Intussusception reduction techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Intussusception reduction techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Intussusception reduction techniques US Medical PG Question 1: A 4-week-old infant is brought to the emergency department by his parents with violent vomiting. It started about 3 days ago and has slowly gotten worse. He vomits after most feedings but seems to keep some formula down. His mother notes that he is eager to feed between episodes and seems to be putting on weight. Other than an uncomplicated course of chlamydia conjunctivitis, the infant has been healthy. He was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The physical exam is significant for a palpable mass in the right upper quadrant. What is the first-line confirmatory diagnostic test and associated finding?
- A. Abdominal ultrasound; elongated pyloric channel and muscle hypertrophy (Correct Answer)
- B. Barium upper GI series; GE junction and portion of the stomach in thorax
- C. Air enema; filling defect and coil spring sign
- D. Barium upper GI series; bird beak sign and corkscrewing
- E. Abdominal X-ray; ‘double bubble’ sign
Intussusception reduction techniques Explanation: ***Abdominal ultrasound; elongated pyloric channel and muscle hypertrophy***
- The clinical picture of **projectile vomiting** in a 4-week-old infant, **eagerness to feed** ("hungry vomiter"), and **palpable olive-shaped mass** in the right upper quadrant is classic for **pyloric stenosis**.
- **Abdominal ultrasonography** is the gold standard for diagnosis, revealing an **elongated pyloric channel** (>16mm) and thickened pyloric muscle (>3-4mm).
- Pyloric stenosis typically presents between 3-6 weeks of age with progressive non-bilious vomiting.
*Barium upper GI series; GE junction and portion of the stomach in thorax*
- A **barium upper GI series** showing the **GE junction and stomach in the thorax** would indicate a **hiatal hernia**, which is not consistent with the palpable mass or "hungry vomiter" presentation.
- While hiatal hernias can cause vomiting and reflux, they typically don't present with this specific type of projectile vomiting or a palpable abdominal mass.
*Air enema; filling defect and coil spring sign*
- An **air enema** showing a **filling defect** and **coil spring sign** is characteristic of **intussusception**, which usually presents with sudden onset of **crampy abdominal pain**, **currant jelly stools**, and a palpable mass in the right lower quadrant.
- The clinical presentation does not fit intussusception, which typically occurs in older infants (6-36 months) and has a more acute presentation.
*Barium upper GI series; bird beak sign and corkscrewing*
- A **barium upper GI series** showing a **bird beak sign** and **corkscrewing** is pathognomonic for **midgut volvulus**, a surgical emergency.
- While volvulus can cause bilious vomiting and abdominal distension, the presentation of non-bilious vomiting with a palpable pyloric mass is more typical of pyloric stenosis.
*Abdominal X-ray; 'double bubble' sign*
- An **abdominal X-ray** revealing a **'double bubble' sign** is indicative of **duodenal atresia** or **annular pancreas**, leading to complete duodenal obstruction.
- This condition typically presents with **bilious vomiting** shortly after birth (within first day of life) and does not involve a palpable hypertrophied pylorus.
Intussusception reduction techniques US Medical PG Question 2: A 7-month-old boy is brought to the ED by his mother because of abdominal pain. Two weeks ago, she noticed he had a fever and looser stools, but both resolved after a few days. One week ago, he began to experience periodic episodes during which he would curl up into a ball, scream, and cry. The episodes lasted a few minutes, and were occasionally followed by vomiting. Between events, he was completely normal. She says the episodes have become more frequent over time, and this morning, she noticed blood in his diaper. In the ED, his vitals are within normal ranges, and his physical exam is normal. After confirming the diagnosis with an abdominal ultrasound, what is the next step in management?
- A. Supportive care
- B. Broad-spectrum antibiotics
- C. Air contrast enema (Correct Answer)
- D. Abdominal laparotomy
- E. Abdominal CT scan
Intussusception reduction techniques Explanation: ***Air contrast enema***
- An **air contrast enema** is both diagnostic and therapeutic for **intussusception**, which is strongly suggested by the patient's symptoms (colicky abdominal pain, drawing legs to chest, currant jelly stools).
