Lymph node sampling techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lymph node sampling techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lymph node sampling techniques US Medical PG Question 1: A 62-year-old woman presents to her physician with a painless breast mass on her left breast for the past 4 months. She mentions that she noticed the swelling suddenly one day and thought it would resolve by itself. Instead, it has been slowly increasing in size. On physical examination of the breasts, the physician notes a single non-tender, hard, and fixed nodule over left breast. An ultrasonogram of the breast shows a solid mass, and a fine-needle aspiration biopsy confirms the mass to be lobular carcinoma of the breast. When the patient asks about her prognosis, the physician says that the prognosis can be best determined after both grading and staging of the tumor. Based on the current diagnostic information, the physician says that they can only grade, but no stage, the neoplasm. Which of the following facts about the neoplasm is currently available to the physician?
- A. The tumor invades the pectoralis major.
- B. The tumor has spread via blood-borne metastasis.
- C. The tumor has not metastasized to the contralateral superior mediastinal lymph nodes.
- D. The tumor has metastasized to the axillary lymph nodes.
- E. The tumor cells exhibit marked nuclear atypia. (Correct Answer)
Lymph node sampling techniques Explanation: ***The tumor cells exhibit marked nuclear atypia.***
- **Grading** assesses the **histological appearance** of cancer cells and tissues, including features like nuclear atypia, mitotic rate, and architectural features, which are directly observable from the **fine-needle aspiration biopsy**.
- **Nuclear atypia** refers to abnormal changes in the size, shape, and chromatin pattern of cell nuclei, indicating a higher degree of anaplasia and aggressiveness.
*The tumor invades the pectoralis major.*
- **Invasion into surrounding tissues**, especially muscle, is a feature determined during **surgical staging** or comprehensive imaging, which is not described as being performed yet.
- This information relates to the **"T" (tumor size/extension)** component of TNM staging, which cannot be fully assessed with only a biopsy.
*The tumor has spread via blood-borne metastasis.*
- **Distant metastasis** is part of the **"M" (metastasis)** component of TNM staging, requiring imaging studies (e.g., PET scan, CT scan) or biopsies of suspected metastatic sites.
- The current diagnostic information (biopsy of the primary tumor) does not provide details about **blood-borne spread**.
*The tumor has not metastasized to the contralateral superior mediastinal lymph nodes.*
- Information about **lymph node involvement**, even in distant locations like the mediastinum, falls under the **"N" (nodes)** component of TNM staging, which requires thorough imaging or surgical dissection.
- The current biopsy focuses on the primary breast mass and cannot rule out distant lymph node metastasis.
*The tumor has metastasized to the axillary lymph nodes.*
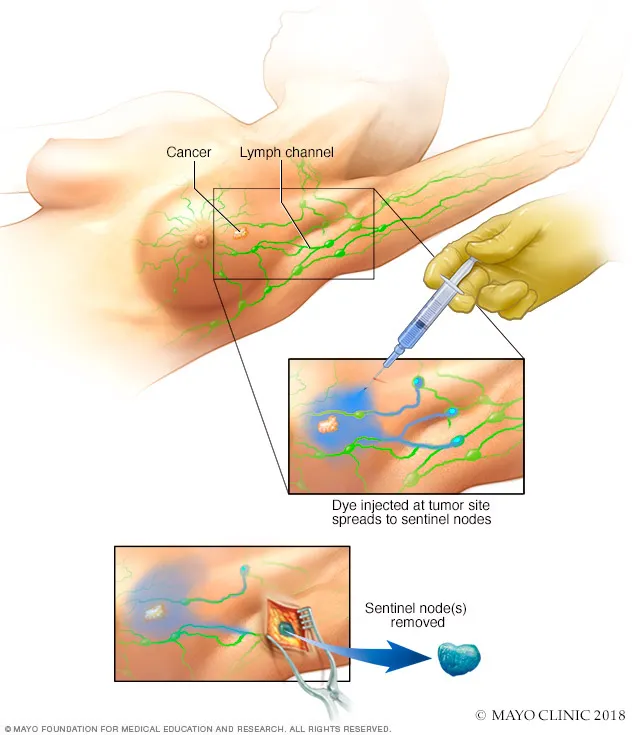
- **Axillary lymph node metastasis** is also part of the **"N" component** of staging and is typically determined by sentinel lymph node biopsy or axillary dissection performed during surgery, or through imaging.
