Tumor biology and surgical planning US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Tumor biology and surgical planning. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Tumor biology and surgical planning US Medical PG Question 1: A 33-year-old woman comes to the physician 1 week after noticing a lump in her right breast. Fifteen years ago, she was diagnosed with osteosarcoma of her left distal femur. Her father died of an adrenocortical carcinoma at the age of 41 years. Examination shows a 2-cm, firm, immobile mass in the lower outer quadrant of the right breast. A core needle biopsy of the mass shows adenocarcinoma. Genetic analysis in this patient is most likely to show a defect in which of the following genes?
- A. BRCA1
- B. KRAS
- C. TP53 (Correct Answer)
- D. Rb
- E. PTEN
Tumor biology and surgical planning Explanation: ***TP53***
- This patient's presentation with **early-onset breast cancer**, a history of **osteosarcoma** at a young age, and a father's death from **adrenocortical carcinoma** at 41 years strongly suggests **Li-Fraumeni syndrome**.
- Li-Fraumeni syndrome is an autosomal dominant disorder caused by a germline mutation in the **tumor suppressor gene TP53**, increasing the risk for multiple primary cancers at a young age.
*BRCA1*
- While **BRCA1 mutations** are associated with an increased risk of breast and ovarian cancer, they are not typically linked to osteosarcoma or adrenocortical carcinoma.
- The constellation of cancers in this patient is more indicative of Li-Fraumeni syndrome than solely a BRCA1-related cancer syndrome.
*KRAS*
- **KRAS** is an oncogene commonly mutated in several cancers, including pancreatic, colorectal, and lung cancer, but is not primarily associated with either Li-Fraumeni syndrome or the specific tumors seen in this family history.
- Mutations in KRAS are typically somatic mutations acquired during a person's lifetime, not germline mutations causing inherited cancer syndromes like the one suggested here.
*Rb*
- Mutations in the **retinoblastoma (Rb) gene** are associated with retinoblastoma and an increased risk of osteosarcoma, but not typically with adrenocortical carcinoma or breast cancer as part of a classic inherited syndrome.
- The combination of breast cancer, osteosarcoma, and adrenocortical carcinoma points more specifically to TP53.
*PTEN*
- **PTEN mutations** are associated with Cowden syndrome, which increases the risk for breast cancer, thyroid cancer, and endometrial cancer, along with benign growths.
- However, Cowden syndrome does not typically include osteosarcoma or adrenocortical carcinoma as prominent features, making PTEN less likely than TP53 for this specific family history.
Tumor biology and surgical planning US Medical PG Question 2: Researchers are investigating oncogenes, specifically the KRAS gene that is associated with colon, lung, and pancreatic cancer. They have established that the gain-of-function mutation in this gene increases the chance of cancer development. They are also working to advance the research further to study tumor suppressor genes. Which of the genes below is considered a tumor suppressor gene?
- A. Her2/neu
- B. BRAF
- C. BCL-2
- D. JAK2
- E. Rb (Correct Answer)
Tumor biology and surgical planning Explanation: ***Rb***
- The **retinoblastoma (Rb)** gene is a classic example of a **tumor suppressor gene**. Its protein product, Rb, plays a critical role in regulating the **cell cycle** by preventing uncontrolled cell division.
- When **Rb is mutated or inactivated**, cells can divide without proper checks, leading to tumor formation, particularly in cases like retinoblastoma.
*Her2/neu*
- **Her2/neu** (also known as ERBB2) is an **oncogene** that encodes a receptor tyrosine kinase involved in cell growth and differentiation.
- Its overexpression or amplification is associated with certain cancers, notably **breast cancer**, but it is not a tumor suppressor.
*BRAF*
- **BRAF** is an **oncogene** that codes for a serine/threonine kinase involved in the RAS/MAPK signaling pathway, which regulates cell growth.
