Hirschsprung disease management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hirschsprung disease management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hirschsprung disease management US Medical PG Question 1: A 4-month-old girl is brought to the office by her parents because they noticed a mass protruding from her rectum and, she has been producing green colored emesis for the past 24 hours. Her parents noticed the mass when she had a bowel movement while changing her diaper. She strained to have this bowel movement 24 hours ago, shortly afterwards she had 3 episodes of greenish vomiting. She has a past medical history of failure to pass meconium for 2 days after birth. Her vital signs include: heart rate 190/min, respiratory rate 44/min, temperature 37.2°C (99.0°F), and blood pressure 80/50 mm Hg. On physical examination, the abdomen is distended. Examination of the anus reveals extrusion of the rectal mucosa through the external anal sphincter, and digital rectal examination produces an explosive expulsion of gas and stool. The abdominal radiograph shows bowel distention and absence of distal gas. What is the most likely cause?
- A. Enterobiasis
- B. Cystic fibrosis
- C. Hirschsprung disease (Correct Answer)
- D. Malnutrition
- E. Myelomeningocele
Hirschsprung disease management Explanation: ***Hirschsprung disease***
- The combination of **failure to pass meconium** at birth, **abdominal distention**, **green emesis**, and **rectal prolapse** with an **explosive expulsion of gas and stool** on digital rectal examination is highly suggestive of Hirschsprung disease.
- This condition is caused by the **absence of ganglion cells** in the distal colon, leading to a functional obstruction.
*Enterobiasis*
- **Enterobiasis**, or pinworm infection, commonly causes **perianal itching**, especially at night.
- It does not typically present with **rectal prolapse**, **abdominal distention**, or **vomiting** in infants.
*Cystic fibrosis*
- While cystic fibrosis can cause **meconium ileus** (failure to pass meconium), other symptoms like **malabsorption**, **respiratory issues**, and specific laboratory findings (e.g., sweat chloride test) would be expected.
- Rectal prolapse in cystic fibrosis is mainly due to chronic **straining from constipation** or **malabsorption**, not a primary motility disorder causing obstruction.
*Malnutrition*
- **Malnutrition** can lead to various symptoms, but it does not directly cause an acute presentation of **rectal prolapse**, **bowel obstruction**, and **explosive stool** on digital rectal examination.
- This patient's symptoms point to a specific congenital anatomical or functional issue.
*Myelomeningocele*
- A **myelomeningocele** is a severe form of spina bifida and involves a sac protruding from the back containing spinal cord and nerves, leading to neurological deficits.
- While it can cause **neurogenic bowel dysfunction** and chronic constipation, it does not typically present with acute **rectal prolapse** and other signs of immediate functional obstruction as observed here.
Hirschsprung disease management US Medical PG Question 2: A 4-week-old infant is brought to the emergency department by his parents with violent vomiting. It started about 3 days ago and has slowly gotten worse. He vomits after most feedings but seems to keep some formula down. His mother notes that he is eager to feed between episodes and seems to be putting on weight. Other than an uncomplicated course of chlamydia conjunctivitis, the infant has been healthy. He was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The physical exam is significant for a palpable mass in the right upper quadrant. What is the first-line confirmatory diagnostic test and associated finding?
- A. Abdominal ultrasound; elongated pyloric channel and muscle hypertrophy (Correct Answer)
- B. Barium upper GI series; GE junction and portion of the stomach in thorax
- C. Air enema; filling defect and coil spring sign
- D. Barium upper GI series; bird beak sign and corkscrewing
- E. Abdominal X-ray; ‘double bubble’ sign
Hirschsprung disease management Explanation: ***Abdominal ultrasound; elongated pyloric channel and muscle hypertrophy***
- The clinical picture of **projectile vomiting** in a 4-week-old infant, **eagerness to feed** ("hungry vomiter"), and **palpable olive-shaped mass** in the right upper quadrant is classic for **pyloric stenosis**.
- **Abdominal ultrasonography** is the gold standard for diagnosis, revealing an **elongated pyloric channel** (>16mm) and thickened pyloric muscle (>3-4mm).
