Orthopedic Surgery Basics

On this page
🏗️ The Orthopedic Foundation: Mastering Bone Architecture
Orthopedic surgery demands more than anatomical knowledge-it requires understanding how bone architecture withstands forces, recognizing injury patterns instantly, and selecting treatments that restore function. You'll build a systematic framework connecting biomechanics to clinical decisions, learning to analyze fractures with diagnostic precision and apply evidence-based algorithms that integrate musculoskeletal pathology with multi-system considerations. This foundation transforms isolated facts into a cohesive decision-making engine for managing orthopedic emergencies and elective cases alike.
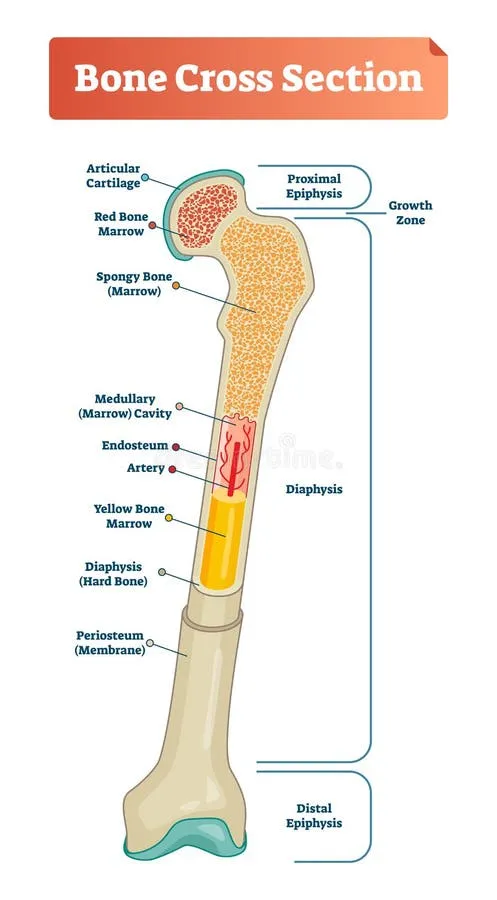
Bone Architecture Fundamentals
Bone tissue demonstrates remarkable engineering efficiency, with cortical bone providing 80% of skeletal mass while cancellous bone contributes 20% but handles 75% of metabolic activity. This dual-architecture system optimizes both structural support and physiological function.
-
Cortical Bone Characteristics
- Density: 1.8-2.0 g/cm³ (4x denser than cancellous)
- Porosity: 5-10% (minimal void space)
- Compressive strength: 130-180 MPa
- Resists axial loading forces
- Primary load-bearing component
- Slower remodeling rate (2-3% annually)
-
Cancellous Bone Properties
- Density: 0.2-0.8 g/cm³ (highly variable)
- Porosity: 75-90% (extensive trabecular network)
- Surface area: 5x greater than cortical bone
- Rapid metabolic turnover (25% annually)
- Primary site for mineral homeostasis
- Enhanced healing capacity
📌 Remember: COMPACT for cortical bone characteristics - Compressive strength, Outer shell, Minimal porosity, Protective function, Axial loading, Circumferential support, Thick walls
Biomechanical Load Distribution
The skeletal system manages forces through sophisticated load-sharing mechanisms. Peak loading during normal activities reaches 3-4x body weight at the hip and 6-8x body weight at the knee during running.
| Bone Region | Cortical % | Cancellous % | Peak Load (xBW) | Failure Threshold | Healing Time |
|---|---|---|---|---|---|
| Femoral Neck | 60% | 40% | 3-4x | 120 MPa | 12-16 weeks |
| Tibial Plateau | 30% | 70% | 6-8x | 85 MPa | 8-12 weeks |
| Vertebral Body | 25% | 75% | 2-3x | 65 MPa | 6-10 weeks |
| Radial Shaft | 85% | 15% | 1-2x | 150 MPa | 10-14 weeks |
| Calcaneus | 20% | 80% | 4-5x | 70 MPa | 8-12 weeks |
Cellular Architecture and Remodeling
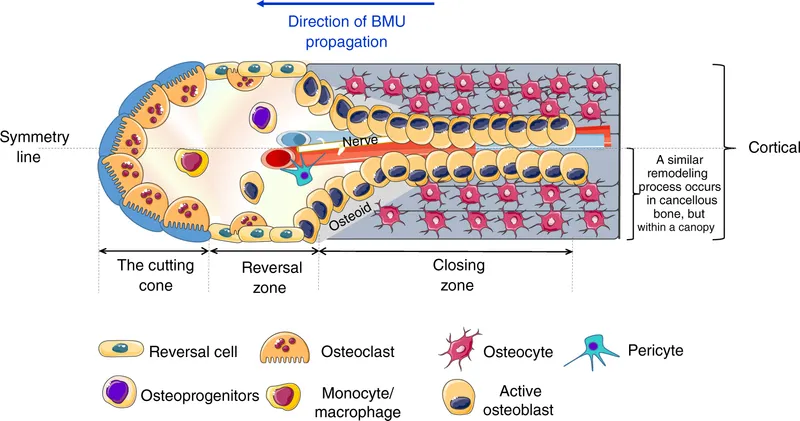
Bone remodeling follows a precisely orchestrated cellular sequence requiring 120-200 days for complete cycle completion. This process maintains skeletal integrity while adapting to mechanical demands.
