Congenital heart defects requiring surgery US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Congenital heart defects requiring surgery. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Congenital heart defects requiring surgery US Medical PG Question 1: A 5-week-old infant born at 36 weeks' gestation is brought to the physician for a well-child examination. Her mother reports that she previously breastfed her for 15 minutes every 2 hours but now feeds her for 40 minutes every 4 hours. The infant has six wet diapers and two stools daily. She currently weighs 3500 g (7.7 lb) and is 52 cm (20.4 in) in length. Vital signs are with normal limits. Cardiopulmonary examination shows a grade 4/6 continuous murmur heard best at the left infraclavicular area. After confirming the diagnosis via echocardiography, which of the following is the most appropriate next step in management of this patient?
- A. Surgical ligation
- B. Indomethacin infusion
- C. Reassurance and follow-up (Correct Answer)
- D. Percutaneous device closure
- E. Prostaglandin E1 infusion
Congenital heart defects requiring surgery Explanation: ***Reassurance and follow-up***
- This 5-week-old infant (41 weeks postmenstrual age) with a PDA is **hemodynamically stable** with normal vital signs, appropriate weight gain (3500g), adequate urine output (6 wet diapers/day), and effective feeding despite longer feeding times.
- The change in feeding pattern (40 minutes every 4 hours vs 15 minutes every 2 hours) actually represents **improved feeding efficiency** with the same total daily feeding time but longer intervals between feeds.
- Despite the loud murmur (grade 4/6), there are **no signs of congestive heart failure** (no tachypnea, no hepatomegaly, no failure to thrive).
- In a **clinically stable infant** without heart failure symptoms, **watchful waiting with close follow-up** is appropriate as many PDAs close spontaneously, particularly in infants born at 36 weeks gestation.
- Intervention would be indicated if the infant develops signs of heart failure or failure to thrive.
*Indomethacin infusion*
- **Indomethacin** (a prostaglandin synthesis inhibitor) is only effective for PDA closure in the **early neonatal period** (typically first 7-10 days of life) when the ductus is still responsive to prostaglandins.
- At **5 weeks of age** (41 weeks postmenstrual age), the ductus arteriosus has undergone structural maturation and is **no longer responsive** to prostaglandin inhibitors.
- This infant is well past the window for pharmacologic closure with indomethacin.
*Surgical ligation*
- **Surgical ligation** would be indicated for a hemodynamically significant PDA causing heart failure symptoms that are refractory to medical management.
- This infant is **hemodynamically stable** without signs of heart failure, so surgical intervention is not warranted at this time.
- Surgery carries significant risks and should be reserved for cases where conservative management has failed.
*Prostaglandin E1 infusion*
- **Prostaglandin E1** is used to **maintain ductal patency** in ductal-dependent congenital heart lesions (e.g., critical coarctation, transposition of great arteries, pulmonary atresia).
- This would be contraindicated in PDA as it would **worsen** the condition by keeping the ductus open.
- The clinical picture suggests isolated PDA, not a ductal-dependent lesion.
*Percutaneous device closure*
- **Percutaneous device closure** is typically performed in **older infants and children** (usually >6 months old and >6 kg) with persistent hemodynamically significant PDA.
- This 5-week-old infant weighing 3500g is **too small** for device closure.
- Additionally, the infant is currently stable and may not require intervention if the PDA closes spontaneously.
Congenital heart defects requiring surgery US Medical PG Question 2: A 2-week-old newborn is brought to the physician for a follow-up examination. He was born at term and the pregnancy was uncomplicated. His mother says he has been feeding well and passing adequate amounts of urine. He appears healthy. He is at the 60th percentile for length and 40th percentile for weight. His temperature is 37.3°C (99.1°F), pulse is 130/min, respirations are 49/min and blood pressure is 62/40 mm Hg. A thrill is present over the third left intercostal space. A 5/6 holosystolic murmur is heard over the left lower sternal border. An echocardiography shows a 3-mm membranous ventricular septal defect. Which of the following is the most appropriate next step in management?
- A. Indomethacin therapy
- B. Cardiac catheterization
- C. Amoxicillin therapy
- D. Prostaglandin E1 therapy
- E. Outpatient follow-up (Correct Answer)
Congenital heart defects requiring surgery Explanation: ***Outpatient follow-up***
- The patient has a **small ventricular septal defect (VSD)** (3 mm) and is **asymptomatic**, feeding well, and growing appropriately. Many small VSDs close spontaneously, so watchful waiting with outpatient follow-up is the most appropriate initial management.
