Arthroscopic procedures overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Arthroscopic procedures overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Arthroscopic procedures overview US Medical PG Question 1: A 21-year-old man comes to the physician for a follow-up examination. Four days ago, he injured his right knee while playing soccer. Increased laxity of the right knee joint is noted when the knee is flexed to 30° and an abducting force is applied to the lower leg. The examination finding in this patient is most likely caused by damage to which of the following structures?
- A. Medial collateral ligament (Correct Answer)
- B. Anterior cruciate ligament
- C. Posterior cruciate ligament
- D. Lateral collateral ligament
- E. Lateral meniscus
Arthroscopic procedures overview Explanation: ***Medial collateral ligament***
- An abducting force applied to the lower leg (a **valgus stress**) when the knee is flexed to 30° tests the integrity of the MCL. Increased laxity indicates damage to this ligament.
- The MCL resists **valgus stress** and is commonly injured in contact sports, especially when a force is applied to the outside of the knee.
*Anterior cruciate ligament*
- The **anterior drawer test** and **Lachman test** (anterior translation of the tibia with the knee flexed) are used to assess ACL integrity.
- ACL injuries usually result from hyperextension, sudden stopping, or pivoting movements, leading to **anterior instability**.
*Posterior cruciate ligament*
- The **posterior drawer test** (posterior translation of the tibia with the knee flexed) is used to assess PCL integrity.
- PCL injuries typically occur from a direct blow to the tibia or an anterior force on the tibia, indicating **posterior instability**.
*Lateral collateral ligament*
- The LCL is assessed by applying an **adducting force** to the lower leg (a **varus stress**).
- Increased laxity during **varus stress** would indicate damage to the LCL.
*Lateral meniscus*
- Meniscal injuries are usually associated with clicking, locking, or catching sensations within the joint, and pain during twisting motions.
- Meniscal tears are primarily diagnosed using specific provocative tests like **McMurray's test** or **Apley's grind test**, not by assessing ligamentous laxity with abducting forces.
Arthroscopic procedures overview US Medical PG Question 2: A surgeon is interested in studying how different surgical techniques impact the healing of tendon injuries. In particular, he will compare 3 different types of suture repairs biomechanically in order to determine the maximum load before failure of the tendon 2 weeks after repair. He collects data on maximum load for 90 different repaired tendons from an animal model. Thirty tendons were repaired using each of the different suture techniques. Which of the following statistical measures is most appropriate for analyzing the results of this study?
- A. Chi-squared
- B. Wilcoxon rank sum
- C. Pearson r coefficient
- D. Student t-test
- E. ANOVA (Correct Answer)
Arthroscopic procedures overview Explanation: ***ANOVA***
- **ANOVA (Analysis of Variance)** is appropriate here because it compares the means of **three or more independent groups** (the three different suture techniques) on a continuous dependent variable (maximum load before failure).
- The study has three distinct repair techniques, each with 30 tendons, making ANOVA suitable for determining if there are statistically significant differences among their mean failure loads.
*Chi-squared*
- The **Chi-squared test** is used for analyzing **categorical data** (frequencies or proportions) to determine if there is an association between two nominal variables.
- This study involves quantitative measurement (maximum load), not categorical data, making Chi-squared inappropriate.
*Wilcoxon rank sum*
- The **Wilcoxon rank sum test** (also known as Mann-Whitney U test) is a **non-parametric test** used to compare two independent groups when the data is not normally distributed or is ordinal.
- While the study has independent groups, it involves three groups, and the dependent variable is continuous, making ANOVA a more powerful and appropriate choice assuming normal distribution.
*Pearson r coefficient*
- The **Pearson r coefficient** measures the **strength and direction of a linear relationship between two continuous variables**.
- This study aims to compare means across different groups, not to determine the correlation between two continuous variables.
*Student t-test*
- The **Student t-test** is used to compare the means of **exactly two groups** (either independent or paired) on a continuous dependent variable.
- This study involves comparing three different suture techniques, not just two, making the t-test unsuitable.
