Survivorship issues after cancer surgery US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Survivorship issues after cancer surgery. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Survivorship issues after cancer surgery US Medical PG Question 1: A 48-year-old man is brought to the emergency department with a stab wound to his chest. The wound is treated in the emergency room. Three months later he develops a firm 4 x 3 cm nodular mass with intact epithelium over the site of the chest wound. On local examination, the scar is firm, non-tender, and there is no erythema. The mass is excised and microscopic examination reveals fibroblasts with plentiful collagen. Which of the following processes is most likely related to the series of events mentioned above?
- A. Development of a fibrosarcoma
- B. Foreign body response from suturing
- C. Staphylococcal wound infection
- D. Poor wound healing from diabetes mellitus
- E. Keloid scar formation (Correct Answer)
Survivorship issues after cancer surgery Explanation: ***Keloid scar formation***
- A **keloid** is a raised, firm, nodular scar that extends beyond the original wound boundaries and is characterized by excessive collagen deposition from **fibroblasts**.
- The delayed presentation (3 months), firm nature, absence of inflammation (no erythema, non-tender), and microscopic findings of fibroblasts with plentiful collagen are classic features of a keloid.
*Development of a fibrosarcoma*
- A fibrosarcoma is a **malignant tumor** of fibroblasts, which would typically present with more aggressive growth, often pain, and possibly ulceration, none of which are described.
- While composed of fibroblasts, fibrosarcomas exhibit **cellular atypia**, mitotic activity, and invasion, which are not mentioned in the microscopic description.
*Foreign body response from suturing*
- A foreign body response usually involves a **granulomatous inflammation** around foreign material, such as suture remnants.
- The microscopic description of "fibroblasts with plentiful collagen" without mention of inflammatory cells or foreign bodies makes this less likely.
*Staphylococcal wound infection*
- A **bacterial infection** would typically present with signs of acute inflammation such as erythema, warmth, pain, and possibly pus, shortly after the wound.
- The mass is described as non-tender with no erythema, and the 3-month delay makes an active infection less probable.
*Poor wound healing from diabetes mellitus*
- Poor wound healing in diabetes often manifests as **delayed closure**, chronic ulcers, and increased susceptibility to infection, rather than an overgrowth of fibrous tissue in the form of a nodular mass.
- While diabetes can affect wound healing, the specific description of a firm, nodular mass with excessive collagen points away from typical diabetic wound complications.
Survivorship issues after cancer surgery US Medical PG Question 2: A 49-year-old woman presents to her primary care physician for a general check up. She has not seen a primary care physician for the past 20 years but states she has been healthy during this time frame. She had breast implants placed when she was 29 years old but otherwise has not had any surgeries. She is concerned about her risk for breast cancer given her friend was recently diagnosed. Her temperature is 97.0°F (36.1°C), blood pressure is 114/64 mmHg, pulse is 70/min, respirations are 12/min, and oxygen saturation is 98% on room air. Physical exam is unremarkable. Which of the following is the most appropriate workup for breast cancer for this patient?
- A. No intervention indicated at this time
- B. Sentinel node biopsy
- C. BRCA genetic testing
- D. Mammography (Correct Answer)
- E. Ultrasound
Survivorship issues after cancer surgery Explanation: ***Mammography***
- The patient is 49 years old, making regular screening **mammography** the most appropriate initial workup for breast cancer, as guidelines recommend screening for women over 40.
- While breast implants can make mammograms more challenging, specialized techniques like **Eklund views** can be used to visualize breast tissue effectively.
*No intervention indicated at this time*
- This is incorrect because the patient's age (49) places her in the demographic for routine **breast cancer screening**.
- Delaying screening in this age group would increase the risk of detecting cancer at a later, less treatable stage.
*Sentinel node biopsy*
- **Sentinel node biopsy** is a procedure typically performed after a breast cancer diagnosis to stage the disease and determine lymph node involvement.
- It is not a screening tool and is therefore inappropriate as an initial workup in an asymptomatic patient without a known mass.
*BRCA genetic testing*
- **BRCA genetic testing** is indicated for individuals with a strong family history of breast or ovarian cancer, or those diagnosed with specific types of breast cancer at a young age.
- This patient has no such risk factors mentioned, making genetic testing unnecessary as a first-line screening step.
