Subdural and epidural hematoma management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Subdural and epidural hematoma management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Subdural and epidural hematoma management US Medical PG Question 1: A previously healthy 10-year-old boy is brought to the emergency department for the evaluation of one episode of vomiting and severe headache since this morning. His mother says he also had difficulty getting dressed on his own. He has not had any trauma. The patient appears nervous. His temperature is 37°C (98.6°F), pulse is 100/min, and blood pressure is 185/125 mm Hg. He is confused and oriented only to person. Ophthalmic examination shows bilateral optic disc swelling. There is an abdominal bruit that is best heard at the right costovertebral angle. A complete blood count is within normal limits. Which of the following is most likely to confirm the diagnosis?
- A. Serum IGF-I level
- B. Oral sodium loading test
- C. Echocardiography
- D. CT angiography (Correct Answer)
- E. High-dose dexamethasone suppression test
Subdural and epidural hematoma management Explanation: ***CT angiography***
- The patient presents with **malignant hypertension** (BP 185/125 mmHg, confusion, optic disc swelling) and an **abdominal bruit** especially at the **right costovertebral angle**, pointing strongly towards **renovascular hypertension** due to **renal artery stenosis**.
- **CT angiography** is the most appropriate imaging modality to confirm **renal artery stenosis** by visualizing the renal arteries and identifying any narrowing.
*Serum IGF-I level*
- This test is used to screen for **growth hormone disorders** like **acromegaly** or **gigantism**, which are not indicated by the patient's symptoms.
- The patient's presentation is focused on acute severe hypertension and neurological changes, rather than chronic growth disturbances.
*Oral sodium loading test*
- This test is used to confirm the diagnosis of **primary aldosteronism**, where **aldosterone levels** fail to suppress after a sodium load.
- While primary aldosteronism can cause hypertension, it typically doesn't present with an **abdominal bruit** or the acute, severe neurological symptoms seen here.
*Echocardiography*
- **Echocardiography** assesses the heart's structure and function, which could show signs of **hypertensive heart disease** (e.g., left ventricular hypertrophy) due to long-standing uncontrolled hypertension.
- However, it does not identify the underlying cause of the hypertension in this acute setting, especially when an **abdominal bruit** suggests a vascular origin.
*High-dose dexamethasone suppression test*
- This test is used to differentiate between **Cushing's disease** (pituitary ACTH-dependent) and other causes of **Cushing's syndrome** (e.g., ectopic ACTH production, adrenal tumor) due to excess cortisol.
- The patient's symptoms are inconsistent with Cushing's syndrome, and the **abdominal bruit** points away from this diagnosis.
Subdural and epidural hematoma management US Medical PG Question 2: A 68-year-old man is brought to the emergency department because of a severe headache, nausea, and vomiting for 30 minutes. Forty-five minutes ago, he fell and struck his head, resulting in loss of consciousness for 1 minute. After regaining consciousness, he felt well for 15 minutes before the headache began. On arrival, the patient becomes rigid and his eyes deviate to the right; he is incontinent of urine. Intravenous lorazepam is administered and the rigidity resolves. Which of the following is the most likely cause of the patient's condition?
- A. Rupture of bridging veins
- B. Cerebrospinal fluid production/absorption mismatch
- C. Acute insufficiency of cerebral blood flow
- D. Bleeding between dura mater and skull (Correct Answer)
- E. Intracerebral hemorrhage
Subdural and epidural hematoma management Explanation: ***Bleeding between dura mater and skull***
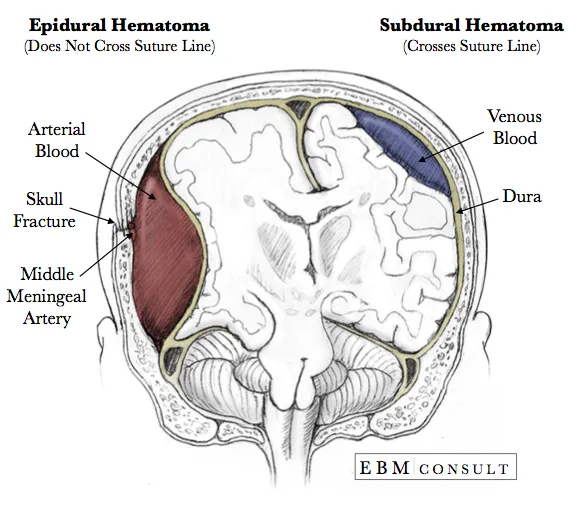
- The classic presentation of an **epidural hematoma** includes a brief **loss of consciousness** followed by a **lucent interval** (patient feeling well) and then rapid neurological deterioration with symptoms like **severe headache**, **nausea**, **vomiting**, and **seizures** due to increasing intracranial pressure.