Arthroscopic procedures overview US Medical PG Question 3: A 20-year-old man comes to the clinic complaining of shoulder pain for the past week. He is a pitcher for the baseball team at his university and reports that the pain started shortly after a game. The pain is described as achy and dull, intermittent, 7/10, and is concentrated around the right shoulder area. He denies any significant medical history, trauma, fever, recent illness, or sensory changes but endorses some difficulty lifting his right arm. A physical examination demonstrates mild tenderness of the right shoulder. When the patient is instructed to resist arm depression when holding his arms parallel to the floor with the thumbs pointing down, he reports significant pain of the right shoulder. Strength is 4/5 on the right and 5/5 on the left with abduction of the upper extremities. What nerve innervates the injured muscle in this patient?
- A. Axillary nerve
- B. Long thoracic nerve
- C. Subscapular nerve
- D. Accessory nerve
- E. Suprascapular nerve (Correct Answer)
Arthroscopic procedures overview Explanation: ***Suprascapular nerve***
- The patient's symptoms, including shoulder pain exacerbated by the <b>"empty can" test</b> (resisted arm depression with thumbs down), are highly suggestive of a <b>rotator cuff injury</b>, specifically involving the <b>supraspinatus muscle</b>.
- The <b>suprascapular nerve</b> innervates both the <b>supraspinatus</b> and <b>infraspinatus muscles</b>, which are critical for shoulder abduction and external rotation.
*Axillary nerve*
- The <b>axillary nerve</b> innervates the <b>deltoid muscle</b> and the <b>teres minor muscle</b>.
- Injury to the axillary nerve or these muscles would primarily affect <b>shoulder abduction</b> beyond the initial 15 degrees and external rotation, but the "empty can" test specifically targets the supraspinatus.
*Long thoracic nerve*
- The <b>long thoracic nerve</b> innervates the <b>serratus anterior muscle</b>, which is responsible for scapular protraction and upward rotation.
- Damage to this nerve typically presents with "<b>winged scapula</b>," which is not indicated in this case.
*Subscapular nerve*
- The <b>subscapular nerve</b> innervates the <b>subscapularis muscle</b> (upper and lower subscapular nerves), which is a key internal rotator of the shoulder.
- While it's a rotator cuff muscle, injury to the subscapularis would primarily manifest as difficulty with internal rotation, not typically identified by the "empty can" test.
*Accessory nerve*
- The <b>accessory nerve (cranial nerve XI)</b> innervates the <b>sternocleidomastoid</b> and <b>trapezius muscles</b>.
- Injury to this nerve would result in difficulty shrugging the shoulders or turning the head, not pain related to rotator cuff function.
Arthroscopic procedures overview US Medical PG Question 4: A 63-year-old man presents to his family physician with limited movement in his left shoulder that has progressed gradually over the past 6 years. He previously had pain when moving his shoulder, but the pain subsided a year ago and now he experiences the inability to fully flex, abduct, and rotate his left arm. He had an injury to his left shoulder 10 years ago when he fell onto his arms and ‘stretched ligaments’. He did not seek medical care and managed the pain with NSAIDs and rest. He has diabetes mellitus that is well controlled with Metformin. His blood pressure is 130/80 mm Hg, the heart rate is 81/min, the respiratory rate is 15/min, and the temperature is 36.6°C (97.9°F). Physical examination reveals limitations of both active and passive abduction and external rotation in the left arm. The range of motion in the right glenohumeral joint is normal. The muscles of the left shoulder look less bulky than those of the right shoulder. There is no change in shoulder muscle power bilaterally. The reflexes and sensation on the upper extremities are normal. Which of the following is the next best step for this patient?
- A. NSAID prescription for 1–2 weeks
- B. Arthroscopic capsular release
- C. Physical therapy (Correct Answer)
- D. No interventions are required at this stage
- E. Corticosteroid injections
Arthroscopic procedures overview Explanation: ***Physical therapy***
- This patient presents with symptoms highly suggestive of **adhesive capsulitis**, or **frozen shoulder**, characterized by progressive stiffness and limited range of motion, particularly in abduction and external rotation, following a history of injury and chronic inflammation.