*Ultrasound*
- **Ultrasound** is often used as a follow-up to an abnormal mammogram or to evaluate specific palpable masses, especially in younger women with dense breasts.
- It is not typically recommended as a primary screening tool for breast cancer in a 49-year-old woman, especially without prior mammographic findings.
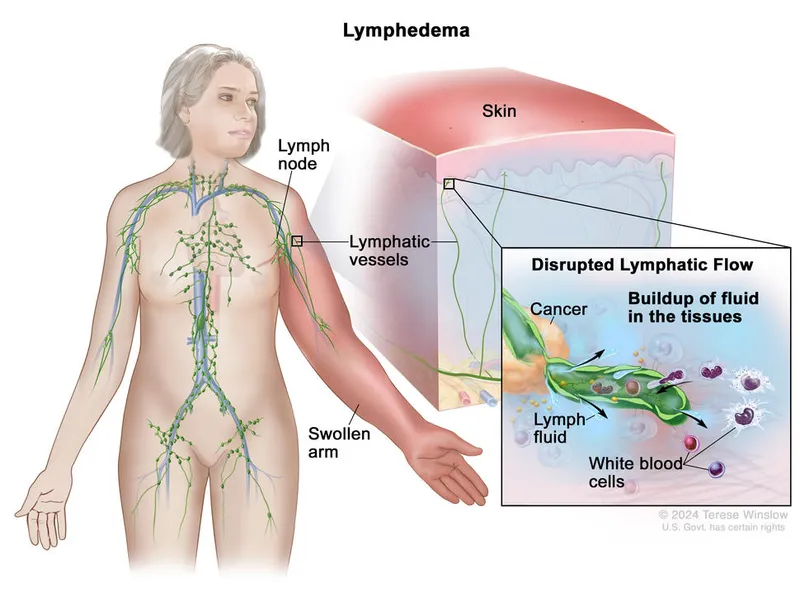
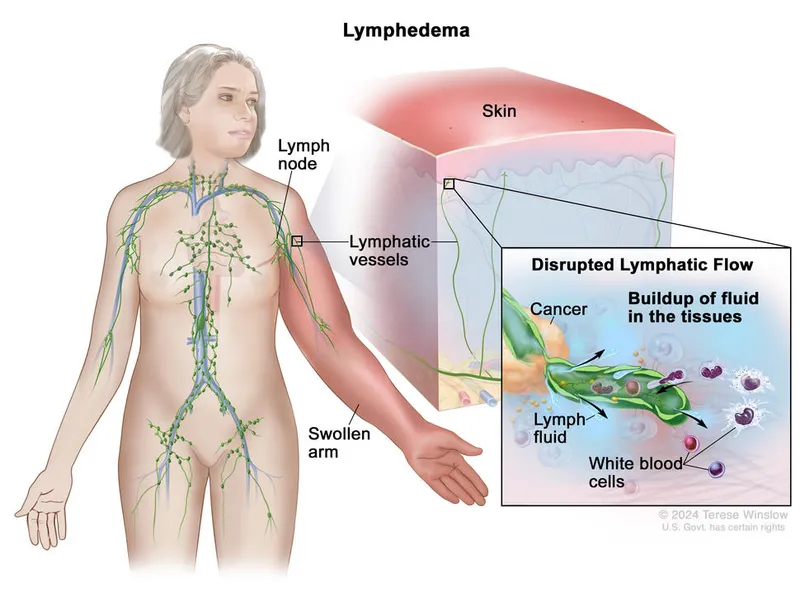
Survivorship issues after cancer surgery US Medical PG Question 3: A 59-year-old woman presents to her primary care provider with a 6-month history of progressive left-arm swelling. Two years ago she had a partial mastectomy and axillary lymph node dissection for left breast cancer. She was also treated with radiotherapy at the time. Upon further questioning, she denies fever, pain, or skin changes, but reports difficulty with daily tasks because her hand feels heavy and weak. She is bothered by the appearance of her enlarged extremity and has stopped playing tennis. On physical examination, nonpitting edema of the left arm is noted with hyperkeratosis, papillomatosis, and induration of the skin. Limb elevation, exercise, and static compression bandaging are started. If the patient has no improvement, which of the following will be the best next step?