- Pyloric stenosis typically presents between 3-6 weeks of age with progressive non-bilious vomiting.
*Barium upper GI series; GE junction and portion of the stomach in thorax*
- A **barium upper GI series** showing the **GE junction and stomach in the thorax** would indicate a **hiatal hernia**, which is not consistent with the palpable mass or "hungry vomiter" presentation.
- While hiatal hernias can cause vomiting and reflux, they typically don't present with this specific type of projectile vomiting or a palpable abdominal mass.
*Air enema; filling defect and coil spring sign*
- An **air enema** showing a **filling defect** and **coil spring sign** is characteristic of **intussusception**, which usually presents with sudden onset of **crampy abdominal pain**, **currant jelly stools**, and a palpable mass in the right lower quadrant.
- The clinical presentation does not fit intussusception, which typically occurs in older infants (6-36 months) and has a more acute presentation.
*Barium upper GI series; bird beak sign and corkscrewing*
- A **barium upper GI series** showing a **bird beak sign** and **corkscrewing** is pathognomonic for **midgut volvulus**, a surgical emergency.
- While volvulus can cause bilious vomiting and abdominal distension, the presentation of non-bilious vomiting with a palpable pyloric mass is more typical of pyloric stenosis.
*Abdominal X-ray; 'double bubble' sign*
- An **abdominal X-ray** revealing a **'double bubble' sign** is indicative of **duodenal atresia** or **annular pancreas**, leading to complete duodenal obstruction.
- This condition typically presents with **bilious vomiting** shortly after birth (within first day of life) and does not involve a palpable hypertrophied pylorus.
Hirschsprung disease management US Medical PG Question 3: A 4-year-old boy is brought to the physician by his parents for bedwetting. He went 3 months without wetting the bed but then started again 6 weeks ago. He has been wetting the bed about 1–2 times per week. He has not had daytime urinary incontinence or dysuria. His teachers report that he is attentive in preschool and plays well with his peers. He is able to name 5 colors, follow three-step commands, and recite his address. He can do a somersault, use scissors, and copy a square. Physical examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. IQ testing
- B. Enuresis alarm
- C. Bladder ultrasound
- D. Oxybutynin therapy
- E. Reassurance (Correct Answer)
Hirschsprung disease management Explanation: ***Reassurance***
- This 4-year-old boy presents with secondary enuresis, which is common and often **resolves spontaneously with time**. Given his age and lack of other concerning symptoms (daytime incontinence, dysuria, developmental delays), initial management should focus on **reassurance** and education for the parents.
- At this age, the **prevalence of enuresis is still high (around 20%)**, and many children have not yet achieved consistent nighttime bladder control. There is **no evidence of organic pathology** or significant psychological distress based on the provided information.
*Enuresis alarm*
- While effective for enuresis, enuresis alarms are generally considered for children **over 5-7 years old** or older with persistent enuresis, after initial conservative measures and observation.
- For a 4-year-old, the primary approach is often to **wait and monitor**, as developmental maturation plays a significant role.
*IQ testing*
- The boy's developmental milestones (naming colors, following commands, gross and fine motor skills) are **appropriate for his age**, and his teachers report no concerns.
- There is **no indication of global developmental delay** or cognitive impairment that would necessitate IQ testing.
*Bladder ultrasound*
- This child exhibits no signs or symptoms suggesting an underlying urological abnormality, such as **daytime incontinence, frequent urinary tract infections, dysuria, or abnormal voiding patterns**.
- A bladder ultrasound would be considered in cases with **red flag symptoms** or if initial conservative management of enuresis fails in older children to rule out structural issues.
*Oxybutynin therapy*
- Oxybutynin is an **anticholinergic medication** used to treat overactive bladder symptoms or severe enuresis, typically in older children when other treatments have failed.
- It is **not a first-line therapy** for a 4-year-old with secondary enuresis without other symptoms, as the condition is likely developmental.
