Oncologic Surgery Principles

On this page
🎯 The Oncologic Surgeon's Strategic Arsenal
Oncologic surgery demands more than technical skill-it requires strategic thinking that transforms cancer from an overwhelming diagnosis into a mappable, attackable target. You'll master how surgeons assess tumor biology and patient fitness, decode the TNM staging system to understand disease spread, select optimal surgical candidates, and orchestrate multimodal therapies that maximize cure while preserving quality of life. Through this lesson, you'll build a systematic framework for approaching cancer surgery: from initial evaluation through cutting-edge techniques, always anchored in multidisciplinary collaboration that defines modern cancer care.
📌 Remember: CANCER - Curative intent, Adjuvant planning, Neoadjuvant timing, Complete resection, Emergency recognition, Reconstruction needs
The foundation of oncologic surgery rests on five core principles: complete tumor removal with negative margins, preservation of function when possible, accurate staging, integration with systemic therapy, and quality of life optimization. Each principle carries specific quantitative thresholds and evidence-based guidelines.
| Surgical Principle | R0 Rate Target | Morbidity Threshold | QoL Preservation | 5-Year Survival | Functional Outcome |
|---|---|---|---|---|---|
| Curative Resection | >95% | <15% major | >80% baseline | Variable by stage | >90% independence |
| Palliative Surgery | N/A | <10% major | >70% baseline | Symptom-dependent | >75% independence |
| Cytoreductive | >90% | <25% major | >60% baseline | 12-18 months | >60% independence |
| Emergency Surgery | Variable | <30% major | >50% baseline | Stage-dependent | >50% independence |
| Reconstructive | N/A | <20% major | >85% baseline | Primary-dependent | >80% independence |
- Complete tumor removal with 2-5cm margins depending on histology
- R0 resection rates >95% for optimal outcomes
- Margin status directly correlates with local recurrence risk
- Positive margins increase recurrence by 300-500%
- Staging Accuracy
- TNM classification guides 80% of treatment decisions
- Lymph node sampling affects staging in 60% of cases
- Sentinel node accuracy 95-98% in appropriate tumors
- False negative rate <5% with proper technique
⭐ Clinical Pearl: Margin status predicts local recurrence more than tumor grade in 75% of solid tumors. A 1mm positive margin increases recurrence risk by 200-400% across most cancer types.
💡 Master This: Complete resection (R0) remains the strongest predictor of long-term survival in solid tumors, with 5-year survival dropping from 70-80% to 20-30% when margins are positive.
Understanding tumor biology transforms surgical planning from anatomical exercise to strategic intervention. Doubling time, growth patterns, and metastatic potential determine surgical timing, extent, and coordination with systemic therapy.
Connect these foundational principles through staging systems to understand how anatomical extent guides treatment algorithms.
🎯 The Oncologic Surgeon's Strategic Arsenal
🗺️ The TNM Navigation System: Decoding Cancer's Geographic Spread
📌 Remember: TNM STAGES - Tumor size/invasion, Nodal involvement, Metastatic spread, Stage grouping, Treatment planning, Adjuvant decisions, Grading integration, Emergency recognition, Survival prediction

| T Classification | Size Criteria | Invasion Depth | Resectability | 5-Year Survival | Surgical Approach |
|---|---|---|---|---|---|
| T1 | <2cm most sites | Superficial | >95% | 85-95% | Wide local excision |
| T2 | 2-5cm most sites | Limited invasion | >90% | 70-85% | Formal resection |
| T3 | >5cm or deep | Extensive local | 70-90% | 50-70% | Extended resection |
| T4 | Any size | Adjacent organs | 30-70% | 20-50% | Multivisceral resection |
- 2cm and 5cm cutoffs apply to 70% of solid tumors
- Size correlates with nodal involvement risk
- T1 tumors: 5-15% nodal involvement
- T2 tumors: 20-40% nodal involvement
- T3 tumors: 40-70% nodal involvement
- Nodal Classification Impact
- N0 vs N1 changes 5-year survival by 20-40%
- Number of positive nodes matters more than size
- 1-3 nodes: Stage IIIA in most systems
- 4+ nodes: Stage IIIB-C with worse prognosis
⭐ Clinical Pearl: Lymph node ratio (positive nodes/total examined) predicts survival better than absolute number in 60% of cancers. Ratio >0.2 significantly worsens prognosis across tumor types.