- A. Diethylcarbamazine
- B. Low molecular weight heparin
- C. Endovascular stenting
- D. Vascularized lymph node transfer (Correct Answer)
- E. Antibiotics
Survivorship issues after cancer surgery Explanation: ***Vascularized lymph node transfer***
- This patient presents with **secondary lymphedema** due to axillary dissection and radiotherapy, which has not responded to conservative management.
- **Vascularized lymph node transfer** is a surgical option that involves transplanting healthy lymph nodes to the affected area to re-establish lymphatic drainage pathways, offering a more definitive solution for refractory cases.
*Diethylcarbamazine*
- **Diethylcarbamazine** is an anti-filarial drug used to treat lymphedema caused by **parasitic infections**, specifically filariasis.
- The patient's lymphedema is secondary to breast cancer treatment, not parasitic infection, making this a **misdirected treatment**.
*Low molecular weight heparin*
- **Low molecular weight heparin** is an anticoagulant used to prevent or treat **venous thromboembolism (VTE)**.
- While patients with cancer are at increased risk for VTE, her symptoms are consistent with lymphedema and not thrombosis, which would typically present with more acute pain and swelling, making this an inappropriate treatment.
*Endovascular stenting*
- **Endovascular stenting** is a procedure used to open blocked or narrowed **blood vessels**, such as in peripheral artery disease or venous obstruction.
- Her condition is specifically lymphedema, a lymphatic circulation issue, not a vascular obstruction, so stenting would not address the underlying problem.
*Antibiotics*
- **Antibiotics** are used to treat **bacterial infections**, which can complicate lymphedema (e.g., cellulitis).
- While chronic lymphedema causes skin changes (hyperkeratosis, papillomatosis, induration), the patient shows no signs of **acute infection** such as fever, pain, erythema, or warmth, making empirical antibiotics unnecessary at this stage.
Survivorship issues after cancer surgery US Medical PG Question 4: A 55-year-old woman is being managed on the surgical floor after having a total abdominal hysterectomy as a definitive treatment for endometriosis. On day 1 after the operation, the patient complains of fevers. She has no other complaints other than aches and pains from lying in bed as she has not moved since the procedure. She is currently receiving ondansetron, acetaminophen, and morphine. Her temperature is 101°F (38.3°C), blood pressure is 127/68 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 94% on room air. Her abdominal exam is within normal limits and cardiopulmonary exam is only notable for mild crackles. Which of the following is the most likely etiology of this patient’s fever?
- A. Deep vein thrombosis
- B. Abscess formation
- C. Inflammatory stimulus of surgery (Correct Answer)
- D. Urinary tract infection
- E. Wound infection
Survivorship issues after cancer surgery Explanation: ***Inflammatory stimulus of surgery***
- Postoperative fever occurring within the first 24-48 hours after surgery, especially a major abdominal procedure, is most commonly due to the **systemic inflammatory response** to tissue trauma and stress from the surgery itself.
- The temperature of 101°F (38.3°C) is a common reactive fever. In this timeframe, **atelectasis** (part of the inflammatory response to surgery) is the classic cause, supported by the patient's **immobility since surgery** and **mild crackles** on exam.
- The patient has no other specific signs of infection, making this the most likely cause.
*Deep vein thrombosis*
- While DVT is a concern post-surgery, it typically presents with **leg pain, swelling, and tenderness**, not primarily as fever alone on day 1.
- A fever from DVT would usually indicate a more advanced complication like pulmonary embolism, which is inconsistent with the mild crackles and stable oxygen saturation.
*Abscess formation*
- Abscesses usually take several days to form and present with significant fevers, localized pain, and possibly purulent drainage, not typically within the first **24 hours post-op**.
- The abdominal exam is noted as within normal limits, making an abscess unlikely at this early stage.
*Urinary tract infection*
- UTIs are common post-op, especially with catheterization, but typically present with **dysuria, frequency, urgency**, and sometimes suprapubic pain, which are absent here.
- While fever can be a symptom, the lack of urinary complaints makes it a less likely primary diagnosis on day 1.
*Wound infection*
- Wound infections rarely develop within the first **24-48 hours** post-surgery, as bacteria require time to proliferate and cause inflammatory signs.
- Typical signs include **erythema, warmth, tenderness, and purulent drainage** at the incision site, which are not mentioned.