- **Physical therapy** is the cornerstone of treatment for frozen shoulder, focusing on stretching exercises and range-of-motion improvement to restore function.
*NSAID prescription for 1–2 weeks*
- While NSAIDs can manage pain and inflammation, the patient's pain has already subsided, and the primary issue is now **limited range of motion**, not acute pain.
- NSAIDs alone will not address the underlying capsular restriction and will not improve the long-term functional outcome in this chronic phase.
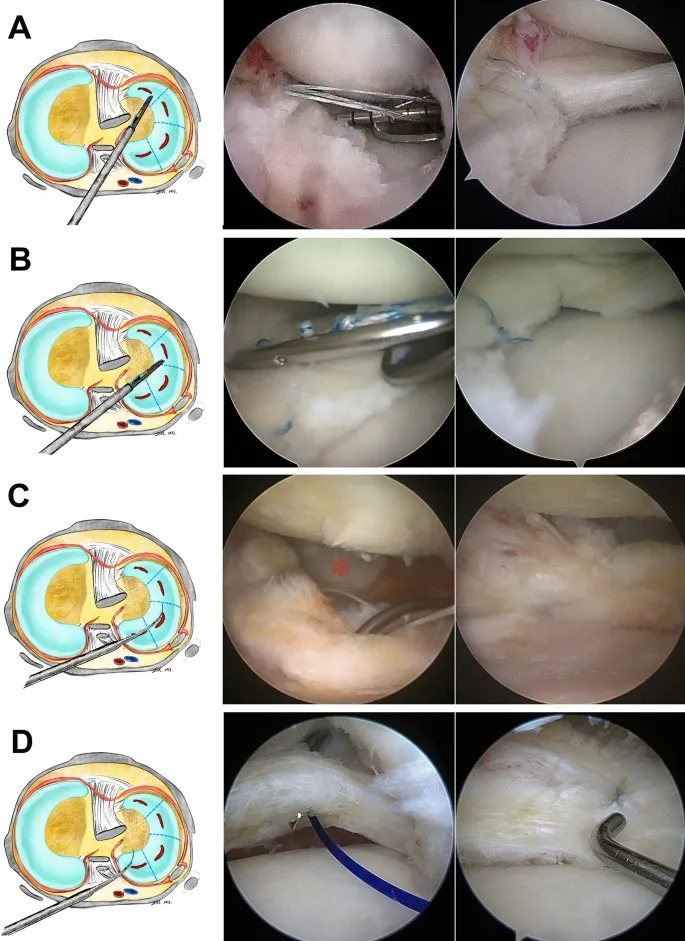
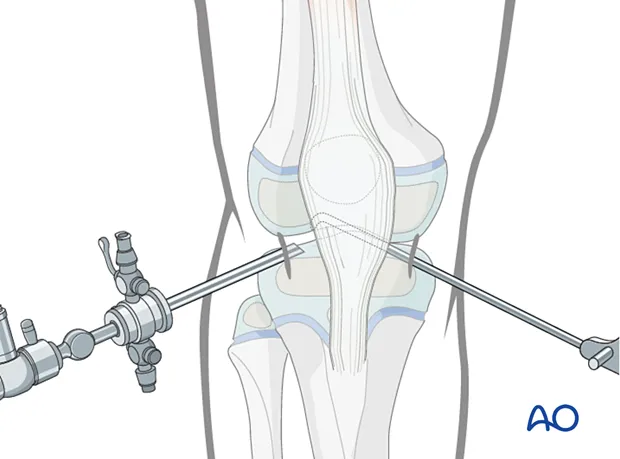
*Arthroscopic capsular release*
- **Arthroscopic capsular release** is an invasive surgical procedure considered for severe, refractory cases of frozen shoulder that have not responded to extensive conservative management.
- It is not typically the initial "next best step," especially before a trial of non-invasive treatments like physical therapy.