Stage Migration occurs when improved imaging detects previously occult disease, artificially improving survival statistics. Will Rogers phenomenon explains why survival appears to improve for all stages when staging accuracy increases.
- Metastatic Disease (M1)
- Changes treatment from curative to palliative in most cases
- Oligometastatic disease: 1-5 lesions may allow curative approach
- 5-year survival 20-40% with complete metastasectomy
- Site-specific considerations affect resectability
💡 Master This: Stage migration from improved imaging can artificially inflate survival statistics. True treatment progress requires stage-specific outcome analysis over time, not overall survival improvements.
Restaging after neoadjuvant therapy uses ypTNM classification, where pathologic complete response (pCR) rates vary by tumor type: breast 20-40%, rectal 15-25%, esophageal 25-35%.
Connect TNM staging through patient selection criteria to understand how staging guides surgical candidacy and approach.
🗺️ The TNM Navigation System: Decoding Cancer's Geographic Spread
🎯 The Surgical Candidacy Matrix: Patient Selection Mastery
📌 Remember: PATIENT FIT - Performance status, Age considerations, Tumor resectability, Imaging findings, Expected outcomes, Nutritional status, Timing factors, Functional reserve, Informed consent, Team consensus
Performance Status Assessment provides objective functional evaluation using ECOG or Karnofsky scales. ECOG 0-1 patients tolerate major surgery with <5% mortality, while ECOG 3-4 patients have >20% perioperative mortality.
| Selection Criteria | Excellent Candidate | Good Candidate | Marginal Candidate | Poor Candidate | Contraindicated |
|---|---|---|---|---|---|
| ECOG Status | 0-1 | 1-2 | 2 | 3 | 4 |
| Cardiac Risk | <1% | 1-5% | 5-10% | 10-20% | >20% |
| Pulmonary Function | >80% predicted | 60-80% | 40-60% | 20-40% | <20% |
| Nutritional Status | Albumin >3.5 | 3.0-3.5 | 2.5-3.0 | 2.0-2.5 | <2.0 |
| Expected Survival | >2 years | 1-2 years | 6-12 months | 3-6 months | <3 months |
- Cardiopulmonary exercise testing predicts surgical risk
- VO2 max <15 mL/kg/min increases mortality 5-fold
- Anaerobic threshold <11 mL/kg/min predicts complications
- Peak oxygen consumption correlates with outcomes
- Pulmonary function tests guide lung resection limits
- FEV1 >2L or >80% predicted for pneumonectomy
- DLCO <40% increases respiratory complications 3-fold
⭐ Clinical Pearl: Frailty assessment predicts surgical outcomes better than chronological age. Fried Frailty Phenotype score ≥3 increases 90-day mortality by 400% regardless of age.
Tumor-Specific Factors influence surgical decision-making beyond staging. Histologic grade, molecular markers, and response to neoadjuvant therapy modify surgical approach and timing.
- Resectability Assessment
- Anatomic resectability: Technical feasibility of complete removal
- Physiologic resectability: Patient tolerance of required procedure
- Hepatectomy: Requires >30% future liver remnant
- Pneumonectomy: Needs FEV1 >2L and DLCO >50%
- Oncologic resectability: Likelihood of achieving R0 resection
💡 Master This: Borderline resectable tumors require multidisciplinary evaluation and often neoadjuvant therapy to convert to resectable status. Response to treatment predicts surgical outcomes better than initial staging.
Age Considerations focus on physiologic age rather than chronological age. Octogenarians with good performance status have similar outcomes to younger patients for many procedures, while frail 60-year-olds may be poor surgical candidates.
Connect patient selection through surgical planning algorithms to understand how candidacy determines operative approach and extent.
🎯 The Surgical Candidacy Matrix: Patient Selection Mastery
🔬 The Surgical Strategy Decoder: From Assessment to Action
📌 Remember: SURGICAL PLAN - Staging completion, Unresectable assessment, Reconstruction needs, Goals clarification, Imaging review, Comorbidity optimization, Anesthesia planning, Lymphatic mapping, Pathway coordination, Length of stay, Adjuvant timing, Nutritional support
Extent of Resection depends on tumor biology, anatomic location, and functional preservation requirements. Margin adequacy varies by histology: sarcomas require 2-5cm margins, while carcinomas may need only 1-2cm.
