Fracture classification and management principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fracture classification and management principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fracture classification and management principles US Medical PG Question 1: A 36-year-old male is taken to the emergency room after jumping from a building. Bilateral fractures to the femur were stabilized at the scene by emergency medical technicians. The patient is lucid upon questioning and his vitals are stable. Pain only at his hips was elicited. Cervical exam was not performed. What is the best imaging study for this patient?
- A. AP and lateral radiographs of hips
- B. Lateral radiograph (x-ray) of hips
- C. Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area
- D. Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area
- E. Computed tomography (CT) scan of cervical spine, hips, and lumbar area (Correct Answer)
Fracture classification and management principles Explanation: ***Computed tomography (CT) scan of cervical spine, hips, and lumbar area***
- In **high-energy trauma** (fall from height), a CT scan is the **gold standard** for evaluating the **spine and pelvis**, providing detailed cross-sectional images superior to plain radiographs.
- Since the **cervical exam was not performed**, cervical spine imaging is **mandatory** per ATLS (Advanced Trauma Life Support) protocols. High-energy falls carry significant risk of **cervical spine injury** even without obvious neurological symptoms.
- CT allows comprehensive assessment of **hip fractures, pelvic injuries, and the entire spine** (cervical, thoracic, lumbar), identifying both obvious and **subtle fractures** that may be missed on plain films.
- This approach provides the most **efficient and thorough evaluation** in the acute trauma setting, allowing for appropriate surgical planning and ruling out life-threatening spinal instability.
*AP and lateral radiographs of hips*
- Plain radiographs provide **limited detail** and may **miss subtle fractures**, particularly in complex areas like the pelvis and acetabulum.
- This option **fails to address cervical spine clearance**, which is essential in all high-energy trauma patients, especially when cervical exam has not been performed.
- Radiographs are insufficient for **comprehensive trauma evaluation** after a fall from height.
*Lateral radiograph (x-ray) of hips*
- A single lateral view is **grossly insufficient** for evaluating hip and pelvic fractures, providing only a **two-dimensional perspective** that can miss significant injuries.
- This option **completely neglects spinal evaluation**, which is dangerous in an uncleared trauma patient with a high-energy mechanism.
*Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area*
- While MRI excels at evaluating **soft tissues, ligaments, and bone marrow**, it is **not the initial imaging modality** for acute bony trauma due to longer scan times and lower sensitivity for acute fractures compared to CT.
- MRI is **time-consuming and impractical** in the emergency setting for initial fracture assessment, potentially delaying definitive treatment.
- CT is superior for evaluating **acute skeletal injuries** in the trauma bay.
*Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area*
- Multiple plain radiographs have **limited sensitivity** for complex or non-displaced fractures, particularly in the **spine and pelvis**, making them inadequate for high-energy trauma evaluation.
- Obtaining multiple radiographic views requires **numerous patient repositionings**, which risks further injury if **spinal instability** is present.
- Plain films provide significantly **less diagnostic information** than CT scanning for trauma assessment.
Fracture classification and management principles US Medical PG Question 2: A 56-year-old man presents to the emergency room after being in a motor vehicle accident. He was driving on an icy road when his car swerved off the road and ran head on into a tree. He complains of severe pain in his right lower extremity. He denies loss of consciousness during the accident. His past medical history is notable for poorly controlled hypertension, hyperlipidemia, and major depressive disorder. He takes enalapril, atorvastatin, and sertraline. His temperature is 99.1°F (37.3°C), blood pressure is 155/85 mmHg, pulse is 110/min, and respirations are 20/min. On exam, he is alert and fully oriented. He is unable to move his right leg due to pain. Sensation is intact to light touch in the sural, saphenous, tibial, deep peroneal, and superficial peroneal distributions. His leg appears adducted, flexed, and internally rotated. An anteroposterior radiograph of his pelvis would most likely demonstrate which of the following findings?
- A. Fracture line extending between the greater and lesser trochanters
- B. Femoral head larger than contralateral side and inferior to acetabulum
- C. Fracture line extending through the femoral neck
- D. Fracture line extending through the subtrochanteric region of the femur
- E. Femoral head smaller than contralateral side and posterior to acetabulum (Correct Answer)
Fracture classification and management principles Explanation: ***Femoral head smaller than contralateral side and posterior to acetabulum***
- This presentation is consistent with a **posterior hip dislocation**, which typically occurs with an **axial load** on a flexed hip, common in head-on collisions.
