Tumor staging and TNM classification US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Tumor staging and TNM classification. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Tumor staging and TNM classification US Medical PG Question 1: An excisional biopsy is performed and the diagnosis of superficial spreading melanoma is confirmed. The lesion is 1.1 mm thick. Which of the following is the most appropriate next step in management?
- A. Surgical excision with 0.5-1 cm safety margins only
- B. Surgical excision with 1 cm safety margins only
- C. Surgical excision with 1-2 cm safety margins only
- D. Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study
- E. Surgical excision with 1-2 cm safety margins and sentinel lymph node study (Correct Answer)
Tumor staging and TNM classification Explanation: ***Surgical excision with 1-2 cm safety margins and sentinel lymph node study***
- A melanoma with a **Breslow thickness between 1.01 mm and 2.0 mm** (like this 1.1 mm lesion) requires a recommended surgical margin of **1 to 2 cm**.
- For melanomas **≥0.8 mm thickness** (or those with ulceration), a **sentinel lymph node biopsy (SLNB)** is recommended to assess for micrometastasis, as it helps in staging and prognosis.
*Surgical excision with 0.5-1 cm safety margins only*
- A 0.5 cm margin is typically reserved for melanoma *in situ* or extremely thin melanomas (less than or equal to 0.5 mm), and 1 cm for lesions 0.51 to 1.0 mm, which is too narrow for a 1.1 mm lesion.
- This option incorrectly omits the **sentinel lymph node study**, which is indicated for a melanoma of this thickness.
*Surgical excision with 1 cm safety margins only*
- While 1 cm is a common margin for lesions up to 1.0 mm, a 1.1 mm melanoma usually warrants a slightly wider margin, ideally 1-2 cm.
- This option also fails to include the **sentinel lymph node study**, which is crucial for staging melanomas ≥0.8 mm thickness.
*Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study*
- The recommended surgical margin for a 1.1 mm melanoma is at least **1 cm, preferably between 1 and 2 cm**, making a 0.5-1 cm range insufficient.
- Although it correctly includes the sentinel lymph node study, the **surgical margin is inadequate** for the given Breslow thickness.
*Surgical excision with 1-2 cm safety margins only*
- While the **1-2 cm surgical margin** is appropriate for a 1.1 mm melanoma, this option **incorrectly excludes the sentinel lymph node study**.
- The sentinel lymph node biopsy is a critical part of the staging and management plan for melanomas of this thickness to detect potential nodal involvement.
Tumor staging and TNM classification US Medical PG Question 2: A 58-year-old man presents with lower back pain that started a couple of weeks ago and is gradually increasing in severity. At present, he rates the intensity of the pain as 6/10. There is no radiation or associated paresthesias. There is no history of trauma. Past medical history is significant for aggressive squamous cell carcinoma of the right lung status post surgical resection followed by adjunct chemotherapy and radiation therapy that was completed 6 months ago. A technetium bone scan reveals metastatic lesions in the lumbar vertebrae at levels L2–L4. The physician explains to the patient that these are likely metastatic lesions from his primary lung cancer. Which of the following best describes the mechanism that most likely led to the development of these metastatic lesions?
- A. Transcoelomic
- B. Lymphatic spread
- C. Collagenase produced by cancer cells dissolves the basement membrane and aids in cellular invasion
- D. Hematogenous spread (Correct Answer)
- E. PTH (parathormone)-related protein production by tumor cells
Tumor staging and TNM classification Explanation: ***Hematogenous spread***
- Lung cancer frequently metastasizes to bone via the **hematogenous (bloodstream) route**, especially to the spine, pelvis, and long bones.
- The rich vascular supply of the vertebrae makes them a common site for metastases from many primary cancers, including those of the lung.
*Transcoelomic*
- **Transcoelomic spread** occurs when tumor cells spread directly within body cavities, such as the peritoneal or pleural cavity.
- This mechanism is typical for cancers of organs within these cavities, like ovarian cancer spreading within the peritoneum, and is not the primary route for lung cancer to distant bone.
*Lymphatic spread*
- **Lymphatic spread** involves tumor cells traveling through the lymphatic system to regional lymph nodes.
- While lung cancer commonly spreads to mediastinal and hilar lymph nodes, it is usually not the direct mechanism for distant bone metastases, which typically involve the circulatory system.
