Biliary atresia and Kasai procedure US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Biliary atresia and Kasai procedure. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Biliary atresia and Kasai procedure US Medical PG Question 1: A 5-day-old male newborn is brought to the physician by his mother because of yellowish discoloration of the skin for 1 day. The discoloration first appeared on his face and then spread to his trunk. There have been no changes in his bowel habits or urination. He was born at 38 weeks' gestation via uncomplicated vaginal delivery. He is exclusively breastfed every 2–3 hours. Examination shows scleral icterus and jaundice of the face, chest, and abdomen. Laboratory studies show:
Hemoglobin 17.6 g/dL
Reticulocytes 0.3%
Maternal blood group A, Rh-negative
Fetal blood group 0, Rh-positive
Serum
Bilirubin, total 7 mg/dL
Direct 0.6 mg/dL
Free T4 12 μg/dL
Which of the following is the most likely diagnosis?
- A. Biliary atresia
- B. Dubin-Johnson syndrome
- C. Physiological neonatal jaundice (Correct Answer)
- D. Rhesus incompatibility
- E. Congenital hypothyroidism
Biliary atresia and Kasai procedure Explanation: ***Physiological neonatal jaundice***
- This newborn’s jaundice is **unconjugated (indirect) hyperbilirubinemia**, indicated by a total bilirubin of 7 mg/dL and a direct bilirubin of 0.6 mg/dL (direct bilirubin is less than 20% of total).
- The onset of jaundice after 24 hours of age (day 4-5), peak at 3-5 days, resolution within 1-2 weeks, and the absence of other concerning symptoms in an otherwise healthy term infant strongly suggest **physiological jaundice**.
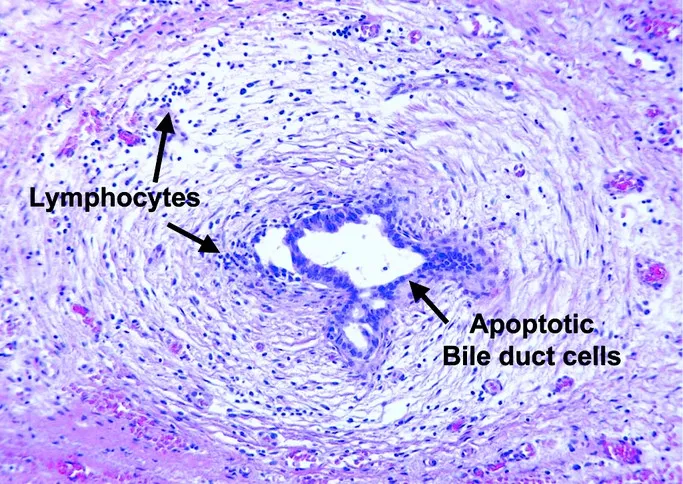
*Biliary atresia*
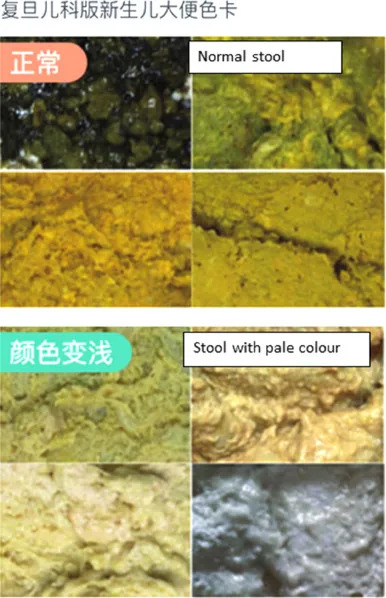
- Characterized by **conjugated (direct) hyperbilirubinemia**, often with dark urine and pale stools, which are not present here.
- Typically presents later, around 2-4 weeks of age, and would show a higher direct bilirubin percentage.
*Dubin-Johnson syndrome*
- An **autosomal recessive disorder** causing conjugated hyperbilirubinemia due to a defect in bilirubin excretion into bile.
- Presents with a high proportion of **direct bilirubin**, not seen in this case.
*Rhesus incompatibility*
- Would cause **hemolytic anemia** with jaundice typically appearing within the first 24 hours of life and often severe.
- The **normal reticulocyte count (0.3%)** and stable hemoglobin (17.6 g/dL) rule out significant hemolysis.
*Congenital hypothyroidism*
- Can cause **prolonged unconjugated jaundice** (lasting beyond 2 weeks of age) due to delayed bilirubin conjugation.