- A fine-needle aspiration of the primary breast mass does not provide information about regional lymph node involvement.
Lymph node sampling techniques US Medical PG Question 2: A 59-year-old woman presents to her primary care provider with a 6-month history of progressive left-arm swelling. Two years ago she had a partial mastectomy and axillary lymph node dissection for left breast cancer. She was also treated with radiotherapy at the time. Upon further questioning, she denies fever, pain, or skin changes, but reports difficulty with daily tasks because her hand feels heavy and weak. She is bothered by the appearance of her enlarged extremity and has stopped playing tennis. On physical examination, nonpitting edema of the left arm is noted with hyperkeratosis, papillomatosis, and induration of the skin. Limb elevation, exercise, and static compression bandaging are started. If the patient has no improvement, which of the following will be the best next step?
- A. Diethylcarbamazine
- B. Low molecular weight heparin
- C. Endovascular stenting
- D. Vascularized lymph node transfer (Correct Answer)
- E. Antibiotics
Lymph node sampling techniques Explanation: ***Vascularized lymph node transfer***
- This patient presents with **secondary lymphedema** due to axillary dissection and radiotherapy, which has not responded to conservative management.
- **Vascularized lymph node transfer** is a surgical option that involves transplanting healthy lymph nodes to the affected area to re-establish lymphatic drainage pathways, offering a more definitive solution for refractory cases.
*Diethylcarbamazine*
- **Diethylcarbamazine** is an anti-filarial drug used to treat lymphedema caused by **parasitic infections**, specifically filariasis.
- The patient's lymphedema is secondary to breast cancer treatment, not parasitic infection, making this a **misdirected treatment**.
*Low molecular weight heparin*
- **Low molecular weight heparin** is an anticoagulant used to prevent or treat **venous thromboembolism (VTE)**.
- While patients with cancer are at increased risk for VTE, her symptoms are consistent with lymphedema and not thrombosis, which would typically present with more acute pain and swelling, making this an inappropriate treatment.
*Endovascular stenting*
- **Endovascular stenting** is a procedure used to open blocked or narrowed **blood vessels**, such as in peripheral artery disease or venous obstruction.
- Her condition is specifically lymphedema, a lymphatic circulation issue, not a vascular obstruction, so stenting would not address the underlying problem.
*Antibiotics*
- **Antibiotics** are used to treat **bacterial infections**, which can complicate lymphedema (e.g., cellulitis).
- While chronic lymphedema causes skin changes (hyperkeratosis, papillomatosis, induration), the patient shows no signs of **acute infection** such as fever, pain, erythema, or warmth, making empirical antibiotics unnecessary at this stage.
Lymph node sampling techniques US Medical PG Question 3: A 40-year-old man presents with a painless firm mass in the right breast. Examination shows retraction of the nipple and the skin is fixed to the underlying mass. The axillary nodes are palpable. Which of the following statements is FALSE regarding the above condition?
- A. Lobular cancer is the most common breast cancer in males (Correct Answer)
- B. BRCA2 mutations are associated with increased risk
- C. These are positive for estrogen receptor
- D. Endocrine therapy plays an important role in treatment
- E. Gynecomastia may be caused by certain medications
Lymph node sampling techniques Explanation: ***Lobular cancer is the most common breast cancer in males***
- This statement is **FALSE** and is the correct answer. The most common type of breast cancer in males is **invasive ductal carcinoma (IDC)**, accounting for about 80-90% of cases.
- **Invasive lobular carcinoma** is rare in men because men have very few lobules in their breast tissue.
*Gynecomastia may be caused by certain medications*
- This statement is **TRUE**. Medications such as spironolactone, cimetidine, finasteride, antipsychotics, and anabolic steroids can cause gynecomastia.
- However, the clinical presentation described (firm mass, nipple retraction, skin fixation, axillary nodes) is consistent with **malignancy**, not gynecomastia.
