Surgical oncology emergencies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surgical oncology emergencies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surgical oncology emergencies US Medical PG Question 1: A 60-year-old patient presents to the urgent care clinic with complaints of pain and abdominal distention for the past several weeks. The pain began with a change in bowel habits 3 months ago, and he gradually defecated less until he became completely constipated, which led to increasing pain and distention. He also mentions that he has lost weight during this period, even though he has not changed his diet. When asked about his family history, the patient reveals that his brother was diagnosed with colorectal cancer at 65 years of age. An abdominal radiograph and CT scan were done which confirmed the diagnosis of obstruction. Which of the following locations in the digestive tract are most likely involved in this patient’s disease process?
- A. Small bowel
- B. Ascending colon
- C. Rectum
- D. Sigmoid colon (Correct Answer)
- E. Cecum
Surgical oncology emergencies Explanation: ***Sigmoid colon***
- This patient's symptoms—**progressive constipation, abdominal distention, weight loss**, and a family history of colorectal cancer—strongly suggest a **colorectal malignancy** causing obstruction.
- The **sigmoid colon** is the most common site for colorectal cancer, especially those presenting with obstructive symptoms due to its narrower lumen compared to the proximal colon.
*Small bowel*
- While small bowel obstruction can cause similar symptoms, **primary small bowel cancers are rare** and typically present differently, often with episodes of partial obstruction.
- The history of a **change in bowel habits preceding complete constipation** is more indicative of a colonic mass.
*Ascending colon*
- Cancers in the **right colon (ascending and cecum)** tend to present with symptoms like **iron deficiency anemia, fatigue, and occult bleeding**, rather than obstruction, due to its wider lumen and more fluid stool.
- **Obstruction is less common** as an initial presentation in this location.
*Rectum*
- Rectal cancers often cause **changes in bowel habits, tenesmus, and hematochezia** (bright red blood per rectum).
- While obstruction can occur, the sigmoid colon is a more frequent site for tumors causing **progressive obstructive symptoms** as described.
*Cecum*
- Similar to the ascending colon, cancers in the **cecum** are more likely to present with **anemia and vague abdominal discomfort** rather than overt obstruction.
- The **wider diameter** of the cecum allows tumors to grow quite large before causing obstructive symptoms.
Surgical oncology emergencies US Medical PG Question 2: A 68-year-old male is diagnosed with squamous cell carcinoma in the upper lobe of his right lung. A chest radiograph can be seen in image A. Which of the following would you most expect to find in this patient?
- A. Anisocoria (Correct Answer)
- B. Superior vena cava syndrome
- C. Digital clubbing
- D. Polydipsia
- E. Lateral gaze palsy
Surgical oncology emergencies Explanation: ***Anisocoria***
- A tumor in the **upper lobe of the right lung** (a **Pancoast tumor**) can compress the **sympathetic chain**, leading to **Horner's syndrome**.
- **Horner's syndrome** classically presents with unilateral symptoms on the affected side, including **miosis** (constricted pupil), **ptosis** (drooping eyelid), and **anhydrosis** (decreased sweating), which would cause an apparent **anisocoria** due to the difference in pupil size.
- This is the **most expected finding** for an upper lobe lung tumor due to direct anatomical proximity to the sympathetic chain.
*Superior vena cava syndrome*
- This syndrome is usually caused by tumors in the **upper or middle mediastinum** compressing the **superior vena cava**, leading to facial and upper extremity edema, and distended neck veins.
- While it can occur with lung cancer, a tumor specifically located in the right upper lobe is **less likely** to directly compress the SVC compared to one in the mediastinum.
*Digital clubbing*
- **Digital clubbing** is a common paraneoplastic syndrome associated with various lung diseases, including **lung cancer**, particularly **adenocarcinoma**.
- While possible with squamous cell carcinoma, it is **not location-specific** and can occur with any lung tumor, making it less specific than the neurological findings expected with a Pancoast tumor.
*Polydipsia*
- **Polydipsia** (excessive thirst) can be a symptom of **hypercalcemia**, a paraneoplastic syndrome sometimes associated with **squamous cell carcinoma of the lung** due to the production of **parathyroid hormone-related peptide (PTHrP)**.
- While a possible paraneoplastic syndrome, it is a **metabolic feature** rather than a direct anatomical finding highly specific to an upper lobe tumor compressing local structures.
*Lateral gaze palsy*
- A **lateral gaze palsy** is caused by damage to the **abducens nerve (CN VI)** or its nucleus, leading to an **inability to move the eye laterally**.