| Resection Type | Margin Requirement | R0 Rate Target | Morbidity Risk | Functional Preservation | Reconstruction Need |
|---|---|---|---|---|---|
| Wide Local | 1-2cm | >95% | <5% | >90% | Minimal |
| Compartmental | 2-5cm | >90% | 10-20% | 70-90% | Moderate |
| Radical | En bloc | >85% | 20-40% | 50-70% | Extensive |
| Debulking | Maximal safe | 60-80% | 15-30% | 60-80% | Variable |
| Palliative | Symptomatic | N/A | <15% | >80% | Minimal |
- Sentinel lymph node biopsy for T1-T2 tumors with <5% nodal risk
- Formal lymphadenectomy when nodal involvement >20% probability
- 15-20 nodes minimum for adequate staging in most sites
- Lymph node ratio affects prognosis more than absolute number
- Extended lymphadenectomy controversial in many tumor types
⭐ Clinical Pearl: Frozen section analysis changes surgical plan in 15-25% of cases. Margin assessment accuracy is 85-90% for most tumor types, but false negative rate can reach 10-15%.
Reconstruction Planning anticipates functional deficits and cosmetic outcomes. Immediate reconstruction is preferred when oncologically safe and patient appropriate.
- Reconstruction Timing
- Immediate: 80-90% of breast cancer cases
- Delayed: When adjuvant radiation planned or margins uncertain
- Tissue expander placement maintains option
- Final reconstruction after 6-12 months
- Functional reconstruction: Nerve grafts, tendon transfers, bone reconstruction
💡 Master This: Oncoplastic principles allow wider resections while maintaining cosmetic outcomes. Volume displacement techniques enable 20-30% larger resections without mastectomy in breast cancer.
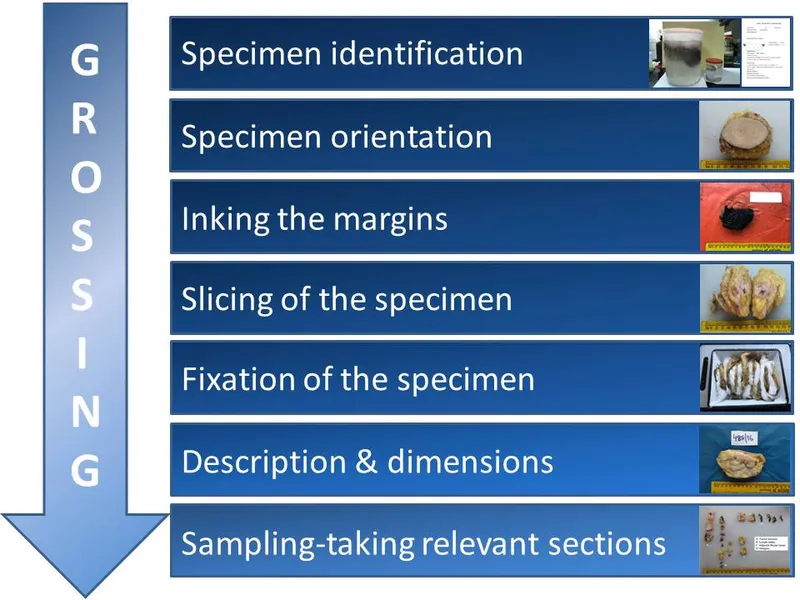
Staging Procedures may be separate or combined with definitive resection. Diagnostic laparoscopy prevents unnecessary laparotomy in 15-20% of patients with suspected peritoneal disease.
Connect surgical planning through treatment algorithms to understand how operative decisions integrate with systemic therapy timing.
🔬 The Surgical Strategy Decoder: From Assessment to Action
⚖️ The Treatment Orchestra: Coordinating Multimodal Therapy
📌 Remember: SEQUENCE MATTERS - Surgery timing, Early response assessment, Quality of life, Unresectable conversion, Emergency situations, Neoadjuvant benefits, Complete response, Evaluation intervals, Monitoring toxicity, Adjuvant planning, Timing coordination, Tumor biology, Endpoint achievement, Response prediction, Survivorship planning
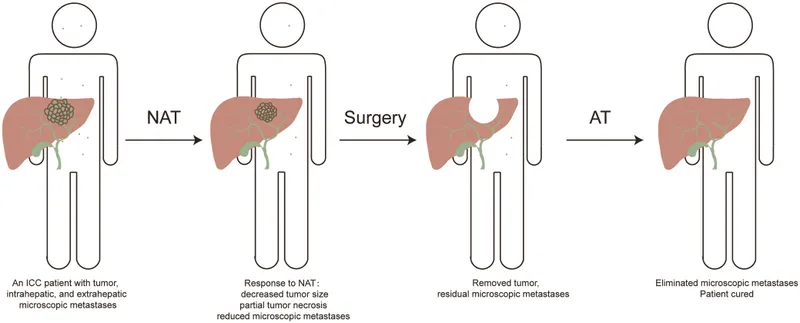
Neoadjuvant Therapy offers biological and clinical advantages in locally advanced disease. Pathologic complete response (pCR) rates predict long-term outcomes and guide adjuvant decisions.