*BRCA2 mutations are associated with increased risk*
- This statement is **TRUE**. Male breast cancer is strongly associated with **BRCA2 mutations** (and less commonly BRCA1), which are hereditary.
- Men with BRCA2 mutations have a 5-10% lifetime risk of developing breast cancer, compared to less than 0.1% in the general male population.
*These are positive for estrogen receptor*
- This statement is **TRUE**. A vast majority (over 90%) of male breast cancers are **estrogen receptor (ER) positive**, which makes them responsive to endocrine therapy.
- This high rate of ER positivity is even greater than in female breast cancers.
*Endocrine therapy plays an important role in treatment*
- This statement is **TRUE**. Given the high prevalence of ER positivity (over 90%), endocrine therapy such as **tamoxifen** or aromatase inhibitors is a cornerstone of treatment for male breast cancer.
- Endocrine therapy is used in both adjuvant and metastatic settings for hormone receptor-positive disease.
Lymph node sampling techniques US Medical PG Question 4: A 76-year-old woman comes to the physician for evaluation of a 3-month history of vulvar itching and pain. She was diagnosed with lichen sclerosus 4 years ago. She has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows a 2.5-cm nodular, ulcerative lesion on the vaginal introitus and left labia minora with surrounding erythema. Punch biopsy shows squamous cell carcinoma. A CT scan of the chest, abdomen, and pelvis shows enlarged lymph nodes concerning for metastatic disease. Which of the following lymph node regions is the most likely primary site of metastasis?
- A. Superficial inguinal (Correct Answer)
- B. Internal iliac
- C. External iliac
- D. Inferior mesenteric
- E. Para-aortic
Lymph node sampling techniques Explanation: ***Superficial inguinal***
- The **vulva** drains primarily into the **superficial inguinal lymph nodes**, making them the most likely first site for metastatic spread from vulvar squamous cell carcinoma.
- The lesion's location on the **vaginal introitus** and **labia minora** directly correlates with this lymphatic drainage pathway.
*Internal iliac*
- **Internal iliac nodes** receive drainage mainly from deep pelvic structures like the cervix, upper vagina, and uterus, not directly from the vulva.
- Metastasis to these nodes usually occurs after involvement of more superficial nodes or in advanced disease with deeper invasion.
*External iliac*
- **External iliac nodes** generally drain the lower extremities and deeper pelvic structures (e.g., bladder, distal ureter), not the vulva as a primary site.
- Involvement here would typically indicate more advanced local spread or secondary metastasis from other pelvic nodes.
*Inferior mesenteric*
- **Inferior mesenteric nodes** drain the hindgut and its derivatives, including the distal colon and rectum, which are distant from the vulva.
- This region is not involved in the lymphatic drainage of the vulva.
*Para-aortic*
- **Para-aortic nodes** drain structures like the ovaries, fallopian tubes, and upper uterus; they are too superior for primary vulvar lymphatic drainage.
- Metastasis to these nodes from vulvar cancer would signify widespread, very advanced disease and not a primary site of spread.
Lymph node sampling techniques US Medical PG Question 5: A 56-year-old woman is referred to a plastic surgeon for breast reconstruction approximately 18 months after undergoing right modified radical mastectomy for breast cancer. Physical exam demonstrates atrophy of the lower portion of the pectoralis major muscle. Damage to which of the following nerves during mastectomy is the most likely cause of her atrophy?
- A. Long thoracic
- B. Intercostobrachial
- C. Lateral intercostal
- D. Lateral pectoral
- E. Medial pectoral (Correct Answer)
Lymph node sampling techniques Explanation: ***Medial pectoral***
- The **medial pectoral nerve** innervates both the pectoralis major and pectoralis minor muscles.
- Damage to this nerve during mastectomy can lead to **atrophy of the lower lateral portion of the pectoralis major**, as this area relies heavily on its innervation.