- However, the free T4 level of 7 µg/dL (assuming it's a TSH newborn screen or a total T4 value given the units) is within or near the normal range, and jaundice in this case is not yet prolonged.
Biliary atresia and Kasai procedure US Medical PG Question 2: A 3-week-old newborn male is brought to the physician because of increasing yellowing of his eyes and skin for 2 weeks. The mother has noticed that his stools have been paler than usual for the past week. He is exclusively formula fed, and feeds every 4 hours with a strong sucking reflex. The patient was delivered vaginally at 39 weeks' gestation to a healthy woman without any complications. Vital signs are within normal limits. He is at the 50th percentile for length and at the 65th percentile for weight. Examination shows scleral icterus and jaundice. Abdominal examination reveals a palpable liver 2 cm below the right costal margin without splenomegaly. Serum studies show:
Bilirubin
Total 17 mg/dL
Direct 13.3 mg/dL
Alkaline phosphatase 1700 U/L
AST 53 U/L
ALT 45 U/L
γ-Glutamyl transferase 174 U/L
Blood group B positive
This patient is at increased risk of developing which of the following?
- A. Dark pigmentation on liver biopsy
- B. Hepatic encephalopathy
- C. Kernicterus
- D. Hepatocellular carcinoma
- E. Early liver cirrhosis (Correct Answer)
Biliary atresia and Kasai procedure Explanation: ***Early liver cirrhosis***
- The combination of **persistent jaundice**, **pale stools**, significantly **elevated direct bilirubin**, and **markedly high alkaline phosphatase and γ-glutamyl transferase (GGT)** in a 3-week-old infant points to **biliary atresia**.
- **Biliary atresia** is a progressive fibrosing obliterative cholangiopathy that, if untreated, rapidly leads to **biliary cirrhosis** and liver failure/death within the first year of life.
*Dark pigmentation on liver biopsy*
- **Dark pigmentation** (black liver) on liver biopsy is characteristic of **Dubin-Johnson syndrome**, a rare autosomal recessive disorder of bilirubin metabolism.
- While it causes **conjugated hyperbilirubinemia**, the clinical picture (e.g., profound elevation of ALP and GGT, rapidly progressive liver damage) is not consistent with Dubin-Johnson syndrome.
*Hepatic encephalopathy*
- **Hepatic encephalopathy** is a complication of advanced liver disease, characterized by altered mental status due to the accumulation of toxins (e.g., ammonia) that the liver fails to clear.
- While this patient is at risk of eventually developing liver failure and its complications, **early liver cirrhosis** is a more direct and immediate outcome of untreated biliary atresia in an infant.
*Kernicterus*
- **Kernicterus** (bilirubin encephalopathy) is caused by the deposition of **unconjugated (indirect) bilirubin** in the brain, leading to neurological damage.
- This patient presents with predominantly **conjugated (direct) hyperbilirubinemia**, which typically does not cross the blood-brain barrier and therefore does not cause kernicterus.
*Hepatocellular carcinoma*
- **Hepatocellular carcinoma (HCC)** is a primary liver cancer, typically seen in older children or adults with chronic liver disease (e.g., chronic viral hepatitis, cirrhosis for many years).
- While long-standing, untreated liver cirrhosis can increase the risk of HCC, it is not an immediate or early complication in a 3-week-old infant with presumed biliary atresia.
Biliary atresia and Kasai procedure US Medical PG Question 3: A 28-year-old woman comes to the emergency department for a 1-week history of jaundice and nausea. She recalls eating some seafood last weekend at a cookout. She lives at home with her 2-year-old son who attends a daycare center. The child's immunizations are up-to-date, and his last hepatitis A vaccine was administered 6 weeks ago. The woman's temperature is 37.5°C (99.5°F), pulse is 82/min, and blood pressure is 134/84 mm Hg. Examination shows scleral icterus. The liver is palpated 2-cm below the right costal margin and is tender. Her serum studies show:
Total bilirubin 3.4 mg/dL
Alkaline phosphatase 89 U/L
AST 185 U/L
ALT 723 U/L
Hepatitis A IgM antibody positive
Hepatitis B surface antibody positive
Hepatitis B surface antigen negative
Hepatitis B core IgM antibody negative
Hepatitis C antibody negative
Which of the following health maintenance recommendations is most appropriate for the child at this time?