- On radiographs, the femoral head appears **smaller** due to magnification differences and is displaced **posteriorly** relative to the acetabulum. The affected leg is classically **shortened, adducted, and internally rotated**.
*Fracture line extending between the greater and lesser trochanters*
- This describes an **intertrochanteric hip fracture**, which typically presents with the leg **externally rotated** and **abducted**, not internally rotated and adducted.
- While caused by trauma, the clinical presentation does not align with the patient's physical exam findings.
*Femoral head larger than contralateral side and inferior to acetabulum*
- This describes an **anterior hip dislocation**, which is far less common and would present with the leg typically held in **abduction** and **external rotation**. The femoral head would also appear **larger** due to magnification from being anteriorly displaced.
- The patient's presentation of adduction and internal rotation is inconsistent with an anterior dislocation.
*Fracture line extending through the femoral neck*
- A **femoral neck fracture** usually presents with the leg in **external rotation** and **shortening**, and often involves older patients with osteoporosis after falls.
- While a severe impact could cause this, the characteristic adduction and internal rotation point more strongly to a dislocation.
*Fracture line extending through the subtrochanteric region of the femur*
- A **subtrochanteric fracture** involves the shaft of the femur just below the trochanters and commonly presents with significant pain and inability to bear weight.
- This type of fracture does not typically result in the specific adducted and internally rotated leg position seen with hip dislocations.
Fracture classification and management principles US Medical PG Question 3: A 6-month-old boy is brought to the emergency department by his mother, who informs the doctor that her alcoholic husband hit the boy hard on his back. The blow was followed by excessive crying for several minutes and the development of redness in the area. On physical examination, the boy is dehydrated, dirty, and irritable and when the vital signs are checked, they reveal tachycardia. He cries immediately upon the physician touching the area around his left scapula. The doctor strongly suspects a fracture of the 6th, 7th, or 8th retroscapular posterior ribs. Evaluation of his skeletal survey is normal. The clinician is concerned about child abuse in this case. Which of the following is the most preferred imaging technique as the next step in the diagnostic evaluation of the infant?
- A. Bedside ultrasonography
- B. Magnetic resonance imaging
- C. Babygram
- D. Chest computed tomography scan
- E. Skeletal survey in 2 weeks (Correct Answer)
Fracture classification and management principles Explanation: ***Skeletal survey in 2 weeks***
- A repeat **skeletal survey in 2 weeks** is the most appropriate next step in suspected child abuse cases with an initial normal survey, as it allows for the detection of **healing fractures** that may not be apparent immediately after injury.
- New bone formation and callus development around a fracture site become radiographically visible after approximately 7 to 14 days, improving the detection rate of subtle or undisplaced fractures.
*Bedside ultrasonography*
- While **ultrasonography** can detect acute fractures, especially in cartilage and non-ossified bones, its utility in a comprehensive assessment for multiple non-displaced rib fractures as part of a child abuse workup is limited.
- It is highly **operator-dependent** and may not provide the full skeletal overview required in suspected child abuse.
*Magnetic resonance imaging*
- **MRI** is excellent for evaluating soft tissue injuries, bone marrow edema, and non-ossified cartilaginous structures. However, it is not the primary imaging modality for detecting acute or subacute fractures of ossified bone and requires **sedation** in infants, making it less practical for routine skeletal screening.
- The **high cost** and limited availability of MRI also make it less suitable as a first-line diagnostic tool for rib fractures in this context.
*Babygram*
- A **babygram** is a single large radiograph of an infant's entire body, often used to rapidly assess for gross developmental anomalies or immediate concerns.
- It provides **less detailed imaging** of individual bones compared to a standard skeletal survey and is insufficient for reliably detecting subtle or non-displaced rib fractures.
*Chest computed tomography scan*
- A **chest CT scan** is highly sensitive for detecting acute rib fractures, even subtle ones. However, it exposes the infant to **significant radiation** and is usually reserved for specific clinical indications, such as suspected internal organ injury, rather than as a primary screening tool for rib fractures in child abuse in an otherwise stable patient.
- It does not provide a comprehensive view of the entire skeleton, which is crucial for identifying other potential abuse-related injuries elsewhere.