- Remodeling Sequence Timeline
- Activation Phase (Days 1-3)
- Osteoclast recruitment and activation
- Bone matrix degradation initiation
- Resorption cavity formation
- Resorption Phase (Days 4-21)
- Active bone removal: 20-40 μm/day
- Cavity depth: 40-60 μm (cortical), 200 μm (cancellous)
- Osteoclast apoptosis and clearance
- Formation Phase (Days 22-120)
- Osteoblast recruitment and differentiation
- Collagen matrix deposition: 1-2 μm/day
- Mineralization completion: 85-90% at 30 days
- Activation Phase (Days 1-3)
💡 Master This: Wolff's Law governs bone adaptation - mechanical stress increases bone density by 2-8% annually in loaded regions, while disuse causes 1-2% monthly bone loss
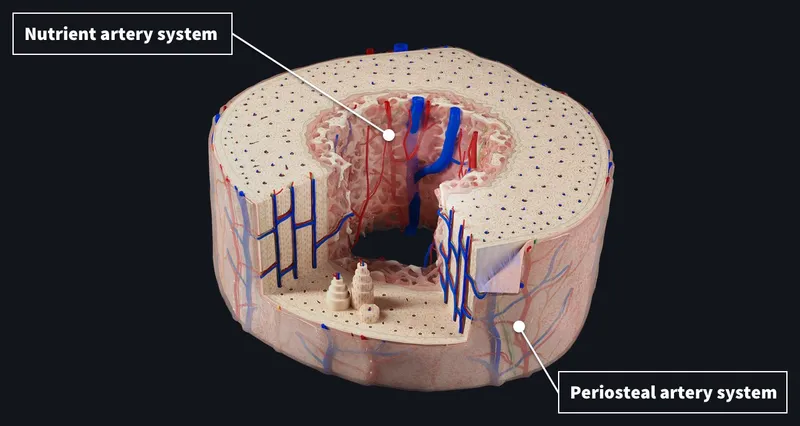
Vascular Supply Architecture
Bone vascularity determines healing potential and surgical outcomes. The dual blood supply system provides redundancy for metabolic demands while creating vulnerability zones where vascular compromise leads to complications.
- Arterial Supply Hierarchy
- Nutrient Artery (Primary supply)
- Provides 60-70% of cortical blood flow
- Enters mid-diaphysis through nutrient foramen
- Branches into ascending/descending medullary vessels
- Periosteal Vessels (Secondary supply)
- Contributes 20-30% of outer cortical perfusion
- Enhanced during fracture healing (3-5x normal flow)
- Critical for callus formation and remodeling
- Metaphyseal Vessels (Tertiary supply)
- Supplies 10-20% of metaphyseal bone
- Anastomoses with medullary circulation
- Vulnerable to growth plate disruption
- Nutrient Artery (Primary supply)
⭐ Clinical Pearl: Fractures in watershed zones (femoral neck, scaphoid waist, fifth metatarsal base) have 15-30% higher nonunion rates due to compromised vascular supply
Understanding this foundational architecture enables prediction of fracture patterns, healing potential, and surgical outcomes. Connect these principles through biomechanical analysis to master load-bearing assessment and treatment planning.
🏗️ The Orthopedic Foundation: Mastering Bone Architecture
⚙️ The Biomechanical Engine: Force Transmission Mastery
Fundamental Stress-Strain Relationships
Bone demonstrates viscoelastic properties with distinct behavioral phases under loading. Understanding these relationships predicts fracture patterns and guides surgical intervention timing.
-
Elastic Phase Characteristics
- Strain range: 0-0.7% deformation
- Complete reversibility upon load removal
- Young's modulus: 15-20 GPa (cortical bone)
- Energy storage: 100% recoverable
- Linear stress-strain relationship
- No permanent structural damage
- Maintains original mechanical properties
-
Plastic Phase Properties
- Strain range: 0.7-3.0% deformation
- Permanent structural changes occur
- Yield strength: 100-150 MPa (cortical)
- Energy absorption: 50-70% dissipated as heat
- Microfracture initiation
- Reduced mechanical properties
- Irreversible matrix damage
Loading Mechanisms and Failure Patterns
Different loading mechanisms create characteristic fracture patterns that reveal injury mechanisms and predict associated injuries. Recognition of these patterns guides diagnostic workup and treatment planning.
| Loading Type | Stress Pattern | Typical Fracture | Energy Level | Associated Injuries |
|---|---|---|---|---|
| Tension | Perpendicular pull | Transverse, clean | Low-moderate | Ligament rupture |
| Compression | Axial crushing | Comminuted, impacted | High | Joint depression |
| Bending | Eccentric loading | Oblique, butterfly | Moderate | Soft tissue stripping |
| Torsion | Rotational shear | Spiral, long oblique | Low-high | Neurovascular injury |
| Shear | Parallel sliding | Horizontal, displaced | Variable | Compartment syndrome |
Rate-Dependent Mechanical Properties
Loading rate dramatically influences bone failure characteristics. High-velocity impacts create different fracture patterns than slow, progressive loading, affecting treatment approaches and prognosis.
-
Low-Rate Loading (<0.01/second)
- Allows stress redistribution and energy dissipation
- Creates simple fracture patterns with minimal comminution
- Preserves 60-80% of surrounding soft tissue viability
- Healing time: 8-12 weeks for uncomplicated fractures
- Ductile failure mode predominates
- Extensive plastic deformation before failure
- Predictable fracture propagation
-
High-Rate Loading (>1.0/second)
- Prevents stress redistribution mechanisms
- Produces complex comminuted patterns with multiple fragments
- Soft tissue damage extends 2-3x fracture zone
- Healing time: 12-20 weeks due to tissue compromise
- Brittle failure mode dominates
- Minimal plastic deformation
- Unpredictable crack propagation
⭐ Clinical Pearl: High-energy mechanisms increase infection risk by 3-5x and nonunion rates by 2-3x compared to low-energy injuries, requiring aggressive soft tissue management
Fatigue and Stress Fracture Mechanics
Repetitive loading below ultimate strength creates cumulative damage leading to fatigue failure. Understanding these mechanisms guides prevention strategies and treatment protocols for stress fractures.