- A. Isolate the child
- B. Administer hepatitis B immunoglobulin and hepatitis B vaccine
- C. No additional steps are needed (Correct Answer)
- D. Administer hepatitis B immunoglobulin only
- E. Administer hepatitis A vaccine and hepatitis A immunoglobulin
Biliary atresia and Kasai procedure Explanation: ***No additional steps are needed***
- The child received his **last hepatitis A vaccine 6 weeks ago**, which provides adequate protection against hepatitis A infection.
- According to **CDC/ACIP guidelines**, children who have received **at least one dose** of hepatitis A vaccine do **not require post-exposure prophylaxis** (neither additional vaccine nor immunoglobulin) after exposure to hepatitis A.
- One dose of hepatitis A vaccine provides protection within **2-4 weeks**, and since 6 weeks have elapsed, the child is already immune.
- The child's **immunizations are up-to-date**, confirming he is on the appropriate hepatitis A vaccination schedule (2-dose series).
*Administer hepatitis A vaccine and hepatitis A immunoglobulin*
- This would be appropriate for **previously unvaccinated** individuals exposed to hepatitis A, immunocompromised patients, or infants under 12 months.
- However, this child has **already been vaccinated** 6 weeks ago and therefore has adequate protection.
- Administering both vaccine and immunoglobulin is **unnecessary** and not indicated per current guidelines when prior vaccination has occurred.
*Isolate the child*
- Isolation is not the primary recommendation for hepatitis A post-exposure management in household contacts.
- The focus should be on **prevention through immunization**, but this child is already protected by prior vaccination.
- Standard hygiene measures (handwashing) are recommended but formal isolation is not necessary.
*Administer hepatitis B immunoglobulin and hepatitis B vaccine*
- The mother's serology shows **HBsAg negative** and **HBsAb positive**, indicating she is **immune to hepatitis B** (likely from prior vaccination) and not currently infected.
- There is **no risk of hepatitis B transmission** from the mother to the child.
- This intervention addresses the wrong infection entirely.
*Administer hepatitis B immunoglobulin only*
- This is inappropriate because the mother does **not have active hepatitis B infection** (HBsAg negative).
- This option does not address the **hepatitis A exposure**, which is the relevant concern in this scenario.
- Hepatitis B immunoglobulin is indicated only for exposure to hepatitis B, not hepatitis A.
Biliary atresia and Kasai procedure US Medical PG Question 4: A 4-day-old girl presents with jaundice for the last 2 days. Although the patient’s parents were initially told that it was neonatal jaundice and would resolve quickly, they think that the yellow color of the patient’s skin appears to be more obvious today. The patient’s mother reports that the girl eats well, has normal stool and urine color. It’s her first child from the first healthy pregnancy. The patient was born at term via a spontaneous transvaginal delivery without any complications. Family history is significant for a paternal aunt who had 2 babies who died as infants from unknown causes and for a maternal uncle who has unexplained jaundice. On physical examination, the patient is awake, calm, and appears healthy except for the yellow tone of the skin and scleral icterus. Laboratory findings are significant for an elevated level of unconjugated bilirubin. A complete blood count and other routine biochemical blood tests are within expected parameters. The patient is treated with phototherapy, but her hyperbilirubinemia becomes more severe. Which of the following is the most appropriate course of treatment in this patient?
- A. No further treatment needed
- B. Exchange transfusion (Correct Answer)
- C. Furosemide
- D. Phenobarbital
- E. Continuation of phototherapy
Biliary atresia and Kasai procedure Explanation: ***Exchange transfusion***
* This patient's **worsening unconjugated hyperbilirubinemia despite phototherapy**, coupled with a family history suggestive of a genetic predisposition (infant deaths in paternal aunt's children, unexplained jaundice in maternal uncle), indicates a severe form of jaundice, possibly **Crigler-Najjar syndrome type I**.
* **Exchange transfusion** is the most effective treatment to rapidly remove **unconjugated bilirubin** from the blood and prevent **kernicterus** (bilirubin encephalopathy) when phototherapy fails in severe neonatal hyperbilirubinemia.
* The procedure replaces the infant's blood with donor blood, immediately lowering serum bilirubin levels by 50% or more.
*Incorrect: No further treatment needed*
* The patient's **worsening hyperbilirubinemia** despite initial management indicates that further intervention is necessary to prevent severe complications like **kernicterus**.
* Simply observing the patient would be inappropriate given the increasing bilirubin levels that pose a significant risk of permanent neurological damage.
*Incorrect: Furosemide*
* **Furosemide** is a loop diuretic primarily used to treat fluid overload and edema; it does not directly impact bilirubin levels or their metabolism.
