Metastasectomy indications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Metastasectomy indications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Metastasectomy indications US Medical PG Question 1: A 64-year-old woman presents to the surgical oncology clinic as a new patient for evaluation of recently diagnosed breast cancer. She has a medical history of type 2 diabetes mellitus for which she takes metformin. Her surgical history is a total knee arthroplasty 7 years ago. Her family history is insignificant. Physical examination is notable for an irregular nodule near the surface of her right breast. Her primary concern today is which surgical approach will be chosen to remove her breast cancer. Which of the following procedures involves the removal of a portion of a breast?
- A. Arthroplasty
- B. Lumpectomy (Correct Answer)
- C. Vasectomy
- D. Mastectomy
- E. Laminectomy
Metastasectomy indications Explanation: ***Lumpectomy***
- A **lumpectomy** is a surgical procedure that removes the **breast cancer tumor** and a small margin of surrounding healthy tissue, preserving most of the breast.
- This procedure is a common treatment for early-stage breast cancer and is often followed by radiation therapy.
*Arthroplasty*
- **Arthroplasty** is a surgical procedure to **repair or replace a joint**, typically due to arthritis or injury.
- The patient's history of a total knee arthroplasty indicates this procedure was performed on her knee, not her breast.
*Vasectomy*
- A **vasectomy** is a surgical procedure for **male sterilization**, involving the cutting and sealing of the vas deferens.
- This procedure is unrelated to breast cancer treatment or breast surgery.
*Mastectomy*
- A **mastectomy** involves the **complete surgical removal of the entire breast**, often including the nipple and areola.
- While it is a breast surgery, it removes the *entire* breast, not just a portion.
*Laminectomy*
- A **laminectomy** is a surgical procedure that removes a portion of the **vertebra (lamina)** to relieve pressure on the spinal cord or nerves.
- This procedure is for spinal conditions and is entirely unrelated to breast cancer surgery.
Metastasectomy indications US Medical PG Question 2: A 70-year-old man comes to the physician because of right-sided back pain, red urine, and weight loss for the last 4 months. He has smoked one pack of cigarettes daily for 40 years. A CT scan of the abdomen shows a large right-sided renal mass. Biopsy of the mass shows polygonal clear cells filled with lipids. Which of the following features is necessary to determine the tumor grade in this patient?
- A. Invasion of surrounding structures
- B. Response to chemotherapy
- C. Nuclear pleomorphism and nucleolar prominence (Correct Answer)
- D. Involvement of regional lymph nodes
- E. Size of malignant proliferation
Metastasectomy indications Explanation: ***Nuclear pleomorphism and nucleolar prominence***
- The **Fuhrman nuclear grading system** (and newer WHO/ISUP grading system) for renal cell carcinoma is based on **nuclear morphologic features**: nuclear size, nuclear contour irregularity, and most importantly, **nucleolar prominence**.
- **Grade 1**: Small uniform nuclei with inconspicuous nucleoli
- **Grade 2**: Slightly irregular nuclei with small nucleoli visible at 400× magnification
- **Grade 3**: Moderately irregular nuclei with prominent nucleoli visible at 100× magnification
- **Grade 4**: Marked nuclear pleomorphism, multilobated nuclei, and prominent nucleoli
- Higher nuclear grades correlate with more aggressive tumor behavior and worse prognosis.
*Invasion of surrounding structures*
- This feature is crucial for **tumor staging (T stage)**, specifically T3 disease when perinephric fat, renal vein, or IVC is invaded, and T4 when beyond Gerota's fascia.
- **Invasion** determines surgical approach and prognosis related to local spread but does not define histological grade.
*Response to chemotherapy*
- **Response to chemotherapy** is evaluated after treatment and is not a feature used for grading at diagnosis.
- Clear cell RCC is **chemoresistant**; treatment typically involves targeted therapy (VEGF inhibitors, mTOR inhibitors) or immunotherapy, not traditional chemotherapy.
*Involvement of regional lymph nodes*
- **Lymph node involvement** is a component of **tumor staging (N stage)**: N0 (no nodes), N1 (regional nodes positive).
- It indicates metastatic spread and significantly worsens prognosis but does not contribute to **histological grade**, which assesses cellular differentiation.