*No interventions are required at this stage*
- The patient has significant **functional impairment** and muscle atrophy, indicating a need for intervention to improve his quality of life and prevent further deterioration.
- Ignoring these symptoms would lead to continued disability and potentially worsen muscle loss.
*Corticosteroid injections*
- **Corticosteroid injections** are more effective during the painful, early inflammatory (freezing) stage of adhesive capsulitis, helping to reduce pain and inflammation.
- In the current "thawing" or chronic stiffness stage, where pain has subsided and the primary issue is mechanical restriction, their benefit is limited compared to physical therapy for restoring range of motion.
Arthroscopic procedures overview US Medical PG Question 5: A 33-year-old man presents to his primary care physician for left-sided knee pain. The patient has a history of osteoarthritis but states that he has been unable to control his pain with escalating doses of ibuprofen and naproxen. His past medical history includes diabetes mellitus and hypertension. His temperature is 102.0°F (38.9°C), blood pressure is 167/108 mmHg, pulse is 100/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam reveals a warm and tender joint that is very tender to the touch and with passive range of motion. The patient declines a gait examination secondary to pain. Which of the following is the best next step in management?
- A. Colchicine
- B. Antibiotics
- C. Arthrocentesis (Correct Answer)
- D. IV steroids
- E. Rest, elevation, and ice
Arthroscopic procedures overview Explanation: ***Arthrocentesis***
- The patient presents with unilateral, **acutely painful**, **warm**, and **tender joint** along with **fever**, suggesting a possible **septic joint**.
- **Arthrocentesis** is the definitive diagnostic procedure to rule out **septic arthritis** by analyzing synovial fluid for cell count, culture, and crystal analysis.
*Colchicine*
- Colchicine is used to treat **gout flares**; however, a definitive diagnosis of gout requires **synovial fluid analysis** for crystals, and **septic arthritis** must be ruled out first.
- The patient's presentation with **fever** and **unilateral warmth/tenderness** makes **septic arthritis** a critical concern that takes precedence over presumptive gout treatment.
*Antibiotics*
- While **septic arthritis** is highly suspected, initiating antibiotics without **synovial fluid culture** is premature and can compromise diagnostic accuracy.
- **Arthrocentesis** is necessary to identify the causative organism and guide appropriate **antibiotic therapy**.
*IV steroids*
- **Systemic steroids** could potentially worsen an underlying **septic infection** by suppressing the immune response.
- They are used in inflammatory arthropathies, but **septic arthritis** must be excluded before considering such treatment.
*Rest, elevation, and ice*
- These are supportive measures for joint pain but do not address the underlying cause of the patient's acute, febrile joint pain, especially the potential for **septic arthritis**.
- Delaying proper diagnosis and treatment of a **septic joint** can lead to significant morbidity including **joint destruction** and **sepsis**.
Arthroscopic procedures overview US Medical PG Question 6: Five days after undergoing right knee arthroplasty for osteoarthritis, a 68-year-old man has severe pain in his right knee preventing him from participating in physical therapy. On the third postoperative day when the dressing was changed, the surgical wound appeared to be intact, slightly swollen, and had a clear secretion. He has a history of diabetes, hyperlipidemia, and hypertension. Current medications include metformin, enalapril, and simvastatin. His temperature is 37.3°C (99.1°F), pulse is 94/min, and blood pressure is 130/88 mm Hg. His right knee is swollen, erythematous, and tender to palpation. There is pain on movement of the joint. The medial parapatellar skin incision appears superficially opened in its proximal and distal part with yellow-green discharge. There is blackening of the skin on both sides of the incision. Which of the following is the next best step in the management of this patient?
- A. Vacuum dressing
- B. Antiseptic dressing
- C. Nafcillin therapy
- D. Removal of prostheses
- E. Surgical debridement (Correct Answer)
Arthroscopic procedures overview Explanation: ***Surgical debridement***
- The patient presents with classic signs of **necrotizing fasciitis** or a severe wound infection: rapidly worsening pain, erythema, swelling, **yellow-green discharge**, and crucially, **blackening of the skin** (indicating tissue necrosis).