- It uses air pressure to **reduce the intussusception**, avoiding surgery if successful and the bowel is not compromised.
*Supportive care*
- While supportive care (IV fluids, pain control) is important, it does not address the underlying mechanical issue of **intussusception** and would not resolve the condition.
- Delaying definitive treatment for intussusception can lead to **bowel ischemia, necrosis, and perforation**, which are life-threatening.
*Broad-spectrum antibiotics*
- Antibiotics are not the primary treatment for **intussusception**, as it is a mechanical obstruction, not typically a primary infection.
- They might be considered if there are signs of **perforation or peritonitis**, but the immediate goal is reduction.
*Abdominal laparotomy*
- An **abdominal laparotomy** is a surgical intervention reserved for cases where **non-operative reduction** (like an air enema) fails or if there are signs of **bowel perforation or gangrene**.
- It is not the *first-line* next step after diagnosis, especially if non-invasive options remain viable.
*Abdominal CT scan*
- An **abdominal CT scan** can diagnose intussusception but is typically not the preferred initial imaging because it involves **radiation exposure** and **does not offer therapeutic benefit**, unlike an air contrast enema.
- Abdominal ultrasound is usually sufficient for diagnosis and safer for pediatric patients.
Intussusception reduction techniques US Medical PG Question 3: A 47-year-old woman presents to the emergency department with abdominal pain. The patient states that she felt this pain come on during dinner last night. Since then, she has felt bloated, constipated, and has been vomiting. Her current medications include metformin, insulin, levothyroxine, and ibuprofen. Her temperature is 99.0°F (37.2°C), blood pressure is 139/79 mmHg, pulse is 95/min, respirations are 12/min, and oxygen saturation is 98% on room air. On physical exam, the patient appears uncomfortable. Abdominal exam is notable for hypoactive bowel sounds, abdominal distension, and diffuse tenderness in all four quadrants. Cardiac and pulmonary exams are within normal limits. Which of the following is the best next step in management?
- A. Metoclopramide
- B. Nasogastric tube, NPO, and IV fluids (Correct Answer)
- C. Stool guaiac
- D. Emergency surgery
- E. IV antibiotics and steroids
Intussusception reduction techniques Explanation: ***Nasogastric tube, NPO, and IV fluids***
- The patient's symptoms (abdominal pain, bloating, constipation, vomiting, distension, and hypoactive bowel sounds) are highly suggestive of a **bowel obstruction**.
- **Nasogastric tube decompression** relieves pressure, **NPO status** prevents further bowel distension, and **intravenous fluids** address dehydration and electrolyte imbalances, stabilizing the patient for further evaluation.
*Metoclopramide*
- This is a **prokinetic agent** that increases gastrointestinal motility.
- Using it in the context of a suspected bowel obstruction could worsen the condition by increasing pressure against the obstruction and potentially leading to **perforation**.
*Stool guaiac*
- A stool guaiac test detects the presence of **occult blood in the stool**, which is useful for evaluating gastrointestinal bleeding.
- While it can be part of a complete workup, it is not the immediate priority for a patient presenting with symptoms of **acute bowel obstruction** requiring stabilization.
*Emergency surgery*
- While surgery may ultimately be required for a bowel obstruction, it is not the immediate first step unless there are clear signs of **perforation**, **ischemia**, or **strangulation**, which are not specified here.
- Initial management involves **stabilization** with NG decompression, NPO, and IV fluids.
*IV antibiotics and steroids*
- **IV antibiotics** are indicated for suspected infection (e.g., appendicitis, diverticulitis with perforation), but the primary presentation here is mechanical obstruction, not infection.
- **Steroids** are typically used for inflammatory conditions or adrenal insufficiency, neither of which is indicated given the patient's symptoms.
