling bleeding from renal injuries. However, it is primarily indicated for **hemodynamically stable patients** with contained hemorrhage or specific pseudoaneurysms/AV fistulas.
- In a hemodynamically unstable patient with a complete renal artery avulsion and non-perfused kidney, embolization is unlikely to revascularize the kidney and may even hinder subsequent surgical repair if revascularization is deemed possible. Furthermore, it might not be sufficient to control diffuse or extensive bleeding associated with avulsion.
*Renal artery embolization with delayed nephrectomy*
- While embolization can precede nephrectomy in certain scenarios for better hemorrhage control, it is not the primary immediate step in a **hemodynamically unstable** patient with renal artery avulsion and a non-enhancing kidney.
- The primary concern is the patient's instability, which requires immediate surgical control, and delaying nephrectomy after embolization often isn't feasible if the kidney is completely devascularized and the patient is unstable. The decision for nephrectomy typically occurs during the initial surgical exploration.
Necrotizing enterocolitis surgical management US Medical PG Question 6: Three days after being admitted to the hospital because of a fall from the roof of a two-story building, a 27-year-old man is being monitored in the intensive care unit. On arrival, the patient was somnolent and not oriented to person, place, or time. A CT scan of the head showed an epidural hemorrhage that was 45 cm3 in size and a midline shift of 7 mm. Emergency surgery was performed with craniotomy and hematoma evacuation on the day of admission. Perioperatively, a bleeding vessel was identified and ligated. Postoperatively, the patient was transferred to the intensive care unit and placed on a ventilator. His temperature is 37°C (98.6°F), pulse is 67/min, and blood pressure is 117/78 mm Hg. The ventilator is set at a FiO2 of 55%, tidal volume of 520 mL, and positive end-expiratory pressure of 5.0 cm H2O. In addition to intravenous administration of fluids, which of the following is the most appropriate next step in managing this patient's nutrition?
- A. Enteral feeding via nasogastric tube (Correct Answer)
- B. Oral feeding
- C. Keep patient NPO
- D. Total parenteral nutrition
- E. Enteral feeding using a percutaneous endoscopic gastrostomy (PEG) tube
Necrotizing enterocolitis surgical management Explanation: ***Enteral feeding via nasogastric tube***
- This patient has been **somnolent** and on a ventilator for 3 days after a significant head injury, indicating a prolonged period without oral intake and an inability to protect his airway for oral feeding. **Early enteral nutrition** via a nasogastric tube is preferred in critically ill patients, especially those with head injuries, as it helps maintain gut integrity and reduces complications compared to parenteral nutrition.
- The patient's **hemodynamic stability** (blood pressure and pulse are within a reasonable range for a ventilated patient) suggests he can tolerate enteral feeding, and there are no signs of gut ischemia or ileus that would contraindicate it.
*Enteral feeding using a percutaneous endoscopic gastrostomy (PEG) tube*
- While a PEG tube provides enteral nutrition, it is typically reserved for patients requiring **long-term enteral support** (usually more than 4-6 weeks) or those who cannot tolerate a nasogastric tube.
- Given that it has only been 3 days post-injury, a **less invasive method** like a nasogastric tube is initially preferred.
*Oral feeding*
- The patient is described as **somnolent** and on a ventilator, meaning he is not awake enough or able to protect his airway to safely receive oral feeding.
- Attempting oral feeding in this state carries a high risk of **aspiration pneumonia**.
*Keep patient NPO*
- Keeping the patient NPO (nil per os) for an extended period in critical illness is associated with several negative outcomes, including **gut mucosal atrophy, increased infection risk**, and poorer clinical outcomes.
- After 3 days, initiating nutritional support is crucial to prevent these complications.
*Total parenteral nutrition*
- **Total parenteral nutrition (TPN)** is generally considered a last resort when the gastrointestinal tract is non-functional or enteral feeding is contraindicated.
- TPN is associated with a **higher risk of complications**, such as central line infections, liver dysfunction, and metabolic disturbances, compared to enteral feeding.