- The presence of a thrill and a loud holosystolic murmur with a small VSD is often due to the **high-velocity jet** of blood across a small opening, rather than indicative of severe hemodynamic instability.
*Indomethacin therapy*
- **Indomethacin** is used to close a **patent ductus arteriosus (PDA)**, not a VSD.
- VSDs do not respond to indomethacin.
*Cardiac catheterization*
- **Cardiac catheterization** or surgical repair is typically reserved for **large, symptomatic VSDs** that cause heart failure, pulmonary hypertension, or significant growth failure, none of which are present in this case.
- Performing an invasive procedure on an asymptomatic infant with a small VSD is unnecessary and carries risks.
*Amoxicillin therapy*
- **Amoxicillin** is an antibiotic and is not indicated for the management of a VSD.
- While it can be used for endocarditis prophylaxis in some high-risk cardiac conditions, a small VSD is typically not considered a high-risk lesion requiring routine prophylaxis.
*Prostaglandin E1 therapy*
- **Prostaglandin E1 (PGE1)** is used to maintain the **patency of the ductus arteriosus** in ductal-dependent cardiac lesions (e.g., critical coarctation, hypoplastic left heart syndrome) to ensure systemic or pulmonary blood flow.
- In this case, the VSD does not require the PDA to remain open; in fact, maintaining PDA patency would worsen a VSD by increasing pulmonary blood flow.
Congenital heart defects requiring surgery US Medical PG Question 3: A 9-year-old boy is brought to the office due to exertional dyspnea and fatigability. He tires easily when walking or playing. His parents say that he was diagnosed with a congenital heart disease during his infancy, but they refused any treatment. They do not remember much about his diagnosis. The patient also had occasional respiratory infections throughout childhood that did not require hospitalization. He takes no medications. The patient has no family history of heart disease. His vital signs iclude: heart rate 98/min, respiratory rate 16/min, temperature 37.2°C (98.9°F), and blood pressure of 110/80 mm Hg. Physical examination shows toe cyanosis and clubbing but no finger abnormalities. Cardiac auscultation reveals a continuous machine-like murmur. All extremity pulses are full and equal. Which of the following is the most likely diagnosis?
- A. Tetralogy of Fallot
- B. Coarctation of the aorta
- C. Ventricular septal defect
- D. Atrial septal defect
- E. Patent ductus arteriosus (Correct Answer)
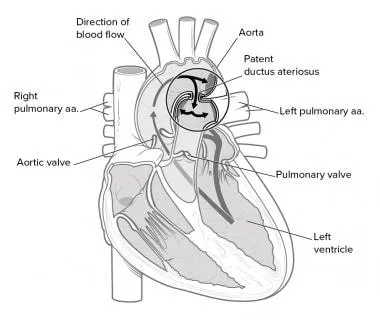
Congenital heart defects requiring surgery Explanation: ***Patent ductus arteriosus***
- A **patent ductus arteriosus (PDA)** can cause differential cyanosis and clubbing (lower extremities more affected than upper) due to preferential flow of deoxygenated blood through the PDA to the descending aorta.
- The classic **continuous machine-like murmur** auscultated in the precordium is highly characteristic of a PDA.
*Tetralogy of Fallot*
- Patients typically present with **cyanosis and clubbing of all four extremities** due to right-to-left shunting at the ventricular level, not isolated toe cyanosis.
- While it can cause exertional dyspnea, the murmur is typically a **systolic ejection murmur** from pulmonary stenosis, not a continuous machine-like murmur.
*Coarctation of the aorta*
- This condition presents with **differential blood pressures and pulses** between the upper and lower extremities, with elevated upper extremity pressures.
- It does not typically cause cyanosis or a continuous machine-like murmur.
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** typically causes a **holosystolic murmur** loudest at the lower left sternal border.
- Cyanosis develops late due to Eisenmenger syndrome, and if it occurs, it's typically central, affecting all extremities.
*Atrial septal defect*
- An **atrial septal defect (ASD)** usually presents with a **fixed split S2** and a **systolic ejection murmur** at the upper left sternal border due to increased flow across the pulmonic valve.