- Fatigue Failure Progression
- Initiation Phase (Cycles 1-10,000)
- Microscopic crack formation at stress concentrators
- Crack length: 10-50 μm
- No clinical symptoms or imaging changes
- Propagation Phase (Cycles 10,000-100,000)
- Stable crack growth: 0.1-1.0 μm/cycle
- Early bone marrow edema on MRI
- Mild activity-related pain develops
- Critical Phase (Cycles 100,000+)
- Unstable crack propagation
- Cortical breach and complete fracture risk
- Severe pain and functional limitation
- Initiation Phase (Cycles 1-10,000)
💡 Master This: Stress fractures occur when loading frequency exceeds bone remodeling capacity (120-200 day cycle), creating net bone loss of 2-5% in high-stress regions
Joint Biomechanics and Load Distribution
Synovial joints distribute loads through sophisticated mechanisms involving articular cartilage, subchondral bone, and surrounding soft tissues. Understanding these relationships guides joint preservation strategies and replacement decisions.
-
Articular Cartilage Properties
- Compressive modulus: 0.5-2.0 MPa (1000x softer than bone)
- Fluid content: 65-80% by weight
- Permeability: 10⁻¹⁵ m⁴/Ns (extremely low)
- Contact stress distribution: 2-5 MPa peak pressures
- Viscoelastic behavior with time-dependent properties
- Load-bearing capacity increases with loading rate
- Nutrition depends on cyclic loading and unloading
-
Load Transfer Mechanisms
- Direct contact: 60-70% of applied load
- Hydrostatic pressure: 20-30% through fluid pressurization
- Interstitial flow: 5-10% through matrix deformation
- Peak pressures occur during heel strike (3-4x body weight)
- Load distribution varies with joint position
- Cartilage thickness correlates with loading magnitude
Connect these biomechanical principles through clinical pattern recognition to master fracture classification and treatment selection strategies.
⚙️ The Biomechanical Engine: Force Transmission Mastery
🎯 The Pattern Recognition Matrix: Clinical Decision Mastery
Mechanism-Based Pattern Recognition
Understanding injury mechanisms enables prediction of fracture patterns, associated injuries, and complications before imaging confirmation. This systematic approach accelerates diagnosis and prevents missed injuries.
-
High-Energy Mechanisms (Motor vehicle, falls >10 feet)
- Expect: Comminuted fractures, multiple injuries, soft tissue compromise
- Look for: Compartment syndrome, vascular injury, contamination
- Timeline: Immediate surgical evaluation within 6-8 hours
- Complications: Infection risk 15-25%, nonunion 10-15%
- Butterfly fragments indicate bending forces
- Spiral patterns suggest torsional loading
- Impaction shows axial compression
-
Low-Energy Mechanisms (Ground-level falls, sports injuries)
- Expect: Simple fracture patterns, isolated injuries
- Look for: Osteoporosis, pathological fractures, ligament injuries
- Timeline: Urgent evaluation within 24-48 hours
- Complications: Infection risk 2-5%, nonunion 3-8%
- Transverse patterns indicate tension failure
- Oblique fractures show combined loading
- Avulsion injuries suggest ligament forces
📌 Remember: SAMPLE history reveals mechanism - Symptoms, Allergies, Medications, Past history, Last meal, Events leading to injury
Systematic Physical Examination Framework
A structured examination sequence identifies critical injuries and guides imaging priorities. Missing key findings delays treatment and increases complication rates.
-
Inspection Priorities (30-second assessment)
- Deformity: Angular, rotational, or length discrepancy
- Swelling: Localized vs diffuse, timing of onset
- Skin integrity: Open wounds, abrasions, contusions
- Position: Guarding, inability to bear weight
- Document with photographs when appropriate
- Compare to contralateral extremity
- Note patient positioning preferences
-
Palpation Sequence (2-minute systematic approach)
- Bony landmarks: Point tenderness, step-offs, crepitus
- Soft tissues: Compartment tension, muscle spasm
- Pulses: Distal circulation, capillary refill <2 seconds
- Temperature: Warmth, coolness, gradient changes
- Use consistent pressure and technique
- Palpate from normal to abnormal areas
- Document findings with anatomical precision
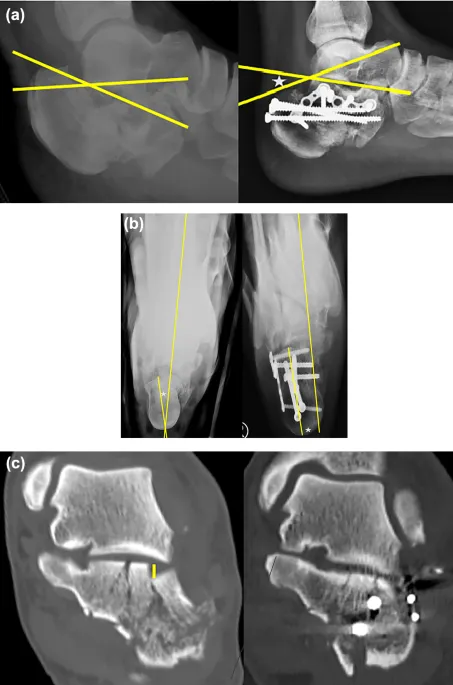
Imaging Strategy and Interpretation
Systematic imaging interpretation prevents missed diagnoses and guides treatment planning. Understanding normal variants and pathological findings accelerates decision-making.
| Imaging Modality | Primary Use | Sensitivity | Specificity | Cost Factor | Radiation Dose |
|---|---|---|---|---|---|
| Plain Radiographs | Initial screening | 85-95% | 90-95% | 1x | 0.1-1.0 mSv |
| CT Scan | Complex fractures | 95-99% | 95-99% | 10x | 5-15 mSv |
| MRI | Soft tissue injury | 90-95% | 85-90% | 20x | None |
| Ultrasound | Dynamic assessment | 70-85% | 80-90% | 2x | None |
| Bone Scan | Stress fractures | 95-99% | 60-70% | 15x | 3-5 mSv |
Red Flag Recognition Patterns
Certain clinical presentations demand immediate intervention to prevent catastrophic complications. Recognizing these patterns enables rapid triage and appropriate resource allocation.