* There is no indication of fluid overload or renal impairment in this patient, and diuretics do not enhance bilirubin clearance.
*Incorrect: Phenobarbital*
* **Phenobarbital** induces **hepatic enzymes**, including **UDP-glucuronosyltransferase (UGT1A1)**, which can enhance **bilirubin conjugation** and excretion over time.
* However, it has a **delayed onset of action** (several days to weeks) and is *not* suitable for rapidly reducing dangerously high bilirubin levels in acute, severe hyperbilirubinemia.
* Phenobarbital may have a role in Crigler-Najjar syndrome type II (which has residual enzyme activity), but is ineffective in type I.
*Incorrect: Continuation of phototherapy*
* The vignette clearly states that the patient's **hyperbilirubinemia became more severe despite phototherapy**, indicating that it is no longer effective enough as a sole treatment.
* While phototherapy is a first-line treatment for neonatal jaundice, its failure necessitates a more aggressive intervention to prevent life-threatening complications.
Biliary atresia and Kasai procedure US Medical PG Question 5: A previously healthy 2-year-old girl is brought to the physician because of a 1-week history of yellow discoloration of her skin, loss of appetite, and 3 episodes of vomiting. Her parents also report darkening of her urine and light stools. During the last 2 days, the girl has been scratching her abdomen and arms and has been crying excessively. She was born at 38 weeks' gestation after an uncomplicated pregnancy and delivery. Her family emigrated from Japan 8 years ago. Immunizations are up-to-date. Her vital signs are within normal limits. Examination shows jaundice of her skin and sclerae. Abdominal examination shows a mass in the right upper abdomen. Serum studies show:
Bilirubin (total) 5 mg/dL
Direct 4.2 mg/dL
Aspartate aminotransferase (AST) 20 U/L
Alanine aminotransferase (ALT) 40 U/L
γ-Glutamyltransferase (GGT) 110 U/L
Abdominal ultrasonography shows dilation of the gall bladder and a fusiform dilation of the extrahepatic bile duct. Which of the following is the most likely diagnosis?
- A. Biliary atresia
- B. Mirizzi syndrome
- C. Pancreatic pseudocyst
- D. Hepatic abscess
- E. Biliary cyst (Correct Answer)
Biliary atresia and Kasai procedure Explanation: ***Biliary cyst***
- The combination of **jaundice**, **pruritus**, **light stools**, **dark urine**, an **RUQ mass**, and **fusiform dilation of the extrahepatic bile duct** on ultrasound is highly suggestive of a biliary cyst (specifically a choledochal cyst).
- The **elevated direct bilirubin** and **GGT** are consistent with **biliary obstruction**, while normal AST/ALT suggest minimal hepatocellular injury.
*Biliary atresia*
- Characterized by **progressive obliteration of the extrahepatic bile ducts**, typically presenting with persistent jaundice in the **first few weeks of life**, not at 2 years old.
- Ultrasound in biliary atresia often shows a **nondilated, atretic or absent common bile duct** and a **small or absent gallbladder**, which contradicts the findings of gallbladder dilation and a fusiform mass.
*Mirizzi syndrome*
- This syndrome involves **common hepatic duct obstruction** due to external compression by an impacted **gallstone in the cystic duct or gallbladder neck**.
- It is typically seen in **adults** and would not explain a congenital fusiform dilation of the extrahepatic bile duct.
*Pancreatic pseudocyst*
- A pancreatic pseudocyst is a **collection of pancreatic fluid** usually resulting from **pancreatitis or pancreatic trauma**.
- While it can cause an abdominal mass and obstructive symptoms, it would typically be located near the pancreas, not specifically presenting as a fusiform dilation of the bile duct, and pancreatic enzyme elevations would be more prominent.
*Hepatic abscess*
- A hepatic abscess is a **localized collection of pus in the liver**, often presenting with **fever, RUQ pain**, and elevated inflammatory markers.
- It would show as a **fluid collection within the liver parenchyma** on ultrasound, not a fusiform dilation of the bile duct.
Biliary atresia and Kasai procedure US Medical PG Question 6: A 31-year-old man presents with jaundice, scleral icterus, dark urine, and pruritus. He also says that he has been experiencing abdominal pain shortly after eating. He says that symptoms started a week ago and have not improved. The patient denies any associated fever or recent weight-loss. He is afebrile and vital signs are within normal limits. On physical examination, the patient’s skin appears yellowish. Scleral icterus is present. Remainder of physical examination is unremarkable. Laboratory findings are significant for:
Conjugated bilirubin 5.1 mg/dL
Total bilirubin 6.0 mg/dL
AST 24 U/L
ALT 22 U/L
Alkaline phosphatase 662 U/L
A contrast CT of the abdomen is unremarkable. An ultrasound of the right upper quadrant reveals a normal gallbladder, but the common bile duct is not visible. Which of the following is the next best step in the management of this patient?