- **Gain-of-function mutations** in BRAF are frequently found in melanoma, thyroid cancer, and colorectal cancer, promoting uncontrolled cell proliferation.
*BCL-2*
- **BCL-2** is an **anti-apoptotic gene**, meaning it prevents programmed cell death. While its overexpression can contribute to cancer by allowing abnormal cells to survive, it is not classified as a tumor suppressor gene.
- Instead, BCL-2 is considered an **oncogene** because mutations or overexpression promote cell survival and inhibit apoptosis.
*JAK2*
- **JAK2** (Janus Kinase 2) is a **proto-oncogene** encoding a tyrosine kinase involved in cytokine receptor signaling, which regulates hematopoiesis.
- **Gain-of-function mutations**, such as JAK2 V617F, are frequently found in **myeloproliferative neoplasms** (e.g., polycythemia vera, essential thrombocythemia, myelofibrosis), leading to uncontrolled blood cell production.
Tumor biology and surgical planning US Medical PG Question 3: A 64-year-old woman presents to the surgical oncology clinic as a new patient for evaluation of recently diagnosed breast cancer. She has a medical history of type 2 diabetes mellitus for which she takes metformin. Her surgical history is a total knee arthroplasty 7 years ago. Her family history is insignificant. Physical examination is notable for an irregular nodule near the surface of her right breast. Her primary concern today is which surgical approach will be chosen to remove her breast cancer. Which of the following procedures involves the removal of a portion of a breast?
- A. Arthroplasty
- B. Lumpectomy (Correct Answer)
- C. Vasectomy
- D. Mastectomy
- E. Laminectomy
Tumor biology and surgical planning Explanation: ***Lumpectomy***
- A **lumpectomy** is a surgical procedure that removes the **breast cancer tumor** and a small margin of surrounding healthy tissue, preserving most of the breast.
- This procedure is a common treatment for early-stage breast cancer and is often followed by radiation therapy.
*Arthroplasty*
- **Arthroplasty** is a surgical procedure to **repair or replace a joint**, typically due to arthritis or injury.
- The patient's history of a total knee arthroplasty indicates this procedure was performed on her knee, not her breast.
*Vasectomy*
- A **vasectomy** is a surgical procedure for **male sterilization**, involving the cutting and sealing of the vas deferens.
- This procedure is unrelated to breast cancer treatment or breast surgery.
*Mastectomy*
- A **mastectomy** involves the **complete surgical removal of the entire breast**, often including the nipple and areola.
- While it is a breast surgery, it removes the *entire* breast, not just a portion.
*Laminectomy*
- A **laminectomy** is a surgical procedure that removes a portion of the **vertebra (lamina)** to relieve pressure on the spinal cord or nerves.
- This procedure is for spinal conditions and is entirely unrelated to breast cancer surgery.
Tumor biology and surgical planning US Medical PG Question 4: A research team develops a new monoclonal antibody checkpoint inhibitor for advanced melanoma that has shown promise in animal studies as well as high efficacy and low toxicity in early phase human clinical trials. The research team would now like to compare this drug to existing standard of care immunotherapy for advanced melanoma. The research team decides to conduct a non-randomized study where the novel drug will be offered to patients who are deemed to be at risk for toxicity with the current standard of care immunotherapy, while patients without such risk factors will receive the standard treatment. Which of the following best describes the level of evidence that this study can offer?
- A. Level 1
- B. Level 3 (Correct Answer)
- C. Level 5
- D. Level 4
- E. Level 2
Tumor biology and surgical planning Explanation: ***Level 3***
- A **non-randomized controlled trial** like the one described, where patient assignment to treatment groups is based on specific characteristics (risk of toxicity), falls into Level 3 evidence.
- This level typically includes **non-randomized controlled trials** and **well-designed cohort studies** with comparison groups, which are prone to selection bias and confounding.
- The study compares two treatments but lacks randomization, making it Level 3 evidence.