Intussusception reduction techniques US Medical PG Question 4: A 6-year-old boy is brought to the emergency department with acute intermittent umbilical abdominal pain that began that morning. The pain radiates to his right lower abdomen and occurs every 15–30 minutes. During these episodes of pain, the boy draws up his knees to the chest. The patient has had several episodes of nonbilious vomiting. He had a similar episode 3 months ago. His temperature is 37.7°C (99.86°F), pulse is 99/min, respirations are 18/min, and blood pressure is 100/60 mm Hg. Abdominal examination shows periumbilical tenderness with no masses palpated. Abdominal ultrasound shows concentric rings of bowel in transverse section. Laboratory studies show:
Leukocyte Count 8,000/mm3
Hemoglobin 10.6 g/dL
Hematocrit 32%
Platelet Count 180,000/mm3
Serum
Sodium 143 mEq/L
Potassium 3.7 mEq/L
Chloride 88 mEq/L
Bicarbonate 28 mEq/L
Urea Nitrogen 19 mg/dL
Creatinine 1.3 mg/dL
Which of the following is the most likely underlying cause of this patient's condition?
- A. Acute appendicitis
- B. Malrotation with volvulus
- C. Intestinal adhesions
- D. Intestinal polyps
- E. Meckel diverticulum (Correct Answer)
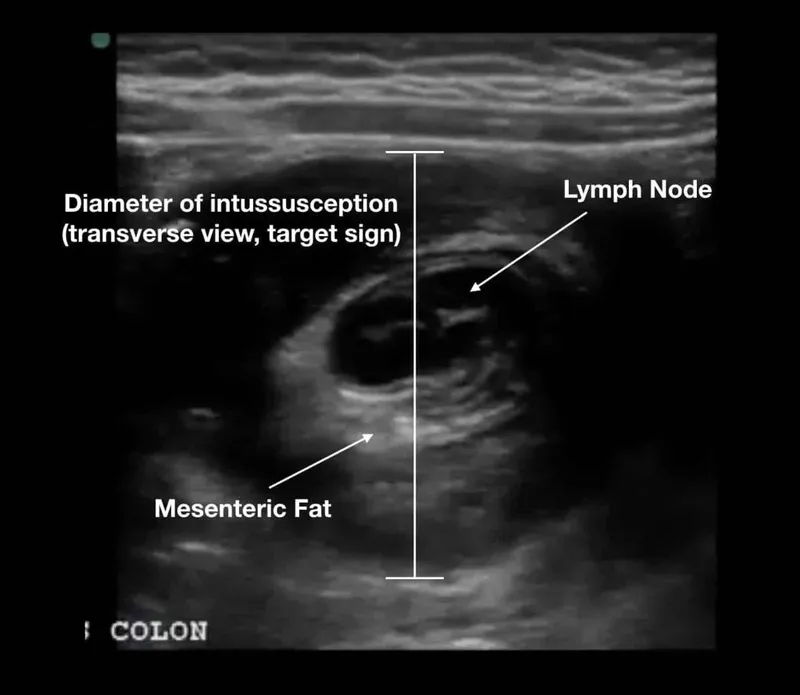
Intussusception reduction techniques Explanation: ***Meckel diverticulum***
- A **Meckel diverticulum** can serve as a **lead point for intussusception**, which is strongly suggested by the description of acute intermittent abdominal pain, drawing knees to the chest, and the ultrasound finding of concentric rings of bowel (**target sign**).
- The history of a similar episode 3 months ago points to a recurrent problem, and a Meckel diverticulum is the most common congenital anomaly of the small intestine that can cause such recurrent symptoms, often manifesting as a lead point for intussusception or bleeding.
*Incorrect Option: Acute appendicitis*
- While appendicitis causes abdominal pain, it is typically **persistent and localized to the right lower quadrant** (often migrating from periumbilical), not intermittent and widespread as described.