- Significant cyanosis is rare and occurs only in advanced stages with Eisenmenger syndrome, affecting all extremities if present.
Congenital heart defects requiring surgery US Medical PG Question 4: Cardiac surgery is consulted on a newborn with a large ventricular septal defect. The child has poor weight gain and feeding difficulties. He requires furosemide and captopril to avoid dyspnea. On physical examination his temperature is 36.9°C (98.4°F), pulse rate is 158/min, respiratory rate is 30/min, and blood pressure is 94/62 mm Hg. Chest auscultation reveals a holosystolic murmur along the left lower sternal border and a mid-diastolic low-pitched rumble at the apex. Abdominal examination reveals the presence of hepatomegaly. An echocardiogram confirms a diagnosis of a membranous VSD while hemodynamic studies show a Qp:Qs ratio of 2.8:1. Which of the following is the best management option?
- A. Continue medical treatment and provide reassurance about spontaneous closure of the defect
- B. Hybrid surgery using both transcatheter device and surgical repair
- C. Transcatheter occlusion of the defect
- D. Surgical closure of the defect (Correct Answer)
- E. Addition of digoxin to the current medical regimen with regular follow-up until spontaneous closure occurs
Congenital heart defects requiring surgery Explanation: ***Surgical closure of the defect***
* This newborn exhibits **symptoms of severe heart failure** due to a large VSD, including poor weight gain, feeding difficulties, and hepatomegaly, despite maximal medical therapy.
* A **Qp:Qs ratio of 2.8:1** indicates a significant left-to-right shunt, which, combined with the clinical picture, necessitates **surgical intervention** to prevent irreversible pulmonary vascular disease and improve prognosis.
*Continue medical treatment and provide reassurance about spontaneous closure of the defect*
* While some small VSDs close spontaneously, this child has a **large VSD** with **symptoms of severe heart failure** that require aggressive medical management (furosemide, captopril) and show no signs of improvement.
* **Reassurance of spontaneous closure** is inappropriate given the significant hemodynamic compromise and the potential for long-term complications without surgical intervention.
*Hybrid surgery using both transcatheter device and surgical repair*
* Hybrid approaches are typically reserved for **complex congenital heart defects** or specific anatomical challenges where a purely transcatheter or open surgical approach is not feasible or optimal.
* For a large membranous VSD requiring definitive closure, a **direct surgical approach** is generally preferred and more effective.
*Transcatheter occlusion of the defect*
* **Transcatheter occlusion** is generally indicated for **smaller, hemodynamically insignificant VSDs** or in specific anatomical situations, and it is usually performed in older children.
* A **large membranous VSD** with significant shunt and symptoms of heart failure is typically **not amenable to transcatheter closure** due to the size and location of the defect, and the risk of complications.
*Addition of digoxin to the current medical regimen with regular follow-up until spontaneous closure occurs*
* The child is already on **maximal medical therapy** (furosemide, captopril) and still experiencing severe symptoms, indicating medicine alone is insufficient.
* While digoxin can improve myocardial contractility, it is unlikely to significantly alter the natural history or **resolve the large shunt** in a VSD of this magnitude, and waiting for spontaneous closure would be detrimental.
Congenital heart defects requiring surgery US Medical PG Question 5: Over the course of a year, 5 children with identical congenital heart defects were referred to a pediatric cardiac surgeon for evaluation. All 5 children had stable vital signs and were on appropriate medication. Upon review of medical records, all of them had a loud holosystolic murmur over the third intercostal space at the left sternal border. The surgeon ordered echocardiograms for all 5 children and recommended surgical closure of the defect in one of them. Which of the following patients required surgical repair of their defect?
- A. A 7-year-old boy with an 11-mm muscular defect and severe pulmonary vascular disease non-responsive to pulmonary vasodilators
- B. An 11-month-old female infant with a 6-mm membranous defect, without heart failure, pulmonary hypertension, or growth failure
- C. A 4-month-old male infant with a 12-mm muscular defect, without heart failure, pulmonary hypertension or growth failure
- D. A 5-year-old girl with a 2-mm membranous defect, no heart failure, a Qp:Qs ratio less than 2:1, and no growth failure
- E. A 2-year-old boy with a 2-mm supracristal defect, without heart failure, pulmonary hypertension, or growth failure (Correct Answer)
Congenital heart defects requiring surgery Explanation: ***A 2-year-old boy with a 2-mm supracristal defect, without heart failure, pulmonary hypertension, or growth failure***
- This patient description most closely matches the criteria for requiring surgical repair. **Supracristal VSDs** are more prone to **aortic valve prolapse** and **aortic regurgitation**, even with small defects and absent or mild symptoms, thus warranting early surgical consideration.