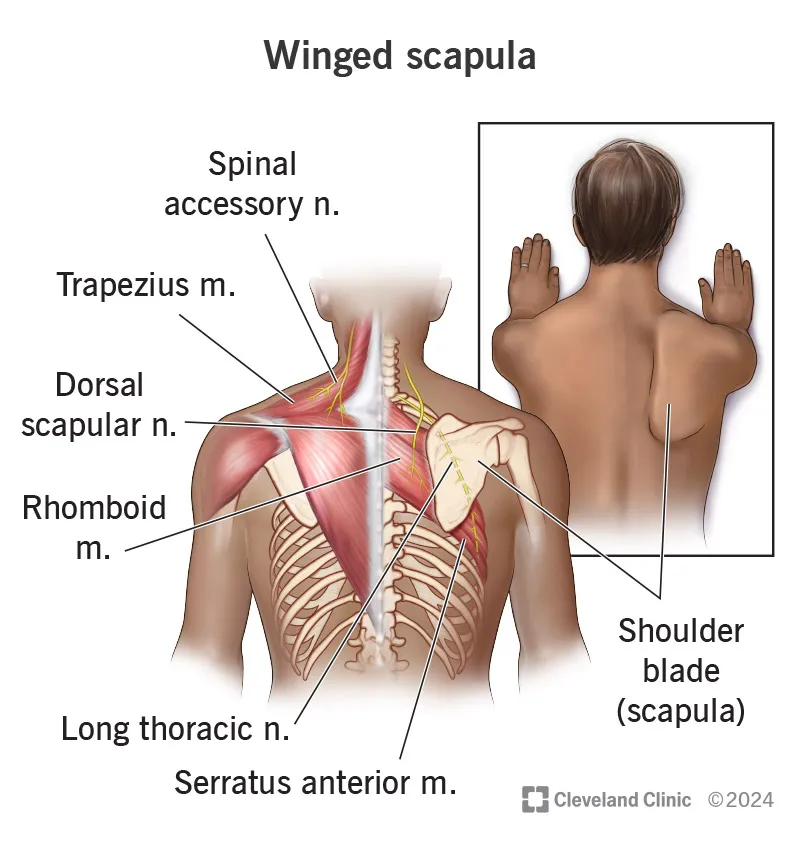
*Long thoracic*
- The **long thoracic nerve** innervates the **serratus anterior muscle**.
- Damage to this nerve would cause **scapular winging**, not atrophy of the pectoralis major.
*Intercostobrachial*
- The **intercostobrachial nerve** is primarily a **sensory nerve** supplying the skin of the upper medial arm and axilla.
- Damage to this nerve would result in **sensory changes** (numbness, pain) in that area, not muscle atrophy.
*Lateral intercostal*
- The **lateral intercostal nerves** are primarily sensory and motor to the intercostal muscles and overlying skin.
- Damage would typically cause **pain or numbness** along the chest wall or trunk, and possibly weakness of intercostal muscles, not pectoralis major atrophy.
*Lateral pectoral*
- The **lateral pectoral nerve** primarily innervates the **clavicular head** and **upper sternocostal portion** of the pectoralis major.
- Damage to this nerve would cause atrophy in the **upper and medial parts** of the pectoralis major, not specifically the lower lateral portion.
Lymph node sampling techniques US Medical PG Question 6: A 72-year-old man presents to the physician with blood in his sputum for 3 days. He also mentions that he has had a cough for the last 3 months but thought that it was because of the winter season. He also has often experienced fatigue recently. His temperature is 37.0°C (98.6°F), the respiratory rate is 15/min, the pulse is 67/min, and the blood pressure is 122/98 mm Hg. Auscultation of his chest reveals normal heart sounds but localized rhonchi over the right infrascapular region. A detailed diagnostic evaluation including a complete blood count and other serum biochemistry, chest radiogram, computed tomography of chest and abdomen, magnetic resonance imaging of the brain, bone scan, and pulmonary function tests are ordered, which confirm a diagnosis of limited-disease small cell lung cancer of 2.5 cm (1 in) in diameter, located in the lower lobe of the right lung, with the involvement of ipsilateral hilar lymph nodes and intrapulmonary lymph nodes. The mediastinal, subcarinal, scalene or supraclavicular lymph nodes are not involved, and there is no distant metastasis. There is no additional comorbidity and his performance status is good. The patient does not have any contraindication to any chemotherapeutic agents or radiotherapy. Which of the following is the best treatment option for this patient?