*Size of malignant proliferation*
- **Tumor size** is the primary criterion for **T staging**: T1a (≤4 cm), T1b (>4-7 cm), T2a (>7-10 cm), T2b (>10 cm), all confined to kidney.
- Size is a prognostic factor but does not determine **histological grade**, which is based exclusively on nuclear microscopic features.
Metastasectomy indications US Medical PG Question 3: An 84-year-old woman is brought to the physician by her son after he found her trying to hang herself from the ceiling because she felt that she was a burden to her family. Her family says that for the past 2 months she has had no energy to leave her room, has been sleeping most of the day, has lost 10 kg (22 lb), and cries every day. She was diagnosed with breast cancer that has metastasized to the liver 4 months ago. She moved in with her son and daughter-in-law shortly after the diagnosis. She initially underwent chemotherapy but discontinued the treatment when the metastases spread to the spine and brain. Her life expectancy is 1–2 weeks and she is currently receiving home-hospice care. Her only current medication is a fentanyl patch. She is 160 cm (5 ft 3 in) tall and weighs 46 kg (101.4 lb); BMI is 18 kg/m2. Her vital signs are within normal limits. Examination shows slow speech, a flat affect, and depressed mood. Which of the following treatments is initially most likely to provide the greatest benefit for this patient?
- A. Electroconvulsive therapy
- B. Methylphenidate (Correct Answer)
- C. Megestrol
- D. Fluoxetine
- E. Bupropion
Metastasectomy indications Explanation: ***Methylphenidate***
- This patient presents with **severe depression** at the end of life with a very limited prognosis (1-2 weeks), making quick symptom relief paramount. **Psychostimulants** like methylphenidate can offer a rapid antidepressant effect (within days) and improve energy and appetite.
- Given her **advanced cancer**, **poor prognosis**, and **suicidal ideation**, a fast-acting treatment that improves quality of life quickly is crucial.
*Electroconvulsive therapy*
- While highly effective for severe depression, **ECT** requires multiple sessions and is a more invasive treatment not typically chosen for immediate symptom relief in a patient with a life expectancy of 1-2 weeks.
- The patient's **metastatic cancer** and overall frail condition would make the associated risks (e.g., anesthesia) disproportionate to the limited time frame for benefit.
*Megestrol*
- **Megestrol acetate** is a progestin sometimes used as an appetite stimulant in patients with cachexia, particularly in cancer or AIDS.
- It would not address the patient's **depressive symptoms** or **suicidal ideation**, which are the primary concerns requiring urgent intervention.
*Fluoxetine*
- **Fluoxetine**, a selective serotonin reuptake inhibitor (SSRI), is a common antidepressant but typically takes **4-6 weeks** to achieve its full therapeutic effect.
- Given the patient's life expectancy of 1-2 weeks and her severe suicidal ideation, a delayed-onset medication like fluoxetine would not be appropriate for immediate symptom management.
*Bupropion*
- **Bupropion** is an antidepressant that also takes several weeks to exert its full effect.
- Like other typical antidepressants, its **delayed onset of action** makes it unsuitable for a patient with such a limited prognosis needing rapid symptom relief for severe depression and suicidality.
Metastasectomy indications US Medical PG Question 4: A 63-year-old man comes to the physician because of a 1-month history of difficulty swallowing, low-grade fever, and weight loss. He has smoked one pack of cigarettes daily for 30 years. An esophagogastroduodenoscopy shows an esophageal mass just distal to the upper esophageal sphincter. Histological examination confirms the diagnosis of locally invasive squamous cell carcinoma. A surgical resection is planned. Which of the following structures is at greatest risk for injury during this procedure?
- A. Bronchial branch of thoracic aorta
- B. Left gastric artery
- C. Left inferior phrenic artery
- D. Esophageal branch of thoracic aorta
- E. Inferior thyroid artery (Correct Answer)
Metastasectomy indications Explanation: **Inferior thyroid artery**
- The esophageal mass is located just distal to the **upper esophageal sphincter**, which is in the neck, close to the **thyroid gland**.
- During surgery for an esophageal tumor in this region, the **inferior thyroid artery**, which supplies the thyroid and adjacent structures, is at the greatest risk of injury due to its proximity.
*Bronchial branch of thoracic aorta*
- The **bronchial branches** of the thoracic aorta primarily supply the bronchi and lungs.