*Collagenase produced by cancer cells dissolves the basement membrane and aids in cellular invasion*
- While **collagenase production** and **basement membrane degradation** are crucial steps in local tumor invasion and intravasation (entering blood or lymphatic vessels), they describe the *how* a cell invades, not the *route* of distant metastasis.
- This mechanism facilitates the initial escape of cancer cells from the primary tumor but does not define the subsequent spread to distant sites like bone.
*PTH (parathormone)-related protein production by tumor cells*
- **PTH-related protein (PTHrP) production** by tumor cells can lead to **hypercalcemia of malignancy** due to its osteolytic effects.
- While this is a common paraneoplastic syndrome associated with squamous cell carcinoma of the lung, it is a *consequence* or *effect* of the tumor and does not describe the *mechanism of metastasis* itself.
Tumor staging and TNM classification US Medical PG Question 3: A 52-year-old man with stage IV melanoma comes to the physician with his wife for a routine follow-up examination. He was recently diagnosed with new bone and brain metastases despite receiving aggressive chemotherapy but has not disclosed this to his wife. He has given verbal consent to discuss his prognosis with his wife and asks the doctor to inform her of his condition because he does not wish to do so himself. She is tearful and has many questions about his condition. Which of the following would be the most appropriate statement by the physician to begin the interview with the patient's wife?
- A. Have you discussed a living will or goals of care together?
- B. We should talk about how we can manage his symptoms with additional chemotherapy.
- C. Why do you think your husband has not discussed his medical condition with you?
- D. What is your understanding of your husband's current condition? (Correct Answer)
- E. Your husband has end-stage cancer, and his prognosis is poor.
Tumor staging and TNM classification Explanation: ***What is your understanding of your husband's current condition?***
- This statement initiates the conversation by **assessing the wife's current knowledge** and emotional state, which is crucial for delivering sensitive and appropriate information.
- It allows the physician to tailor the discussion to her specific understanding and concerns, ensuring that information is delivered compassionately and effectively.
*Have you discussed a living will or goals of care together?*
- This question is too abrupt and **premature** as an opening, as the wife is clearly distressed and unaware of the full severity of her husband's condition.
- Discussions about end-of-life planning should only occur after the patient's wife has a clear understanding of the diagnosis and prognosis, and has processed this information.
*Your husband has end-stage cancer, and his prognosis is poor.*
- While factual, this statement is **too blunt and lacks empathy** for an opening, especially given the wife's emotional state and lack of prior knowledge.
- Delivering such devastating news directly without first assessing her understanding or providing context can be traumatic and impede effective communication.
*We should talk about how we can manage his symptoms with additional chemotherapy.*
- This statement implies a focus on further aggressive treatment which may not be appropriate given the **new bone and brain metastases** and aggressive prior chemotherapy, suggesting a limited benefit of more chemotherapy.
- It also **diverts from the primary need to discuss the overall prognosis** and the patient's rapidly declining condition, which the doctor has been asked to convey.
*Why do you think your husband has not discussed his medical condition with you?*
- This question is **accusatory** and places blame on either the patient or the wife, which is inappropriate and unhelpful in a sensitive medical discussion.
- It shifts the focus away from providing medical information and empathy towards a speculative and potentially confrontational topic.
Tumor staging and TNM classification US Medical PG Question 4: A 70-year-old man comes to the physician because of right-sided back pain, red urine, and weight loss for the last 4 months. He has smoked one pack of cigarettes daily for 40 years. A CT scan of the abdomen shows a large right-sided renal mass. Biopsy of the mass shows polygonal clear cells filled with lipids. Which of the following features is necessary to determine the tumor grade in this patient?
- A. Invasion of surrounding structures
- B. Response to chemotherapy
- C. Nuclear pleomorphism and nucleolar prominence (Correct Answer)
- D. Involvement of regional lymph nodes
- E. Size of malignant proliferation
Tumor staging and TNM classification Explanation: ***Nuclear pleomorphism and nucleolar prominence***
- The **Fuhrman nuclear grading system** (and newer WHO/ISUP grading system) for renal cell carcinoma is based on **nuclear morphologic features**: nuclear size, nuclear contour irregularity, and most importantly, **nucleolar prominence**.