- This symptom is **not typically associated** with a primary lung tumor in the upper lobe unless there is widespread metastatic disease affecting the brainstem or cranial nerves, which is not directly indicated.
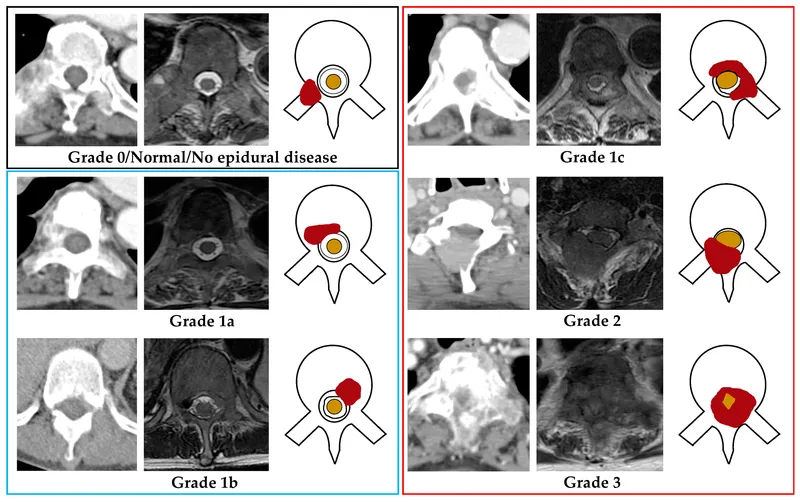
Surgical oncology emergencies US Medical PG Question 3: A 36-year-old man is seen in the emergency department for back pain that has been getting progressively worse over the last 4 days. Upon further questioning, he also notes that he has been having a tingling and burning sensation rising up from his feet to his knees bilaterally. The patient states he is having difficulty urinating and having bowel movements over the last several days. His temperature is 97.4°F (36.3°C), blood pressure is 122/80 mmHg, pulse is 85/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for weak leg flexion bilaterally along with decreased anal sphincter tone. Which of the following is the best next step in management?
- A. Emergency surgery
- B. CT
- C. Pulmonary function tests
- D. Lumbar puncture
- E. MRI (Correct Answer)
Surgical oncology emergencies Explanation: ***MRI***
- The patient's symptoms (back pain, ascending paresthesias, bladder/bowel dysfunction, and decreased anal sphincter tone) are highly suggestive of **cauda equina syndrome**. An **MRI of the spine** is the gold standard for diagnosing this condition, as it can visualize the spinal cord and nerve roots directly.
- Early diagnosis and intervention with MRI are crucial to prevent **permanent neurological deficits** in cauda equina syndrome.
*Emergency surgery*
- While emergency surgery might be the next step *after* diagnosis, it is **not the initial diagnostic step**. The cause of the cauda equina syndrome (e.g., disc herniation, tumor) must first be identified.
- Performing surgery without proper imaging could lead to operating on the wrong level or for the wrong pathology.
*CT*
- A **CT scan** can provide information about bony structures but is generally **inferior to MRI** for visualizing soft tissue structures like the spinal cord, nerve roots, and intervertebral discs, which are critical in cauda equina syndrome.
- It may miss subtle compressions or pathologies of the nerve roots.
*Pulmonary function tests*
- **Pulmonary function tests** are used to assess lung function and are **irrelevant** to the patient's acute neurological symptoms and back pain.
- This test would not provide any diagnostic information for suspected cauda equina syndrome.
*Lumbar puncture*
- A **lumbar puncture** is primarily used to analyze cerebrospinal fluid for conditions like infection or inflammation (e.g., meningitis, Guillain-Barré syndrome).
- While Guillain-Barré can cause ascending paralysis, the prominent back pain, bowel/bladder dysfunction, and decreased anal sphincter tone make **cauda equina syndrome** a more likely diagnosis, for which LP is not the primary diagnostic tool.
Surgical oncology emergencies US Medical PG Question 4: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Surgical oncology emergencies Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
Surgical oncology emergencies US Medical PG Question 5: An otherwise healthy 57-year-old man presents to the emergency department because of progressive shortness of breath and exercise intolerance for the past 5 days. He denies recent travel or illicit habits. His temperature is 36.7°C (98.1°F), the blood pressure is 88/57 mm Hg, and the pulse is 102/min. The radial pulse weakens with inspiration. Physical examination reveals bilateral 1+ pedal edema. There is jugular venous distention at 13 cm and muffled heart sounds. Transthoracic echocardiogram shows reciprocal respiratory ventricular inflow and ventricular diastolic collapse. Which of the following is the best next step in the management of this patient condition?