- These vessels are located deeper in the thorax, away from the **upper esophageal sphincter** and the initial surgical field for an upper esophageal tumor.
*Left gastric artery*
- The **left gastric artery** supplies the stomach and is a branch of the celiac trunk.
- This artery is located in the **abdomen**, far from the surgical site involving an esophageal mass near the upper esophageal sphincter.
*Left inferior phrenic artery*
- The **left inferior phrenic artery** primarily supplies the diaphragm.
- This vessel originates from the aorta in the **abdominal region**, which is distant from the upper esophageal sphincter.
*Esophageal branch of thoracic aorta*
- **Esophageal branches** directly supply the esophagus; however, the question refers to the **thoracic aorta branches**.
- Tumors near the **upper esophageal sphincter** are usually accessed via a cervical incision, making thoracic branches less likely to be injured compared to arteries located in the neck.
Metastasectomy indications US Medical PG Question 5: A 19-year-old woman presents to the physician for a routine health maintenance examination. She has a past medical history of gastroesophageal reflux disease. She recently moved to a new city to begin her undergraduate studies. Her father was diagnosed with colon cancer at age 46. Her father's brother died because of small bowel cancer. Her paternal grandfather died because of stomach cancer. She takes a vitamin supplement. Current medications include esomeprazole and a multivitamin. She smoked 1 pack of cigarettes daily for 3 years but quit 2 years ago. She drinks 1–2 alcoholic beverages on the weekends. She appears healthy. Vital signs are within normal limits. Physical examination shows no abnormalities. Colonoscopy is unremarkable. Germline testing via DNA sequencing in this patient shows mutations in DNA repair genes MLH1 and MSH2. Which of the following will this patient most likely require at some point in her life?
- A. Celecoxib or sulindac therapy
- B. Surgical removal of a desmoid tumor
- C. Prophylactic proctocolectomy with ileoanal anastomosis
- D. Annual colonoscopy beginning at 20–25 years of age (Correct Answer)
- E. Measurement of carcinoembryonic antigen and CA 19-9 yearly
Metastasectomy indications Explanation: ***Annual colonoscopy beginning at 20–25 years of age***
- This patient's family history of multiple cancers at young ages (father with colon cancer at 46, uncle with small bowel cancer, grandfather with stomach cancer) combined with **germline mutations in MLH1 and MSH2** is highly indicative of **Lynch syndrome (hereditary non-polyposis colorectal cancer - HNPCC)**.
- Individuals with Lynch syndrome have a significantly increased risk of colorectal cancer, and screening with **annual colonoscopies starting at a young age (20-25 years or 2-5 years younger than the earliest age of diagnosis in the family)** is crucial for early detection and prevention.
*Celecoxib or sulindac therapy*
- **NSAID therapy** (like celecoxib or sulindac) is sometimes used for **chemoprevention in familial adenomatous polyposis (FAP)** to reduce polyp burden, especially in attenuated FAP.
- However, this patient's presentation and genetic findings point to **Lynch syndrome**, for which NSAID chemoprevention is not the primary or most effective strategy compared to surveillance.
*Surgical removal of a desmoid tumor*
- **Desmoid tumors** are benign but locally aggressive soft tissue tumors that are a characteristic **extracolonic manifestation of familial adenomatous polyposis (FAP)**, especially in patients with mutations in the APC gene.
- This patient has **Lynch syndrome**, which is associated with different extracolonic cancers (e.g., endometrial, ovarian, gastric, small bowel), but **desmoid tumors are not a typical feature of Lynch syndrome**.
*Prophylactic proctocolectomy with ileoanal anastomosis*
- **Prophylactic proctocolectomy** is the standard preventive surgery for individuals with **familial adenomatous polyposis (FAP)** to prevent the inevitable development of colorectal cancer due to hundreds to thousands of polyps.
- While Lynch syndrome carries a high risk of colorectal cancer, prophylactic colectomy is generally **not recommended as the initial management** given that surveillance via colonoscopy allows for removal of precancerous polyps and early-stage cancers, reserving surgery for when clinically indicated.
*Measurement of carcinoembryonic antigen and CA 19-9 yearly*
- **Carcinoembryonic antigen (CEA) and CA 19-9** are **tumor markers** that can be elevated in certain cancers (e.g., colorectal for CEA, pancreatic/biliary for CA 19-9).