-
Compartment Syndrome Indicators
- Pain: Out of proportion, passive stretch pain >8/10
- Pressure: Compartment pressure >30 mmHg or within 30 mmHg of diastolic BP
- Paresthesias: Early neurological changes in 60-80%
- Paralysis: Late finding indicating irreversible damage
- Time to fasciotomy: <6 hours for optimal outcomes
- Delay increases amputation risk by 25% per hour
- Monitor high-risk fractures every 2-4 hours
-
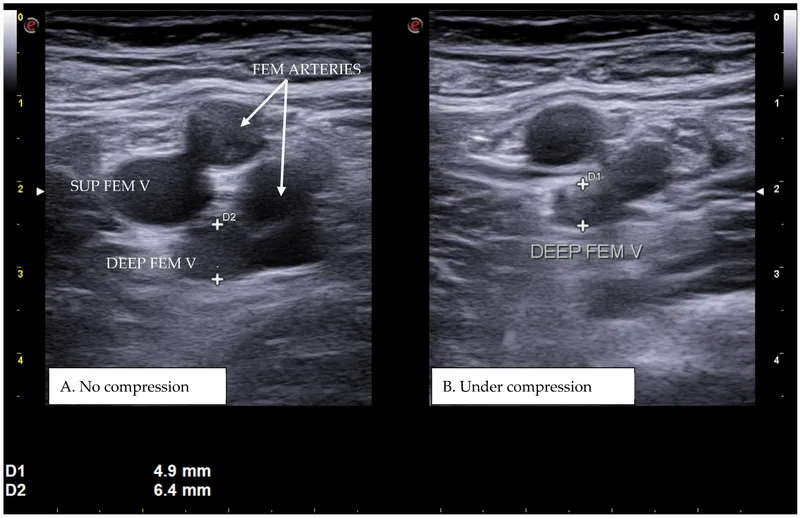
Vascular Injury Patterns
- Hard signs: Absent pulses, active bleeding, expanding hematoma
- Soft signs: Diminished pulses, ABI <0.9, proximity injury
- Associated fractures: Knee dislocation (30% incidence), supracondylar humerus (5-10%)
- Immediate vascular surgery consultation
- Ischemia time >6 hours threatens limb viability
- Document serial neurovascular examinations
💡 Master This: LEAP criteria predict amputation risk - Life-threatening injuries, Energy level, Age >50 years, Poor soft tissue coverage; scores >7 indicate 85% amputation risk
Decision Algorithm Integration
Combining mechanism, examination findings, and imaging results creates systematic decision pathways that optimize outcomes while minimizing complications and costs.
- Treatment Decision Matrix
- Stable, non-displaced: Conservative management 80-90% success
- Unstable, displaced: Surgical fixation 90-95% union rates
- Open fractures: Immediate debridement within 6-8 hours
- Pathological fractures: Oncology consultation, prophylactic fixation
- Consider patient factors: age, activity level, comorbidities
- Evaluate fracture characteristics: location, pattern, displacement
- Assess soft tissue status: open vs closed, contamination level
Connect these recognition patterns through systematic treatment algorithms to master surgical decision-making and complication prevention strategies.
🎯 The Pattern Recognition Matrix: Clinical Decision Mastery
🔬 The Diagnostic Precision Engine: Systematic Analysis Mastery
Fracture Classification Discrimination
Understanding classification systems enables precise communication, treatment selection, and outcome prediction. Each system provides specific prognostic information that guides surgical planning and patient counseling.
- AO/OTA Classification Precision
- Type A: Simple fractures (2 fragments)
- A1: Spiral fractures (low energy)
- A2: Oblique fractures (moderate energy)
- A3: Transverse fractures (high energy)
- Type B: Wedge fractures (3 fragments)
- B1: Spiral wedge (torsional mechanism)
- B2: Bending wedge (butterfly fragment)
- B3: Fragmented wedge (high energy)
- Type C: Complex fractures (>3 fragments)
- C1: Simple articular, simple metaphyseal
- C2: Simple articular, multifragmentary metaphyseal
- C3: Multifragmentary articular and metaphyseal
- Type A: Simple fractures (2 fragments)
| Classification | Union Rate | Infection Risk | Reoperation Rate | Functional Outcome | Time to Union |
|---|---|---|---|---|---|
| AO Type A | 95-98% | 2-5% | 5-8% | Excellent 85% | 8-12 weeks |
| AO Type B | 90-95% | 5-10% | 10-15% | Good 70% | 10-14 weeks |
| AO Type C | 80-90% | 10-20% | 15-25% | Fair 50% | 12-20 weeks |
| Open Grade I | 95-98% | 5-8% | 8-12% | Good 75% | 10-16 weeks |
| Open Grade II | 90-95% | 10-15% | 12-18% | Fair 60% | 12-18 weeks |
| Open Grade III | 75-85% | 20-40% | 25-40% | Poor 40% | 16-24 weeks |
Open Fracture Assessment Framework
Gustilo-Anderson classification guides treatment protocols and predicts outcomes. Accurate grading within 6 hours of injury optimizes antibiotic selection and surgical planning.