- **Grade 1**: Small uniform nuclei with inconspicuous nucleoli
- **Grade 2**: Slightly irregular nuclei with small nucleoli visible at 400× magnification
- **Grade 3**: Moderately irregular nuclei with prominent nucleoli visible at 100× magnification
- **Grade 4**: Marked nuclear pleomorphism, multilobated nuclei, and prominent nucleoli
- Higher nuclear grades correlate with more aggressive tumor behavior and worse prognosis.
*Invasion of surrounding structures*
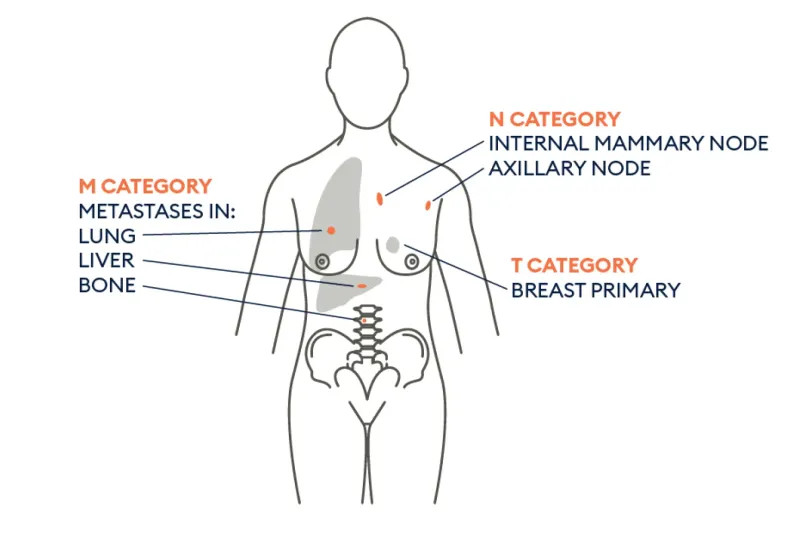
- This feature is crucial for **tumor staging (T stage)**, specifically T3 disease when perinephric fat, renal vein, or IVC is invaded, and T4 when beyond Gerota's fascia.
- **Invasion** determines surgical approach and prognosis related to local spread but does not define histological grade.
*Response to chemotherapy*
- **Response to chemotherapy** is evaluated after treatment and is not a feature used for grading at diagnosis.
- Clear cell RCC is **chemoresistant**; treatment typically involves targeted therapy (VEGF inhibitors, mTOR inhibitors) or immunotherapy, not traditional chemotherapy.
*Involvement of regional lymph nodes*
- **Lymph node involvement** is a component of **tumor staging (N stage)**: N0 (no nodes), N1 (regional nodes positive).
- It indicates metastatic spread and significantly worsens prognosis but does not contribute to **histological grade**, which assesses cellular differentiation.
*Size of malignant proliferation*
- **Tumor size** is the primary criterion for **T staging**: T1a (≤4 cm), T1b (>4-7 cm), T2a (>7-10 cm), T2b (>10 cm), all confined to kidney.
- Size is a prognostic factor but does not determine **histological grade**, which is based exclusively on nuclear microscopic features.
Tumor staging and TNM classification US Medical PG Question 5: Patient 1 – A 26-year-old woman presents to her primary care physician for an annual exam. She currently does not have any acute concerns and says her health has been generally well. Medical history is significant for asthma, which is managed with an albuterol inhaler. Her last pap smear was unremarkable. She is currently sexually active with one male and consistently uses condoms. She occasionally smokes marijuana and drinks wine once per week. Her mother recently passed away from advanced ovarian cancer. Her sister is 37-years-old and was recently diagnosed with breast cancer and ovarian cancer. Physical examination is remarkable for a mildly anxious woman.
Patient 2 – A 27-year-old woman presents to her primary care physician for an annual exam. She says that she would like to be screened for breast cancer since two of her close friends were recently diagnosed. She noticed she has a small and mobile mass on her left breast, which increases in size and becomes tender around her time of menses. Family history is remarkable for hypertension in the father. The physical exam is significant for a small, well-defined, and mobile mass on her left breast that is not tender to palpation.
Which of the following is the best next step in management for patient 1 and 2?