- This type of bleeding is typically arterial, usually from the **middle meningeal artery**, and occurs between the dura mater and the inner table of the skull.
*Rupture of bridging veins*
- This describes a **subdural hematoma**, which usually results in a more gradual onset of symptoms due to slower venous bleeding, often over days to weeks.
- While a fall can cause it, the rapid deterioration after a lucid interval is less typical for a subdural hematoma.
*Cerebrospinal fluid production/absorption mismatch*
- This mechanism is associated with conditions like **hydrocephalus** or **idiopathic intracranial hypertension**, which typically present with a more gradual onset of symptoms such as chronic headache, visual changes, or gait disturbances.
- It does not account for an acute traumatic event, loss of consciousness, and rapid deterioration seen in this patient.
*Acute insufficiency of cerebral blood flow*
- This typically refers to an **ischemic stroke** or **transient ischemic attack (TIA)**, where symptoms arise from a lack of oxygenated blood to brain regions.
- While it can cause neurological deficits, the history of head trauma, lucid interval, and rapid progression to severe symptoms and seizures points away from a primary ischemic event.
*Intracerebral hemorrhage*
- This involves bleeding within the **brain parenchyma** itself, which can present acutely with headache, vomiting, and neurological deficits.
- However, the distinct **lucid interval** following initial loss of consciousness, as described, is much more characteristic of an **epidural hematoma** rather than bleeding directly into the brain tissue.
Subdural and epidural hematoma management US Medical PG Question 3: A 15-year-old boy is brought to the emergency department one hour after sustaining an injury during football practice. He collided head-on into another player while wearing a mouthguard and helmet. Immediately after the collision he was confused but able to use appropriate words. He opened his eyes spontaneously and followed commands. There was no loss of consciousness. He also had a headache with dizziness and nausea. He is no longer confused upon arrival. He feels well. Vital signs are within normal limits. He is fully alert and oriented. His speech is organized and he is able to perform tasks demonstrating full attention, memory, and balance. Neurological examination shows no abnormalities. There is mild tenderness to palpation over the crown of his head but no signs of skin break or fracture. Which of the following is the most appropriate next step?
- A. Discharge without activity restrictions
- B. Discharge and refrain from all physical activity for one week
- C. Observe for 6 hours in the ED and refrain from contact sports for one week (Correct Answer)
- D. Administer prophylactic levetiracetam and observe for 24 hours
- E. Administer prophylactic phenytoin and observe for 24 hours
Subdural and epidural hematoma management Explanation: ***Observe for 6 hours in the ED and refrain from contact sports for one week***
- This patient experienced a brief period of **confusion, headache, dizziness**, and **nausea** immediately after a head injury, which are symptoms consistent with a **mild traumatic brain injury (mTBI)** or **concussion**.
- Although his symptoms have resolved at presentation, observation in the ED for a few hours is prudent to ensure no delayed onset of more severe symptoms, and he should **refrain from contact sports** for at least one week as part of concussion management.
*Discharge without activity restrictions*
- Discharging without activity restrictions is unsafe given the initial symptoms of **confusion** and the potential for delayed symptom presentation or complications from a concussion.
- Concussion management requires a period of **physical and cognitive rest** to allow the brain to heal and prevent **second impact syndrome**.
*Discharge and refrain from all physical activity for one week*
- While refraining from all physical activity for one week is part of concussion management, discharging immediately without any observation period after initial neurological symptoms could be risky.
- An observation period allows for monitoring of any **worsening neurological signs** or symptoms that might indicate a more serious injury.
*Administer prophylactic levetiracetam and observe for 24 hours*
- **Prophylactic anticonvulsants** like levetiracetam are typically not recommended for routine management of **mild traumatic brain injury** or concussion.
- Their use is generally reserved for patients with more severe injuries, evolving conditions, or those who have had **seizures post-trauma**.
*Administer prophylactic phenytoin and observe for 24 hours*
- Similar to levetiracetam, **phenytoin** is an anticonvulsant and its prophylactic use is not indicated for **mild head injuries** or concussions.
- Anticonvulsant prophylaxis is associated with potential side effects and is reserved for specific high-risk scenarios, such as **severe TBI** or **penetrating head trauma**.