| Cancer Type | Neoadjuvant pCR Rate | Surgery Timing | Adjuvant Benefit | 5-Year Survival | Downstaging Rate |
|---|---|---|---|---|---|
| Breast (HER2+) | 40-60% | 4-6 weeks post | 20-30% reduction | 85-95% | 60-80% |
| Rectal Cancer | 15-25% | 6-8 weeks post | 10-15% reduction | 70-85% | 40-60% |
| Esophageal | 25-35% | 4-6 weeks post | 15-25% reduction | 40-60% | 50-70% |
| Pancreatic | 5-10% | 4-6 weeks post | 10-20% reduction | 20-40% | 20-30% |
| Sarcoma | 10-20% | 2-4 weeks post | 5-15% reduction | 60-80% | 30-50% |
- Tumor downstaging improves resectability by 20-40%
- Early systemic therapy addresses micrometastatic disease
- Circulating tumor cells decrease in 60-80% of responders
- Treatment tolerance better before surgery
- Response assessment guides adjuvant planning
- Poor responders need alternative regimens
- Complete responders may avoid adjuvant therapy
⭐ Clinical Pearl: Pathologic complete response to neoadjuvant therapy predicts excellent long-term outcomes across tumor types. pCR patients have 80-90% 5-year survival compared to 60-70% for partial responders.
Adjuvant Therapy addresses residual disease risk based on pathologic findings. High-risk features include positive margins, lymph node involvement, high grade, and lymphovascular invasion.
- Adjuvant Decision Factors
- Pathologic stage determines recurrence risk
- Molecular markers predict treatment benefit
- Hormone receptor status in breast cancer
- Microsatellite instability in colorectal cancer
- EGFR mutations in lung cancer
- Performance status affects treatment tolerance
💡 Master This: Adjuvant therapy timing is critical - delays >8 weeks after surgery reduce survival benefit by 10-20%. Wound healing and performance status recovery must balance with optimal timing.
Radiation Therapy Integration requires careful coordination with surgery. Preoperative radiation may improve local control but increases surgical complications by 15-25%.
Connect treatment coordination through multidisciplinary integration to understand how team-based care optimizes outcomes.
⚖️ The Treatment Orchestra: Coordinating Multimodal Therapy
🤝 The Cancer Care Ecosystem: Multidisciplinary Excellence
📌 Remember: TEAM APPROACH - Tumor board review, Expertise integration, All disciplines represented, Multiple perspectives, Appropriate timing, Patient-centered focus, Plan coordination, Resource optimization, Outcome tracking, Adjustment capability, Communication clarity, Holistic care
Tumor Board Composition includes core members and consultative specialists who contribute disease-specific expertise and patient-specific insights. Attendance rates >80% correlate with improved outcomes and reduced treatment delays.

| Team Member | Primary Role | Decision Weight | Attendance Rate | Consultation Timing | Outcome Impact |
|---|---|---|---|---|---|
| Medical Oncologist | Systemic therapy | 25-30% | >90% | Pre/post surgery | Survival +15-20% |
| Surgical Oncologist | Resection planning | 25-30% | >95% | Primary evaluation | R0 rate +10-15% |
| Radiation Oncologist | Local control | 15-20% | >85% | Treatment planning | Local control +10% |
| Pathologist | Diagnosis/staging | 20-25% | >80% | Tissue review | Accuracy +5-10% |
| Radiologist | Imaging interpretation | 15-20% | >75% | Staging/response | Staging +5-10% |
- Case presentation with complete staging information
- Treatment option discussion with evidence-based recommendations
- Level 1 evidence guides 60-70% of decisions
- Institutional experience influences 20-30% of choices
- Consensus building through structured discussion
- Unanimous agreement in 70-80% of cases
- Majority consensus acceptable for complex cases
⭐ Clinical Pearl: Multidisciplinary care improves 5-year survival by 10-15% across cancer types. Treatment plan adherence increases from 60-70% to 85-90% with team-based decisions.