- A. Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam
- B. Patient 1 – Reassurance. Patient 2 – Breast ultrasound
- C. Patient 1 – CA-125 testing. Patient 2 – BRCA testing
- D. Patient 1 – BRCA testing. Patient 2 – Breast ultrasound (Correct Answer)
- E. Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography
Tumor staging and TNM classification Explanation: ***Patient 1 – BRCA testing. Patient 2 – Breast ultrasound***
- Patient 1 has a strong family history of early-onset **breast and ovarian cancer** (**mother and sister**), suggesting a high probability of an inherited genetic mutation, such as **BRCA1/2**, which warrants genetic testing.
- Patient 2 presents with a **small, mobile, well-defined breast mass** that is likely benign, and a **breast ultrasound** is the appropriate initial imaging for further characterization in a young woman.
*Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam*
- Patient 1's primary concern is genetic predisposition due to family history, an **ultrasound** is not the initial or primary screening method for future cancer risk.
- Patient 2 has a palpable mass; waiting 3 months for a **clinical breast exam** without initial imaging (ultrasound) is not appropriate for evaluating a new breast lump.
*Patient 1 – Reassurance. Patient 2 – Breast ultrasound*
- Patient 1's family history of **early-onset breast and ovarian cancer** is a significant risk factor; therefore, simple **reassurance** without further investigation is inappropriate.
- While a **breast ultrasound** is appropriate for Patient 2, the recommendation for Patient 1 is incorrect.
*Patient 1 – CA-125 testing. Patient 2 – BRCA testing*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer treatment or recurrence, not for initial screening in asymptomatic individuals, especially in a young woman with no active symptoms.
- **BRCA testing** is indicated for Patient 1 due to family history, but not for Patient 2 who has a likely benign breast mass and no significant family history.
*Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography*
- Regular **breast and ovarian ultrasounds** are not recommended as primary screening tools for genetic risk in asymptomatic high-risk individuals like Patient 1.
- **Mammography** is less sensitive in young women (under 30) due to higher breast tissue density, making **ultrasound** the preferred initial imaging for Patient 2.
Tumor staging and TNM classification US Medical PG Question 6: A 65-year-old man with a 40-pack-year smoking history presents with hemoptysis and a persistent cough. Chest CT shows a 3.5 cm centrally located mass in the right main bronchus. Positron emission tomography confirms a malignant nodule. Bronchoscopy with transbronchial biopsy is performed and a specimen sample of the nodule is sent for frozen section analysis. The tissue sample is most likely to show which of the following tumor types?
- A. Carcinoid tumor
- B. Metastasis of colorectal cancer
- C. Small cell lung carcinoma
- D. Large cell carcinoma
- E. Squamous cell carcinoma (Correct Answer)
Tumor staging and TNM classification Explanation: ***Squamous cell carcinoma***
- This is the most likely diagnosis given the **central location** in the main bronchus, **heavy smoking history**, and presentation with **hemoptysis**.
- **Squamous cell carcinoma** accounts for 25-30% of lung cancers and characteristically arises in **central/proximal airways**, making it readily accessible by **bronchoscopy**.
- Histologically, it shows **keratin pearls** and **intercellular bridges** on biopsy.
- The **central endobronchial location** and ability to obtain tissue via transbronchial biopsy strongly favor squamous cell over peripheral tumors.
*Carcinoid tumor*
- **Carcinoid tumors** are **neuroendocrine tumors** that can present as central endobronchial masses and cause hemoptysis.
- However, they are typically **slow-growing** with more indolent presentation, and PET scans show **variable uptake** (often less intense than aggressive carcinomas).
- They represent only **1-2% of lung tumors** and occur more commonly in **younger, non-smoking patients**.
*Metastasis of colorectal cancer*
- While lung is a common site for **colorectal metastases**, these typically present as **multiple peripheral nodules** rather than a solitary central endobronchial mass.
- The clinical presentation strongly suggests **primary lung cancer** rather than metastatic disease.
- Without history of colorectal cancer, this is unlikely.
*Small cell lung carcinoma*
- **Small cell lung carcinoma** (SCLC) represents 15% of lung cancers and typically presents as a **large central mass** with early mediastinal involvement.
- However, SCLC is usually **too extensive at presentation** for transbronchial biopsy alone and often requires mediastinoscopy or CT-guided biopsy.
- Histology shows **small cells with scant cytoplasm**, **salt-and-pepper chromatin**, and **oat-cell morphology**.
- While possible, the single accessible endobronchial mass is more characteristic of squamous cell.