- While other symptomatic VSDs might require surgery, this specific type of VSD carries a unique risk to the aortic valve, making surgical intervention often necessary to prevent future complications.
*A 7-year-old boy with an 11-mm muscular defect and severe pulmonary vascular disease non-responsive to pulmonary vasodilators*
- This patient likely has **Eisenmenger syndrome**, characterized by **irreversible pulmonary vascular disease** and right-to-left shunting.
- Surgical repair of the VSD is **contraindicated** in such cases and would likely worsen the patient's condition.
*An 11-month-old female infant with a 6-mm membranous defect, without heart failure, pulmonary hypertension, or growth failure*
- Small to moderate membranous VSDs in asymptomatic infants often **close spontaneously**, especially in the first year of life.
- Without signs of **heart failure**, **pulmonary hypertension**, or **growth failure**, a watch-and-wait approach is typically preferred over immediate surgery.
*A 4-month-old male infant with a 12-mm muscular defect, without heart failure, pulmonary hypertension or growth failure*
- Although this is a **large muscular VSD**, the infant is currently **asymptomatic** without heart failure, pulmonary hypertension, or growth failure.
- In the **absence of symptoms or hemodynamic compromise**, initial management includes close observation with medical therapy as needed. Surgery would be indicated if symptoms develop or significant shunting occurs.
- Note: While small muscular VSDs (<5mm) often close spontaneously, large defects like this require vigilant monitoring as they may eventually require intervention.
*A 5-year-old girl with a 2-mm membranous defect, no heart failure, a Qp:Qs ratio less than 2:1, and no growth failure*
- A 2-mm membranous defect is considered a **small VSD**, and a Qp:Qs ratio less than 2:1 indicates an **insignificant shunt**.
- Small VSDs, particularly in older children who are asymptomatic, very often close spontaneously or remain hemodynamically insignificant, and typically do not require surgical intervention.
Congenital heart defects requiring surgery US Medical PG Question 6: A 4-year-old Caucasian male suffers from cyanosis and dyspnea relieved by squatting. Which of the following abnormalities is most likely present?
- A. Atrial septal defect
- B. Coarctation of the aorta
- C. Bicuspid aortic valve
- D. Ventricular septal defect
- E. Tetralogy of Fallot (Correct Answer)
Congenital heart defects requiring surgery Explanation: ***Tetralogy of Fallot***
- **Cyanosis** and **dyspnea relieved by squatting** are the hallmark clinical features of **Tetralogy of Fallot**, making this the correct diagnosis.
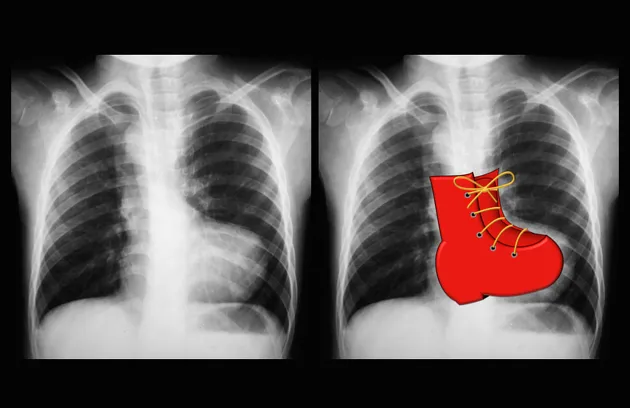
- The condition consists of four anatomic abnormalities: **ventricular septal defect (VSD)**, **right ventricular outflow tract obstruction**, **right ventricular hypertrophy**, and **overriding aorta**.
- The right-to-left shunt across the VSD causes **deoxygenated blood** to enter systemic circulation, producing **cyanosis**.
- **Squatting increases systemic vascular resistance (SVR)**, which decreases the right-to-left shunt, improves pulmonary blood flow, and relieves cyanosis and dyspnea during **"tet spells"**.
*Atrial septal defect*
- ASDs typically cause **left-to-right shunts** and are **acyanotic lesions**.