-
Grade I Characteristics (Infection rate: 2-5%)
- Wound size: <1 cm
- Mechanism: Low energy, inside-out puncture
- Soft tissue damage: Minimal
- Bone exposure: Limited
- Clean wound edges
- Minimal contamination
- Simple fracture pattern
-
Grade II Features (Infection rate: 5-10%)
- Wound size: 1-10 cm
- Mechanism: Moderate energy
- Soft tissue damage: Moderate without extensive stripping
- Bone exposure: Moderate
- Some contamination present
- Viable tissue coverage possible
- May require limited debridement
-
Grade III Subtypes (Infection rate: 10-50%)
- IIIA: Adequate soft tissue coverage despite extensive laceration
- IIIB: Inadequate soft tissue coverage, requires flap reconstruction
- IIIC: Associated arterial injury requiring vascular repair
- High-energy mechanisms
- Extensive contamination
- Significant bone and soft tissue loss
⭐ Clinical Pearl: Upgrade classification if >6 hours to treatment, farmyard contamination, or high-energy mechanism regardless of wound size; infection rates increase 2-3x with delayed treatment
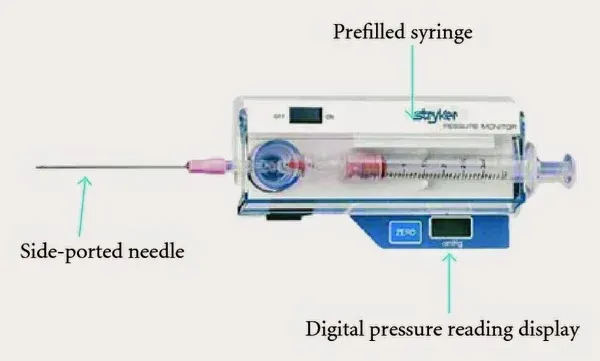
Compartment Syndrome Diagnostic Criteria
Compartment syndrome requires immediate recognition and treatment within 6 hours to prevent permanent disability. Objective measurements supplement clinical findings for accurate diagnosis.
-
Pressure Measurement Thresholds
- Normal: 0-8 mmHg
- Elevated: >15 mmHg (monitor closely)
- Critical: >30 mmHg or within 30 mmHg of diastolic BP
- Absolute indication: >40 mmHg or delta pressure <30 mmHg
- Delta pressure = Diastolic BP - Compartment pressure
- Continuous monitoring in high-risk patients
- Multiple compartment assessment required
-
Clinical Progression Timeline
- 0-2 hours: Pain out of proportion, early paresthesias
- 2-4 hours: Passive stretch pain, decreased sensation
- 4-6 hours: Motor weakness, absent pulses (late finding)
- >6 hours: Irreversible muscle necrosis, contracture formation
- 5 P's are late findings: Pain, Pallor, Paresthesias, Paralysis, Pulselessness
- Early diagnosis based on clinical suspicion
- Compartment pressure monitoring in unconscious patients
Infection Diagnosis and Staging
Musculoskeletal infections require rapid diagnosis and aggressive treatment. Laboratory markers and imaging findings guide antibiotic selection and surgical planning.
| Parameter | Normal | Acute Infection | Chronic Infection | Post-Operative | Significance |
|---|---|---|---|---|---|
| WBC Count | 4-11 K/μL | >15 K/μL | Variable | 10-15 K/μL | Systemic response |
| ESR | <20 mm/hr | >50 mm/hr | >30 mm/hr | >40 mm/hr | Inflammation marker |
| CRP | <3 mg/L | >50 mg/L | >20 mg/L | >100 mg/L | Acute phase protein |
| Procalcitonin | <0.25 ng/mL | >2.0 ng/mL | Variable | >0.5 ng/mL | Bacterial infection |
| Synovial WBC | <200/μL | >50,000/μL | >25,000/μL | Variable | Local infection |
Pathological Fracture Evaluation
Distinguishing pathological from traumatic fractures guides oncological workup and treatment planning. Specific patterns suggest underlying pathology requiring immediate evaluation.
- High-Risk Patterns
- Location: Proximal femur, spine, pelvis, humerus
- Mechanism: Low-energy or atraumatic
- Age: >50 years (metastatic) or <20 years (primary tumor)
- Imaging: Lytic lesions, cortical destruction, soft tissue mass
- Mirels score >8 indicates prophylactic fixation
- Biopsy before stabilization in suspected primary tumors
- Staging studies before surgical intervention
Connect these diagnostic principles through evidence-based treatment algorithms to master therapeutic decision-making and outcome optimization strategies.
🔬 The Diagnostic Precision Engine: Systematic Analysis Mastery
⚖️ The Treatment Algorithm Engine: Evidence-Based Decision Mastery
Surgical vs Conservative Decision Matrix
Treatment selection depends on fracture characteristics, patient factors, and functional demands. Systematic evaluation prevents inappropriate treatment choices and optimizes outcomes.
-
Conservative Treatment Indications
- Displacement: <2 mm or <10° angulation
- Stability: Inherently stable fracture patterns
- Patient factors: High surgical risk, limited functional demands
- Success rates: 85-95% for appropriate indications
- Healing time: 6-12 weeks depending on location
- Functional outcomes: 80-90% return to baseline
- Complication rates: <5% for appropriate cases
-
Surgical Fixation Criteria
- Displacement: >2 mm articular step-off, >20° angulation
- Instability: Unstable fracture patterns, ligamentous injury
- Functional demands: High activity level, occupational requirements
- Success rates: 90-98% union rates with appropriate technique
- Operating time: 1-3 hours depending on complexity
- Hospital stay: 1-3 days for routine cases
- Return to function: 3-6 months for complex injuries
| Treatment Option | Union Rate | Infection Risk | Reoperation Rate | Functional Score | Cost Factor |
|---|---|---|---|---|---|
| Conservative | 85-95% | <1% | 5-10% | 80-90% | 1x |
| ORIF | 95-98% | 2-5% | 8-12% | 85-95% | 5x |
| External Fixation | 90-95% | 5-15% | 15-25% | 70-85% | 3x |
| Arthroplasty | 98-99% | 1-3% | 5-8% | 75-90% | 8x |
| Arthrodesis | 95-98% | 3-8% | 10-15% | 70-80% | 6x |
Timing and Urgency Classification
Surgical timing affects outcomes, complication rates, and resource utilization. Understanding urgency classifications optimizes scheduling and prevents complications.