*Level 1*
- Level 1 evidence is the **highest level of evidence**, derived from **systematic reviews and meta-analyses** of multiple well-designed randomized controlled trials or large, high-quality randomized controlled trials.
- The described study is explicitly stated as non-randomized, ruling out Level 1.
*Level 2*
- Level 2 evidence involves at least one **well-designed randomized controlled trial** (RCT) or **systematic reviews** of randomized trials.
- The current study is *non-randomized*, which means it cannot be classified as Level 2 evidence, as randomization is a key criterion for this level.
*Level 4*
- Level 4 evidence includes **case series**, **case-control studies**, and **poorly designed cohort or case-control studies**.
- While the study is non-randomized, it is a controlled comparative trial rather than a case series or retrospective case-control study, placing it at Level 3.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, typically consisting of **expert opinion** without explicit critical appraisal, or based on physiology, bench research, or animal studies.
- While the drug was initially tested in animal studies, the current human comparative study offers a higher level of evidence than expert opinion or preclinical data.
Tumor biology and surgical planning US Medical PG Question 5: A 58-year-old man presents with lower back pain that started a couple of weeks ago and is gradually increasing in severity. At present, he rates the intensity of the pain as 6/10. There is no radiation or associated paresthesias. There is no history of trauma. Past medical history is significant for aggressive squamous cell carcinoma of the right lung status post surgical resection followed by adjunct chemotherapy and radiation therapy that was completed 6 months ago. A technetium bone scan reveals metastatic lesions in the lumbar vertebrae at levels L2–L4. The physician explains to the patient that these are likely metastatic lesions from his primary lung cancer. Which of the following best describes the mechanism that most likely led to the development of these metastatic lesions?
- A. Transcoelomic
- B. Lymphatic spread
- C. Collagenase produced by cancer cells dissolves the basement membrane and aids in cellular invasion
- D. Hematogenous spread (Correct Answer)
- E. PTH (parathormone)-related protein production by tumor cells
Tumor biology and surgical planning Explanation: ***Hematogenous spread***
- Lung cancer frequently metastasizes to bone via the **hematogenous (bloodstream) route**, especially to the spine, pelvis, and long bones.
- The rich vascular supply of the vertebrae makes them a common site for metastases from many primary cancers, including those of the lung.
*Transcoelomic*
- **Transcoelomic spread** occurs when tumor cells spread directly within body cavities, such as the peritoneal or pleural cavity.
- This mechanism is typical for cancers of organs within these cavities, like ovarian cancer spreading within the peritoneum, and is not the primary route for lung cancer to distant bone.
*Lymphatic spread*
- **Lymphatic spread** involves tumor cells traveling through the lymphatic system to regional lymph nodes.
- While lung cancer commonly spreads to mediastinal and hilar lymph nodes, it is usually not the direct mechanism for distant bone metastases, which typically involve the circulatory system.
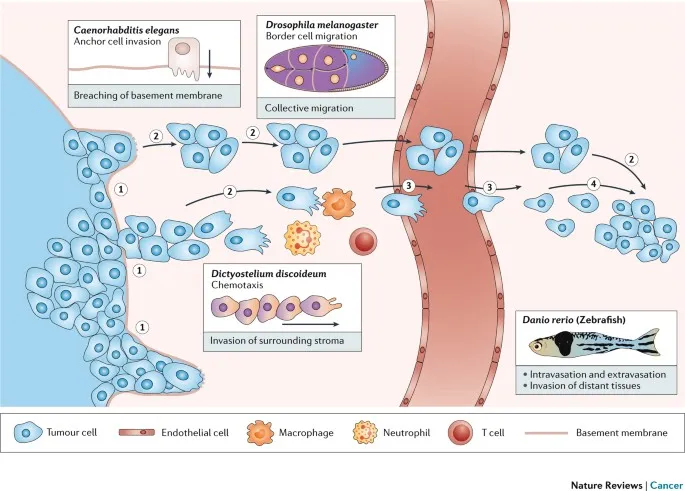
*Collagenase produced by cancer cells dissolves the basement membrane and aids in cellular invasion*
- While **collagenase production** and **basement membrane degradation** are crucial steps in local tumor invasion and intravasation (entering blood or lymphatic vessels), they describe the *how* a cell invades, not the *route* of distant metastasis.