- Patients may be asymptomatic or present with **exertional dyspnea** and **fatigue** in later childhood or adulthood.
- Cyanosis would only occur if **Eisenmenger syndrome** develops (reversal to right-to-left shunt due to pulmonary hypertension), which is rare at age 4 and does not improve with squatting.
*Coarctation of the aorta*
- This is an **acyanotic** lesion characterized by **narrowing of the descending aorta**.
- Classic findings include **upper extremity hypertension**, **diminished or delayed femoral pulses**, and **lower extremity hypotension**.
- Does not cause cyanosis or squatting relief.
*Bicuspid aortic valve*
- A common **acyanotic** congenital abnormality that may lead to **aortic stenosis** or **regurgitation** over time.
- Usually asymptomatic in childhood; may present with **murmur**, chest pain, or syncope in adulthood.
- Does not cause cyanosis or relief with squatting.
*Ventricular septal defect*
- Isolated VSDs typically cause **left-to-right shunts** and are **acyanotic**.
- May present with **heart failure symptoms** (tachypnea, poor feeding, failure to thrive) in infancy if the defect is large.
- Cyanosis occurs only if **Eisenmenger syndrome** develops (usually takes years to decades), and symptoms are not relieved by squatting.
Congenital heart defects requiring surgery US Medical PG Question 7: A 1-day-old infant in the general care nursery, born at full term by uncomplicated cesarean section delivery, is noted to have a murmur, but otherwise appears well. On examination, respiratory rate is 40/min and pulse oximetry is 96%. Precordium is normoactive. With auscultation, S1 is normal, S2 is single, and a 2/6 systolic ejection murmur is heard at the left upper sternal border. Echocardiography shows infundibular pulmonary stenosis, overriding aorta, ventricular septal defect and concentric right ventricular hypertrophy. Which of the following correlate with the presence or absence of cyanosis in this baby?
- A. The degree of right ventricular outflow tract obstruction (Correct Answer)
- B. The ratio of reduced hemoglobin to oxyhemoglobin
- C. The concentration of hemoglobin
- D. The size of ventricular septal defect
- E. The concentration of pulmonary surfactant
Congenital heart defects requiring surgery Explanation: ***The degree of right ventricular outflow tract obstruction***
- The severity of **pulmonary stenosis** in **tetralogy of Fallot** dictates the amount of blood shunted from the right ventricle to the aorta via the **ventricular septal defect (VSD)**.
- A **less severe obstruction** allows more blood to flow to the lungs, leading to less right-to-left shunting and consequently **less cyanosis**.
*The ratio of reduced hemoglobin to oxyhemoglobin*
- While this ratio directly reflects the presence of cyanosis, it does not explain its *cause* in the context of the given congenital heart defect.
- The question asks what *correlates* with the presence or absence of cyanosis, implying a causal or pathophysiological link rather than a descriptive measure.
*The concentration of hemoglobin*
- **Hemoglobin concentration** affects the *visibility* of cyanosis (e.g., polycythemia can make mild desaturation appear more cyanotic), but it doesn't primarily determine the *presence* or *absence* of shunt-related cyanosis itself.
- A patient can be significantly desaturated with a normal hemoglobin concentration, and the degree of desaturation is largely driven by the shunt.
*The size of ventricular septal defect*
- In tetralogy of Fallot, the **VSD is typically large and non-restrictive**, meaning its size itself doesn't limit blood flow between the ventricles.
- The **pulmonary stenosis** is the primary determinant of the shunt direction and magnitude, not the size of the VSD.
*The concentration of pulmonary surfactant*
- **Pulmonary surfactant** is crucial for maintaining alveolar stability and preventing atelectasis, thereby ensuring efficient gas exchange in the lungs.
- While important for overall respiratory function, it does not directly correlate with the degree of shunting and cyanosis in **tetralogy of Fallot**.
Congenital heart defects requiring surgery US Medical PG Question 8: A 3-year-old boy is brought to a respiratory specialist. The family physician referred the child because of recurrent respiratory infections over the past 2 years. Chest X-rays showed a lesion of < 2 cm that includes glands and cysts in the upper lobe of the right lung. Diseases affecting the immune system were investigated and ruled out. No family history of any pulmonary disease or congenital malformations exists. He was born at full term via a normal vaginal delivery with an APGAR score of 10. Which of the following should be highly considered for effective management of this child’s condition?