- A. Pericardiectomy
- B. Pericardial drainage (Correct Answer)
- C. Cardiac catheterization
- D. Cardiac MRI
- E. Chest X-ray
Surgical oncology emergencies Explanation: ***Pericardial drainage***
- The clinical presentation, including progressive **shortness of breath**, **hypotension**, **tachycardia**, **pulsus paradoxus** (weak radial pulse with inspiration), **jugular venous distention**, **muffled heart sounds**, and **bilateral pedal edema**, strongly suggests **cardiac tamponade** due to a pericardial effusion.
- Prompt **pericardial drainage** (pericardiocentesis) is a life-saving intervention for cardiac tamponade, as it relieves the pressure on the heart and restores cardiac output.
*Pericardiectomy*
- This is a surgical procedure to remove part or all of the pericardium, typically performed in cases of **constrictive pericarditis** or recurrent effusions that fail conservative management.
- It is a more invasive procedure and not the immediate life-saving intervention required for acute cardiac tamponade.
*Cardiac catheterization*
- This procedure involves inserting a catheter into a blood vessel to measure pressures within the heart chambers and great vessels, often used for diagnosing **coronary artery disease** or valvular heart disease.
- While it can provide hemodynamic data, it is not the most immediate or direct therapeutic intervention for cardiac tamponade.
*Cardiac MRI*
- **Cardiac MRI** provides detailed anatomical imaging of the heart and pericardium, useful for characterizing pericardial effusions or detecting myocardial abnormalities.
- Although it could confirm the diagnosis, it takes time and is not the emergent therapeutic step needed for an unstable patient with cardiac tamponade.
*Chest X-ray*
- A **chest X-ray** might show an enlarged cardiac silhouette (water bottle sign) in cases of large pericardial effusions.
- However, it is not sufficiently sensitive or specific for diagnosing cardiac tamponade and does not provide detailed information about ventricular collapse or hemodynamic compromise.
Surgical oncology emergencies US Medical PG Question 6: A 69-year-old man is brought to the emergency department because of severe abdominal pain radiating to his left flank for 30 minutes. He is weak and has been unable to stand since the onset of the pain. He vomited twice on the way to the hospital. He has not passed stools for 3 days. He has hypertension, coronary heart disease, and peptic ulcer disease. He has smoked half a pack of cigarettes daily for 46 years. Current medications include enalapril, metoprolol, aspirin, simvastatin, and pantoprazole. He appears ill. His temperature is 37°C (98.6°F), pulse is 131/min, respirations are 31/min, and blood pressure is 82/56 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. Examination shows a painful pulsatile abdominal mass. Intravenous fluid resuscitation is begun. Which of the following is the most appropriate next step in management?
- A. Transfusion of packed red blood cells
- B. CT scan of the abdomen and pelvis with contrast
- C. Open emergency surgery (Correct Answer)
- D. Colonoscopy
- E. Supine and erect x-rays of the abdomen
Surgical oncology emergencies Explanation: ***Open emergency surgery***
- The patient presents with classic signs of a **ruptured abdominal aortic aneurysm (AAA)**: sudden onset severe abdominal pain radiating to the flank, **hemodynamic instability** (hypotension, tachycardia), and a **painful pulsatile abdominal mass**.
- Given the patient's critical condition and high suspicion for a ruptured AAA, immediate **open emergency surgery** is the most appropriate next step to control the hemorrhage and repair the aneurysm.
*Transfusion of packed red blood cells*
- While **blood transfusion** is indicated and necessary due to presumed significant blood loss, it is a supportive measure, not the definitive treatment.
- Transfusion alone will not stop the ongoing hemorrhage from a ruptured aneurysm, which requires surgical intervention.
*CT scan of the abdomen and pelvis with contrast*
- A **CT scan** would confirm the diagnosis of a ruptured AAA, but obtaining it would cause a dangerous delay in a patient with severe hemodynamic instability.
- In a patient with classic signs of rupture and hypovolemic shock, surgical exploration takes precedence over diagnostic imaging.
*Colonoscopy*
- **Colonoscopy** is an invasive diagnostic procedure used to visualize the colon and rectum, primarily for gastrointestinal bleeding, polyps, or inflammatory bowel disease.