Survivorship issues after cancer surgery US Medical PG Question 5: A 51-year-old woman presents for her annual wellness visit. She says she feels healthy and has no specific concerns. Past medical history is significant for bipolar disorder, hypertension, and diabetes mellitus type 2, managed with lithium, lisinopril, and metformin, respectively. Her family history is significant for hypertension and diabetes mellitus type 2 in her father, who died from lung cancer at age 67. Her vital signs include: temperature 36.8°C (98.2°F), pulse 97/min, respiratory rate 16/min, blood pressure 120/75 mm Hg. Physical examination is unremarkable. Mammogram findings are labeled breast imaging reporting and data system-3 (BIRADS-3) (probably benign). Which of the following is the next best step in management in this patient?
- A. Follow-up mammogram in 6 months (Correct Answer)
- B. Follow-up mammogram in 1 year
- C. Treatment
- D. Biopsy
- E. Breast MRI
Survivorship issues after cancer surgery Explanation: ***Follow-up mammogram in 6 months***
- A **BIRADS-3** (Breast Imaging Reporting and Data System 3) classification indicates a **probably benign finding**, with a less than 2% chance of malignancy.
- The recommended management for BIRADS-3 is a **short-interval follow-up mammogram in 6 months** to assess for stability or changes.
*Follow-up mammogram in 1 year*
- This follow-up interval is typically recommended for **BIRADS-1 (negative)** or **BIRADS-2 (benign)** findings, not for BIRADS-3.
- Waiting a full year would delay the detection of any potential malignancy in a BIRADS-3 lesion.
*Treatment*
- Treatment is indicated for confirmed malignancy, typically after a biopsy has confirmed cancerous cells.
- Starting treatment at the BIRADS-3 stage would be premature given the low probability of malignancy.
*Biopsy*
- A biopsy is generally warranted for **BIRADS-4 (suspicious)** or **BIRADS-5 (highly suggestive of malignancy)** lesions.
- While biopsy can be considered for BIRADS-3 if there are high-risk factors or patient preference, **short-interval follow-up** is the standard and preferred initial approach.
*Breast MRI*
- Breast MRI is often used for high-risk patients, for **staging known breast cancer**, or to evaluate **dense breast tissue**.
- It is not the standard next step for a BIRADS-3 finding in a patient with no specific high-risk indications beyond the mammogram result.
Survivorship issues after cancer surgery US Medical PG Question 6: A 45-year-old man undergoes elective vasectomy for permanent contraception. The procedure is performed under local anesthesia. There are no intra-operative complications and he is discharged home with ibuprofen for post-operative pain. This patient is at increased risk for which of the following complications?
- A. Prostatitis
- B. Seminoma
- C. Testicular torsion
- D. Sperm granuloma (Correct Answer)
- E. Inguinal hernia
Survivorship issues after cancer surgery Explanation: **Sperm granuloma**
- A **sperm granuloma** can occur after vasectomy due to the extravasation of sperm from the severed vas deferens, leading to a foreign body granulomatous reaction.
- This complication presents as a **palpable, tender nodule** at the vasectomy site and is a relatively common long-term issue.
*Prostatitis*
- **Prostatitis** is an inflammation of the prostate gland, and there is no direct mechanistic link or increased risk following a vasectomy.
- It is typically caused by bacterial infection or non-infectious inflammatory processes, unrelated to the **vas deferens** ligation.
*Seminoma*
- **Seminoma** is a type of testicular germ cell tumor, and extensive research has shown no increased risk of developing testicular cancer after vasectomy.
- The procedure does not alter the cellular processes or environment within the testicles that predispose to germ cell tumor formation.
*Testicular torsion*
- **Testicular torsion** is a urological emergency involving the twisting of the spermatic cord, which cuts off blood supply to the testis.
- This condition is not associated with vasectomy; it typically occurs due to an anatomical abnormality (e.g., **bell-clapper deformity**) or trauma.
*Inguinal hernia*
- An **inguinal hernia** is a protrusion of abdominal contents through a weakness in the abdominal wall, specifically in the inguinal canal.
- Vasectomy is a superficial procedure that does not involve manipulating or weakening the abdominal wall in a way that would increase the risk of an inguinal hernia.