Fracture classification and management principles US Medical PG Question 4: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Fracture classification and management principles Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Fracture classification and management principles US Medical PG Question 5: A 25-year-old man is admitted to the emergency department because of an episode of acute psychosis with suicidal ideation. He has no history of serious illness and currently takes no medications. Despite appropriate safety precautions, he manages to leave the examination room unattended. Shortly afterward, he is found lying outside the emergency department. A visitor reports that she saw the patient climbing up the facade of the hospital building. He does not respond to questions but points to his head when asked about pain. His pulse is 131/min, respirations are 22/min, and blood pressure is 95/61 mm Hg. Physical examination shows a 1-cm head laceration and an open fracture of the right tibia. He opens his eyes spontaneously. Pupils are equal, round, and reactive to light. Breath sounds are decreased over the right lung field, and the upper right hemithorax is hyperresonant to percussion. Which of the following is the most appropriate next step in management?
- A. Obtain a chest x-ray
- B. Perform a needle thoracostomy (Correct Answer)
- C. Perform an endotracheal intubation
- D. Apply a cervical collar
- E. Perform an open reduction of the tibia fracture
Fracture classification and management principles Explanation: ***Perform a needle thoracostomy***
- The patient presents with **clinical signs of tension pneumothorax**: hypotension (95/61 mm Hg), tachycardia (131/min), decreased breath sounds, and hyperresonance over the right hemithorax following significant trauma from a fall.
- According to **ATLS (Advanced Trauma Life Support) principles**, the primary survey follows the **ABC priority**: Airway, Breathing, Circulation. A **tension pneumothorax is an immediately life-threatening condition** that compromises both breathing and circulation (obstructive shock).
- **Needle thoracostomy (needle decompression)** is the immediate, life-saving intervention for tension pneumothorax and must be performed **before** or concurrent with other interventions. This takes precedence over spinal immobilization when there is an immediate life threat.
- The clinical presentation strongly suggests tension physiology requiring immediate decompression; waiting for imaging would be inappropriate and potentially fatal.
*Apply a cervical collar*
- While **cervical spine protection** is important in this polytrauma patient with head injury and fall mechanism, it does **not take precedence over treating immediately life-threatening conditions** like tension pneumothorax.
- C-spine can be protected with **manual in-line stabilization** during the needle thoracostomy procedure.
- Modern trauma protocols emphasize that **life threats to airway, breathing, and circulation must be addressed immediately**, even if it requires brief spinal movement with appropriate precautions.
*Obtain a chest x-ray*
- **Tension pneumothorax is a clinical diagnosis** that requires immediate intervention without waiting for imaging confirmation.
- The combination of hypotension, tachycardia, decreased breath sounds, and hyperresonance in a trauma patient is sufficient to warrant emergent needle decompression.
- Delaying treatment for imaging in a hemodynamically unstable patient would be dangerous and violates patient safety principles.
*Perform an endotracheal intubation*
- While the patient has a **GCS of approximately 10** (eyes open spontaneously = 4, no verbal response = 1-2, localizes pain = 5-6), intubation is not the immediate priority.
- The **tension pneumothorax must be decompressed first** before attempting intubation, as positive pressure ventilation could worsen the tension pneumothorax and cause cardiovascular collapse.
- If intubation is needed, it should occur after needle decompression.
*Perform an open reduction of the tibia fracture*
- While the open tibia fracture requires urgent surgical management, it is **not immediately life-threatening** in the same timeframe as tension pneumothorax.
- According to ATLS principles, **life-threatening injuries are addressed before limb-threatening injuries**.
- The fracture should be stabilized temporarily, and definitive surgical management can occur after the patient is hemodynamically stable.
Fracture classification and management principles US Medical PG Question 6: A 17-year-old boy comes to the emergency department following an injury during football practice. He fell and landed on the lateral aspect of his right shoulder. He is holding his right arm supported by his left arm, with his right arm adducted against his side. He is tender to palpation directly over the middle third of his clavicle. Radiographs reveal a non-displaced fracture of the middle third of the clavicle. Which of the following is the most appropriate treatment at this time?