*Large cell carcinoma*
- **Large cell carcinoma** is a **diagnosis of exclusion** made when tumors lack features of adenocarcinoma, squamous cell, or small cell differentiation.
- It typically presents as **large peripheral masses** rather than central endobronchial lesions.
- It represents only **10% of lung cancers** and is less common than squamous cell carcinoma in this clinical scenario.
Tumor staging and TNM classification US Medical PG Question 7: A 56-year-old woman comes to the physician because she palpated a mass in her right breast during self-examination a week ago. Menarche was at the age of 14, and her last menstrual period was at the age of 51. Vital signs are within normal limits. Examination shows a nontender, firm and hard mass in the upper outer quadrant of the right breast. Mammography shows large, dense breasts, with a 1.7-cm mass in the right upper outer quadrant. The patient undergoes right upper outer quadrant lumpectomy with subsequent sentinel node biopsy, which reveals moderately differentiated invasive ductal carcinoma and micrometastasis to one axillary lymph node. There is no evidence of extranodal metastasis. The tumor tests positive for both estrogen and progesterone receptors and does not show human epidermal growth factor receptor 2 (HER2) over-expression. Flow-cytometry reveals aneuploid tumor cells. Which of the following factors has the greatest effect on this patient's prognosis?
- A. Age
- B. Tumor size
- C. Hormone receptor status
- D. Nodal status (Correct Answer)
- E. HER2 receptor status
Tumor staging and TNM classification Explanation: **Nodal status**
- The presence of **micrometastasis to one axillary lymph node** is the *most significant prognostic indicator* in this patient's case.
- **Lymph node involvement** signifies systemic spread and is the strongest predictor of recurrence and overall survival in breast cancer.
*Age*
- While **age** can influence treatment choices and comorbidity, it is generally *less impactful on long-term prognosis* than nodal status.
- Very young or very old age can sometimes be associated with more aggressive disease or worse outcomes, but it is not the primary determinant.
*Tumor size*
- The **tumor size of 1.7 cm** is a prognostic factor, with larger tumors generally having a worse prognosis.
- However, for this patient, the **presence of lymph node metastasis** is a more powerful indicator of systemic disease than the primary tumor size alone.
*Hormone receptor status*
- **Positive estrogen and progesterone receptors** indicate that the tumor is likely to respond to endocrine therapies.
- This is a *favorable prognostic factor* as it opens up additional treatment options, but it does not outweigh the negative impact of nodal involvement.
*HER2 receptor status*
- **Absence of HER2 overexpression** is a positive factor, as HER2-positive cancers are generally more aggressive and require targeted therapy.
- However, while HER2 status guides treatment, the presence of **lymph node metastasis** still holds greater weight in determining overall prognosis.
Tumor staging and TNM classification US Medical PG Question 8: A 57-year-old man presents to his oncologist to discuss management of small cell lung cancer. The patient is a lifelong smoker and was diagnosed with cancer 1 week ago. The patient states that the cancer was his fault for smoking and that there is "no hope now." He seems disinterested in discussing the treatment options and making a plan for treatment and followup. The patient says "he does not want any treatment" for his condition. Which of the following is the most appropriate response from the physician?
- A. "You seem upset at the news of this diagnosis. I want you to go home and discuss this with your loved ones and come back when you feel ready to make a plan together for your care."
- B. "It must be tough having received this diagnosis; however, new cancer therapies show increased efficacy and excellent outcomes."
- C. "It must be very challenging having received this diagnosis. I want to work with you to create a plan." (Correct Answer)
- D. "We are going to need to treat your lung cancer. I am here to help you throughout the process."
- E. "I respect your decision and we will not administer any treatment. Let me know if I can help in any way."
Tumor staging and TNM classification Explanation: ***"It must be very challenging having received this diagnosis. I want to work with you to create a plan."***
- This response **acknowledges the patient's emotional distress** and feelings of guilt and hopelessness, which is crucial for building rapport and trust.
- It also gently **re-engages the patient** by offering a collaborative approach to treatment, demonstrating the physician's commitment to supporting him through the process.
*"You seem upset at the news of this diagnosis. I want you to go home and discuss this with your loved ones and come back when you feel ready to make a plan together for your care."*
- While acknowledging distress, sending the patient home without further engagement **delays urgent care** for small cell lung cancer, which is aggressive.