- However, these markers have **poor sensitivity and specificity for screening healthy, asymptomatic individuals** at high risk for cancer and are primarily used for monitoring disease recurrence or treatment response in diagnosed cancers. They are not recommended for routine surveillance in Lynch syndrome.
Metastasectomy indications US Medical PG Question 6: A 66-year-old man comes to the physician because of a 3-month history of constipation and streaks of blood in his stool. He has had a 10-kg (22-lb) weight loss during this period. Colonoscopy shows an exophytic tumor in the sigmoid colon. A CT scan of the abdomen shows liver metastases and enlarged mesenteric and para-aortic lymph nodes. A diagnosis of stage IV colorectal cancer is made, and palliative chemotherapy is initiated. The chemotherapy regimen includes a monoclonal antibody that inhibits tumor growth by preventing ligand binding to a protein directly responsible for epithelial cell proliferation and organogenesis. Which of the following proteins is most likely inhibited by this drug?
- A. VEGF
- B. TNF-α
- C. EGFR (Correct Answer)
- D. ALK
- E. CD52
Metastasectomy indications Explanation: ***EGFR***
- The description of a monoclonal antibody preventing ligand binding to a protein responsible for **epithelial cell proliferation** and organogenesis strongly points to the **epidermal growth factor receptor (EGFR)**.
- EGFR is highly expressed in many colorectal cancers and its activation by ligands like EGF promotes cell growth, survival, and metastasis. Inhibiting it reduces tumor progression.
*VEGF*
- **Vascular endothelial growth factor (VEGF)** is primarily involved in **angiogenesis**, the formation of new blood vessels.
- While anti-VEGF therapies (e.g., bevacizumab) are used in colorectal cancer, their mechanism is inhibiting blood supply to the tumor, not directly blocking a receptor responsible for epithelial cell proliferation as described.
*TNF-α*
- **Tumor necrosis factor-alpha (TNF-α)** is a **cytokine** primarily involved in inflammation and immune responses.
- Antibodies against TNF-α (e.g., infliximab) are used in inflammatory conditions like Crohn's disease, not typically as targeted therapy for colorectal cancer directly inhibiting epithelial proliferation.
*ALK*
- **Anaplastic lymphoma kinase (ALK)** is a **receptor tyrosine kinase** often implicated in lung cancer and lymphomas.
- ALK rearrangements lead to oncogenic fusion proteins, but it is not a primary target for widespread epithelial cell proliferation in colorectal cancer.
*CD52*
- **CD52** is a glycoprotein found on the surface of various immune cells, including lymphocytes.
- Antibodies targeting CD52 (e.g., alemtuzumab) are used in certain leukemias and lymphomas to deplete these cells, not for inhibiting epithelial cell proliferation in solid tumors.
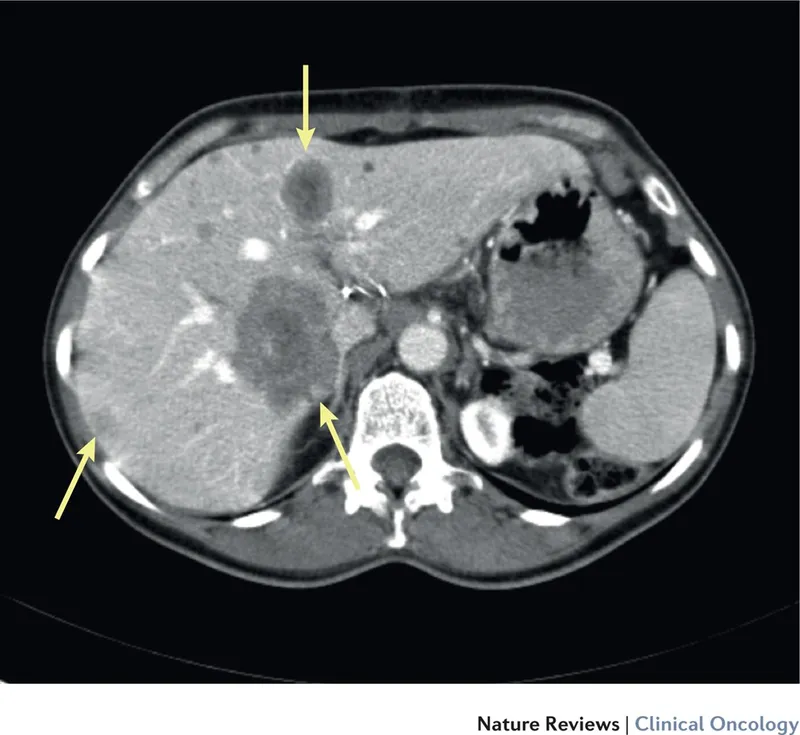