-
Emergent (Within 6 hours)
- Indications: Open fractures, compartment syndrome, vascular injury
- Rationale: Prevent infection, tissue necrosis, limb loss
- Outcomes: 2-3x better with appropriate timing
- Complications: 50-75% increase with delay
- Immediate OR availability required
- Multidisciplinary team coordination
- Damage control principles
-
Urgent (Within 24 hours)
- Indications: Unstable spine fractures, hip fractures in elderly
- Rationale: Prevent secondary complications, early mobilization
- Outcomes: 20-30% better functional results
- Mortality: 15-25% reduction with early surgery
- Optimize medical comorbidities
- Coordinate anesthesia clearance
- Prepare appropriate implants
-
Elective (Within 1-2 weeks)
- Indications: Stable fractures requiring fixation
- Rationale: Allow swelling resolution, optimize patient condition
- Outcomes: Similar to urgent when appropriately delayed
- Planning: Comprehensive preoperative optimization
- Soft tissue condition assessment
- Implant planning and templating
- Patient education and consent

⭐ Clinical Pearl: Hip fracture surgery within 24 hours reduces 1-year mortality by 19% and 30-day complications by 25% in patients >65 years
Implant Selection Strategy
Choosing appropriate implants depends on fracture pattern, bone quality, patient factors, and surgeon experience. Systematic selection optimizes outcomes and minimizes complications.
-
Plate Fixation Indications
- Fracture types: Metaphyseal, diaphyseal with good bone quality
- Advantages: Anatomical reduction, stable fixation, early mobilization
- Disadvantages: Extensive exposure, soft tissue stripping
- Success rates: 95-98% union, 5-10% complication rate
- Locking vs conventional based on bone quality
- Bridge vs compression plating technique
- Minimally invasive vs open approaches
-
Intramedullary Nail Applications
- Fracture types: Diaphyseal, some metaphyseal patterns
- Advantages: Load-sharing, minimal soft tissue disruption
- Disadvantages: Technical demands, specific instrumentation
- Success rates: 96-99% union, 3-8% complication rate
- Reamed vs unreamed based on bone quality
- Static vs dynamic locking options
- Entry point and reduction techniques
-
External Fixation Scenarios
- Indications: Damage control, infected nonunions, complex soft tissue injury
- Advantages: Minimal surgical trauma, adjustable reduction
- Disadvantages: Pin site complications, patient compliance
- Success rates: 85-95% union, 15-30% complication rate
- Temporary vs definitive treatment
- Hybrid vs circular frame constructs
- Pin site care protocols
Postoperative Protocol Optimization
Standardized postoperative protocols improve outcomes, reduce complications, and accelerate recovery. Evidence-based pathways guide rehabilitation and monitoring.
-
Immediate Postoperative (0-48 hours)
- Pain management: Multimodal analgesia, regional blocks
- Monitoring: Neurovascular status every 2-4 hours
- Mobilization: Early weight-bearing as tolerated for stable fixation
- Complications: DVT prophylaxis, infection surveillance
- Continuous passive motion for articular fractures
- Compartment monitoring in high-risk cases
- Wound inspection and dressing changes
-
Early Recovery (2-6 weeks)
- Radiographic: Weekly films for 3 weeks, then biweekly
- Physical therapy: Range of motion, strengthening progression
- Weight-bearing: Progressive loading based on fracture healing
- Return to work: 2-8 weeks for sedentary, 6-12 weeks for manual labor
- Callus formation assessment
- Hardware position monitoring
- Functional milestone achievement
💡 Master This: RICE postoperative protocol - Rest appropriate tissues, Ice for swelling control, Compression dressings, Elevation above heart level; reduces complications by 30-40%
Connect these treatment algorithms through comprehensive outcome assessment to master long-term patient management and complication prevention strategies.
⚖️ The Treatment Algorithm Engine: Evidence-Based Decision Mastery
🔗 The Integration Command Center: Multi-System Mastery
Cardiovascular-Orthopedic Integration
Musculoskeletal trauma significantly impacts cardiovascular function through blood loss, inflammatory responses, and immobilization effects. Understanding these relationships guides resuscitation and prevents complications.
-
Hemorrhage Assessment and Management
- Femur fracture: Blood loss 1-2 liters (closed), 2-3 liters (open)
- Pelvic fracture: Blood loss 2-4 liters, potential exsanguination
- Multiple fractures: Cumulative loss >40% blood volume
- Shock threshold: >20% blood volume loss (>1000 mL in 70kg adult)
- Class I: <15% loss, minimal symptoms
- Class II: 15-30% loss, tachycardia, anxiety
- Class III: 30-40% loss, hypotension, confusion
- Class IV: >40% loss, severe shock, obtundation
-
Thromboembolism Risk Stratification
- High-risk procedures: Hip/knee arthroplasty, spine surgery, trauma
- Patient factors: Age >60, obesity (BMI >30), malignancy
- Immobilization: DVT risk 2-3% per day of bed rest
- PE incidence: 0.5-2% orthopedic surgery, 15-20% mortality untreated
- Mechanical prophylaxis: 40-60% risk reduction
- Chemical prophylaxis: 60-80% risk reduction
- Combined approach: 80-90% risk reduction
| Risk Factor | DVT Risk Increase | PE Risk Increase | Duration of Risk | Prophylaxis Duration |
|---|---|---|---|---|
| Hip Fracture | 10-15x | 8-12x | 3-6 months | 35 days |
| Knee Replacement | 5-8x | 4-6x | 2-3 months | 14 days |
| Spine Surgery | 3-5x | 2-4x | 1-2 months | 7-10 days |
| Multiple Trauma | 15-20x | 10-15x | 6-12 months | Variable |
| Immobilization | 2-3x | 2-3x | Duration + 2 weeks | Until mobile |
Neurological-Musculoskeletal Coordination
The nervous system controls movement, sensation, and healing responses. Neurological injuries complicate orthopedic management while musculoskeletal trauma can cause secondary neurological damage.