Necrotizing enterocolitis surgical management US Medical PG Question 7: A 6-year-old baby is brought to the hospital by her parents complaining about right upper quadrant pain. On examination the baby is found to have jaundice and palpable abdominal mass. USG of the baby is shown below. What is the most likely cause?
- A. Pseudo pancreatic cyst
- B. Hydatid cyst
- C. Choledochal cyst (Correct Answer)
- D. Amoebic liver abscess
- E. Biliary atresia
Necrotizing enterocolitis surgical management Explanation: ***Choledochal cyst***
- The classic triad of **abdominal pain**, **jaundice**, and a **palpable right upper quadrant mass** in a child is highly suggestive of a choledochal cyst.
- The ultrasound image shows a **cystic dilatation of the common bile duct** (labeled X), which is the hallmark of a choledochal cyst.
*Pseudo pancreatic cyst*
- Pancreatic pseudocysts usually develop after **pancreatitis** or pancreatic trauma, and are typically located in the **epigastric region**.
- They are not directly associated with jaundice related to biliary obstruction, though large cysts can cause obstruction via compression.
*Hydatid cyst*
- Hydatid cysts are typically seen in the **liver** and are caused by *Echinococcus granulosus*, often presenting with a **multiloculated appearance** and daughter cysts.
- While they can cause hepatomegaly and pain, jaundice and a palpable mass, they do not typically manifest as a primary dilatation of the bile duct.
*Amoebic liver abscess*
- An amoebic liver abscess is caused by *Entamoeba histolytica* and typically presents with **fever**, **right upper quadrant pain**, and sometimes hepatomegaly.
- While it can cause biliary obstruction in rare cases, the ultrasound appearance is usually that of a **hypoechoic lesion** within the liver parenchyma, not a distinct cystic dilatation of the bile duct.
*Biliary atresia*
- Biliary atresia typically presents in **early infancy** (first 2-3 months of life) with progressive jaundice and acholic stools.
- While it causes biliary obstruction, the ultrasound findings show **absent or atretic bile ducts** rather than cystic dilatation, and the age of presentation (6 years) makes this diagnosis unlikely.
Necrotizing enterocolitis surgical management US Medical PG Question 8: A 12-year-old patient with esophageal varices is managed by the procedure shown in the image. All of the following statements regarding this condition are true except:
- A. Sengstaken-Blakemore tube
- B. Gastric balloon is inflated with 400 mL of air
- C. Esophageal balloon is inflated with 40 mm Hg pressure of air
- D. This is the definitive treatment (Correct Answer)
- E. Should be kept inflated for a maximum of 24-48 hours
Necrotizing enterocolitis surgical management Explanation: ***This is the definitive treatment***
- The image shows a **Sengstaken-Blakemore tube** being used, which is a temporary measure for controlling **bleeding esophageal varices**.
- It is an emergency treatment used for stabilization and does not address the underlying cause of varices or prevent future bleeding.
- **Definitive treatments** include endoscopic variceal ligation (EVL), sclerotherapy, or TIPS procedure.
*Sengstaken-Blakemore tube*
- The device shown in the image, with balloons and multiple lumens, is indeed a **Sengstaken-Blakemore tube**, used for **tamponade of actively bleeding esophageal varices**.
- This tube features a gastric balloon and an esophageal balloon, along with lumens for suction, designed to exert pressure on the bleeding varices.
*Gastric balloon is inflated with 400 mL of air*
- The **gastric balloon** of a Sengstaken-Blakemore tube is typically inflated with **200-500 mL of air** (often around 250-300 ml in adults, 150 ml in children) to anchor the tube and compress gastric varices.
- While 400 mL is within the general range, the exact volume can vary based on patient size and clinical protocol.
*Esophageal balloon is inflated with 40 mm Hg pressure of air*
- The **esophageal balloon** is indeed inflated to a pressure of **20-45 mmHg (typically 30-45 mmHg)** to compress esophageal varices.