Hirschsprung disease management US Medical PG Question 4: A mother brings her 4-year-old boy to the physician, as the boy has a 7-day history of foul-smelling diarrhea, abdominal cramps, and fever. The mother adds that he has been vomiting as well, and she is very much worried. The child is in daycare, and the mother endorses sick contacts with both family and friends. The boy has not been vaccinated as the parents do not think it is necessary. On physical exam, the child appears dehydrated. Stool examination is negative for blood cells, pus, and ova or parasites. What is the most likely diagnosis?
- A. Rotavirus infection (Correct Answer)
- B. Cryptosporidiosis
- C. Irritable bowel syndrome
- D. C. difficile colitis
- E. Norovirus infection
Hirschsprung disease management Explanation: ***Rotavirus infection***
- The classic presentation of **foul-smelling diarrhea**, vomiting, abdominal cramps, and fever in an **unvaccinated child** attending daycare strongly suggests rotavirus. This virus is a common cause of **severe gastroenteritis** in young children.
- The absence of bacterial or parasitic indicators in the stool (blood cells, pus, ova/parasites) further narrows the diagnosis to a **viral cause**, with rotavirus being highly prevalent in this age group, especially without vaccination.
*Cryptosporidiosis*
- While it causes **watery diarrhea** and abdominal cramps, it is typically associated with **contaminated water sources** and often produces **oocysts** detectable in stool, which were not found in this case.
- The symptoms in the child are more classic for a common viral gastroenteritis rather than a parasitic infection, especially given the **absence of parasitic elements** on examination.
*Irritable bowel syndrome*
- **IBS** is a chronic functional gastrointestinal disorder and rarely presents acutely with fever and vomiting in a 4-year-old.
- Its diagnosis involves specific **Rome IV criteria** related to chronic abdominal pain and changes in bowel habits, which are not met by the acute presentation here.
*C. difficile colitis*
- **C. difficile colitis** typically follows **antibiotic use** or is acquired in healthcare settings and commonly causes **bloody diarrhea** and significant abdominal pain.
- The diarrhea is usually more profuse and the stool may contain **leukocytes** or be positive for C. difficile toxin, neither of which is indicated in the patient's presentation.
*Norovirus infection*
- Norovirus causes acute gastroenteritis with **vomiting** and **diarrhea**, but the diarrhea is often less foul-smelling and of shorter duration than described.
- While possible, the classic triad of **foul-smelling diarrhea, vomiting, and fever** in an unvaccinated child with sick contacts more strongly points to rotavirus, which tends to cause more severe and prolonged symptoms in young, unvaccinated children.
Hirschsprung disease management US Medical PG Question 5: A 2-year-old boy is brought in to his pediatrician for a routine checkup. The parents mention that the child has been developing appropriately, although they have been noticing that the child appears to have chronic constipation. The parents report that their child does not routinely have daily bowel movements, and they have noticed that his abdomen has become more distended recently. In the past, they report that the patient was also delayed in passing meconium, but this was not further worked up. On exam, his temperature is 98.6°F (37.0°C), blood pressure is 110/68 mmHg, pulse is 74/min, and respirations are 14/min. The patient is noted to have a slightly distended abdomen that is nontender. Eventually, this patient undergoes a biopsy. Which of the following layers most likely reveals the causative pathologic finding of this disease?