Metastasectomy indications US Medical PG Question 7: A 62-year-old man presents to his primary care physician. He was brought in by his daughter as he has refused to see a physician for the past 10 years. The patient has been having worsening abdominal pain. He claims that it was mild initially but has gotten worse over the past week. The patient has been eating lots of vegetables recently to help with his pain. The patient has a past medical history of constipation and a 50 pack-year smoking history. He is not currently taking any medications. On review of systems, the patient endorses trouble defecating and blood that coats his stool. His temperature is 99.5°F (37.5°C), blood pressure is 197/128 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 98% on room air. On abdominal exam, the patient complains of right upper quadrant tenderness and a palpable liver edge that extends 4 cm beneath the costal margin. Murphy's sign is positive. HEENT exam is notable for poor dentition, normal sclera, and normal extraocular movements. There are no palpable lymph nodes. Laboratory studies are ordered as seen below.
Hemoglobin: 9 g/dL
Hematocrit: 30%
Leukocyte count: 7,500/mm^3 with normal differential
Platelet count: 199,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.0 mEq/L
HCO3-: 23 mEq/L
BUN: 29 mg/dL
Glucose: 197 mg/dL
Creatinine: 1.4 mg/dL
Ca2+: 10.2 mg/dL
Total bilirubin: 1.1 mg/dL
AST: 150 U/L
ALT: 112 U/L
Which of the following is the most likely diagnosis?
- A. Hepatocellular carcinoma
- B. Colon cancer (Correct Answer)
- C. Pancreatic cancer
- D. Acute cholecystitis
- E. Acute appendicitis
Metastasectomy indications Explanation: ***Colon cancer***
- The patient's presentation with **worsening abdominal pain**, chronic constipation, **blood coating the stool (hematochezia)**, and **significant anemia** (hemoglobin 9 g/dL, hematocrit 30%) are highly suggestive of **colorectal malignancy**. His **50 pack-year smoking history** is a significant risk factor for colon cancer.
- The **palpable liver edge extending 4 cm below the costal margin** and **elevated AST/ALT** (150/112 U/L) suggest **hepatic metastases**, which are common with advanced colon cancer and explain the hepatomegaly and liver enzyme elevation.
- While the positive Murphy's sign suggests concurrent **acute cholecystitis**, the constellation of chronic GI symptoms (constipation, hematochezia, anemia) indicates that **colon cancer is the underlying primary diagnosis**, with possible complications including liver metastases and secondary cholecystitis (which can occur in cancer patients due to biliary obstruction from liver metastases or other factors).
- This is the **most likely unifying diagnosis** that explains the majority of clinical findings.
*Hepatocellular carcinoma*
- While **hepatocellular carcinoma (HCC)** can cause hepatomegaly, RUQ pain, and elevated liver enzymes, it does not explain the pronounced lower GI symptoms such as **chronic constipation** and **blood coating the stool (hematochezia)**.
- HCC typically requires risk factors like **chronic viral hepatitis (HBV/HCV)** or **cirrhosis**, which are not mentioned in this case. The patient's presentation is more consistent with a primary GI malignancy with hepatic metastases.
*Pancreatic cancer*
- **Pancreatic cancer** typically presents with **epigastric pain radiating to the back**, weight loss, and **painless jaundice** (courvoisier sign), but the bilirubin is only minimally elevated (1.1 mg/dL) here.
- It does not typically cause **hematochezia** or the pattern of **chronic constipation** seen in this patient, making it less likely than colon cancer.
*Acute cholecystitis*
- **Acute cholecystitis** would explain the **RUQ pain**, **positive Murphy's sign**, and **low-grade fever** (99.5°F), and may indeed be present concurrently.