- A. Serologies for antimitochondrial antibodies
- B. Endoscopic retrograde cholangiopancreatography (ERCP) (Correct Answer)
- C. HIDA scan
- D. Hepatitis serologies
- E. Antibiotics and admit to observation
Biliary atresia and Kasai procedure Explanation: ***Endoscopic retrograde cholangiopancreatography (ERCP)***
- The patient's presentation with **jaundice, scleral icterus, dark urine, pruritus, unremarked CT abdomen, and significantly elevated alkaline phosphatase** (suggesting **cholestasis**), coupled with an ultrasound showing **non-visualization of the common bile duct**, points to a **biliary obstruction**. ERCP is both diagnostic and therapeutic in this setting, allowing for direct visualization and potential relief of the obstruction.
- The combination of **conjugated hyperbilirubinemia** and isolated elevated alkaline phosphatase with normal AST/ALT indicates a **biliary outflow problem**, warranting further imaging of the biliary tree beyond initial ultrasound and CT.
*Serologies for antimitochondrial antibodies*
- **Antimitochondrial antibodies (AMAs)** are characteristic of **primary biliary cholangitis (PBC)**, which presents with similar symptoms like pruritus and elevated alkaline phosphatase.
- However, PBC primarily affects **intrahepatic bile ducts** and typically does not present with an acute, complete common bile duct obstruction that would lead to non-visualization on ultrasound.
*HIDA scan*
- A **HIDA scan** (hepatobiliary iminodiacetic acid scan) is used to assess **gallbladder function** and patency of the cystic duct in cases of suspected **acute cholecystitis**.
- The ultrasound already showed a normal gallbladder, and the primary concern here is a common bile duct obstruction, not gallbladder inflammation or function.
*Hepatitis serologies*
- **Hepatitis serologies** (e.g., for Hepatitis A, B, C) would be appropriate if the clinical picture suggested **hepatitis** (e.g., markedly elevated AST/ALT, fever, malaise).
- In this patient, the **transaminases (AST, ALT) are normal**, which makes acute viral hepatitis an unlikely primary diagnosis for his acute presentation and cholestatic pattern.
*Antibiotics and admit to observation*
- While **cholangitis** (biliary infection) can cause fever and severe abdominal pain, the patient denies fever and his vital signs are stable, making acute cholangitis less likely as the primary problem needing immediate antibiotics.
- Admitting for observation without further diagnostic intervention would delay identifying and treating the underlying cause of the **biliary obstruction**, which could lead to serious complications.
Biliary atresia and Kasai procedure US Medical PG Question 7: A 45-year-old woman comes to the emergency department complaining of abdominal pain for the past day. The pain is situated in the right upper quadrant, colicky, 8/10, and radiates to the tip of the right shoulder with no aggravating or relieving factors. The pain is associated with nausea but no vomiting. She tried to take over-the-counter antacids which relieved her pain to a certain extent, but not entirely. She does not smoke cigarettes or drink alcohol. She has no past medical illness. Her father died of pancreatic cancer at the age of 75, and her mother has diabetes controlled with medications. Temperature is 38°C (100.4°F), blood pressure is 125/89 mm Hg, pulse is 104/min, respiratory rate is 20/min, and BMI is 29 kg/m2. On abdominal examination, her abdomen is tender to shallow and deep palpation of the right upper quadrant.
Laboratory test
Complete blood count
Hemoglobin 13 g/dL
WBC 15,500/mm3
Platelets 145,000/mm3
Basic metabolic panel
Serum Na+ 137 mEq/L
Serum K+ 3.6 mEq/L
Serum Cl- 95 mEq/L
Serum HCO3- 25 mEq/L
BUN 10 mg/dL
Serum creatinine 0.8 mg/dL
Liver function test
Total bilirubin 1.3 mg/dL
AST 52 U/L
ALT 60 U/L
Ultrasonography of the abdomen shows normal findings. What is the best next step in management of this patient?