- A. Thoracic radiation therapy followed by prophylactic cranial irradiation
- B. Platinum-based chemotherapy plus etoposide and thoracic radiation therapy (Correct Answer)
- C. Lobectomy with adjuvant topotecan-based chemotherapy
- D. Pneumonectomy with adjuvant platinum-based chemotherapy and thoracic radiation therapy
- E. Topotecan-based chemotherapy plus thoracic radiation therapy
Lymph node sampling techniques Explanation: ***Platinum-based chemotherapy plus etoposide and thoracic radiation therapy***
- For **limited-stage small cell lung cancer (SCLC)**, combined modality treatment with **platinum-based chemotherapy (cisplatin or carboplatin) and etoposide** given concurrently with **thoracic radiation therapy** is the standard of care as it improves survival.
- This patient has limited-stage disease, defined as disease confined to one hemithorax and regional lymph nodes that can be encompassed within a tolerable radiation field.
*Thoracic radiation therapy followed by prophylactic cranial irradiation*
- While **prophylactic cranial irradiation (PCI)** is indicated for limited-stage SCLC after systemic therapy to reduce brain metastases, it's not the initial primary treatment by itself.
- **Chemotherapy** is a mandatory component of initial treatment for SCLC due to its highly metastatic nature.
*Lobectomy with adjuvant topotecan-based chemotherapy*
- **Surgery (lobectomy or pneumonectomy)** is generally not indicated for SCLC, even in limited stages, because it is a highly aggressive and systemic disease that responds better to chemotherapy and radiation.
- **Topotecan** is typically used as a second-line agent for recurrent or refractory SCLC, not as adjuvant therapy after surgery.
*Pneumonectomy with adjuvant platinum-based chemotherapy and thoracic radiation therapy*
- **Pneumonectomy** is an extensive surgery with significant morbidity and mortality and is rarely, if ever, performed for SCLC.
- While chemotherapy and radiation are components of treatment, **surgical resection (pneumonectomy in this case)** is not the standard primary therapy for SCLC given its systemic nature.
*Topotecan-based chemotherapy plus thoracic radiation therapy*
- **Topotecan** is generally reserved for **relapsed or refractory SCLC** as a second-line or later agent.
- The standard first-line chemotherapy for limited-stage SCLC involves a **platinum agent (cisplatin or carboplatin) with etoposide**.
Lymph node sampling techniques US Medical PG Question 7: A 47-year-old woman comes to the physician for a mass in her left breast she noticed 2 days ago during breast self-examination. She has hypothyroidism treated with levothyroxine. There is no family history of breast cancer. Examination shows large, moderately ptotic breasts. The mass in her left breast is small (approximately 1 cm x 0.5 cm), firm, mobile, and painless. It is located 4 cm from her nipple-areolar complex at the 7 o'clock position. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. No masses are palpable in her right breast. A urine pregnancy test is negative. Mammogram showed a soft tissue mass with poorly defined margins. Core needle biopsy confirms a low-grade infiltrating ductal carcinoma. The pathological specimen is positive for estrogen receptors and negative for progesterone and human epidermal growth factor receptor 2 (HER2) receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate next step in management?
- A. Lumpectomy with sentinel lymph node biopsy followed by hormone therapy
- B. Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy
- C. Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy
- D. Radical mastectomy followed by hormone therapy
- E. Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy (Correct Answer)
Lymph node sampling techniques Explanation: **Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy**
- The patient has **early-stage (T1N0M0) estrogen receptor (ER)-positive, HER2-negative invasive ductal carcinoma** suitable for **breast-conserving surgery (lumpectomy)**.
- **Lumpectomy** must be followed by **radiation therapy** to the remaining breast tissue to reduce the risk of local recurrence, and **endocrine therapy** (due to ER positivity) is indicated to reduce systemic recurrence risk.
- **Sentinel lymph node biopsy** is performed to stage the axilla; if positive, an axillary lymph node dissection may be indicated. However, in this case, the mass is small, and there is no palpable axillary adenopathy, making sentinel lymph node biopsy the appropriate initial step.