- Immediate **surgical debridement** is critical for source control, removal of necrotic tissue, and preventing further spread of infection, which can be life-threatening.
*Vacuum dressing*
- A vacuum-assisted closure (VAC) dressing is used for wound management after adequate debridement or for wounds without signs of aggressive infection to promote healing.
- Applying a VAC dressing to a wound with widespread necrosis and active infection, especially necrotizing fasciitis, without prior debridement would be ineffective and potentially harmful.
*Antiseptic dressing*
- While antiseptic dressings can help reduce bacterial load in some superficial wounds, they are entirely insufficient for deep-seated, rapidly spreading infections with tissue necrosis.
- This approach fails to address the underlying necrotic tissue and the extent of the infection, leading to rapid deterioration.
*Nafcillin therapy*
- **Antibiotic therapy** is essential for treating severe infections; however, it must be combined with source control, especially when necrosis is present.
- Giving antibiotics alone without **surgical debridement** in cases of necrotizing fasciitis is inadequate and will not prevent progression of the infection or improve patient outcomes.
*Removal of prostheses*
- While **prosthesis removal** may be necessary in some cases of established periprosthetic joint infection, it is a definitive and often late measure.
- The immediate priority in a rapidly progressing, necrotic wound infection is **surgical debridement** to remove devitalized tissue and control the local infection, prior to considering implant removal unless the infection is directly on the implant.
Arthroscopic procedures overview US Medical PG Question 7: A 25-year-old man comes to the emergency department with right knee pain. He was playing soccer when an opposing player tackled him from the side and they both fell down. He immediately heard a popping sound and felt severe pain in his right knee that prevented him from standing or walking. On physical examination, his right knee is swollen and there is local tenderness, mostly at the medial aspect. External rotation of the right knee elicits a significant sharp pain with a locking sensation. Which of the following structures is most likely injured?
- A. Medial meniscus tear (Correct Answer)
- B. Posterior cruciate ligament
- C. Medial collateral ligament
- D. Anterior cruciate ligament
- E. Lateral meniscus tear
Arthroscopic procedures overview Explanation: ***Medial meniscus tear***
- The injury mechanism (tackle from the side) and symptoms (popping sound, severe pain, swelling, locking sensation, and pain on external rotation) are highly characteristic of a **meniscal tear**.
- **Locking** and pain with specific rotational movements are classic signs of a meniscal injury, and the **medial meniscus** is more frequently injured due to its stronger attachment to the **medial collateral ligament** and less mobility.
*Posterior cruciate ligament*
- Injuries to the **PCL** typically result from direct trauma to the anterior aspect of the tibia with the knee flexed, or from hyperextension, neither of which is consistent with the described injury mechanism.
- A torn PCL primarily causes posterior instability of the tibia, and a **locking sensation** is less common.
*Medial collateral ligament*
- An **MCL injury** is usually caused by a valgus stress (force from the side, pushing the knee inward), which could occur from a lateral tackle.
- While it would cause pain and swelling, an isolated MCL injury does not typically present with a **popping sound**, **locking sensation**, or pain exacerbated by **external rotation** in the same manner as a meniscal tear.
*Anterior cruciate ligament*
- **ACL tears** commonly result from non-contact or contact injuries involving sudden deceleration, cutting, or jumping, often accompanied by a **popping sound**.
- While it causes instability and swelling, an ACL tear generally does not present with a **mechanical locking sensation**; rather, patients often complain of feeling the knee "give way."
*Lateral meniscus tear*
- While a **lateral meniscus tear** can also cause popping, pain, and locking, the mechanism described (tackle from the side, implying a valgus force) typically puts more stress on the **medial aspect** of the knee.
- Pain on **external rotation** is more indicative of a medial meniscal injury compared to a lateral one, which would more likely be aggravated by internal rotation.