- A. Open reduction and internal fixation with a compression plate
- B. Open reduction and internal fixation with an intramedullary nail
- C. Figure-of-eight splinting (Correct Answer)
- D. Mobilization
- E. Open reduction and internal fixation with lag screws
Fracture classification and management principles Explanation: ***Figure-of-eight splinting***
- For **undisplaced or minimally displaced midshaft clavicle fractures**, conservative management with a **simple arm sling or figure-of-eight splint** is the preferred initial treatment.
- Both methods provide **adequate immobilization** and support for healing, especially in pediatric and adolescent patients, with excellent functional outcomes.
- Current evidence suggests **simple sling support** is equally effective and often better tolerated than figure-of-eight splinting.
*Open reduction and internal fixation with a compression plate*
- **ORIF with a compression plate** is typically reserved for **displaced or comminuted clavicle fractures** (displacement >2cm, shortening >2cm, or open fractures), or those with associated neurovascular compromise, which are not present in this non-displaced fracture.
- Surgical intervention for non-displaced fractures carries **risks of infection, hardware irritation**, and non-union that often outweigh the benefits when conservative options are effective.
*Open reduction and internal fixation with an intramedullary nail*
- **Intramedullary nailing** is an alternative surgical option for some clavicle fractures but is generally considered for **displaced or comminuted fracture patterns**, and is not indicated for a non-displaced fracture.
- It involves specific technical challenges and is **less commonly used** for routine, non-displaced mid-shaft clavicle fractures, especially when simpler conservative measures suffice.
*Mobilization*
- **Immediate mobilization** without any form of immobilization would **risk further displacement** of the non-displaced fracture and hinder proper bone healing in the acute phase.
- Although early motion is introduced during the healing process, **initial support and immobilization** is crucial for stability and pain control.
*Open reduction and internal fixation with lag screws*
- **Lag screws** are primarily used for **interfragmentary compression** in specific oblique or spiral fracture patterns, which is not the typical mechanism for midshaft clavicle fractures.
- This method is a form of surgical fixation, which is **not indicated for a non-displaced clavicle fracture** given the excellent outcomes (>95% union rate) with conservative care.
Fracture classification and management principles US Medical PG Question 7: A 36-year-old man comes to the emergency department 4 hours after a bike accident for severe pain and swelling in his right leg. He has not had a headache, nausea, vomiting, abdominal pain, or blood in his urine. He has a history of gastroesophageal reflux disease and allergic rhinitis. He has smoked one pack of cigarettes daily for 17 years and drinks an average of one alcoholic beverage daily. His medications include levocetirizine and pantoprazole. He is in moderate distress. His temperature is 37°C (98.6°F), pulse is 112/min, and blood pressure is 140/80 mm Hg. Examination shows multiple bruises over both lower extremities and the face. There is swelling surrounding a 2 cm laceration 13 cm below the right knee. The lower two-thirds of the tibia is tender to palpation and the skin is pale and cool to the touch. The anterior tibial, posterior tibial, and dorsalis pedis pulses are weak. Capillary refill time of the right big toe is 4 seconds. Dorsiflexion of his right foot causes severe pain in his calf. Cardiopulmonary examination is normal. An x-ray is ordered, which is shown below. Which of the following is the most appropriate next step in management?
- A. Above knee cast
- B. IVC filter placement
- C. Fasciotomy (Correct Answer)
- D. Low molecular weight heparin
- E. Open reduction and internal fixation
Fracture classification and management principles Explanation: ***Fasciotomy***
- The patient's symptoms (severe pain, swelling, pain with passive dorsiflexion, weak pulses, pale/cool skin, and prolonged capillary refill) after a traumatic injury are highly suggestive of **acute compartment syndrome**.
- **Fasciotomy** is the definitive treatment for acute compartment syndrome to relieve pressure and prevent irreversible tissue damage.
*Above knee cast*
- While a cast is used for immobilization of fractures, it would worsen **compartment syndrome** by externally compressing an already swollen limb.
- This patient has signs of compartment syndrome which requires urgent surgical decompression, not just immobilization.
*IVC filter placement*
- **IVC filter placement** is indicated for preventing pulmonary embolism in patients with deep vein thrombosis (DVT) who have contraindications to anticoagulation.
- There is no clinical evidence to suggest DVT in this patient, and the primary concern is acute compartment syndrome.
*Low molecular weight heparin*
- **Low molecular weight heparin (LMWH)** is an anticoagulant used for DVT prophylaxis or treatment.