- The ultrasound finding of **concentric rings of bowel** is characteristic of intussusception, not appendicitis.
*Incorrect Option: Malrotation with volvulus*
- **Malrotation with volvulus** typically presents with **bilious vomiting** and severe, constant pain due to intestinal ischemia, which is not described in this patient.
- The intermittent nature of the pain and the specific ultrasound findings are more indicative of intussusception rather than volvulus.
*Incorrect Option: Intestinal adhesions*
- **Intestinal adhesions** can cause intermittent abdominal pain and bowel obstruction, but usually, a history of **previous abdominal surgery** is present, which is not mentioned here.
- Adhesions typically lead to a **mechanical obstruction pattern** on imaging, not the "target sign" characteristic of intussusception.
*Incorrect Option: Intestinal polyps*
- **Intestinal polyps**, especially in children, can act as **lead points for intussusception**, similar to a Meckel diverticulum.
- However, the description of **intermittent pain**, the age of the patient, and the lack of specific mention of bleeding make **Meckel diverticulum** a more common and direct underlying cause for recurrent intussusception in this age group without other associated symptoms like significant rectal bleeding often seen with polyps.
Intussusception reduction techniques US Medical PG Question 5: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Intussusception reduction techniques Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
Intussusception reduction techniques US Medical PG Question 6: An institutionalized 65-year-old man is brought to the emergency department because of abdominal pain and distension for 12 hours. The pain was acute in onset and is a cramping-type pain associated with nausea, vomiting, and constipation. He has a history of chronic constipation and has used laxatives for years. There is no history of inflammatory bowel disease in his family. He has not been hospitalized recently. There is no recent history of weight loss or change in bowel habits. On physical examination, the patient appears ill. The abdomen is distended with tenderness mainly in the left lower quadrant and is tympanic on percussion. The blood pressure is 110/79 mm Hg, heart rate is 100/min, the respiratory rate is 20/min, and the temperature is 37.2°C (99.0°F). The CBC shows an elevated white blood cell count. The plain abdominal X-ray is shown in the accompanying image. What is the most likely cause of his condition?
- A. Sigmoid volvulus (Correct Answer)
- B. Intussusception
- C. Acute diverticulitis
- D. Toxic megacolon
- E. Colon cancer
Intussusception reduction techniques Explanation: ***Sigmoid volvulus***
- The patient’s symptoms of acute **abdominal pain**, distension, and cramping strongly indicate **sigmoid volvulus**, often seen in chronic constipation and institutionalized patients.
- Physical examination revealing **tenderness in the left lower quadrant** and a tympanic abdomen supports the diagnosis of bowel obstruction typically caused by **volvulus**.
*Intussusception*
- Generally presents with **currant jelly stools** and is more common in children; the acute symptoms here are less typical.
- It often involves a **lead point** or associated conditions like **polyps** or tumors, which are not indicated in this case.
*Acute diverticulitis*
- Usually associated with **localized pain** in the left lower quadrant but would present with fever and changes in bowel habits, which the patient lacks.
- Typically shows **peritoneal signs** and may have complications like abscess or perforation, not indicated here.
*Toxic megacolon*
- Commonly associated with underlying **inflammatory bowel disease** or infections, not indicated in this patient with no recent history of **IBD**.
- Symptoms would include severe **diarrhea** and abdominal pain, which do not fit the current acute cramping and constipation pattern.
*Colon cancer*
- While it can cause abdominal symptoms, it presents more insidiously with **weight loss** or **change in bowel habits**, none of which are reported here.
- The acute presentation and findings do not align with a malignancy, which would often be chronic in nature.