- A. Emergency cholecystectomy
- B. CT scan
- C. Reassurance and close follow up
- D. Cholescintigraphy (Correct Answer)
- E. Percutaneous cholecystostomy
Biliary atresia and Kasai procedure Explanation: ***Cholescintigraphy***
- The patient presents with **right upper quadrant pain**, fever, **leukocytosis**, and elevated liver enzymes, pointing towards **acute cholecystitis**. Despite a normal ultrasound, cholescintigraphy (HIDA scan) is the gold standard for diagnosing acute cholecystitis when imaging is equivocal.
- Cholescintigraphy can assess the **patency of the cystic duct**, which is often obstructed in acute cholecystitis, by observing whether the gallbladder fills with tracer.
*Emergency cholecystectomy*
- **Acute cholecystitis** usually requires cholecystectomy, but it's typically performed **after confirmation** of the diagnosis, often after a period of stabilization with antibiotics and fluids, not immediately as an emergency for this stable patient.
- There is no evidence of severe complications such as **gallbladder perforation** or gangrene that would necessitate immediate emergency surgery without further diagnostic confirmation.
*CT scan*
- A **CT scan** is not the primary imaging modality for acute cholecystitis as it is **less sensitive** than ultrasound or cholescintigraphy for detecting gallbladder inflammation and cystic duct obstruction.
- While CT can identify complications such as abscess formation or perforation, the initial diagnostic work-up should focus on confirming the inflammation of the gallbladder itself.
*Reassurance and close follow up*
- The patient's symptoms (severe **colicky pain**, fever, **leukocytosis**, elevated liver enzymes) indicate an **acute inflammatory process** requiring active medical management and diagnosis, not mere reassurance.
- Delaying appropriate diagnosis and treatment for acute cholecystitis can lead to severe complications like gallbladder perforation, sepsis, or cholangitis.
*Percutaneous cholecystostomy*
- **Percutaneous cholecystostomy** is generally reserved for patients with acute cholecystitis who are **too unstable for surgery**, or in cases where surgical risk is very high.
- The patient is hemodynamically stable and does not have contraindications for surgery, making a definitive surgical approach (after diagnosis) preferable over a temporizing measure.
Biliary atresia and Kasai procedure US Medical PG Question 8: A 66-year-old man comes to the physician because of yellowish discoloration of his eyes and skin, abdominal discomfort, and generalized fatigue for the past 2 weeks. He has had dark urine and pale stools during this period. He has had a 10-kg (22-lb) weight loss since his last visit 6 months ago. He has hypertension. He has smoked one pack of cigarettes daily for 34 years. He drinks three to four beers over the weekends. His only medication is amlodipine. His temperature is 37.3°C (99.1°F), pulse is 89/min, respirations are 14/min, and blood pressure is 114/74 mm Hg. Examination shows jaundice of the sclera and skin and excoriation marks on his trunk and extremities. The lungs are clear to auscultation. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 12 g/dL
Leukocyte count 5,000/mm3
Platelet count 400,000/mm3
Serum
Urea nitrogen 28 mg/dL
Creatinine 1.2 mg/dL
Bilirubin
Total 7.0 mg/dL
Direct 5.5 mg/dL
Alkaline phosphatase 615 U/L
Aspartate aminotransferase (AST, GOT) 170 U/L
Alanine aminotransferase (ALT, GPT) 310 U/L
γ-Glutamyltransferase (GGT) 592 U/L (N = 5–50 U/L)
An ultrasound shows extrahepatic biliary dilation. A CT scan of the abdomen shows a 2.5-cm (1-in) mass in the head of the pancreas with no abdominal lymphadenopathy. The patient undergoes biliary stenting. Which of the following is the most appropriate next step in the management of this patient?
- A. Gemcitabine and 5-fluorouracil therapy
- B. Stereotactic radiation therapy
- C. Central pancreatectomy
- D. Gastroenterostomy
- E. Pancreaticoduodenectomy (Correct Answer)
Biliary atresia and Kasai procedure Explanation: ***Pancreaticoduodenectomy***
- The patient presents with **obstructive jaundice**, a **pancreatic head mass** on CT, and **significant weight loss**, highly suggestive of **pancreatic adenocarcinoma**.
- Given the mass is localized to the head of the pancreas without evidence of metastases or lymphadenopathy on CT, **surgical resection (Whipple procedure)** is the only potentially curative treatment.
*Gemcitabine and 5-fluorouracil therapy*
- This is a form of **chemotherapy** commonly used for **advanced or metastatic pancreatic cancer**, or as adjuvant therapy after surgical resection.
- It is not the most appropriate *initial* step for a potentially resectable tumor, as surgery offers the best chance for cure.