- It is not indicated for the immediate management of acute compartment syndrome and could increase the risk of bleeding in a patient who likely needs urgent surgery.
*Open reduction and internal fixation*
- **Open reduction and internal fixation (ORIF)** is a surgical procedure to stabilize complex fractures, which may be needed later for a tibial fracture if present.
- However, the immediate priority is to address the limb-threatening acute compartment syndrome before performing definitive fracture repair.
Fracture classification and management principles US Medical PG Question 8: A 23-year-old man is brought to the emergency department because of severe right shoulder pain and inability to move the shoulder for the past 30 minutes. The pain began after being tackled while playing football. He has nausea but has not vomited. He is in no apparent distress. Examination shows the right upper extremity externally rotated and slightly abducted. Palpation of the right shoulder joint shows tenderness and an empty glenoid fossa. The right humeral head is palpated below the coracoid process. The left upper extremity is unremarkable. The radial pulses are palpable bilaterally. Which of the following is the most appropriate next step in management?
- A. Drop arm test
- B. Closed reduction
- C. Neer impingement test
- D. Arthroscopic shoulder repair
- E. Test sensation of the lateral shoulder (Correct Answer)
Fracture classification and management principles Explanation: ***Test sensation of the lateral shoulder***
- The patient presents with classic signs of an **anterior shoulder dislocation**, including **externally rotated** and **abducted upper extremity**, an **empty glenoid fossa**, and a **humeral head palpated below the coracoid**.
- Assessing sensation of the **lateral shoulder** is crucial to check for **axillary nerve injury**, which is a common complication of shoulder dislocations and can cause deltoid weakness and sensory loss over the lateral deltoid region.
*Drop arm test*
- The **drop arm test** is used to evaluate for a **rotator cuff tear**, particularly involving the supraspinatus muscle.
- In this scenario, the primary concern is an acute shoulder dislocation, not a rotator cuff tear, although the latter can coexist.
*Closed reduction*
- While **closed reduction** is the definitive treatment for an acute shoulder dislocation, it should only be performed *after* neurovascular status has been thoroughly assessed.
- Reducing the dislocation before checking for nerve damage could mask an existing injury or worsen it.
*Neer impingement test*
- The **Neer impingement test** is used to diagnose **rotator cuff impingement syndrome**, a condition where soft tissues are compressed in the subacromial space.
- This patient's symptoms are indicative of an acute dislocation, not chronic impingement.
*Arthroscopic shoulder repair*
- **Arthroscopic shoulder repair** is a surgical procedure for certain shoulder conditions, often for recurrent instability or significant structural damage, after initial closed reduction has failed or if there are contraindications to closed reduction.
- It is not the immediate next step in managing an acute, primary shoulder dislocation before proper assessment.
Fracture classification and management principles US Medical PG Question 9: A 50-year-old manual laborer sustained a comminuted distal radius fracture treated with ORIF 3 months ago. Despite supervised hand therapy, he has persistent stiffness with 30-degree wrist extension (normal 70), weak grip strength at 40% of contralateral side, and visible muscle atrophy. He reports burning pain with light touch and keeps his hand wrapped in a sock. Skin appears mottled with decreased hair growth. He is applying for disability and has a pending lawsuit. Evaluate the clinical picture and appropriate next step.
- A. EMG/NCS to evaluate for nerve injury
- B. Psychiatric evaluation for malingering assessment
- C. Repeat surgery for hardware removal and capsular release
- D. Independent functional capacity evaluation
- E. Triple-phase bone scan and referral to pain management (Correct Answer)
Fracture classification and management principles Explanation: ***Triple-phase bone scan and referral to pain management***
- The presence of **allodynia** (pain with light touch), **autonomic dysfunction** (mottled skin, hair changes), and **atrophy** following trauma is classic for **Complex Regional Pain Syndrome (CRPS)**.
- A **triple-phase bone scan** typically shows increased periarticular uptake in the delayed phase, and multidisciplinary **pain management** is the gold standard for treatment.
*EMG/NCS to evaluate for nerve injury*
- While nerve injury can cause pain, it does not explain the **vasomotor changes** and skin/hair trophic changes seen in this patient.
- This patient likely has **CRPS Type I** (reflex sympathetic dystrophy), which occurs in the absence of a defined nerve injury.