- A. Submucosa
- B. Mucosa
- C. Lamina propria
- D. Muscularis mucosa
- E. Muscularis propria (between muscle layers) (Correct Answer)
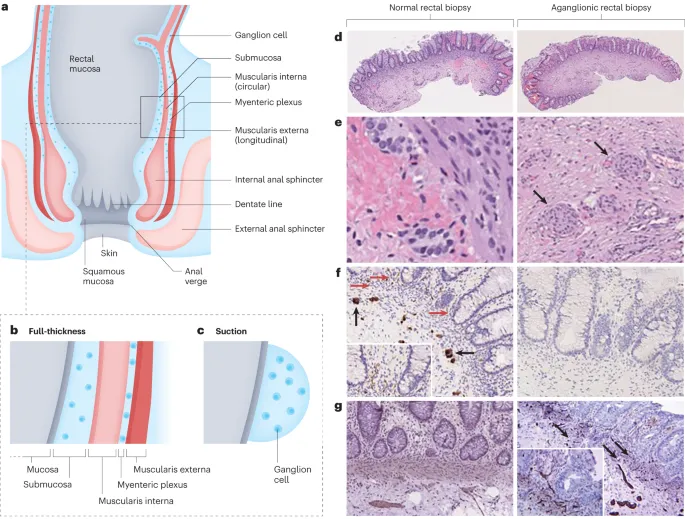
Hirschsprung disease management Explanation: ***Muscularis propria (between muscle layers)***
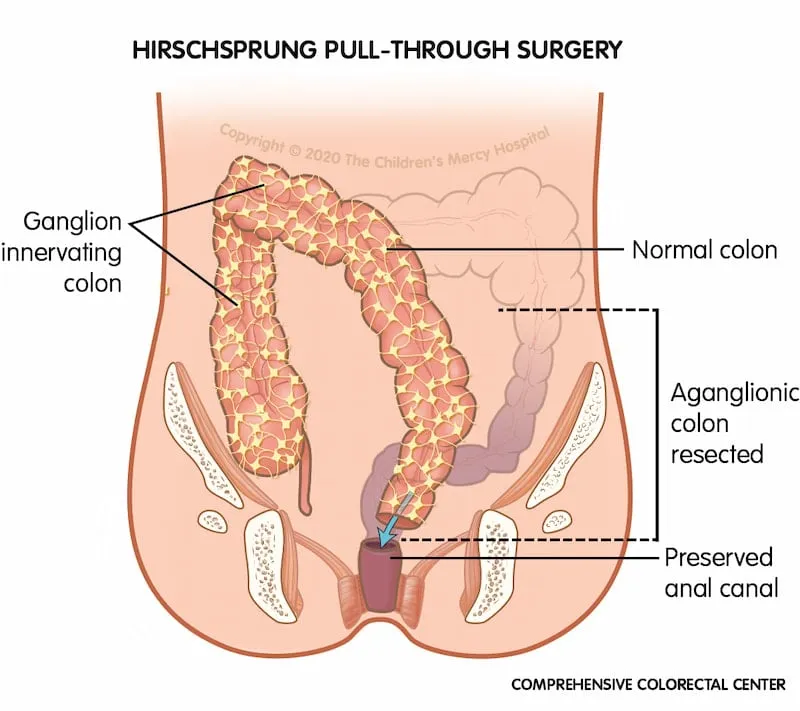
- This patient's presentation with **chronic constipation**, **abdominal distention**, and **delayed meconium passage** is highly suggestive of **Hirschsprung disease**.
- The causative pathology in Hirschsprung disease is the **absence of ganglion cells** in the **myenteric (Auerbach's) and submucosal (Meissner's) plexuses**, which is definitively diagnosed by a rectal biopsy showing this lack of innervation.
- The **myenteric plexus** is located **between the inner circular and outer longitudinal layers** of the **muscularis propria**, making this the primary layer examined for diagnostic findings.
*Submucosa*
- While the **submucosal (Meissner's) plexus** is also affected in Hirschsprung disease and the submucosa can show absent ganglion cells, the **myenteric plexus** in the muscularis propria is the primary diagnostic target in rectal biopsies.
- Both plexuses are affected, but the muscularis propria is considered the most definitive layer for diagnosis.
*Mucosa*
- The **mucosa** is the innermost layer of the gastrointestinal tract, consisting of epithelium, lamina propria, and muscularis mucosa.
- This layer does **not** contain the enteric nervous system plexuses (myenteric or submucosal) responsible for gut motility, so biopsy of this layer alone would not reveal the absent ganglion cells characteristic of Hirschsprung disease.
*Lamina propria*
- The **lamina propria** is a thin layer of connective tissue found within the **mucosa**, beneath the epithelium.
- This layer primarily contains blood vessels, lymphatics, and immune cells, and it is **not** where the ganglion cells of the enteric nervous system are located or where the primary pathology of Hirschsprung disease is found.