*Stereotactic radiation therapy*
- **Radiation therapy** is typically used for **locally advanced, unresectable pancreatic cancer** to control tumor growth and symptoms, or as an adjunct to chemotherapy.
- It is not a primary curative treatment for resectable pancreatic head masses.
*Central pancreatectomy*
- **Central pancreatectomy** is a less common procedure typically reserved for tumors in the **neck or body of the pancreas**, aiming to preserve the pancreatic head and tail.
- It is not appropriate for a mass located in the **head of the pancreas** that is causing biliary obstruction.
*Gastroenterostomy*
- **Gastroenterostomy** is a **palliative surgical procedure** used to bypass an obstructed duodenum, often due to an **unresectable pancreatic head mass** causing gastric outlet obstruction.
- While the patient has obstructive jaundice, the primary goal here is to resect the tumor, not merely bypass the obstruction, especially since it appears resectable.
Biliary atresia and Kasai procedure US Medical PG Question 9: A 62-year-old man presents to his primary care physician. He was brought in by his daughter as he has refused to see a physician for the past 10 years. The patient has been having worsening abdominal pain. He claims that it was mild initially but has gotten worse over the past week. The patient has been eating lots of vegetables recently to help with his pain. The patient has a past medical history of constipation and a 50 pack-year smoking history. He is not currently taking any medications. On review of systems, the patient endorses trouble defecating and blood that coats his stool. His temperature is 99.5°F (37.5°C), blood pressure is 197/128 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 98% on room air. On abdominal exam, the patient complains of right upper quadrant tenderness and a palpable liver edge that extends 4 cm beneath the costal margin. Murphy's sign is positive. HEENT exam is notable for poor dentition, normal sclera, and normal extraocular movements. There are no palpable lymph nodes. Laboratory studies are ordered as seen below.
Hemoglobin: 9 g/dL
Hematocrit: 30%
Leukocyte count: 7,500/mm^3 with normal differential
Platelet count: 199,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.0 mEq/L
HCO3-: 23 mEq/L
BUN: 29 mg/dL
Glucose: 197 mg/dL
Creatinine: 1.4 mg/dL
Ca2+: 10.2 mg/dL
Total bilirubin: 1.1 mg/dL
AST: 150 U/L
ALT: 112 U/L
Which of the following is the most likely diagnosis?
- A. Hepatocellular carcinoma
- B. Colon cancer (Correct Answer)
- C. Pancreatic cancer
- D. Acute cholecystitis
- E. Acute appendicitis
Biliary atresia and Kasai procedure Explanation: ***Colon cancer***
- The patient's presentation with **worsening abdominal pain**, chronic constipation, **blood coating the stool (hematochezia)**, and **significant anemia** (hemoglobin 9 g/dL, hematocrit 30%) are highly suggestive of **colorectal malignancy**. His **50 pack-year smoking history** is a significant risk factor for colon cancer.
- The **palpable liver edge extending 4 cm below the costal margin** and **elevated AST/ALT** (150/112 U/L) suggest **hepatic metastases**, which are common with advanced colon cancer and explain the hepatomegaly and liver enzyme elevation.
- While the positive Murphy's sign suggests concurrent **acute cholecystitis**, the constellation of chronic GI symptoms (constipation, hematochezia, anemia) indicates that **colon cancer is the underlying primary diagnosis**, with possible complications including liver metastases and secondary cholecystitis (which can occur in cancer patients due to biliary obstruction from liver metastases or other factors).
- This is the **most likely unifying diagnosis** that explains the majority of clinical findings.
*Hepatocellular carcinoma*
- While **hepatocellular carcinoma (HCC)** can cause hepatomegaly, RUQ pain, and elevated liver enzymes, it does not explain the pronounced lower GI symptoms such as **chronic constipation** and **blood coating the stool (hematochezia)**.
- HCC typically requires risk factors like **chronic viral hepatitis (HBV/HCV)** or **cirrhosis**, which are not mentioned in this case. The patient's presentation is more consistent with a primary GI malignancy with hepatic metastases.
*Pancreatic cancer*
- **Pancreatic cancer** typically presents with **epigastric pain radiating to the back**, weight loss, and **painless jaundice** (courvoisier sign), but the bilirubin is only minimally elevated (1.1 mg/dL) here.
- It does not typically cause **hematochezia** or the pattern of **chronic constipation** seen in this patient, making it less likely than colon cancer.
*Acute cholecystitis*
- **Acute cholecystitis** would explain the **RUQ pain**, **positive Murphy's sign**, and **low-grade fever** (99.5°F), and may indeed be present concurrently.