- It is completely inappropriate for a patient presenting with acute, severe abdominal pain, hemodynamic instability, and a pulsatile mass, as it carries risks and would critically delay life-saving intervention.
*Supine and erect x-rays of the abdomen*
- **Plain abdominal x-rays** have limited utility in diagnosing a ruptured AAA; they might show calcification of the aortic wall but cannot reliably detect rupture or retroperitoneal hemorrhage.
- This imaging modality would not provide sufficient information to guide immediate management and would delay definitive treatment in a critically ill patient.
Surgical oncology emergencies US Medical PG Question 7: Three days after undergoing laparoscopic colectomy, a 67-year-old man reports swelling and pain in his right leg. He was diagnosed with colon cancer 1 month ago. His temperature is 38.5°C (101.3°F). Physical examination shows swelling of the right leg from the ankle to the thigh. There is no erythema or rash. Which of the following is likely to be most helpful in establishing the diagnosis?
- A. D-dimer level
- B. Compression ultrasonography (Correct Answer)
- C. CT pulmonary angiography
- D. Transthoracic echocardiography
- E. Blood cultures
Surgical oncology emergencies Explanation: ***Compression ultrasonography***
- This patient's presentation with **unilateral leg swelling and pain** after surgery, especially given his recent **colon cancer diagnosis** (a hypercoagulable state), is highly suspicious for a **deep vein thrombosis (DVT)**.
- **Compression ultrasonography** is the gold standard, non-invasive imaging modality for diagnosing DVT, allowing direct visualization of thrombi and assessing venous compressibility.
*D-dimer level*
- While a **positive D-dimer** indicates recent or ongoing clot formation, it is **non-specific** and can be elevated in many conditions, including surgery, cancer, and infection.
- A normal D-dimer can rule out DVT in low-probability patients, but a high D-dimer in a high-probability patient (like this case) requires further imaging for confirmation, making it less definitive than ultrasound.
*CT pulmonary angiography*
- This imaging is used to diagnose a **pulmonary embolism (PE)**, which is a complication of DVT, but the primary symptoms here are localized to the leg.
- While PE is a concern, diagnosing the source (DVT) in the leg is the immediate priority for treatment and prevention of future complications.
*Transthoracic echocardiography*
- **Echocardiography** evaluates cardiac structure and function and can sometimes detect large clots in the right heart leading to PE, but it is not the primary diagnostic tool for DVT in the leg.
- It would be done if signs of cardiac strain or shunting associated with acute PE were prominent, which is not the case here.
*Blood cultures*
- **Blood cultures** are used to diagnose **bacteremia or sepsis**, which might explain a fever, but the prominent, unilateral leg swelling and pain are not typical for a primary infectious cause in the leg without local signs of cellulitis or abscess.
- While a low-grade fever is present, the absence of erythema or rash makes a primary infectious etiology less likely than DVT given the risk factors.
Surgical oncology emergencies US Medical PG Question 8: A 67-year-old man presents to the emergency department with altered mental status. The patient is non-verbal at baseline, but his caretakers at the nursing home noticed he was particularly somnolent recently. The patient has a past medical history of diabetes and Alzheimer dementia. His temperature is 99.7°F (37.6°C), blood pressure is 157/98 mmHg, pulse is 150/min, respirations are 16/min, and oxygen saturation is 98% on room air. Laboratory values are obtained and shown below.
Hemoglobin: 9 g/dL
Hematocrit: 33%
Leukocyte count: 8,500/mm^3 with normal differential
Platelet count: 197,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 102 mEq/L
K+: 4.3 mEq/L
HCO3-: 25 mEq/L
BUN: 37 mg/dL
Glucose: 99 mg/dL
Creatinine: 2.4 mg/dL
Ca2+: 12.2 mg/dL
The patient has lost 20 pounds over the past month. His parathyroid hormone is within normal limits, and his urinary calcium is increased. Physical exam demonstrates discomfort when the patient's lower back and extremities are palpated. Which of the following is the most accurate diagnostic test for this patient's underlying diagnosis?
- A. Peripheral blood smear
- B. Urine protein levels
- C. Bone marrow biopsy (Correct Answer)
- D. Radiograph of the lumbar spine
- E. Urine, blood, and cerebrospinal fluid cultures
Surgical oncology emergencies Explanation: **Bone marrow biopsy**
- The patient presents with **hypercalcemia**, **elevated creatinine** (acute kidney injury), **anemia**, **weight loss**, and bony pain, which are classic features of **multiple myeloma**; a bone marrow biopsy is crucial for diagnosis and staging by identifying plasma cell infiltration.