Communication Coordination ensures seamless information flow between specialists, patients, and families. Electronic health records facilitate real-time updates and decision tracking.
- Patient Navigation
- Dedicated navigators reduce treatment delays by 20-30%
- Appointment coordination minimizes patient burden
- Same-day consultations when possible
- Telemedicine integration for follow-up visits
- Education provision improves treatment compliance

💡 Master This: Patient navigation reduces time to treatment initiation by 25-40% and improves patient satisfaction scores by 15-25%. Navigator involvement correlates with better treatment completion rates.
Quality Metrics track multidisciplinary effectiveness through process measures and outcome indicators. Time to treatment, plan adherence, and patient satisfaction serve as key performance indicators.
Connect multidisciplinary care through advanced surgical techniques to understand how team coordination enables complex procedures and optimal outcomes.
🤝 The Cancer Care Ecosystem: Multidisciplinary Excellence
🚀 The Precision Surgery Revolution: Advanced Techniques and Future Horizons
📌 Remember: PRECISION TOOLS - Precision robotics, Real-time imaging, Enhanced visualization, Computer navigation, Intraoperative monitoring, Sentinel mapping, Image guidance, Oncologic principles, Navigation systems, Tissue preservation, Optimal outcomes, Operative efficiency, Learning curves, Safety protocols
Robotic Surgery provides enhanced dexterity, 3D visualization, and tremor elimination that enable complex procedures through minimal access. Learning curves vary by procedure complexity and surgeon experience.

| Surgical Approach | Conversion Rate | Operative Time | Blood Loss | Hospital Stay | Complication Rate |
|---|---|---|---|---|---|
| Open Surgery | N/A | Baseline | Baseline | 5-7 days | 15-25% |
| Laparoscopic | 5-15% | +20-40% | -50-70% | 2-4 days | 10-20% |
| Robotic | 2-8% | +10-30% | -60-80% | 1-3 days | 8-15% |
| NOTES | 10-20% | +30-50% | -70-90% | 1-2 days | 5-12% |
| Single-port | 8-18% | +15-35% | -40-60% | 1-3 days | 8-18% |
- 7 degrees of freedom vs 4 for laparoscopic instruments
- 10x magnification with 3D visualization
- Depth perception improves precision by 40-60%
- Tremor filtration enables microsurgical techniques
- Ergonomic benefits reduce surgeon fatigue
- Seated position allows longer procedures
- Intuitive controls shorten learning curves
⭐ Clinical Pearl: Robotic surgery reduces positive margin rates by 20-30% in complex anatomical locations while maintaining equivalent oncologic outcomes to open surgery in experienced hands.
Image-Guided Surgery integrates real-time imaging with surgical navigation to optimize tumor localization and critical structure preservation. Intraoperative ultrasound changes surgical plans in 15-25% of cases.
- Navigation Technologies
- Electromagnetic tracking with <2mm accuracy
- Optical tracking systems for surface registration
- Fiducial markers improve registration accuracy
- Real-time updates compensate for tissue deformation
- Augmented reality overlays imaging data on surgical field

💡 Master This: Intraoperative imaging reduces positive margin rates by 30-50% and re-excision rates by 40-60% in breast-conserving surgery. Real-time feedback enables immediate surgical adjustment.
Molecular Surgery uses fluorescent tracers and targeted imaging agents to visualize tumor margins and identify residual disease with cellular-level precision. Fluorescence-guided surgery improves complete resection rates by 15-25%.
Connect advanced techniques through rapid mastery frameworks to understand how modern oncologic surgeons integrate technology with fundamental surgical principles.