- This pressure application is critical for achieving local hemostasis in acute bleeding episodes.
*Should be kept inflated for a maximum of 24-48 hours*
- The balloons should be deflated after **24-48 hours maximum** to prevent complications such as **esophageal necrosis, ulceration, or perforation**.
- Prolonged inflation can cause pressure necrosis of the esophageal or gastric mucosa.
Necrotizing enterocolitis surgical management US Medical PG Question 9: What does the intraoperative image shown below depict?
- A. Transverse colon volvulus
- B. Meckel's diverticulum
- C. Intussusception (Correct Answer)
- D. Intestinal duplication cyst
- E. Malrotation with midgut volvulus
Necrotizing enterocolitis surgical management Explanation: ***Intussusception***
- The image clearly shows a segment of bowel telescoping into an adjacent segment, characteristic of **intussusception**
- This condition involves the invagination of one part of the intestine into another, often presenting clinically with abdominal pain, vomiting, and **"red jelly" stools**
- The classic intraoperative finding is the appearance of bowel within bowel, creating a sausage-shaped mass
*Transverse colon volvulus*
- **Transverse colon volvulus** involves the twisting of the transverse colon around its mesentery, which would appear as a dilated, twisted loop of bowel
- The image does not show the characteristic twisting or significant dilation associated with a volvulus
*Meckel's diverticulum*
- A **Meckel's diverticulum** is a true diverticulum, a remnant of the vitelline duct, which appears as a small pouch or bulge on the wall of the small intestine
- The image depicts a larger-scale bowel obstruction caused by one segment of bowel entering another, not an abnormal outpouching
*Intestinal duplication cyst*
- **Intestinal duplication cysts** are spherical or tubular structures that share a common wall with the bowel and are lined with gastrointestinal mucosa
- These appear as separate cystic masses adjacent to the bowel, not as telescoping segments
*Malrotation with midgut volvulus*
- **Malrotation with midgut volvulus** presents with twisting of the small bowel around the superior mesenteric artery, creating a characteristic "whirlpool" or "corkscrew" appearance
- The image shows telescoping of bowel segments rather than the rotational twisting pattern seen in volvulus
Necrotizing enterocolitis surgical management US Medical PG Question 10: Which of the following is true regarding this condition?
- A. Most common site is anterior triangle neck
- B. It is due to vascular malformation
- C. Usually decreases on crying
- D. Needle aspiration yields fluid that does not coagulate (Correct Answer)
- E. Typically appears after 5 years of age
Necrotizing enterocolitis surgical management Explanation: ***Needle aspiration yields fluid that does not coagulate***
- The image depicts a large, translucent, fluid-filled cystic mass, characteristic of a **cystic hygroma** (lymphatic malformation).
- Aspiration of a cystic hygroma typically yields **clear to straw-colored fluid** that is rich in protein but **does not coagulate** because it is lymphatic fluid, not blood.
*Most common site is anterior triangle neck*
- While cystic hygromas most commonly occur in the **neck**, they are typically found in the **posterior triangle**, not the anterior triangle.
- The lesion in the image appears to be a large, diffuse cystic mass extending from the neck into the mediastinum or axilla.
*It is due to vascular malformation*
- This condition is a **lymphatic malformation**, specifically a cystic hygroma, not a vascular malformation.
- **Vascular malformations** involve blood vessels and would typically present with different characteristics, such as being compressible and potentially blanching.
*Usually decreases on crying*
- Crying or straining typically **increases the size** of a cystic hygroma due to increased intrathoracic pressure, which impedes lymphatic flow and causes distention of the lymphatic sacs.
- This characteristic helps differentiate it from conditions that might decrease in size with pressure.
*Typically appears after 5 years of age*
- Cystic hygromas are **congenital malformations** that are usually present at birth or become apparent within the **first 2 years of life** (approximately 90% by age 2).
- Late presentation after 5 years of age is uncommon and would be unusual for this condition.
More Necrotizing enterocolitis surgical management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.