- However, it does NOT explain the **chronic constipation**, **hematochezia**, **significant anemia** (Hgb 9 g/dL), or the chronic nature of symptoms. These findings point to an underlying GI malignancy as the primary diagnosis.
- Acute cholecystitis alone would not cause blood in the stool or chronic anemia, making it less likely to be the primary/most likely diagnosis.
*Acute appendicitis*
- **Acute appendicitis** presents with **acute onset right lower quadrant (RLQ) pain**, rebound tenderness, fever, and typically **leukocytosis** (WBC often >10,000/mm³).
- This patient has **normal WBC** (7,500/mm³), **RUQ pain** (not RLQ), chronic symptoms, and findings suggesting liver involvement, making appendicitis highly unlikely.
Metastasectomy indications US Medical PG Question 8: A 56-year-old woman comes to the physician because she palpated a mass in her right breast during self-examination a week ago. Menarche was at the age of 14, and her last menstrual period was at the age of 51. Vital signs are within normal limits. Examination shows a nontender, firm and hard mass in the upper outer quadrant of the right breast. Mammography shows large, dense breasts, with a 1.7-cm mass in the right upper outer quadrant. The patient undergoes right upper outer quadrant lumpectomy with subsequent sentinel node biopsy, which reveals moderately differentiated invasive ductal carcinoma and micrometastasis to one axillary lymph node. There is no evidence of extranodal metastasis. The tumor tests positive for both estrogen and progesterone receptors and does not show human epidermal growth factor receptor 2 (HER2) over-expression. Flow-cytometry reveals aneuploid tumor cells. Which of the following factors has the greatest effect on this patient's prognosis?
- A. Age
- B. Tumor size
- C. Hormone receptor status
- D. Nodal status (Correct Answer)
- E. HER2 receptor status
Metastasectomy indications Explanation: **Nodal status**
- The presence of **micrometastasis to one axillary lymph node** is the *most significant prognostic indicator* in this patient's case.
- **Lymph node involvement** signifies systemic spread and is the strongest predictor of recurrence and overall survival in breast cancer.
*Age*
- While **age** can influence treatment choices and comorbidity, it is generally *less impactful on long-term prognosis* than nodal status.
- Very young or very old age can sometimes be associated with more aggressive disease or worse outcomes, but it is not the primary determinant.
*Tumor size*
- The **tumor size of 1.7 cm** is a prognostic factor, with larger tumors generally having a worse prognosis.
- However, for this patient, the **presence of lymph node metastasis** is a more powerful indicator of systemic disease than the primary tumor size alone.
*Hormone receptor status*
- **Positive estrogen and progesterone receptors** indicate that the tumor is likely to respond to endocrine therapies.
- This is a *favorable prognostic factor* as it opens up additional treatment options, but it does not outweigh the negative impact of nodal involvement.
*HER2 receptor status*
- **Absence of HER2 overexpression** is a positive factor, as HER2-positive cancers are generally more aggressive and require targeted therapy.
- However, while HER2 status guides treatment, the presence of **lymph node metastasis** still holds greater weight in determining overall prognosis.
Metastasectomy indications US Medical PG Question 9: A 63-year-old female with known breast cancer presents with progressive motor weakness in bilateral lower extremities and difficulty ambulating. Physical exam shows 4 of 5 motor strength in her legs and hyper-reflexia in her patellar tendons. Neurologic examination 2 weeks prior was normal. Imaging studies, including an MRI, show significant spinal cord compression by the metastatic lesion and complete erosion of the T12 vertebrae. She has no metastatic disease to the visceral organs and her oncologist reports her life expectancy to be greater than one year. What is the most appropriate treatment?
- A. Palliative pain management consultation
- B. Surgical decompression and postoperative radiotherapy (Correct Answer)
- C. High-dose corticosteroids and clinical observation
- D. Radiation therapy alone
- E. Chemotherapy alone
Metastasectomy indications Explanation: ***Surgical decompression and postoperative radiotherapy***
- There is **spinal cord compression** by a metastatic lesion in a patient with a good prognosis (>1 year life expectancy) and rapidly progressive neurological deficits. **Surgical decompression** offers immediate relief of compression, while **postoperative radiotherapy** helps local tumor control.
- This combined approach is superior in preserving neurological function and improving quality of life for patients with **epidural spinal cord compression (ESCC)** in this clinical context.