- This mechanism facilitates the initial escape of cancer cells from the primary tumor but does not define the subsequent spread to distant sites like bone.
*PTH (parathormone)-related protein production by tumor cells*
- **PTH-related protein (PTHrP) production** by tumor cells can lead to **hypercalcemia of malignancy** due to its osteolytic effects.
- While this is a common paraneoplastic syndrome associated with squamous cell carcinoma of the lung, it is a *consequence* or *effect* of the tumor and does not describe the *mechanism of metastasis* itself.
Tumor biology and surgical planning US Medical PG Question 6: Patient 1 – A 26-year-old woman presents to her primary care physician for an annual exam. She currently does not have any acute concerns and says her health has been generally well. Medical history is significant for asthma, which is managed with an albuterol inhaler. Her last pap smear was unremarkable. She is currently sexually active with one male and consistently uses condoms. She occasionally smokes marijuana and drinks wine once per week. Her mother recently passed away from advanced ovarian cancer. Her sister is 37-years-old and was recently diagnosed with breast cancer and ovarian cancer. Physical examination is remarkable for a mildly anxious woman.
Patient 2 – A 27-year-old woman presents to her primary care physician for an annual exam. She says that she would like to be screened for breast cancer since two of her close friends were recently diagnosed. She noticed she has a small and mobile mass on her left breast, which increases in size and becomes tender around her time of menses. Family history is remarkable for hypertension in the father. The physical exam is significant for a small, well-defined, and mobile mass on her left breast that is not tender to palpation.
Which of the following is the best next step in management for patient 1 and 2?
- A. Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam
- B. Patient 1 – Reassurance. Patient 2 – Breast ultrasound
- C. Patient 1 – CA-125 testing. Patient 2 – BRCA testing
- D. Patient 1 – BRCA testing. Patient 2 – Breast ultrasound (Correct Answer)
- E. Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography
Tumor biology and surgical planning Explanation: ***Patient 1 – BRCA testing. Patient 2 – Breast ultrasound***
- Patient 1 has a strong family history of early-onset **breast and ovarian cancer** (**mother and sister**), suggesting a high probability of an inherited genetic mutation, such as **BRCA1/2**, which warrants genetic testing.
- Patient 2 presents with a **small, mobile, well-defined breast mass** that is likely benign, and a **breast ultrasound** is the appropriate initial imaging for further characterization in a young woman.
*Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam*
- Patient 1's primary concern is genetic predisposition due to family history, an **ultrasound** is not the initial or primary screening method for future cancer risk.
- Patient 2 has a palpable mass; waiting 3 months for a **clinical breast exam** without initial imaging (ultrasound) is not appropriate for evaluating a new breast lump.
*Patient 1 – Reassurance. Patient 2 – Breast ultrasound*
- Patient 1's family history of **early-onset breast and ovarian cancer** is a significant risk factor; therefore, simple **reassurance** without further investigation is inappropriate.
- While a **breast ultrasound** is appropriate for Patient 2, the recommendation for Patient 1 is incorrect.
*Patient 1 – CA-125 testing. Patient 2 – BRCA testing*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer treatment or recurrence, not for initial screening in asymptomatic individuals, especially in a young woman with no active symptoms.
- **BRCA testing** is indicated for Patient 1 due to family history, but not for Patient 2 who has a likely benign breast mass and no significant family history.
*Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography*
- Regular **breast and ovarian ultrasounds** are not recommended as primary screening tools for genetic risk in asymptomatic high-risk individuals like Patient 1.