Intussusception reduction techniques US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Intussusception reduction techniques Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Intussusception reduction techniques US Medical PG Question 8: A 50-year-old male presents to the emergency with abdominal pain. He reports he has had abdominal pain associated with meals for several months and has been taking over the counter antacids as needed, but experienced significant worsening pain one hour ago in the epigastric region. The patient reports the pain radiating to his shoulders. Vital signs are T 38, HR 120, BP 100/60, RR 18, SpO2 98%. Physical exam reveals diffuse abdominal rigidity with rebound tenderness. Auscultation reveals hypoactive bowel sounds. Which of the following is the next best step in management?
- A. Admission and observation
- B. Chest radiograph
- C. 12 lead electrocardiogram
- D. Abdominal CT scan (Correct Answer)
- E. Abdominal ultrasound
Intussusception reduction techniques Explanation: ***Abdominal CT scan***
- This patient presents with classic signs of a **perforated peptic ulcer**: sudden severe epigastric pain radiating to the shoulders (diaphragmatic irritation), fever, tachycardia, hypotension, and peritoneal signs (rigid abdomen with rebound tenderness).
- While the patient shows signs of **early shock** (BP 100/60, HR 120), he is **conscious and maintaining adequate oxygenation** (SpO2 98%), making him stable enough for rapid CT imaging.
- **Abdominal CT scan** is the **most sensitive and specific** test for detecting free air, identifying the location of perforation, and assessing for complications (abscess, contained perforation).
- CT provides **critical surgical planning information** about the extent and location of perforation, which can guide the surgical approach.
- This should be followed by **immediate surgical consultation** and preparation for emergency laparotomy.
*Chest radiograph*
- While an **upright chest X-ray** can detect free air under the diaphragm (pneumoperitoneum), it has **lower sensitivity** (70-80%) compared to CT scan (>95%).
- In a patient who is stable enough for imaging, **CT is preferred** as it provides more information for surgical planning.
- Chest X-ray would be the appropriate choice only if **CT is unavailable** or if the patient is **too unstable** to be transported to the CT scanner.
*Admission and observation*
- This patient has **acute peritonitis** from a likely perforated viscus, which is a **surgical emergency** requiring operative intervention.
- Observation would be inappropriate and dangerous, leading to **septic shock**, **multi-organ failure**, and death.
*12 lead electrocardiogram*
- While epigastric pain can sometimes be cardiac in origin, the **peritoneal signs** (rigid abdomen, rebound tenderness, hypoactive bowel sounds) clearly indicate an **intra-abdominal pathology**.
- The pain radiation to **both shoulders** (Kehr's sign) suggests diaphragmatic irritation from intraperitoneal air or fluid, not cardiac ischemia.
*Abdominal ultrasound*
- Ultrasound is useful for evaluating **solid organ injury**, **free fluid**, and conditions like **cholecystitis** or **appendicitis**.
- However, it is **poor at detecting free air** due to bowel gas artifact and has limited sensitivity for perforated viscus.
- It would not provide adequate information for this surgical emergency.
Intussusception reduction techniques US Medical PG Question 9: A 63-year-old female with known breast cancer presents with progressive motor weakness in bilateral lower extremities and difficulty ambulating. Physical exam shows 4 of 5 motor strength in her legs and hyper-reflexia in her patellar tendons. Neurologic examination 2 weeks prior was normal. Imaging studies, including an MRI, show significant spinal cord compression by the metastatic lesion and complete erosion of the T12 vertebrae. She has no metastatic disease to the visceral organs and her oncologist reports her life expectancy to be greater than one year. What is the most appropriate treatment?
- A. Palliative pain management consultation
- B. Surgical decompression and postoperative radiotherapy (Correct Answer)
- C. High-dose corticosteroids and clinical observation
- D. Radiation therapy alone
- E. Chemotherapy alone
Intussusception reduction techniques Explanation: ***Surgical decompression and postoperative radiotherapy***
- There is **spinal cord compression** by a metastatic lesion in a patient with a good prognosis (>1 year life expectancy) and rapidly progressive neurological deficits. **Surgical decompression** offers immediate relief of compression, while **postoperative radiotherapy** helps local tumor control.