*Psychiatric evaluation for malingering assessment*
- Despite the **secondary gain** considerations (lawsuit/disability), the physical findings of **mottled skin** and decreased hair growth are objective clinical signs that cannot be faked.
- Labeling the patient as malingering before ruling out organic conditions like **CRPS** is inappropriate and delays necessary care.
*Repeat surgery for hardware removal and capsular release*
- Additional surgery is often **contraindicated** in the acute/active phase of CRPS as it can significantly worsen the pain and inflammatory response.
- Stiffness in CRPS is due to **neurogenic inflammation** and sympathetic overactivity rather than simple mechanical obstruction by hardware.
*Independent functional capacity evaluation*
- While useful for measuring work readiness, this is a **diagnostic tool** for disability status rather than a clinical management step for an active pathology.
- The priority is to confirm the diagnosis of **CRPS** and initiate treatment to prevent permanent **joint contracture** and functional loss.
Fracture classification and management principles US Medical PG Question 10: A 16-year-old basketball player presents with chronic anterior knee pain worse with jumping and kneeling. Examination shows tenderness at the inferior pole of the patella and pain with resisted knee extension. X-ray shows elongation and fragmentation of the inferior patellar pole. He has failed 6 months of physical therapy, activity modification, and NSAIDs. His AAU season starts in 6 weeks and a college scout will be attending. His parents want definitive treatment. Evaluate the management approach balancing medical and contextual factors.
- A. Recommend season withdrawal, continued conservative management for 6 more months (Correct Answer)
- B. Corticosteroid injection to allow play through season with surgery after
- C. Arthroscopic excision of inferior pole fragments allowing return to play in 4 weeks
- D. Open excision of ossicle with patellar tendon repair, 4-6 month recovery
- E. PRP injection series with continued play and close monitoring
Fracture classification and management principles Explanation: ***Recommend season withdrawal, continued conservative management for 6 more months***
- This patient presents with **Sinding-Larsen-Johansson syndrome**, a traction **apophysitis** of the inferior patellar pole that typically resolves with skeletal maturity and conservative care.
- Despite external pressures like college scouting, standard medical management mandates at least **12 months of conservative treatment** before considering surgery, as outcomes for surgical intervention in adolescents are often poor.
*Corticosteroid injection to allow play through season with surgery after*
- **Intratendinous corticosteroid injections** are strictly contraindicated as they significantly increase the risk of **patellar tendon rupture**.
- While they may provide short-term pain relief, they do not address the underlying **apophysitis** and compromise the structural integrity of the extensor mechanism.
*Arthroscopic excision of inferior pole fragments allowing return to play in 4 weeks*
- Surgical excision is rarely indicated in **skeletally immature** patients and is never the first-line treatment even after 6 months of failed therapy.
- A 4-week return-to-play timeline is clinically unrealistic following any surgical intervention on the **patellar tendon** or bone interface.
*Open excision of ossicle with patellar tendon repair, 4-6 month recovery*
- **Open excision** is considered only in refractory cases after the growth plates have closed and at least one year of non-operative management has failed.
- Performing an invasive repair in a 16-year-old unnecessarily risks damaging the **physes** and may lead to long-term functional deficits.
*PRP injection series with continued play and close monitoring*
- There is currently **insufficient evidence** to support the use of Platelet-Rich Plasma (PRP) as a definitive treatment for pediatric traction apophysitis.
- Continuing high-impact jumping and kneeling while relying on injections does not allow the **traction-induced inflammation** and fragmentation to heal.
More Fracture classification and management principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
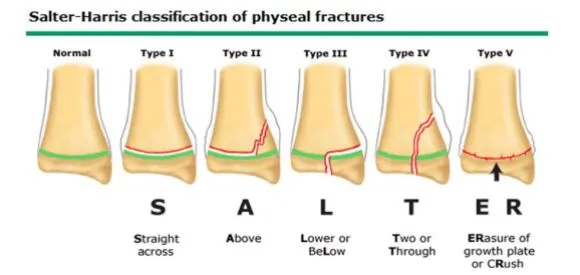 📌 SALTER Mnemonic: Straight, Above, Lower, Through, ERasure/cRush.
📌 SALTER Mnemonic: Straight, Above, Lower, Through, ERasure/cRush.