- Identification of > **10% clonal plasma cells** in the bone marrow confirms the diagnosis of multiple myeloma in patients with myeloma-defining events (e.g., hypercalcemia, renal failure, anemia, bone lesions).
*Peripheral blood smear*
- While a peripheral blood smear might show **rouleaux formation** in multiple myeloma due to increased plasma proteins, it is not specific or diagnostic as rouleaux can be seen in other conditions like inflammation.
- It does not quantify the percentage of **clonal plasma cells**, which is essential for diagnosing multiple myeloma.
*Urine protein levels*
- **Urine protein electrophoresis (UPEP)** and **immunofixation** are important for detecting Bence-Jones proteinuria (clonal free light chains) which supports the diagnosis of multiple myeloma, but quantifying general urine protein levels (e.g., with a 24-hour collection) is not as specific or diagnostic.
- While **elevated urine protein** is expected in multiple myeloma due to light chain excretion, it doesn't provide definitive evidence of plasma cell dyscrasia or bone marrow involvement.
*Radiograph of the lumbar spine*
- **Skeletal surveys** (including radiographs) are used to identify **lytic bone lesions** characteristic of multiple myeloma, which contribute to pain and hypercalcemia.
- Although important for identifying bone involvement, radiographs are not the most accurate diagnostic test for the underlying disease itself, as they do not directly evaluate the presence of **clonal plasma cells**.
*Urine, blood, and cerebrospinal fluid cultures*
- These cultures are primarily used to diagnose **infections**, which can cause altered mental status and fever.
- While infection is a consideration, the constellation of hypercalcemia, renal failure, anemia, and bone pain points strongly toward multiple myeloma, making cultures less likely to reveal the primary underlying diagnosis.
Surgical oncology emergencies US Medical PG Question 9: An obese 52-year-old man is brought to the emergency department because of increasing shortness of breath for the past 8 hours. Two months ago, he noticed a mass on the right side of his neck and was diagnosed with laryngeal cancer. He has smoked two packs of cigarettes daily for 27 years. He drinks two pints of rum daily. He appears ill. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 111/min, respirations are 34/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 89%. Examination shows a 9-cm, tender, firm subglottic mass on the right side of the neck. Cervical lymphadenopathy is present. His breathing is labored and he has audible inspiratory stridor but is able to answer questions. The lungs are clear to auscultation. Arterial blood gas analysis on room air shows:
pH 7.36
PCO2 45 mm Hg
PO2 74 mm Hg
HCO3- 25 mEq/L
He has no advanced directive. Which of the following is the most appropriate next step in management?
- A. Comfort care measures
- B. Cricothyroidotomy (Correct Answer)
- C. Tracheostomy
- D. Intramuscular epinephrine
- E. Tracheal stenting
Surgical oncology emergencies Explanation: ***Correct: Cricothyroidotomy***
- This patient has **impending complete airway obstruction** evidenced by inspiratory stridor, severe tachypnea (34/min), hypoxia (O2 sat 89%), and a large obstructing laryngeal mass
- **Cricothyroidotomy** is the emergent surgical airway procedure of choice when there is **imminent or actual complete upper airway obstruction** and endotracheal intubation cannot be safely performed
- The subglottic mass makes endotracheal intubation **extremely dangerous** - instrumentation could precipitate complete obstruction and inability to ventilate
- Cricothyroidotomy provides **immediate airway access** (can be performed in 30-60 seconds) below the level of obstruction, making it life-saving in this emergency
- In the "cannot intubate, cannot ventilate" scenario, cricothyroidotomy is the definitive emergency intervention per ATLS and airway management guidelines
*Incorrect: Tracheostomy*
- While tracheostomy provides definitive airway management, it is a **controlled, elective procedure** typically performed in the OR that takes 20-30 minutes
- This patient requires **immediate airway access** - waiting for OR setup and performing tracheostomy risks complete airway collapse and death
- Tracheostomy may be performed later as a planned procedure once the airway is secured with cricothyroidotomy