Survivorship issues after cancer surgery US Medical PG Question 7: A 25-year-old man presents to his primary care physician for recurrent headaches. The patient states that the headaches have been going on for the past week, and he is concerned that he may have cancer. Based on his symptoms, he strongly believes that he needs further diagnostic workup. The patient works as a nurse at the local hospital and is concerned that he is going to lose his job. The patient is also concerned about his sexual performance with his girlfriend, and as a result he has ceased to engage in sexual activities. Finally, the patient is concerned about his relationship with his family. He states that his concerns related to these issues have persisted for the past year. The patient has a past medical history of obesity, diabetes, hypertension, and irritable bowel syndrome. His current medications include metformin, insulin, lisinopril, and hydrochlorothiazide. The patient has a family history of colorectal cancer in his grandfather and father. The patient's neurological exam is within normal limits. The patient denies having a headache currently. Which of the following is the best initial step in management?
- A. Buspirone
- B. Sumatriptan
- C. Fluoxetine (Correct Answer)
- D. Clonazepam
- E. MRI head
Survivorship issues after cancer surgery Explanation: ***Fluoxetine***
- The patient exhibits symptoms consistent with **generalized anxiety disorder** (GAD), including excessive worry about multiple areas of life (health, job, relationships, sexual performance) for over a year, and associated physical symptoms (headaches). **SSRIs like fluoxetine** are first-line treatment for GAD.
- The patient's multiple health concerns, despite a normal neurological exam, and his persistent worries suggest an underlying anxiety disorder that would benefit from pharmacological intervention.
*Buspirone*
- Buspirone is an **anxiolytic** that can be used for GAD, but it typically has a **slower onset of action** and is often considered a second-line agent or an add-on therapy rather than the initial monotherapy for severe, pervasive anxiety.
- While it may be suitable, an **SSRI (like fluoxetine)** is generally preferred as the first-line and most effective option for chronic GAD due to its broader efficacy profile.
*Sumatriptan*
- **Sumatriptan is a triptan** used for the acute treatment of **migraines** and cluster headaches.
- The patient's headaches are recurrent but he denies having one currently, and the primary concern appears to be underlying anxiety rather than the acute management of a headache.
*Clonazepam*
- Clonazepam is a **benzodiazepine**, which can provide rapid relief for anxiety symptoms. However, it is typically used for **short-term management** of acute anxiety or as an adjunct due to its potential for **dependence** and withdrawal symptoms.
- It is not recommended as a first-line, long-term monotherapy for chronic GAD, as it does not address the underlying anxious thought patterns as effectively as SSRIs.
*MRI head*
- This patient has a normal neurological exam, making a **diagnostic MRI head** for headaches in the absence of **focal neurological deficits** or "red flag" symptoms (e.g., papilledema, thunderclap headache) unnecessary as an initial step.
- While the patient is concerned about cancer, further imaging is not indicated given the current clinical presentation strongly suggesting an **anxiety disorder**.
Survivorship issues after cancer surgery US Medical PG Question 8: An 84-year-old woman is brought to the physician by her son after he found her trying to hang herself from the ceiling because she felt that she was a burden to her family. Her family says that for the past 2 months she has had no energy to leave her room, has been sleeping most of the day, has lost 10 kg (22 lb), and cries every day. She was diagnosed with breast cancer that has metastasized to the liver 4 months ago. She moved in with her son and daughter-in-law shortly after the diagnosis. She initially underwent chemotherapy but discontinued the treatment when the metastases spread to the spine and brain. Her life expectancy is 1–2 weeks and she is currently receiving home-hospice care. Her only current medication is a fentanyl patch. She is 160 cm (5 ft 3 in) tall and weighs 46 kg (101.4 lb); BMI is 18 kg/m2. Her vital signs are within normal limits. Examination shows slow speech, a flat affect, and depressed mood. Which of the following treatments is initially most likely to provide the greatest benefit for this patient?
- A. Electroconvulsive therapy
- B. Methylphenidate (Correct Answer)
- C. Megestrol
- D. Fluoxetine
- E. Bupropion
Survivorship issues after cancer surgery Explanation: ***Methylphenidate***
- This patient presents with **severe depression** at the end of life with a very limited prognosis (1-2 weeks), making quick symptom relief paramount. **Psychostimulants** like methylphenidate can offer a rapid antidepressant effect (within days) and improve energy and appetite.