*Lumpectomy with sentinel lymph node biopsy followed by hormone therapy*
- While **lumpectomy with sentinel lymph node biopsy** and **hormone therapy** are part of the appropriate management, **radiation therapy** to the conserved breast is a critical component that is missing from this option.
- Omitting **radiation therapy** after lumpectomy for invasive breast cancer significantly increases the risk of local recurrence.
*Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy*
- A **nipple-sparing mastectomy** is a more aggressive surgical approach than typically required for a **small, early-stage tumor** like this, which is amenable to breast-conserving surgery.
- **Axillary lymph node dissection** is usually reserved for cases with clinically positive lymph nodes or a positive sentinel lymph node biopsy, not as an initial step when there is no palpable axillary adenopathy.
*Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy*
- This option involves an **unnecessarily extensive surgical procedure (nipple-sparing mastectomy with axillary lymph node dissection)** for a **small (1cm x 0.5cm) early-stage tumor** that can be managed with breast-conserving therapy.
- While radiation and hormone therapy are relevant, the initial surgical choice is too aggressive given the clinical presentation.
*Radical mastectomy followed by hormone therapy*
- **Radical mastectomy** (which includes removal of the breast, underlying chest muscle, and axillary lymph nodes) is rarely performed today due to its significant morbidity and is not indicated for this **early-stage tumor**.
- **Modified radical mastectomy**, which removes the breast and axillary lymph nodes while preserving the chest muscle, is typically only considered if breast-conserving surgery is not feasible or desired, and **hormone therapy** would be indicated, but **radiation** may also be needed depending on other factors.
Lymph node sampling techniques US Medical PG Question 8: An excisional biopsy is performed and the diagnosis of superficial spreading melanoma is confirmed. The lesion is 1.1 mm thick. Which of the following is the most appropriate next step in management?
- A. Surgical excision with 0.5-1 cm safety margins only
- B. Surgical excision with 1 cm safety margins only
- C. Surgical excision with 1-2 cm safety margins only
- D. Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study
- E. Surgical excision with 1-2 cm safety margins and sentinel lymph node study (Correct Answer)
Lymph node sampling techniques Explanation: ***Surgical excision with 1-2 cm safety margins and sentinel lymph node study***
- A melanoma with a **Breslow thickness between 1.01 mm and 2.0 mm** (like this 1.1 mm lesion) requires a recommended surgical margin of **1 to 2 cm**.
- For melanomas **≥0.8 mm thickness** (or those with ulceration), a **sentinel lymph node biopsy (SLNB)** is recommended to assess for micrometastasis, as it helps in staging and prognosis.
*Surgical excision with 0.5-1 cm safety margins only*
- A 0.5 cm margin is typically reserved for melanoma *in situ* or extremely thin melanomas (less than or equal to 0.5 mm), and 1 cm for lesions 0.51 to 1.0 mm, which is too narrow for a 1.1 mm lesion.
- This option incorrectly omits the **sentinel lymph node study**, which is indicated for a melanoma of this thickness.
*Surgical excision with 1 cm safety margins only*
- While 1 cm is a common margin for lesions up to 1.0 mm, a 1.1 mm melanoma usually warrants a slightly wider margin, ideally 1-2 cm.
- This option also fails to include the **sentinel lymph node study**, which is crucial for staging melanomas ≥0.8 mm thickness.
*Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study*
- The recommended surgical margin for a 1.1 mm melanoma is at least **1 cm, preferably between 1 and 2 cm**, making a 0.5-1 cm range insufficient.
- Although it correctly includes the sentinel lymph node study, the **surgical margin is inadequate** for the given Breslow thickness.
*Surgical excision with 1-2 cm safety margins only*
- While the **1-2 cm surgical margin** is appropriate for a 1.1 mm melanoma, this option **incorrectly excludes the sentinel lymph node study**.
- The sentinel lymph node biopsy is a critical part of the staging and management plan for melanomas of this thickness to detect potential nodal involvement.