*Palliative pain management consultation*
- While pain management is important in cancer care, this option alone does not address the **progressive neurological deficits** due to spinal cord compression.
- This patient's condition requires active treatment to prevent further neurological compromise and is not solely focused on comfort measures at this stage given her prognosis.
*Spinal dose corticosteroids and clinical observation*
- **Corticosteroids** can temporarily reduce edema around the spinal cord, but they do not resolve the mechanical compression caused by the eroded T12 vertebrae.
- **Clinical observation** without definitive intervention risks irreversible neurological damage given the rapid progression of symptoms.
*Radiation therapy alone*
- While radiation therapy is effective for local tumor control, it may not provide **rapid enough decompression** for acute or rapidly progressing neurological deficits due to significant mechanical compression.
- In cases of severe compression, such as bone erosion and cord involvement, surgery is usually needed prior to or in combination with radiation.
*Chemotherapy alone*
- **Chemotherapy** for breast cancer is a systemic treatment and may take time to reduce tumor burden, which is not suitable for urgent relief of **spinal cord compression**.
- It does not provide immediate mechanical decompression and is generally not the primary treatment for acute ESCC, especially with bone involvement.
Metastasectomy indications US Medical PG Question 10: A 77-year-old man is brought to the emergency department by his wife because of headache, nausea, and vomiting for 24 hours. His wife says that over the past 2 weeks, he has been more irritable and has had trouble remembering to do routine errands. Two weeks ago, he fell during a skiing accident but did not lose consciousness. He has coronary artery disease and hypertension. He has smoked one pack of cigarettes daily for 50 years. He has had 2 glasses of wine daily since his retirement 10 years ago. Current medications include atenolol, enalapril, furosemide, atorvastatin, and aspirin. He appears acutely ill. He is oriented to person but not to place or time. His temperature is 37°C (98.6°F), pulse is 99/min, respirations are 16/min, and blood pressure is 160/90 mm Hg. During the examination, he is uncooperative and unable to answer questions. Deep tendon reflexes are 4+ on the left and 2+ on the right. Babinski's sign is present on the left. There is mild weakness of the left iliopsoas and hamstring muscles. A CT scan of the head without contrast shows a high-density, 15-mm crescentic collection across the right hemispheric convexity. Which of the following is the most appropriate next step in the management of this patient?
- A. Recombinant tissue plasminogen activator administration
- B. Obtain an Electroencephalography
- C. Obtain an MRI of the head
- D. Surgical evacuation (Correct Answer)
- E. Observation
Metastasectomy indications Explanation: ***Surgical evacuation***
- The CT scan reveals a **high-density, crescentic collection**, strongly indicative of an **acute subdural hematoma**, which is causing significant neurological deficits and mass effect (e.g., increased intracranial pressure symptoms like headache, nausea, vomiting, and altered mental status, and focal neurological signs).
- Given the patient's **acute neurological decline**, significant mass effect from the 15-mm hematoma, and age, prompt **surgical evacuation** is the definitive treatment to relieve pressure and prevent further brain injury.
*Recombinant tissue plasminogen activator administration*
- **tPA** is indicated for **acute ischemic stroke**, not hemorrhagic stroke or subdural hematoma. Administering tPA in this context would be harmful, potentially worsening the hemorrhage.
- The patient's CT scan clearly shows a **hemorrhagic lesion**, not an ischemic event.
*Obtain an Electroencephalography*
- **EEG** is primarily used to evaluate **seizure disorders** or certain types of encephalopathy. While the patient has altered mental status, the primary issue identified on CT is a subdural hematoma requiring immediate intervention.
- EEG would not provide information relevant to the immediate management of an **acute subdural hematoma**.
*Obtain an MRI of the head*
- An **MRI** can provide more detailed imaging, but in the context of an **acute subdural hematoma** with significant neurological compromise, it would delay crucial and time-sensitive surgical intervention.
- The **CT scan** has already provided sufficient diagnostic information to warrant immediate surgical planning.
*Observation*
- **Observation** is not appropriate for a patient with a rapidly expanding **acute subdural hematoma** causing significant neurological deficits and a 15-mm collection, especially given the patient's age and clinical presentation.
- Delaying treatment would likely lead to further neurological deterioration, **herniation**, and potentially death.
More Metastasectomy indications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.