🚀 The Precision Surgery Revolution: Advanced Techniques and Future Horizons
🎯 The Oncologic Surgery Mastery Toolkit: Essential Arsenal for Excellence
📌 Remember: MASTERY ESSENTIALS - Margin assessment, Anatomic knowledge, Staging accuracy, Technique selection, Emergency recognition, Reconstruction planning, Yield optimization, Evidence integration, Safety protocols, System coordination, Ethical considerations, Navigation skills, Timing precision, Innovation adoption, Adaptability, Lifelong learning, Survivorship focus
The R0 Resection Commandments provide non-negotiable principles for complete tumor removal with optimal outcomes:
| Commandment | Quantitative Target | Clinical Impact | Monitoring Method | Failure Consequence | Mastery Indicator |
|---|---|---|---|---|---|
| Adequate Margins | >2mm most tumors | Local control +80% | Frozen section | Recurrence +300% | R0 rate >95% |
| Complete Staging | >15 nodes when indicated | Survival +15-20% | Pathology review | Understaging risk | Staging accuracy >90% |
| Functional Preservation | >80% baseline function | QoL maintenance | Functional testing | Disability burden | Function >85% |
| Complication Minimization | <15% major morbidity | Recovery optimization | Outcome tracking | Prolonged disability | Morbidity <10% |
| Team Coordination | 100% communication | Plan adherence | Process metrics | Treatment delays | Coordination >95% |
- ABCDE of Oncologic Surgery: Anatomy mastery, Biology understanding, Complete resection, Decision algorithms, Emergency recognition
- Critical Decision Points: Resectability, extent planning, reconstruction needs, staging requirements
- <5 minutes for initial assessment
- <15 minutes for complete evaluation
- Pattern Recognition Drills: High-yield scenarios with decision trees
⭐ Clinical Pearl: Master surgeons achieve R0 resection rates >95% with major morbidity <10% through systematic approaches, meticulous technique, and continuous quality improvement.
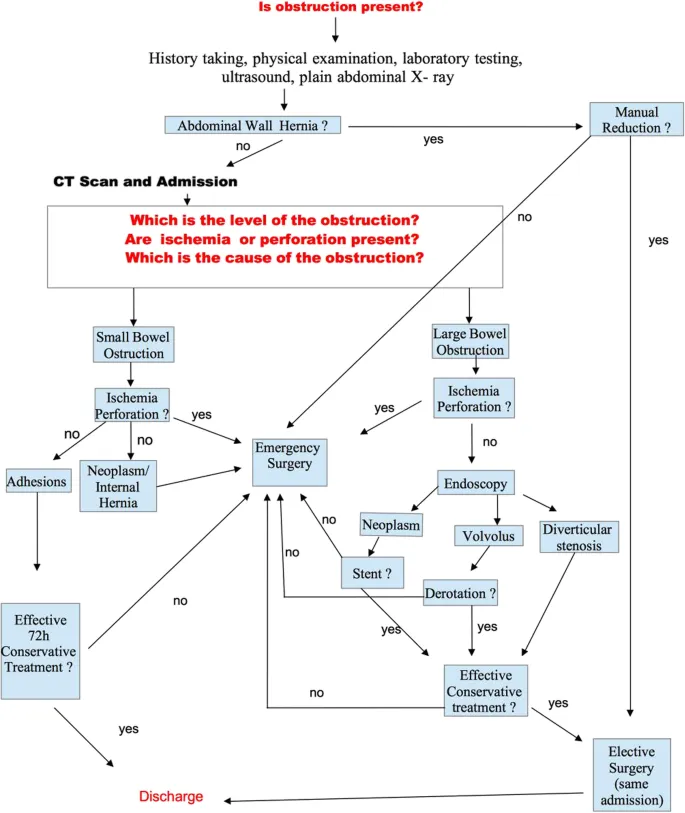
Emergency Recognition Protocols enable rapid identification and appropriate management of oncologic emergencies that require immediate intervention:
- Surgical Emergencies (<6 hours): Perforation, bleeding, obstruction, compartment syndrome
- Urgent Situations (<24 hours): Spinal cord compression, superior vena cava syndrome, tumor lysis syndrome
- Semi-urgent (<72 hours): Hypercalcemia, brain metastases, pleural effusion
💡 Master This: Oncologic emergencies occur in 15-20% of cancer patients. Early recognition and appropriate triage reduce morbidity by 40-60% and mortality by 20-30%.
Quality Metrics Dashboard tracks performance indicators and outcome measures for continuous improvement:
- Process Metrics: Time to treatment, R0 rates, complication rates, length of stay
- Outcome Metrics: Survival rates, functional outcomes, quality of life, patient satisfaction
- Learning Metrics: Case volume, complexity progression, skill acquisition, knowledge updates
🎯 The Oncologic Surgery Mastery Toolkit: Essential Arsenal for Excellence
Practice Questions: Oncologic Surgery Principles
Test your understanding with these related questions
An excisional biopsy is performed and the diagnosis of superficial spreading melanoma is confirmed. The lesion is 1.1 mm thick. Which of the following is the most appropriate next step in management?