- However, it does NOT explain the **chronic constipation**, **hematochezia**, **significant anemia** (Hgb 9 g/dL), or the chronic nature of symptoms. These findings point to an underlying GI malignancy as the primary diagnosis.
- Acute cholecystitis alone would not cause blood in the stool or chronic anemia, making it less likely to be the primary/most likely diagnosis.
*Acute appendicitis*
- **Acute appendicitis** presents with **acute onset right lower quadrant (RLQ) pain**, rebound tenderness, fever, and typically **leukocytosis** (WBC often >10,000/mm³).
- This patient has **normal WBC** (7,500/mm³), **RUQ pain** (not RLQ), chronic symptoms, and findings suggesting liver involvement, making appendicitis highly unlikely.
Biliary atresia and Kasai procedure US Medical PG Question 10: A 50-year-old man is brought to the emergency department because of a 3-day history of left flank pain. The patient has had two episodes of urolithiasis during the last year. He initially had pain with urination that improved with oxycodone. Over the past day, the pain has worsened and he has additionally developed fever and chills. He has hypertension and type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for 20 years. He does not drink alcohol. His current medications include metformin and lisinopril. The patient appears ill and uncomfortable. His temperature is 39.1°C (102.3°F), pulse is 108/min, respirations are 22/min, and blood pressure is 90/62 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. Examination of the back shows left costovertebral angle tenderness. Physical and neurologic examinations show no other abnormalities. Laboratory studies show:
Hemoglobin 14.2 g/dL
Leukocyte count 13,900/mm3
Hemoglobin A1c 8.2%
Serum
Na+ 138 mEq/L
K+ 3.8 mEq/L
Cl-
98 mEq/L
Calcium 9.3 mg/dL
Glucose 190 mg/dL
Creatinine 2.1 mg/dL
Urine pH 8.3
Urine microscopy
Bacteria moderate
RBC 6–10/hpf
WBC 10–15/hpf
WBC casts numerous
Ultrasound shows enlargement of the left kidney with a dilated pelvis and echogenic debris. CT scan shows a 16-mm stone at the left ureteropelvic junction, dilation of the collecting system, thickening of the wall of the renal pelvis, and signs of perirenal inflammation. Intravenous fluid resuscitation and intravenous ampicillin, gentamicin, and morphine are begun. Which of the following is the most appropriate next step in the management of this patient?
- A. Intravenous pyelography
- B. Tamsulosin therapy
- C. Percutaneous nephrostomy (Correct Answer)
- D. Shock wave lithotripsy
- E. Ureteroscopy and stent placement
Biliary atresia and Kasai procedure Explanation: ***Percutaneous nephrostomy***
- The patient presents with **obstructive pyelonephritis** due to a large **ureteral stone** (16 mm) and signs of **urosepsis** (fever, chills, hypotension, leukocytosis, elevated creatinine).
- **Urgent decompression** of the obstructed kidney is critical to relieve pressure, improve renal function, and control infection. A percutaneous nephrostomy provides immediate drainage, which is life-saving in this severe context.
*Intravenous pyelography*
- This is an imaging study used to visualize the urinary tract and is **contraindicated** in patients with **renal insufficiency** (creatinine 2.1 mg/dL) due to the risk of contrast-induced nephropathy.
- Furthermore, it would only provide diagnostic information and **would not address the urgent need for renal decompression** in a patient with urosepsis.
*Tamsulosin therapy*
- **Alpha-blockers** like tamsulosin can facilitate the passage of **smaller ureteral stones** (typically <10 mm) by relaxing ureteral smooth muscle.
- However, this patient has a **large stone (16 mm)**, signs of **sepsis**, and **renal obstruction**, making medical expulsive therapy ineffective and dangerous as a primary intervention.
*Shock wave lithotripsy*
- **Extracorporeal shock wave lithotripsy (ESWL)** is a non-invasive procedure for breaking up kidney stones into smaller fragments.
- It is **contraindicated** in patients with active **urinary tract infections** or **sepsis** because of the risk of disseminating the infection.
*Ureteroscopy and stent placement*
- While ureteroscopy with stent placement can relieve obstruction, it is an **invasive procedure** that may be challenging in a patient with severe sepsis and inflammation.
- **Percutaneous nephrostomy** offers a less invasive and more immediate way to achieve **decompression** in an unstable patient, with definitive stone management to follow once the infection is controlled.
More Biliary atresia and Kasai procedure US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.