*Muscularis mucosa*
- The **muscularis mucosa** is a thin layer of smooth muscle that forms the outermost layer of the **mucosa**.
- It does not contain the enteric plexuses (myenteric or submucosal) responsible for gut motility, so its biopsy would not reveal the absent ganglion cells characteristic of Hirschsprung disease.
Hirschsprung disease management US Medical PG Question 6: A 3175-g (7-lb) female newborn is delivered at term. Initial examination shows a distended abdomen and a flat perineal region without an opening. A dark green discharge is coming out of the vulva. Which of the following is the most likely diagnosis?
- A. Hirschsprung disease
- B. Meconium plug syndrome
- C. Imperforate anus (Correct Answer)
- D. Meconium ileus
- E. Colonic atresia
Hirschsprung disease management Explanation: ***Imperforate anus***
- The combination of a **distended abdomen**, **flat perineal region without an opening**, and **dark green discharge from the vulva** (indicating meconium passage through a rectovaginal fistula) is pathognomonic for imperforate anus.
- This congenital anomaly results from abnormal development of the **hindgut** and **urogenital sinus**, leading to a spectrum of anorectal malformations.
*Hirschsprung disease*
- Characterized by the absence of **ganglion cells** in the distal colon, leading to functional obstruction.
- While it can cause **abdominal distension** and delayed meconium passage, it typically presents with a **normal-appearing anus** and no meconium from the vulva.
*Meconium plug syndrome*
- This is a transient obstruction of the colon by a **mucous plug**, without an anatomical defect of the anus.
- The anus would be **patent**, and though abdominal distension might occur, meconium would not be seen exiting the vulva.
*Meconium ileus*
- This condition involves obstruction of the **small bowel** by thick, inspissated meconium, primarily associated with **cystic fibrosis**.
- It would cause abdominal distension and delayed meconium passage, but the anus would be **patent**, and meconium would not be expelled through the vulva.
*Colonic atresia*
- This is a congenital complete obstruction of the colon, causing abdominal distension and vomiting.
- However, the **perineum would appear normal**, and there would be no meconium discharge from the vulva.
Hirschsprung disease management US Medical PG Question 7: A 56-year-old woman is one week status post abdominal hysterectomy when she develops a fever of 101.4°F (38.6°C). Her past medical history is significant for type II diabetes mellitus and a prior history of alcohol abuse. The operative report and intraoperative cystoscopy indicate that the surgery was uncomplicated. The nurse reports that since the surgery, the patient has also complained of worsening lower abdominal pain. She has given the patient the appropriate pain medications with little improvement. The patient has tolerated an oral diet well and denies nausea, vomiting, or abdominal distension. Her blood pressure is 110/62 mmHg, pulse is 122/min, and respirations are 14/min. Since being given 1000 mL of intravenous fluids yesterday, the patient has excreted 800 mL of urine. On physical exam, she is uncomfortable, shivering, and sweating. The surgical site is intact, but the surrounding skin appears red. No drainage is appreciated. The abdominal examination reveals tenderness to palpation and hypoactive bowel sounds. Labs and a clean catch urine specimen are obtained as shown below:
Leukocyte count and differential:
Leukocyte count: 18,000/mm^3
Segmented neutrophils: 80%
Bands: 10%
Eosinophils: 1%
Basophils: < 1%
Lymphocytes: 5%
Monocytes: 4%
Platelet count: 300,000/mm^3
Hemoglobin: 12.5 g/dL
Hematocrit: 42%
Urine:
Epithelial cells: 15/hpf
Glucose: positive
RBC: 1/hpf
WBC: 2/hpf
Bacteria: 50 cfu/mL
Ketones: none
Nitrites: negative
Leukocyte esterase: negative
Which of the following is most likely the cause of this patient’s symptoms?
- A. Surgical error
- B. Post-operative ileus
- C. Wound infection (Correct Answer)
- D. Alcohol withdrawal
- E. Urinary tract infection
Hirschsprung disease management Explanation: ***Wound infection***
- The patient presents with **fever**, worsening **lower abdominal pain**, **tachycardia**, and **local signs of inflammation** (redness around the surgical site, tenderness) one week post-hysterectomy, with a **leukocytosis and left shift** (elevated neutrophils and bands). These findings are highly characteristic of a common **post-surgical wound infection**.