-
Spinal Cord Injury Integration
- Complete injury: 0% motor/sensory function below level
- Incomplete injury: Variable preservation, better prognosis
- Neurogenic shock: Hypotension, bradycardia, hypothermia
- Autonomic dysreflexia: Hypertensive crisis in injuries >T6
- ASIA scale assessment within 72 hours
- Methylprednisolone controversial, 8-hour window
- Early mobilization prevents complications
-
Peripheral Nerve Injury Patterns
- Neuropraxia: Temporary dysfunction, full recovery in 6-12 weeks
- Axonotmesis: Axon damage, regeneration at 1 mm/day
- Neurotmesis: Complete division, surgical repair required
- Recovery timeline: 3-6 months for proximal, 12-18 months for distal
- Electrodiagnostic studies at 3-4 weeks
- Surgical exploration if no improvement at 3-6 months
- Tendon transfers for permanent deficits
⭐ Clinical Pearl: Tinel's sign progression indicates nerve regeneration; advancing tingling suggests 1 mm/day axonal growth, predicting functional recovery timeline
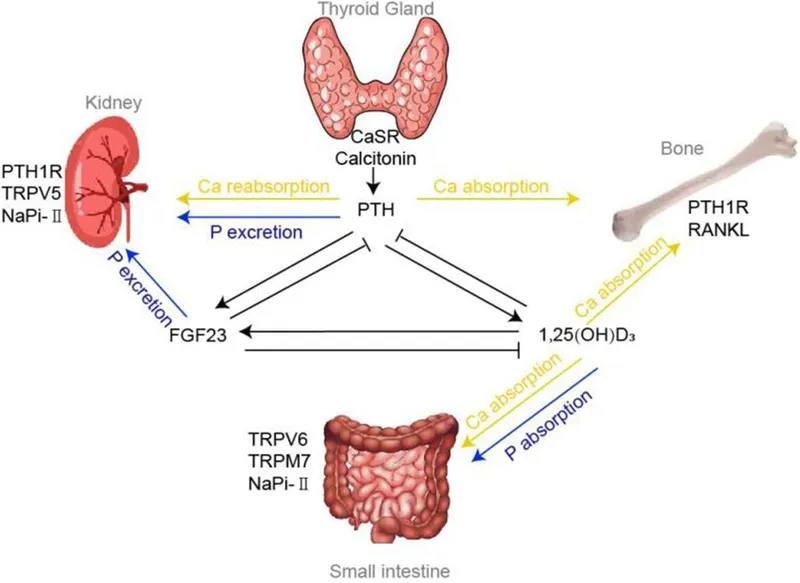
Metabolic-Endocrine Bone Health
Bone healing depends on complex metabolic processes involving calcium homeostasis, vitamin D metabolism, and hormonal regulation. Understanding these relationships optimizes healing and prevents complications.
-
Calcium-Phosphate Homeostasis
- Serum calcium: 8.5-10.5 mg/dL (ionized 4.5-5.5 mg/dL)
- Phosphate levels: 2.5-4.5 mg/dL
- PTH response: Increases calcium absorption, phosphate excretion
- Vitamin D: 25(OH)D >30 ng/mL optimal for bone health
- Deficiency in >50% of fracture patients
- Supplementation improves healing by 15-25%
- Monitor levels every 3-6 months
-
Hormonal Influences on Healing
- Growth hormone: Stimulates osteoblast activity, peaks during sleep
- Thyroid hormones: T3/T4 regulate bone turnover
- Sex hormones: Estrogen/testosterone maintain bone density
- Cortisol: Inhibits bone formation, increases resorption
- Diabetes delays healing by 30-50%
- Smoking reduces healing by 25-40%
- NSAIDs may delay union by 10-20%
Immune System-Healing Integration
Fracture healing involves coordinated inflammatory and immune responses. Understanding these processes guides treatment timing and optimization strategies.
-
Inflammatory Phase (Days 1-7)
- Hematoma formation: Platelet aggregation, fibrin clot
- Inflammatory mediators: IL-1, TNF-α, PDGF release
- Cellular infiltration: Neutrophils, macrophages, lymphocytes
- Vascular response: Increased permeability, angiogenesis initiation
- Peak inflammation at 24-48 hours
- Anti-inflammatory drugs may impair healing
- Infection risk highest during this phase
-
Repair Phase (Days 7-21)
- Soft callus formation: Chondrocytes, type II collagen
- Angiogenesis: New vessel formation, oxygen delivery
- Osteoblast recruitment: Bone matrix deposition begins
- Growth factors: BMP, TGF-β, IGF-1 expression
- Callus volume peaks at 2-3 weeks
- Mechanical stimulation enhances formation
- Smoking significantly impairs this phase
💡 Master This: HEAL factors optimize bone repair - Healthy nutrition (protein 1.2-1.6 g/kg/day), Exercise (weight-bearing as tolerated), Avoid smoking/NSAIDs, Limit alcohol (<2 drinks/day)
Connect these integration principles through comprehensive patient optimization to master holistic orthopedic care and outcome maximization strategies.
🔗 The Integration Command Center: Multi-System Mastery
🎯 The Clinical Mastery Arsenal: Rapid Decision Tools
Emergency Decision Matrix
Critical situations demand immediate recognition and systematic response. These decision trees guide rapid triage and intervention priorities.