- This response might be perceived as dismissive of his immediate feelings and can **exacerbate his sense of hopelessness** and isolation.
*"It must be tough having received this diagnosis; however, new cancer therapies show increased efficacy and excellent outcomes."*
- This statement moves too quickly to treatment efficacy without adequately addressing the patient's current **emotional state and fatalism**.
- While factual, it **lacks empathy** for his personal feelings of blame and hopelessness, potentially making him feel unheard.
*"We are going to need to treat your lung cancer. I am here to help you throughout the process."*
- This response is **too directive and authoritarian**, which can alienate a patient who is already feeling guilty and resistant to treatment.
- It fails to acknowledge his stated feelings of "no hope now" or his disinterest in treatment, which are critical to address before discussing the necessity of treatment.
*"I respect your decision and we will not administer any treatment. Let me know if I can help in any way."*
- While respecting patient autonomy is vital, immediately accepting a patient's decision to refuse treatment without exploring the underlying reasons (e.g., guilt, hopelessness, lack of information) is **premature and potentially harmful**.
- The physician has a responsibility to ensure the patient is making an informed decision, especially for a rapidly progressing condition like small cell lung cancer.
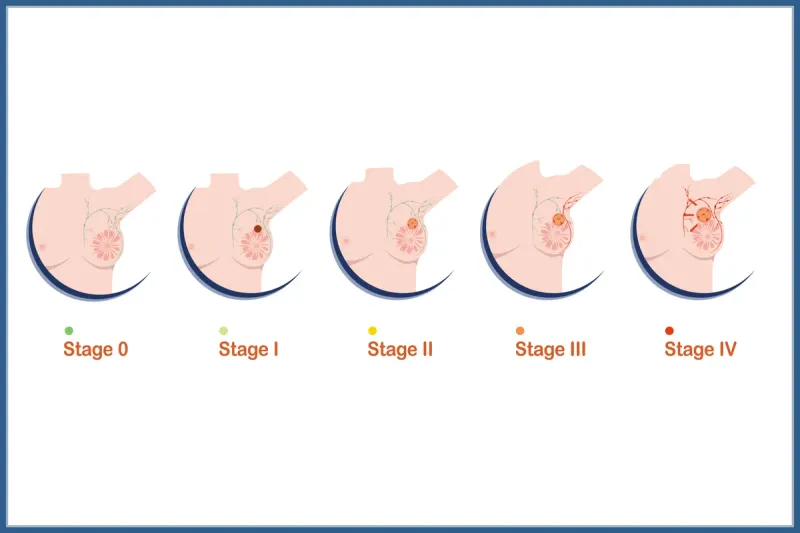
Tumor staging and TNM classification US Medical PG Question 9: A 39-year-old African American woman is admitted to the hospital following a seizure with a severe post-ictal headache. She was diagnosed with breast cancer 1 year ago when she presented with a hard, rock-like, immobile mass with irregular borders accompanied by changes in the breast skin, including erythema and dimpling. She had ipsilateral mobile axillary lymphadenopathy at that time. A biopsy confirmed the diagnosis of stage 2B invasive breast cancer. Her mother died at 42 years of age due to the same type of breast cancer. A CT scan done during this admission reveals multiple metastatic lesions in the brain and liver, along with the involvement of supra- and infra-clavicular lymph nodes. Which of the following molecular profile most likely characterizes this patient?
- A. PR, ER, HER2 positive
- B. HER2 positive
- C. Progesterone receptor (PR) positive
- D. ER, PR, HER2 negative (Correct Answer)
- E. Estrogen receptor (ER) positive
Tumor staging and TNM classification Explanation: ***ER, PR, HER2 negative***
- This patient's presentation with aggressive breast cancer at a relatively young age (39 years old), family history of early-onset breast cancer, rapid progression to metastatic disease in the brain and liver, and involvement of multiple lymph nodes (axillary, supra- and infra-clavicular) are all highly suggestive of a **triple-negative breast cancer (TNBC)**.
- TNBC is characterized by the absence of **estrogen receptors (ER)**, **progesterone receptors (PR)**, and **human epidermal growth factor receptor 2 (HER2)** overexpression, making it an aggressive subtype with limited targeted treatment options and a poor prognosis, consistent with the patient's rapidly worsening condition.