- The lack of significant drainage initially does not rule out infection, and the symptoms are localized to the surgical area.
*Surgical error*
- The operative report and intraoperative cystoscopy indicated the surgery was **uncomplicated**, making an immediate post-operative surgical error less likely to be the primary cause of these symptoms.
- While complications can arise later, the current presentation points more directly to an infectious process rather than an unnoted immediate surgical complication.
*Post-operative ileus*
- Although bowel sounds are hypoactive, the patient is **tolerating an oral diet well** and denies nausea, vomiting, or abdominal distension, which are key symptoms of a clinically significant ileus.
- Her primary complaint is localized pain and systemic signs of infection, rather than generalized abdominal distension and inability to pass flatus or stool.
*Alcohol withdrawal*
- While the patient has a history of alcohol abuse, the primary symptoms (fever, localized abdominal pain, redness around the incision, leukocytosis) are more indicative of an **infectious process** than alcohol withdrawal.
- Alcohol withdrawal typically presents with tremors, agitation, hallucinations, and autonomic instability, and while some overlap (tachycardia) exists, the overall clinical picture doesn't fit.
*Urinary tract infection*
- The urine analysis shows **negative nitrites and leukocyte esterase**, with only 2 WBC/hpf, which makes a **urinary tract infection (UTI) highly unlikely** despite the presence of some bacteria (50 cfu/mL, which is often considered contamination in a clean catch).
- The patient's symptoms are also predominantly localized to the surgical wound area rather than dysuria, frequency, or urgency.
Hirschsprung disease management US Medical PG Question 8: A 2-day-old newborn boy has failed to pass meconium after 48 hours. There is an absence of stool in the rectal vault. Family history is significant for MEN2A syndrome. Which of the following confirms the diagnosis?
- A. Barium enema demonstrating absence of a transition zone
- B. Atrophic nerve fibers and increased acetylcholinesterase activity
- C. Rectal manometry demonstrating relaxation of the internal anal sphincter with distension of the rectum
- D. Genetic testing confirming mutation in the RET oncogene
- E. Absence of ganglion cells demonstrated by rectal suction biopsy (Correct Answer)
Hirschsprung disease management Explanation: ***Absence of ganglion cells demonstrated by rectal suction biopsy***
- The **absence of ganglion cells** in the colorectum, particularly on a **rectal suction biopsy**, is the definitive diagnostic feature of **Hirschsprung disease**.
- This congenital condition is characterized by the **failure of neural crest cells to migrate** to the distal bowel, leading to an aganglionic segment that cannot relax, resulting in functional obstruction.
*Barium enema demonstrating absence of a transition zone*
- A **barium enema** is a useful initial imaging study for suspected **Hirschsprung disease**, often showing a **transition zone** between a constricted aganglionic segment and a dilated, normally innervated proximal bowel.
- The *absence* of a transition zone would make **Hirschsprung disease** *less likely* or could indicate **total colonic aganglionosis**, but it is not a direct confirmatory diagnostic finding and still requires biopsy.
*Atrophic nerve fibers and increased acetylcholinesterase activity*
- While increased **acetylcholinesterase activity** in hypertrophied nerve fibers is a characteristic finding in the muscularis mucosa and submucosa of aganglionic segments in **Hirschsprung disease**, the description of "*atrophic* nerve fibers" is incorrect.
- The abnormal nerve fibers are typically hypertrophic, and this finding from specialized staining on a biopsy supports the diagnosis but is not the primary confirmatory feature itself; the **absence of ganglion cells** is paramount.
*Rectal manometry demonstrating relaxation of the internal anal sphincter with distension of the rectum*
- **Rectal manometry** is used to assess the neuromuscular function of the rectum and anal sphincter. In **Hirschsprung disease**, there is a characteristic **failure of the internal anal sphincter to relax** when the rectum is distended.