Arthroscopic procedures overview US Medical PG Question 8: A 6-year-old boy presents to his primary care physician with hip pain that started this morning. The patient claims the pain is severe and is stopping him from skateboarding. The patient recently recovered from an upper respiratory infection that he caught from his siblings but has otherwise been healthy. The patient has a past medical history of obesity. His temperature is 98.1°F (36.7°C), blood pressure is 100/55 mmHg, pulse is 90/min, respirations are 22/min, and oxygen saturation is 98% on room air. On physical exam, you note an obese boy in no acute distress. Cardiopulmonary exam is within normal limits. Inspection of the hip reveals no abnormalities or swelling. The hip exhibits a normal range of motion and physical exam only elicits minor pain. The patient's gait appears normal and pain is elicited when the patient jumps or runs. Which of the following is the best next step in management for this patient's most likely diagnosis?
- A. Ibuprofen and rest (Correct Answer)
- B. Radiography
- C. CT scan
- D. MRI
- E. Aspiration and broad spectrum antibiotics
Arthroscopic procedures overview Explanation: ***Ibuprofen and rest***
- This patient's presentation with hip pain after an **upper respiratory infection**, normal physical exam findings except for pain on high-impact activities, and absence of fever, points towards **transient synovitis of the hip**.
- **Treatment for transient synovitis** is supportive, involving anti-inflammatory medications like ibuprofen and rest, as it is a self-limiting condition.
*Radiography*
- While imaging might be considered, **radiographs of the hip** are typically normal in transient synovitis and are primarily used to rule out other more serious conditions like Legg-Calvé-Perthes disease or slipped capital femoral epiphysis, which usually present with more distinct physical exam findings or chronic symptoms.
- Given the acute onset, recent viral illness, and mild exam findings, this is not the immediate next step for the most likely diagnosis.
*CT scan*
- A **CT scan** exposes the patient to radiation and is generally not indicated as a first-line diagnostic tool for transient synovitis due to its low diagnostic yield for this condition and higher cost compared to other modalities.
- It would only be considered if there was a strong suspicion of bony pathology not visible on plain radiographs or if surgery was being contemplated.
*MRI*
- An **MRI** would be highly sensitive for detecting inflammation or effusion in the hip joint, but it is an expensive and time-consuming procedure typically reserved for cases where the diagnosis is unclear or other serious conditions are strongly suspected (e.g., osteomyelitis, avascular necrosis).
- It is not necessary for the initial management of suspected transient synovitis, which is a clinical diagnosis.
*Aspiration and broad spectrum antibiotics*
- **Aspiration of the joint** and treatment with broad-spectrum antibiotics are indicated for **septic arthritis**, which is characterized by fever, significant pain with even gentle passive range of motion, and elevated inflammatory markers.
- This patient is afebrile, has only minor pain on physical exam, and has no systemic signs of infection, making septic arthritis highly unlikely.
Arthroscopic procedures overview US Medical PG Question 9: A 45-year-old male presents to his primary care provider with an abnormal gait. He was hospitalized one week prior for acute cholecystitis and underwent a laparoscopic cholecystectomy. He received post-operative antibiotics via intramuscular injection. He recovered well and he was discharged on post-operative day #3. However, since he started walking after the operation, he noticed a limp that has not improved. On exam, his left hip drops every time he raises his left foot to take a step. In which of the following locations did this patient likely receive the intramuscular injection?
- A. Superomedial quadrant of the buttock (Correct Answer)
- B. Superolateral quadrant of the buttock
- C. Anteromedial thigh
- D. Inferomedial quadrant of the buttock
- E. Inferolateral quadrant of the buttock
Arthroscopic procedures overview Explanation: ***Superomedial quadrant of the buttock***
- An injection in the **superomedial quadrant of the buttock** is the most common site for iatrogenic injury to the **superior gluteal nerve**.
- The superior gluteal nerve exits the pelvis through the greater sciatic foramen above the piriformis muscle and runs in the **superomedial** region of the buttock.