Lymph node sampling techniques US Medical PG Question 9: A 56-year-old woman comes to the physician because she palpated a mass in her right breast during self-examination a week ago. Menarche was at the age of 14, and her last menstrual period was at the age of 51. Vital signs are within normal limits. Examination shows a nontender, firm and hard mass in the upper outer quadrant of the right breast. Mammography shows large, dense breasts, with a 1.7-cm mass in the right upper outer quadrant. The patient undergoes right upper outer quadrant lumpectomy with subsequent sentinel node biopsy, which reveals moderately differentiated invasive ductal carcinoma and micrometastasis to one axillary lymph node. There is no evidence of extranodal metastasis. The tumor tests positive for both estrogen and progesterone receptors and does not show human epidermal growth factor receptor 2 (HER2) over-expression. Flow-cytometry reveals aneuploid tumor cells. Which of the following factors has the greatest effect on this patient's prognosis?
- A. Age
- B. Tumor size
- C. Hormone receptor status
- D. Nodal status (Correct Answer)
- E. HER2 receptor status
Lymph node sampling techniques Explanation: **Nodal status**
- The presence of **micrometastasis to one axillary lymph node** is the *most significant prognostic indicator* in this patient's case.
- **Lymph node involvement** signifies systemic spread and is the strongest predictor of recurrence and overall survival in breast cancer.
*Age*
- While **age** can influence treatment choices and comorbidity, it is generally *less impactful on long-term prognosis* than nodal status.
- Very young or very old age can sometimes be associated with more aggressive disease or worse outcomes, but it is not the primary determinant.
*Tumor size*
- The **tumor size of 1.7 cm** is a prognostic factor, with larger tumors generally having a worse prognosis.
- However, for this patient, the **presence of lymph node metastasis** is a more powerful indicator of systemic disease than the primary tumor size alone.
*Hormone receptor status*
- **Positive estrogen and progesterone receptors** indicate that the tumor is likely to respond to endocrine therapies.
- This is a *favorable prognostic factor* as it opens up additional treatment options, but it does not outweigh the negative impact of nodal involvement.
*HER2 receptor status*
- **Absence of HER2 overexpression** is a positive factor, as HER2-positive cancers are generally more aggressive and require targeted therapy.
- However, while HER2 status guides treatment, the presence of **lymph node metastasis** still holds greater weight in determining overall prognosis.
Lymph node sampling techniques US Medical PG Question 10: A 39-year-old man presents with painless swelling of the right testis and a sensation of heaviness. The physical examination revealed an intra-testicular solid mass that could not be felt separately from the testis. After a thorough evaluation, he was diagnosed with testicular seminoma. Which of the following group of lymph nodes are most likely involved?
- A. Superficial inguinal lymph nodes (lateral group)
- B. Deep inguinal lymph nodes
- C. Superficial inguinal lymph nodes (medial group)
- D. Para-rectal lymph nodes
- E. Para-aortic lymph nodes (Correct Answer)
Lymph node sampling techniques Explanation: ***Para-aortic lymph nodes***
- The **testes** develop in the abdomen and descend into the scrotum, retaining their original lymphatic drainage. Therefore, **testicular cancer** typically metastasizes to the **para-aortic** (or retroperitoneal) lymph nodes, which are located near the renal veins at the level of L1-L2.
- This is the primary lymphatic drainage pathway for the testes.
*Superficial inguinal lymph nodes (lateral group)*
- These lymph nodes primarily drain the skin of the **scrotum**, perineum, and lower limbs, but not the **testes** themselves.
- Involvement would suggest spread to the scrotal skin or compromised lymphatic flow due to prior scrotal surgery or infection, which is not indicated here.
*Deep inguinal lymph nodes*
- **Deep inguinal lymph nodes** drain structures deeper in the leg and gluteal region, as well as receiving efferent vessels from the superficial inguinal nodes.
- They are not the primary drainage site for the **testes**.
*Superficial inguinal lymph nodes (medial group)*
- Similar to the lateral group, the **medial superficial inguinal lymph nodes** primarily drain the external genitalia (excluding the testes), perineum, and lower abdominal wall.
- They are not the direct drainage route for **testicular cancer**.
*Para-rectal lymph nodes*
- **Para-rectal lymph nodes** are located near the rectum and are involved in the drainage of the rectum and lower sigmoid colon.
- They have no direct connection to the lymphatic drainage of the **testes**.
More Lymph node sampling techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.