- Demonstrating normal *relaxation* of the internal anal sphincter would effectively *rule out* **Hirschsprung disease**, as the **failure of relaxation** is a key physiological abnormality.
*Genetic testing confirming mutation in the RET oncogene*
- Mutations in the **RET oncogene** are associated with **Hirschsprung disease**, especially in familial cases and those associated with syndromic forms like **MEN2A**.
- While a positive genetic test can support the diagnosis and guide genetic counseling, it is **not sufficient for a definitive diagnosis** on its own, as penetrance is variable and the definitive diagnosis relies on histological confirmation of aganglionosis.
Hirschsprung disease management US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Hirschsprung disease management Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
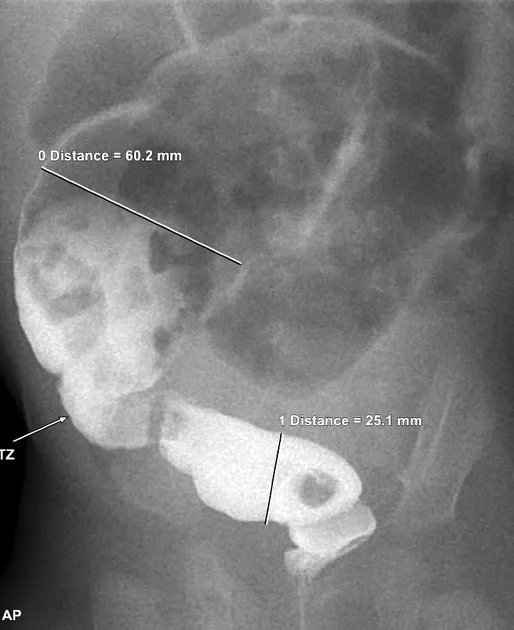
Hirschsprung disease management US Medical PG Question 10: An institutionalized 65-year-old man is brought to the emergency department because of abdominal pain and distension for 12 hours. The pain was acute in onset and is a cramping-type pain associated with nausea, vomiting, and constipation. He has a history of chronic constipation and has used laxatives for years. There is no history of inflammatory bowel disease in his family. He has not been hospitalized recently. There is no recent history of weight loss or change in bowel habits. On physical examination, the patient appears ill. The abdomen is distended with tenderness mainly in the left lower quadrant and is tympanic on percussion. The blood pressure is 110/79 mm Hg, heart rate is 100/min, the respiratory rate is 20/min, and the temperature is 37.2°C (99.0°F). The CBC shows an elevated white blood cell count. The plain abdominal X-ray is shown in the accompanying image. What is the most likely cause of his condition?
- A. Sigmoid volvulus (Correct Answer)
- B. Intussusception
- C. Acute diverticulitis
- D. Toxic megacolon
- E. Colon cancer
Hirschsprung disease management Explanation: ***Sigmoid volvulus***
- The patient’s symptoms of acute **abdominal pain**, distension, and cramping strongly indicate **sigmoid volvulus**, often seen in chronic constipation and institutionalized patients.
- Physical examination revealing **tenderness in the left lower quadrant** and a tympanic abdomen supports the diagnosis of bowel obstruction typically caused by **volvulus**.
*Intussusception*
- Generally presents with **currant jelly stools** and is more common in children; the acute symptoms here are less typical.
- It often involves a **lead point** or associated conditions like **polyps** or tumors, which are not indicated in this case.
*Acute diverticulitis*
- Usually associated with **localized pain** in the left lower quadrant but would present with fever and changes in bowel habits, which the patient lacks.
- Typically shows **peritoneal signs** and may have complications like abscess or perforation, not indicated here.
*Toxic megacolon*
- Commonly associated with underlying **inflammatory bowel disease** or infections, not indicated in this patient with no recent history of **IBD**.
- Symptoms would include severe **diarrhea** and abdominal pain, which do not fit the current acute cramping and constipation pattern.
*Colon cancer*
- While it can cause abdominal symptoms, it presents more insidiously with **weight loss** or **change in bowel habits**, none of which are reported here.
- The acute presentation and findings do not align with a malignancy, which would often be chronic in nature.
More Hirschsprung disease management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.