*PR, ER, HER2 positive*
- This molecular profile (also known as triple-positive breast cancer) generally indicates a more favorable prognosis due to the availability of **hormonal therapy** (for ER/PR positivity) and **anti-HER2 targeted therapy**.
- The aggressive course and rapid metastatic spread described in the patient are less typical for triple-positive disease, which often responds well to various targeted treatments.
*HER2 positive*
- HER2-positive breast cancer can be aggressive, but the presence of HER2 positivity allows for **HER2-targeted therapies** (e.g., trastuzumab, pertuzumab), which significantly improve outcomes.
- While HER2-positive cancers can metastasize to the brain, the overall clinical picture, especially the aggressive growth and lack of other receptor expression, aligns more with triple-negative disease.
*Progesterone receptor (PR) positive*
- PR positivity, often alongside ER positivity, indicates a **hormone-sensitive breast cancer**, which typically has a better prognosis and is amenable to **endocrine therapy**.
- The aggressive and rapid metastatic progression to multiple sites, including brain and liver, is not characteristic of a purely PR-positive tumor without other aggressive features.
*Estrogen receptor (ER) positive*
- ER-positive breast cancer is the most common subtype and is generally associated with a **better prognosis** and responsiveness to **endocrine therapy**.
- The patient's aggressive disease course, including early metastasis and family history of early-onset, aggressive breast cancer, does not align with the typical presentation of an exclusively ER-positive tumor.
Tumor staging and TNM classification US Medical PG Question 10: An 84-year-old woman is brought to the physician by her son after he found her trying to hang herself from the ceiling because she felt that she was a burden to her family. Her family says that for the past 2 months she has had no energy to leave her room, has been sleeping most of the day, has lost 10 kg (22 lb), and cries every day. She was diagnosed with breast cancer that has metastasized to the liver 4 months ago. She moved in with her son and daughter-in-law shortly after the diagnosis. She initially underwent chemotherapy but discontinued the treatment when the metastases spread to the spine and brain. Her life expectancy is 1–2 weeks and she is currently receiving home-hospice care. Her only current medication is a fentanyl patch. She is 160 cm (5 ft 3 in) tall and weighs 46 kg (101.4 lb); BMI is 18 kg/m2. Her vital signs are within normal limits. Examination shows slow speech, a flat affect, and depressed mood. Which of the following treatments is initially most likely to provide the greatest benefit for this patient?
- A. Electroconvulsive therapy
- B. Methylphenidate (Correct Answer)
- C. Megestrol
- D. Fluoxetine
- E. Bupropion
Tumor staging and TNM classification Explanation: ***Methylphenidate***
- This patient presents with **severe depression** at the end of life with a very limited prognosis (1-2 weeks), making quick symptom relief paramount. **Psychostimulants** like methylphenidate can offer a rapid antidepressant effect (within days) and improve energy and appetite.
- Given her **advanced cancer**, **poor prognosis**, and **suicidal ideation**, a fast-acting treatment that improves quality of life quickly is crucial.
*Electroconvulsive therapy*
- While highly effective for severe depression, **ECT** requires multiple sessions and is a more invasive treatment not typically chosen for immediate symptom relief in a patient with a life expectancy of 1-2 weeks.
- The patient's **metastatic cancer** and overall frail condition would make the associated risks (e.g., anesthesia) disproportionate to the limited time frame for benefit.
*Megestrol*
- **Megestrol acetate** is a progestin sometimes used as an appetite stimulant in patients with cachexia, particularly in cancer or AIDS.
- It would not address the patient's **depressive symptoms** or **suicidal ideation**, which are the primary concerns requiring urgent intervention.
*Fluoxetine*
- **Fluoxetine**, a selective serotonin reuptake inhibitor (SSRI), is a common antidepressant but typically takes **4-6 weeks** to achieve its full therapeutic effect.
- Given the patient's life expectancy of 1-2 weeks and her severe suicidal ideation, a delayed-onset medication like fluoxetine would not be appropriate for immediate symptom management.
*Bupropion*
- **Bupropion** is an antidepressant that also takes several weeks to exert its full effect.
- Like other typical antidepressants, its **delayed onset of action** makes it unsuitable for a patient with such a limited prognosis needing rapid symptom relief for severe depression and suicidality.
More Tumor staging and TNM classification US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.