- **Mammography** is less sensitive in young women (under 30) due to higher breast tissue density, making **ultrasound** the preferred initial imaging for Patient 2.
Tumor biology and surgical planning US Medical PG Question 7: A 76-year-old woman comes to the physician for evaluation of a 3-month history of vulvar itching and pain. She was diagnosed with lichen sclerosus 4 years ago. She has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows a 2.5-cm nodular, ulcerative lesion on the vaginal introitus and left labia minora with surrounding erythema. Punch biopsy shows squamous cell carcinoma. A CT scan of the chest, abdomen, and pelvis shows enlarged lymph nodes concerning for metastatic disease. Which of the following lymph node regions is the most likely primary site of metastasis?
- A. Superficial inguinal (Correct Answer)
- B. Internal iliac
- C. External iliac
- D. Inferior mesenteric
- E. Para-aortic
Tumor biology and surgical planning Explanation: ***Superficial inguinal***
- The **vulva** drains primarily into the **superficial inguinal lymph nodes**, making them the most likely first site for metastatic spread from vulvar squamous cell carcinoma.
- The lesion's location on the **vaginal introitus** and **labia minora** directly correlates with this lymphatic drainage pathway.
*Internal iliac*
- **Internal iliac nodes** receive drainage mainly from deep pelvic structures like the cervix, upper vagina, and uterus, not directly from the vulva.
- Metastasis to these nodes usually occurs after involvement of more superficial nodes or in advanced disease with deeper invasion.
*External iliac*
- **External iliac nodes** generally drain the lower extremities and deeper pelvic structures (e.g., bladder, distal ureter), not the vulva as a primary site.
- Involvement here would typically indicate more advanced local spread or secondary metastasis from other pelvic nodes.
*Inferior mesenteric*
- **Inferior mesenteric nodes** drain the hindgut and its derivatives, including the distal colon and rectum, which are distant from the vulva.
- This region is not involved in the lymphatic drainage of the vulva.
*Para-aortic*
- **Para-aortic nodes** drain structures like the ovaries, fallopian tubes, and upper uterus; they are too superior for primary vulvar lymphatic drainage.
- Metastasis to these nodes from vulvar cancer would signify widespread, very advanced disease and not a primary site of spread.
Tumor biology and surgical planning US Medical PG Question 8: A 57-year-old man presents to the emergency department for weight loss and abdominal pain. The patient states that he has felt steadily more fatigued over the past month and has lost 22 pounds without effort. Today, he fainted prompting his presentation. The patient has no significant past medical history. He does have a 33 pack-year smoking history and drinks 4 to 5 alcoholic drinks per day. His temperature is 99.5°F (37.5°C), blood pressure is 100/58 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you see a patient who is very thin and appears to be pale. Stool fecal occult blood testing is positive. A CT scan of the abdomen is performed demonstrating a mass in the colon with multiple metastatic lesions scattered throughout the abdomen. The patient is informed of his diagnosis of metastatic colon cancer. When the patient conveys the information to his family he focuses his efforts on discussing the current literature in the field and the novel therapies that have been invented. He demonstrates his likely mortality outcome which he calculated using the results of a large multi-center study. Which of the following is this patient most likely demonstrating?
- A. Intellectualization (Correct Answer)
- B. Dissociation
- C. Rationalization
- D. Optimism
- E. Pessimism
Tumor biology and surgical planning Explanation: ***Intellectualization***
- This defense mechanism involves **focusing on the intellectual aspects** of a stressful situation, using logical reasoning and factual analysis to avoid experiencing distressing emotions.
- The patient demonstrates this by discussing **literature, novel therapies, and mortality statistics** regarding his metastatic colon cancer.
*Dissociation*
- **Dissociation** involves a mental process that causes a lack of connection in a person's thoughts, memory, and sense of identity.
- This patient is actively engaging with the information, not disconnecting from it.
*Rationalization*
- **Rationalization** is creating logical but false explanations for unacceptable thoughts, feelings, or behaviors to justify them.