- A. Lobectomy
- B. Antibiotics
- C. Observation
- D. Bronchoscopy (Correct Answer)
- E. Pneumonectomy
Congenital heart defects requiring surgery Explanation: ***Bronchoscopy***
- A **bronchoscopy** would be highly considered to **visualize** the lesion, obtain a **biopsy**, and potentially **remove** any obstructing foreign bodies or mucous plugs contributing to recurrent infections.
- Given the description of a lesion < 2 cm with glands and cysts, it is crucial to further characterize it to guide definitive treatment and rule out possibilities like a **bronchial anomaly** or a **benign tumor**.
*Lobectomy*
- **Lobectomy** is a surgical procedure to remove an entire lung lobe; it might be considered if the lesion is definitively diagnosed as a **congenital pulmonary airway malformation (CPAM)** or other localized, symptomatic anomaly, but not as the initial management step without a clear diagnosis.
- Doing a lobectomy without proper diagnosis might be too invasive and aggressive when other less invasive management options are available.
*Antibiotics*
- **Antibiotics** are appropriate for treating the recurrent respiratory infections themselves but will not address the underlying structural lesion causing them.
- While they might provide temporary relief from infections, they do not offer a long-term solution for the **structural abnormality** described.
*Observation*
- **Observation** might be considered for small, asymptomatic lesions, but this child has **recurrent respiratory infections**, suggesting the lesion is clinically significant and warrants intervention.
- Delaying diagnosis and treatment could lead to persistent morbidity and potentially irreversible lung damage.
*Pneumonectomy*
- **Pneumonectomy**, the removal of an entire lung, is a major and highly aggressive surgery reserved for extensive, **life-threatening conditions** such as large malignancies or widespread irreversible lung disease.
- Given the lesion is < 2 cm and localized to one lobe, a pneumonectomy is an **overly extreme measure** and not indicated at this stage.
Congenital heart defects requiring surgery US Medical PG Question 9: A 62-year-old man presents to his primary care physician. He was brought in by his daughter as he has refused to see a physician for the past 10 years. The patient has been having worsening abdominal pain. He claims that it was mild initially but has gotten worse over the past week. The patient has been eating lots of vegetables recently to help with his pain. The patient has a past medical history of constipation and a 50 pack-year smoking history. He is not currently taking any medications. On review of systems, the patient endorses trouble defecating and blood that coats his stool. His temperature is 99.5°F (37.5°C), blood pressure is 197/128 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 98% on room air. On abdominal exam, the patient complains of right upper quadrant tenderness and a palpable liver edge that extends 4 cm beneath the costal margin. Murphy's sign is positive. HEENT exam is notable for poor dentition, normal sclera, and normal extraocular movements. There are no palpable lymph nodes. Laboratory studies are ordered as seen below.
Hemoglobin: 9 g/dL
Hematocrit: 30%
Leukocyte count: 7,500/mm^3 with normal differential
Platelet count: 199,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.0 mEq/L
HCO3-: 23 mEq/L
BUN: 29 mg/dL
Glucose: 197 mg/dL
Creatinine: 1.4 mg/dL
Ca2+: 10.2 mg/dL
Total bilirubin: 1.1 mg/dL
AST: 150 U/L
ALT: 112 U/L
Which of the following is the most likely diagnosis?
- A. Hepatocellular carcinoma
- B. Colon cancer (Correct Answer)
- C. Pancreatic cancer
- D. Acute cholecystitis
- E. Acute appendicitis
Congenital heart defects requiring surgery Explanation: ***Colon cancer***
- The patient's presentation with **worsening abdominal pain**, chronic constipation, **blood coating the stool (hematochezia)**, and **significant anemia** (hemoglobin 9 g/dL, hematocrit 30%) are highly suggestive of **colorectal malignancy**. His **50 pack-year smoking history** is a significant risk factor for colon cancer.
- The **palpable liver edge extending 4 cm below the costal margin** and **elevated AST/ALT** (150/112 U/L) suggest **hepatic metastases**, which are common with advanced colon cancer and explain the hepatomegaly and liver enzyme elevation.
- While the positive Murphy's sign suggests concurrent **acute cholecystitis**, the constellation of chronic GI symptoms (constipation, hematochezia, anemia) indicates that **colon cancer is the underlying primary diagnosis**, with possible complications including liver metastases and secondary cholecystitis (which can occur in cancer patients due to biliary obstruction from liver metastases or other factors).