- Injury to the superior gluteal nerve results in weakness of the **gluteus medius and minimus muscles**, leading to a **Trendelenburg gait** (hip drops on the contralateral side when lifting that leg), which is consistent with the patient's symptoms.
- This is why the **superolateral quadrant** is recommended for safe IM injections.
*Superolateral quadrant of the buttock*
- The **superolateral quadrant** is the **safest site** for intramuscular gluteal injections precisely because it avoids the superior gluteal nerve.
- This is the recommended injection site to prevent the complication that this patient experienced.
- An injection here would not cause superior gluteal nerve injury or Trendelenburg gait.
*Inferomedial quadrant of the buttock*
- Injections in the **inferomedial quadrant** put the **sciatic nerve** at significant risk of injury.
- Sciatic nerve injury would lead to symptoms affecting the posterior thigh and lower leg, such as **foot drop, loss of ankle reflexes, or paresthesias in the posterior leg and foot**, not isolated hip abductor weakness.
*Inferolateral quadrant of the buttock*
- This area is close to the **sciatic nerve** and **inferior gluteal nerve**.
- Inferior gluteal nerve injury would affect the **gluteus maximus**, leading to difficulty with hip extension (trouble climbing stairs, rising from a chair), not a Trendelenburg gait.
- Sciatic nerve injury would present with foot drop and sensory deficits.
*Anteromedial thigh*
- Injections in the **anteromedial thigh** could injure the **femoral nerve** or its branches.
- This would cause **quadriceps weakness** with impaired knee extension and difficulty walking (buckling knee), not hip abductor weakness or Trendelenburg gait.
- The femoral nerve does not control hip abduction.
Arthroscopic procedures overview US Medical PG Question 10: A 25-year-old male wrestler presents to his primary care physician for knee pain. He was in a wrestling match yesterday when he was abruptly taken down. Since then, he has had pain in his left knee. The patient states that at times it feels as if his knee locks as he moves it. The patient has a past medical history of anabolic steroid abuse; however, he claims to no longer be using them. His current medications include NSAIDs as needed for minor injuries from participating in sports. On physical exam, you note medial joint tenderness of the patient’s left knee, as well as some erythema and bruising. The patient has an antalgic gait as you observe him walking. Passive range of motion reveals a subtle clicking of the joint. There is absent anterior displacement of the tibia relative to the femur on an anterior drawer test. The rest of the physical exam, including examination of the contralateral knee is within normal limits. Which of the following structures is most likely damaged in this patient?
- A. Lateral meniscus
- B. Lateral collateral ligament
- C. Anterior cruciate ligament
- D. Medial collateral ligament
- E. Medial meniscus (Correct Answer)
Arthroscopic procedures overview Explanation: ***Medial meniscus***
- The patient's history of knee trauma during a wrestling match, followed by **locking** and **clicking** sensations, is highly indicative of a meniscal tear.
- **Medial joint line tenderness** specifically points towards involvement of the medial meniscus, which is more commonly injured than the lateral meniscus.
*Lateral meniscus*
- While a meniscal tear is likely, the presence of **medial joint tenderness** makes a lateral meniscus tear less probable.
- A lateral meniscus tear would typically present with pain localized to the **lateral aspect** of the knee.
*Lateral collateral ligament*
- Injury to the LCL typically results from a **varus stress** to the knee, often causing pain on the lateral side and instability, which are not primary complaints here.
- The physical exam did not describe any instability on **varus stress testing**, making an isolated LCL injury less likely.
*Anterior cruciate ligament*
- ACL injuries usually involve a distinct "pop" sensation and **knee instability**, particularly during activities requiring pivoting or cutting.
- The **absent anterior displacement** on the anterior drawer test effectively rules out an acute ACL tear.
*Medial collateral ligament*
- MCL injuries result from a **valgus stress** to the knee, causing pain and tenderness along the medial aspect of the knee and often **instability** during valgus stress testing.
- While there is medial tenderness, the presence of **locking and clicking** strongly points towards a meniscal injury rather than an isolated ligamentous injury, and significant instability is not described.
More Arthroscopic procedures overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.