- The presence of stridor indicates **critical airway narrowing** requiring emergency intervention, not elective surgery
*Incorrect: Comfort care measures*
- The patient is **alert and oriented** without an advanced directive indicating wishes for comfort care only
- This is an **acute, reversible condition** with appropriate emergency airway intervention
- Presumed consent applies in life-threatening emergencies when the patient cannot formally consent but intervention would be life-saving
- Comfort care would be inappropriate without documented patient wishes or irreversible terminal condition
*Incorrect: Intramuscular epinephrine*
- Epinephrine is indicated for **anaphylaxis** or angioedema causing airway edema from allergic/inflammatory mechanisms
- This patient has **mechanical obstruction** from a solid tumor mass, which will not respond to epinephrine
- Epinephrine causes vasoconstriction and reduces mucosal edema but cannot reduce tumor mass
- Would delay definitive airway management and not address the underlying problem
*Incorrect: Tracheal stenting*
- Tracheal stenting requires **bronchoscopy** in a controlled setting and is used for palliation of tracheal narrowing
- Cannot be performed emergently in an unstable patient with impending airway obstruction
- The obstruction is at the **laryngeal/subglottic level**, not typically amenable to emergency stenting
- Requires time for procedure setup and sedation, which this patient cannot afford given the critical airway emergency
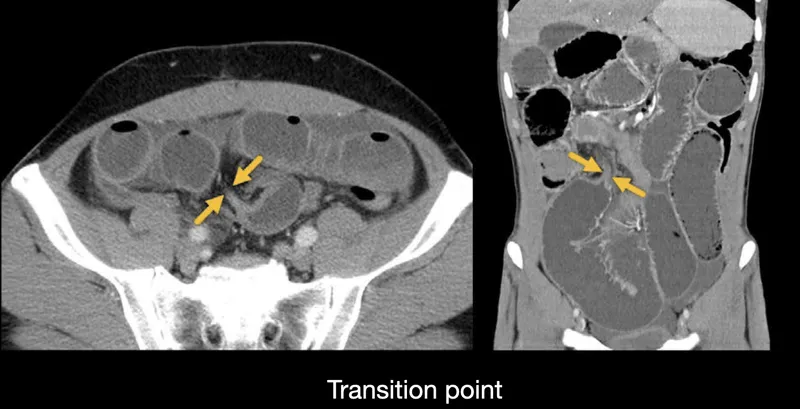
Surgical oncology emergencies US Medical PG Question 10: A 32-year-old Caucasian female is admitted to the emergency department with a 48-hour history of severe and diffuse abdominal pain, nausea, vomiting, and constipation. Her personal history is unremarkable except for an ectopic pregnancy 5 years ago. Upon admission, she is found to have a blood pressure of 120/60 mm Hg, a pulse of 105/min, a respiratory rate 20/min, and a body temperature of 37°C (98.6°F). She has diffuse abdominal tenderness, hypoactive bowel sounds, and mild distention on examination of her abdomen. Rectal and pelvic examination findings are normal. What is the most likely cause of this patient's condition?
- A. Adhesions (Correct Answer)
- B. Enlarged Peyer’s plaques
- C. Gastrointestinal malignancy
- D. Malrotation
- E. Hernia
Surgical oncology emergencies Explanation: ***Adhesions***
- The patient's history of **ectopic pregnancy** is a significant risk factor for **intra-abdominal adhesions**, particularly if surgical intervention was required, which can cause **small bowel obstruction**.
- Symptoms like diffuse abdominal pain, nausea, vomiting, constipation, and hypoactive bowel sounds are classic signs of **bowel obstruction**.
- **Adhesions** are the most common cause of small bowel obstruction in patients with prior abdominal or pelvic procedures.
*Enlarged Peyer's plaques*
- Enlarged Peyer's patches are typically associated with conditions like **intussusception** in children or infections, and less commonly in adults as a cause of obstruction unless severely inflamed.
- This condition does not typically present with a history linked to previous gynecological conditions or procedures that commonly induce adhesive disease.
*Gastrointestinal malignancy*
- While gastrointestinal malignancy can cause bowel obstruction, it's less likely in a 32-year-old without other risk factors for **cancer** (e.g., family history, chronic inflammatory disease, weight loss).
- The acute presentation in a young patient with a history of prior pelvic pathology makes adhesions a much more probable cause than an undiagnosed malignancy.
*Malrotation*
- **Malrotation** is a congenital anomaly usually presenting in **infancy or early childhood** with symptoms like bilious vomiting due to midgut volvulus.
- It is highly unlikely to present for the first time with this constellation of symptoms in a 32-year-old adult.
*Hernia*
- An **external hernia** would typically present with a visible or palpable lump, which was not mentioned in the physical exam findings.
- An **internal hernia** is possible but less common than adhesions as a cause of obstruction, especially in patients with a history of prior abdominal or pelvic pathology.
More Surgical oncology emergencies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.