- Given her **advanced cancer**, **poor prognosis**, and **suicidal ideation**, a fast-acting treatment that improves quality of life quickly is crucial.
*Electroconvulsive therapy*
- While highly effective for severe depression, **ECT** requires multiple sessions and is a more invasive treatment not typically chosen for immediate symptom relief in a patient with a life expectancy of 1-2 weeks.
- The patient's **metastatic cancer** and overall frail condition would make the associated risks (e.g., anesthesia) disproportionate to the limited time frame for benefit.
*Megestrol*
- **Megestrol acetate** is a progestin sometimes used as an appetite stimulant in patients with cachexia, particularly in cancer or AIDS.
- It would not address the patient's **depressive symptoms** or **suicidal ideation**, which are the primary concerns requiring urgent intervention.
*Fluoxetine*
- **Fluoxetine**, a selective serotonin reuptake inhibitor (SSRI), is a common antidepressant but typically takes **4-6 weeks** to achieve its full therapeutic effect.
- Given the patient's life expectancy of 1-2 weeks and her severe suicidal ideation, a delayed-onset medication like fluoxetine would not be appropriate for immediate symptom management.
*Bupropion*
- **Bupropion** is an antidepressant that also takes several weeks to exert its full effect.
- Like other typical antidepressants, its **delayed onset of action** makes it unsuitable for a patient with such a limited prognosis needing rapid symptom relief for severe depression and suicidality.
Survivorship issues after cancer surgery US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Survivorship issues after cancer surgery Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Survivorship issues after cancer surgery US Medical PG Question 10: A 68-year-old man comes to the physician because of a 6-month history of difficulty swallowing pieces of meat and choking frequently during meal times. He also sometimes regurgitates foul-smelling, undigested food particles. Examination shows a 3 x 3 cm soft cystic, immobile mass in the upper third of the left side of his neck anterior to the left sternocleidomastoid muscle that becomes prominent when he coughs. A barium swallow shows an accumulation of contrast on the lateral aspect of the neck at the C5 level. Which of the following is the most likely underlying cause for this patient's condition?
- A. Remnant of the embryological omphalomesenteric duct
- B. Inadequate relaxation of lower esophageal sphincter
- C. Remnant of the thyroglossal duct
- D. Increased intrapharyngeal pressure (Correct Answer)
- E. Remnant of the second branchial cleft
Survivorship issues after cancer surgery Explanation: ***Increased intrapharyngeal pressure***
- The symptoms of **dysphagia**, **regurgitation of undigested food**, and a **neck mass prominent with coughing** are classic for a **Zenker's diverticulum**, which results from increased intrapharyngeal pressure causing herniation of mucosa through Killian's triangle.
- The barium swallow showing **contrast accumulation** and the location of the mass further support this diagnosis, as Zenker's diverticula are pseudo-diverticula caused by pulsion from high pressure during swallowing.
*Remnant of the embryological omphalomesenteric duct*
- An **omphalomesenteric duct remnant** typically presents as a **Meckel's diverticulum** in the small intestine or an umbilical fistula, not as a neck mass with swallowing difficulties.
- This embryological anomaly is related to the midgut development and has no connection to pharyngeal issues.
*Inadequate relaxation of lower esophageal sphincter*
- **Inadequate relaxation of the lower esophageal sphincter** (LES) is characteristic of **achalasia**, which causes dysphagia and regurgitation, but typically of *fermented* rather than *undigested* food, and does not present with a palpable neck mass as described.
- Achalasia involves the distal esophagus and does not lead to a pharyngeal outpouching.
*Remnant of the thyroglossal duct*
- A **thyroglossal duct cyst** is a midline neck mass that moves with swallowing and tongue protrusion, which is not consistent with the lateral, pulsion-type mass that becomes prominent with coughing.
- While it can be found in the upper third of the neck, its embryological origin and presentation differ significantly from a Zenker's diverticulum.
*Remnant of the second branchial cleft*
- A **second branchial cleft cyst** is typically a lateral neck mass, often located anterior to the sternocleidomastoid muscle, but it is congenital and does not typically present with progressive dysphagia and regurgitation of undigested food in adulthood, nor does it typically become prominent with coughing due to increased intrapharyngeal pressure.
- These cysts are usually asymptomatic unless infected and are not directly related to swallowing mechanics.
More Survivorship issues after cancer surgery US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.