- This combined approach is superior in preserving neurological function and improving quality of life for patients with **epidural spinal cord compression (ESCC)** in this clinical context.
*Palliative pain management consultation*
- While pain management is important in cancer care, this option alone does not address the **progressive neurological deficits** due to spinal cord compression.
- This patient's condition requires active treatment to prevent further neurological compromise and is not solely focused on comfort measures at this stage given her prognosis.
*Spinal dose corticosteroids and clinical observation*
- **Corticosteroids** can temporarily reduce edema around the spinal cord, but they do not resolve the mechanical compression caused by the eroded T12 vertebrae.
- **Clinical observation** without definitive intervention risks irreversible neurological damage given the rapid progression of symptoms.
*Radiation therapy alone*
- While radiation therapy is effective for local tumor control, it may not provide **rapid enough decompression** for acute or rapidly progressing neurological deficits due to significant mechanical compression.
- In cases of severe compression, such as bone erosion and cord involvement, surgery is usually needed prior to or in combination with radiation.
*Chemotherapy alone*
- **Chemotherapy** for breast cancer is a systemic treatment and may take time to reduce tumor burden, which is not suitable for urgent relief of **spinal cord compression**.
- It does not provide immediate mechanical decompression and is generally not the primary treatment for acute ESCC, especially with bone involvement.
Intussusception reduction techniques US Medical PG Question 10: A 67-year-old woman has fallen from the second story level of her home while hanging laundry. She was brought to the emergency department immediately and presented with severe abdominal pain. The patient is anxious, and her hands and feet feel very cold to the touch. There is no evidence of bone fractures, superficial skin wounds, or a foreign body penetration. Her blood pressure is 102/67 mm Hg, respirations are 19/min, pulse is 87/min, and temperature is 36.7°C (98.0°F). Her abdominal exam reveals rigidity and severe tenderness. A Foley catheter and nasogastric tube are inserted. The central venous pressure (CVP) is 5 cm H2O. The medical history is significant for hypertension. Which of the following is best indicated for the evaluation of this patient?
- A. X-Ray
- B. Ultrasound
- C. Peritoneal lavage
- D. CT scan (Correct Answer)
- E. Diagnostic laparotomy
Intussusception reduction techniques Explanation: ***CT scan***
- A **CT scan of the abdomen and pelvis** is the most indicated imaging modality for evaluating blunt abdominal trauma due to its high sensitivity and specificity in detecting solid organ injuries, free fluid, and active bleeding.
- Given the patient's severe abdominal pain, rigidity, and tenderness after a significant fall, a CT scan will provide detailed anatomical information crucial for guiding further management.
*X-Ray*
- An **X-ray** is useful for detecting bone fractures, but it has limited utility in assessing soft tissue and organ injuries within the abdomen.
- It would not effectively visualize internal bleeding or organ damage, which are primary concerns in this patient given the mechanism of injury and symptoms.
*Ultrasound*
- An **ultrasound (FAST exam)** is effective for rapid detection of free fluid in the abdomen (indicating bleeding or fluid leakage) and can be done at the bedside.
- However, it is operator-dependent and less sensitive than CT for identifying specific organ injuries, retroperitoneal hematomas, or the source of bleeding.
*Peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** is an invasive procedure primarily used to detect intra-abdominal bleeding in hemodynamically unstable patients, but it has largely been replaced by ultrasound and CT in stable patients.
- While it can detect blood, it is less specific for identifying the source of bleeding and does not provide anatomical detail, and carries risks of complications like bowel perforation.
*Diagnostic laparotomy*
- **Diagnostic laparotomy** is a surgical procedure to directly visualize abdominal contents and is indicated in cases of clear signs of peritonitis, hemodynamic instability with confirmed intra-abdominal bleeding, or evisceration.
- It is an invasive intervention and would not be the initial diagnostic step in a hemodynamically stable patient without clear indication for immediate surgery.
More Intussusception reduction techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.