- This is the **most likely unifying diagnosis** that explains the majority of clinical findings.
*Hepatocellular carcinoma*
- While **hepatocellular carcinoma (HCC)** can cause hepatomegaly, RUQ pain, and elevated liver enzymes, it does not explain the pronounced lower GI symptoms such as **chronic constipation** and **blood coating the stool (hematochezia)**.
- HCC typically requires risk factors like **chronic viral hepatitis (HBV/HCV)** or **cirrhosis**, which are not mentioned in this case. The patient's presentation is more consistent with a primary GI malignancy with hepatic metastases.
*Pancreatic cancer*
- **Pancreatic cancer** typically presents with **epigastric pain radiating to the back**, weight loss, and **painless jaundice** (courvoisier sign), but the bilirubin is only minimally elevated (1.1 mg/dL) here.
- It does not typically cause **hematochezia** or the pattern of **chronic constipation** seen in this patient, making it less likely than colon cancer.
*Acute cholecystitis*
- **Acute cholecystitis** would explain the **RUQ pain**, **positive Murphy's sign**, and **low-grade fever** (99.5°F), and may indeed be present concurrently.
- However, it does NOT explain the **chronic constipation**, **hematochezia**, **significant anemia** (Hgb 9 g/dL), or the chronic nature of symptoms. These findings point to an underlying GI malignancy as the primary diagnosis.
- Acute cholecystitis alone would not cause blood in the stool or chronic anemia, making it less likely to be the primary/most likely diagnosis.
*Acute appendicitis*
- **Acute appendicitis** presents with **acute onset right lower quadrant (RLQ) pain**, rebound tenderness, fever, and typically **leukocytosis** (WBC often >10,000/mm³).
- This patient has **normal WBC** (7,500/mm³), **RUQ pain** (not RLQ), chronic symptoms, and findings suggesting liver involvement, making appendicitis highly unlikely.
Congenital heart defects requiring surgery US Medical PG Question 10: A previously healthy 64-year-old man comes to the physician 3 days after noticing a lump in his right groin while he was bathing. He has no history of trauma to the region. He has hypercholesterolemia and hypertension treated with atorvastatin and labetalol. He has smoked 2 packs of cigarettes daily for 35 years. His vital signs are within normal limits. Examination shows a 4-cm (1.6-in), nontender, pulsatile mass with a palpable thrill at the right midinguinal point. On auscultation, a harsh continuous murmur is heard over the mass. Femoral and pedal pulses are palpable bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Femoral lymphadenopathy
- B. Femoral abscess
- C. Femoral hernia
- D. Arteriovenous fistula of the femoral vessels
- E. Femoral artery aneurysm (Correct Answer)
Congenital heart defects requiring surgery Explanation: ***Femoral artery aneurysm***
- A **pulsatile mass** with a **palpable thrill** and a **harsh continuous murmur** heard over the mass in the groin is highly indicative of an aneurysm with turbulent flow.
- The patient's history of **smoking** and **hypercholesterolemia** are significant risk factors for **atherosclerosis**, which is the most common cause of peripheral aneurysms.
*Femoral lymphadenopathy*
- Lymphadenopathy typically presents as a **nontender, firm, rubbery mass** that is usually **non-pulsatile**.
- It would not typically be associated with a **thrill** or a **harsh continuous murmur**, which are signs of vascular flow.
*Femoral abscess*
- An abscess would present with signs of **inflammation**, such as redness, warmth, tenderness, and possibly fever, none of which are mentioned here.
- An abscess is typically a **non-pulsatile, fluctuant mass** and would not exhibit a thrill or a continuous murmur.
*Femoral hernia*
- A hernia is a protrusion of abdominal contents through a weakened area, often reducible and typically **non-pulsatile**.
- A hernia would not characteristically present with a **thrill** or a **harsh continuous murmur**, which are vascular findings.
*Arteriovenous fistula of the femoral vessels*
- While an AV fistula can cause a **pulsatile mass**, **thrill**, and **continuous murmur**, it typically arises from trauma or iatrogenic injury, which is not present in this case.
- An AV fistula would also likely involve more immediate symptoms and potentially distal ischemia or signs of venous congestion, which are not described.
More Congenital heart defects requiring surgery US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.