- The patient is not trying to justify his actions or feelings, but rather to understand his disease intellectually.
*Optimism*
- **Optimism** is a disposition to look on the favorable side of events or conditions and to expect the most favorable outcome.
- While hope for novel therapies could be seen as optimistic, his detailed calculation of mortality outcomes is a realistic, rather than purely optimistic, approach.
*Pessimism*
- **Pessimism** is a tendency to see the worst aspect of things or believe that the worst will happen.
- The patient is engaging with the facts of his diagnosis, even calculating his mortality outcome, which is not necessarily a pessimistic but rather a realistic and intellectual approach.
Tumor biology and surgical planning US Medical PG Question 9: A 47-year-old woman comes to the physician for a mass in her left breast she noticed 2 days ago during breast self-examination. She has hypothyroidism treated with levothyroxine. There is no family history of breast cancer. Examination shows large, moderately ptotic breasts. The mass in her left breast is small (approximately 1 cm x 0.5 cm), firm, mobile, and painless. It is located 4 cm from her nipple-areolar complex at the 7 o'clock position. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. No masses are palpable in her right breast. A urine pregnancy test is negative. Mammogram showed a soft tissue mass with poorly defined margins. Core needle biopsy confirms a low-grade infiltrating ductal carcinoma. The pathological specimen is positive for estrogen receptors and negative for progesterone and human epidermal growth factor receptor 2 (HER2) receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate next step in management?
- A. Lumpectomy with sentinel lymph node biopsy followed by hormone therapy
- B. Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy
- C. Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy
- D. Radical mastectomy followed by hormone therapy
- E. Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy (Correct Answer)
Tumor biology and surgical planning Explanation: **Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy**
- The patient has **early-stage (T1N0M0) estrogen receptor (ER)-positive, HER2-negative invasive ductal carcinoma** suitable for **breast-conserving surgery (lumpectomy)**.
- **Lumpectomy** must be followed by **radiation therapy** to the remaining breast tissue to reduce the risk of local recurrence, and **endocrine therapy** (due to ER positivity) is indicated to reduce systemic recurrence risk.
- **Sentinel lymph node biopsy** is performed to stage the axilla; if positive, an axillary lymph node dissection may be indicated. However, in this case, the mass is small, and there is no palpable axillary adenopathy, making sentinel lymph node biopsy the appropriate initial step.
*Lumpectomy with sentinel lymph node biopsy followed by hormone therapy*
- While **lumpectomy with sentinel lymph node biopsy** and **hormone therapy** are part of the appropriate management, **radiation therapy** to the conserved breast is a critical component that is missing from this option.
- Omitting **radiation therapy** after lumpectomy for invasive breast cancer significantly increases the risk of local recurrence.
*Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy*
- A **nipple-sparing mastectomy** is a more aggressive surgical approach than typically required for a **small, early-stage tumor** like this, which is amenable to breast-conserving surgery.
- **Axillary lymph node dissection** is usually reserved for cases with clinically positive lymph nodes or a positive sentinel lymph node biopsy, not as an initial step when there is no palpable axillary adenopathy.
*Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy*
- This option involves an **unnecessarily extensive surgical procedure (nipple-sparing mastectomy with axillary lymph node dissection)** for a **small (1cm x 0.5cm) early-stage tumor** that can be managed with breast-conserving therapy.
- While radiation and hormone therapy are relevant, the initial surgical choice is too aggressive given the clinical presentation.
*Radical mastectomy followed by hormone therapy*
- **Radical mastectomy** (which includes removal of the breast, underlying chest muscle, and axillary lymph nodes) is rarely performed today due to its significant morbidity and is not indicated for this **early-stage tumor**.
- **Modified radical mastectomy**, which removes the breast and axillary lymph nodes while preserving the chest muscle, is typically only considered if breast-conserving surgery is not feasible or desired, and **hormone therapy** would be indicated, but **radiation** may also be needed depending on other factors.