-
Trauma Priority Assessment (30-second evaluation)
- Life-threatening: Pelvic fracture with shock, open femur with bleeding
- Limb-threatening: Compartment syndrome, vascular injury, open Grade III
- Function-threatening: Displaced articular fractures, spine instability
- Routine urgent: Closed displaced fractures, stable spine injuries
- ATLS protocol takes precedence over orthopedic injuries
- Damage control principles for multiply injured patients
- Golden hour concept for optimal outcomes
-
Critical Threshold Recognition
- Compartment pressure: >30 mmHg or <30 mmHg from diastolic
- Blood loss: >20% volume (>1000 mL) indicates shock
- Ischemia time: >6 hours threatens limb viability
- Open fracture: <6 hours to debridement optimal
- ABI <0.9 indicates vascular compromise
- Capillary refill >3 seconds suggests poor perfusion
- Neurological deficit requires immediate evaluation
| Emergency Condition | Time Window | Critical Action | Success Rate | Complication if Delayed |
|---|---|---|---|---|
| Compartment Syndrome | <6 hours | Fasciotomy | 95% | Amputation 25% |
| Vascular Injury | <6 hours | Revascularization | 90% | Limb loss 50% |
| Open Fracture | <6 hours | Debridement | 95% | Infection 3x |
| Cauda Equina | <24 hours | Decompression | 80% | Permanent deficit |
| Hip Fracture (elderly) | <24 hours | Surgical fixation | 85% | Mortality 2x |
Rapid Assessment Tools
Systematic examination sequences ensure comprehensive evaluation while maintaining efficiency during busy clinical situations.
-
5-Minute Orthopedic Screen
- Inspection (30 seconds): Deformity, swelling, wounds
- Palpation (60 seconds): Tenderness, pulses, temperature
- Movement (90 seconds): Active/passive ROM, strength
- Neurovascular (120 seconds): Sensation, motor, circulation
- Special tests (60 seconds): Stability, provocative maneuvers
- Document findings immediately
- Compare to contralateral side
- Photograph significant findings
-
Pain Assessment Integration
- 0-3: Minimal impact, conservative management appropriate
- 4-6: Moderate impact, consider intervention
- 7-10: Severe impact, urgent evaluation required
- Functional impact: Work, sleep, activities of daily living
- Use validated pain scales consistently
- Consider cultural and age factors
- Document response to interventions
Essential Number Arsenal
Critical quantitative thresholds that guide immediate clinical decisions and treatment modifications.
-
Fracture Healing Thresholds
- Displacement: >2 mm articular, >1 cm shaft shortening
- Angulation: >10° metaphyseal, >5° articular
- Rotation: >15° any location requires correction
- Union timeline: 6-8 weeks upper extremity, 12-16 weeks lower extremity
- Delayed union: 50% longer than expected
- Nonunion: No progression at 6 months
- Malunion: Healed in unacceptable position
-
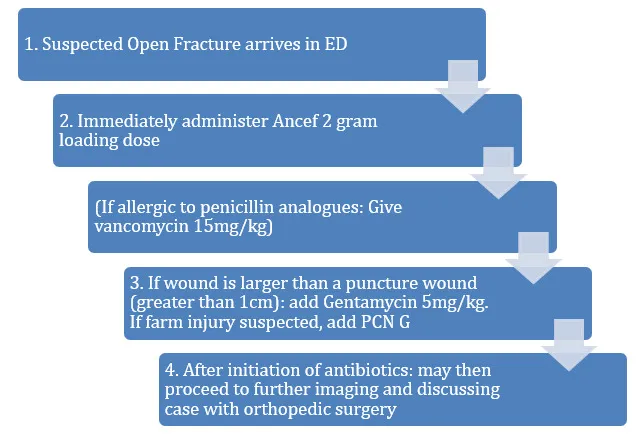
Antibiotic Prophylaxis Guidelines
- Cefazolin: 2 grams IV within 60 minutes of incision
- Duration: 24 hours for routine cases, 72 hours for trauma
- Redosing: Every 4 hours during long procedures
- Allergies: Clindamycin 900 mg or vancomycin 15 mg/kg
- MRSA risk: Add vancomycin 15 mg/kg
- Gram-negative coverage: Add gentamicin 5 mg/kg
- Open fractures: Extend to 72 hours minimum
⭐ Clinical Pearl: Rule of 2s for fracture acceptability - 2 mm articular displacement, 2 weeks for swelling resolution, 2 cm shortening tolerance in femur, 20° angulation in metaphysis
Rapid Reference Protocols
Standardized protocols ensure consistent care delivery and prevent critical omissions during high-stress situations.
-
Open Fracture Management Checklist
- Immediate: Photograph wound, sterile dressing, splint, tetanus
- <1 hour: IV antibiotics, pain control, NPO status
- <6 hours: Surgical debridement, irrigation, stabilization
- 24-48 hours: Second-look surgery if indicated
- Irrigation volume: >9 liters for Grade III
- Antibiotic duration: 72 hours minimum
- Soft tissue coverage: <7 days for Grade IIIB
-
Compartment Syndrome Protocol
- Clinical suspicion: Pain out of proportion, passive stretch pain
- Pressure measurement: >30 mmHg or <30 mmHg from diastolic
- Surgical intervention: 4-compartment fasciotomy
- Post-operative: Delayed closure at 48-72 hours
- Incision placement: Lateral and medial approaches
- Complete release: All compartments must be opened
- Wound care: Negative pressure therapy if available
💡 Master This: FAST decision-making - Focus on life/limb threats first, Assess systematically, Standardize protocols, Time-sensitive interventions prioritized; reduces errors by 40-60% in emergency situations
These rapid-access tools enable confident decision-making during critical situations while maintaining systematic approaches that optimize patient outcomes and minimize complications.
🎯 The Clinical Mastery Arsenal: Rapid Decision Tools
Practice Questions: Orthopedic Surgery Basics
Test your understanding with these related questions
A 36-year-old male is taken to the emergency room after jumping from a building. Bilateral fractures to the femur were stabilized at the scene by emergency medical technicians. The patient is lucid upon questioning and his vitals are stable. Pain only at his hips was elicited. Cervical exam was not performed. What is the best imaging study for this patient?