Tumor biology and surgical planning US Medical PG Question 10: An excisional biopsy is performed and the diagnosis of superficial spreading melanoma is confirmed. The lesion is 1.1 mm thick. Which of the following is the most appropriate next step in management?
- A. Surgical excision with 0.5-1 cm safety margins only
- B. Surgical excision with 1 cm safety margins only
- C. Surgical excision with 1-2 cm safety margins only
- D. Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study
- E. Surgical excision with 1-2 cm safety margins and sentinel lymph node study (Correct Answer)
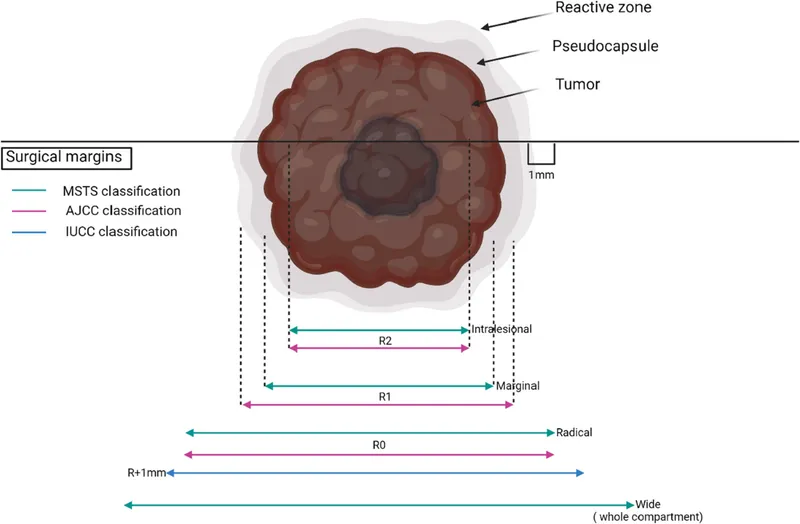
Tumor biology and surgical planning Explanation: ***Surgical excision with 1-2 cm safety margins and sentinel lymph node study***
- A melanoma with a **Breslow thickness between 1.01 mm and 2.0 mm** (like this 1.1 mm lesion) requires a recommended surgical margin of **1 to 2 cm**.
- For melanomas **≥0.8 mm thickness** (or those with ulceration), a **sentinel lymph node biopsy (SLNB)** is recommended to assess for micrometastasis, as it helps in staging and prognosis.
*Surgical excision with 0.5-1 cm safety margins only*
- A 0.5 cm margin is typically reserved for melanoma *in situ* or extremely thin melanomas (less than or equal to 0.5 mm), and 1 cm for lesions 0.51 to 1.0 mm, which is too narrow for a 1.1 mm lesion.
- This option incorrectly omits the **sentinel lymph node study**, which is indicated for a melanoma of this thickness.
*Surgical excision with 1 cm safety margins only*
- While 1 cm is a common margin for lesions up to 1.0 mm, a 1.1 mm melanoma usually warrants a slightly wider margin, ideally 1-2 cm.
- This option also fails to include the **sentinel lymph node study**, which is crucial for staging melanomas ≥0.8 mm thickness.
*Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study*
- The recommended surgical margin for a 1.1 mm melanoma is at least **1 cm, preferably between 1 and 2 cm**, making a 0.5-1 cm range insufficient.
- Although it correctly includes the sentinel lymph node study, the **surgical margin is inadequate** for the given Breslow thickness.
*Surgical excision with 1-2 cm safety margins only*
- While the **1-2 cm surgical margin** is appropriate for a 1.1 mm melanoma, this option **incorrectly excludes the sentinel lymph node study**.
- The sentinel lymph node biopsy is a critical part of the staging and management plan for melanomas of this thickness to detect potential nodal involvement.
More Tumor biology and surgical planning US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.