Subdural and epidural hematoma management US Medical PG Question 4: A 60-year-old male is admitted to the ICU for severe hypertension complicated by a headache. The patient has a past medical history of insulin-controlled diabetes, hypertension, and hyperlipidemia. He smokes 2 packs of cigarettes per day. He states that he forgot to take his medications yesterday and started getting a headache about one hour ago. His vitals on admission are the following: blood pressure of 160/110 mmHg, pulse 95/min, temperature 98.6 deg F (37.2 deg C), and respirations 20/min. On exam, the patient has an audible abdominal bruit. After administration of antihypertensive medications, the patient has a blood pressure of 178/120 mmHg. The patient reports his headache has increased to a 10/10 pain level, that he has trouble seeing, and he can't move his extremities. After stabilizing the patient, what is the best next step to diagnose the patient's condition?
- A. Doppler ultrasound of the carotids
- B. CT head with intravenous contrast
- C. MRI head without intravenous contrast
- D. CT head without intravenous contrast (Correct Answer)
- E. MRI head with intravenous contrast
Subdural and epidural hematoma management Explanation: ***CT head without intravenous contrast***
- The sudden onset of severe headache, visual disturbances, and neurological deficits (inability to move extremities), coupled with uncontrolled severe hypertension despite initial treatment, is highly suggestive of an **intracranial pathology**, most likely a **hemorrhagic stroke**.
- A **non-contrast CT scan of the head** is the **gold standard** for rapidly identifying acute intracranial hemorrhage, as it can be performed quickly and is readily available in emergency settings.
*Doppler ultrasound of the carotids*
- This test is primarily used to evaluate **carotid artery stenosis** due to atherosclerosis, which can lead to ischemic stroke.
- While the patient has risk factors for atherosclerosis, his acute presentation with severe central neurological symptoms points more towards an acute intracranial event rather than carotid disease.
*CT head with intravenous contrast*
- While a contrast CT can be useful for identifying tumors, abscesses, or vascular malformations, it is **contraindicated in the initial assessment of acute stroke** if an intracranial hemorrhage is suspected.
- Contrast can sometimes obscure subtle bleeds or complicate the interpretation of acute hemorrhage, and it also carries a risk of **contrast-induced nephropathy**, especially in a patient with diabetes.
*MRI head without intravenous contrast*
- An MRI provides superior soft tissue resolution compared to CT and is excellent for detecting ischemic strokes in later stages, as well as subtle hemorrhages, tumors, and other conditions.
- However, it is **less available, takes longer to perform**, and is often not the first choice in an acute neurological emergency where time is critical, particularly when differentiating between ischemic and hemorrhagic stroke.
*MRI head with intravenous contrast*
- Similar to a contrast CT, an MRI with contrast is generally **not the initial imaging choice for acute stroke** due to time constraints and the need to quickly rule out hemorrhage before considering contrast administration.
- Contrast agents for MRI, such as gadolinium, have their own risks, including **nephrogenic systemic fibrosis** in patients with renal impairment, which is a concern in a diabetic patient.
Subdural and epidural hematoma management US Medical PG Question 5: A 53-year-old man is brought to the emergency department for confusion. He was in his usual state of health until about 3 hours ago when he tried to use his sandwich to turn off the TV. He also complained to his wife that he had a severe headache. Past medical history is notable for hypertension, which has been difficult to control on multiple medications. His temperature is 36.7°C (98°F), the pulse is 70/min, and the blood pressure is 206/132 mm Hg. On physical exam he is alert and oriented only to himself, repeating over and over that his head hurts. The physical exam is otherwise unremarkable and his neurologic exam is nonfocal. The noncontrast CT scan of the patient's head is shown and reveals an acute intraparenchymal hemorrhage in the basal ganglia. Which of the following diagnostic tests would be most helpful in determining the underlying cause of this patient's hemorrhage?
- A. Lumbar puncture
- B. Electroencephalogram (EEG)
- C. MRI of the brain
- D. CT angiography of the neck
- E. CT angiography of the brain (Correct Answer)
Subdural and epidural hematoma management Explanation: ***CT angiography of the brain***
- Following identification of an **intracerebral hemorrhage** on noncontrast CT, **CT angiography (CTA) of the brain** is the most appropriate next diagnostic test to identify underlying vascular abnormalities such as **arteriovenous malformations (AVMs)**, **aneurysms**, **dural arteriovenous fistulas**, or **moyamoya disease**.
- While this patient has severe hypertension (a common cause of basal ganglia hemorrhage), CTA should still be performed to rule out secondary causes, particularly in patients under 70 years old or those with atypical features.
- CTA can be performed rapidly in the acute setting and has high sensitivity for detecting vascular lesions that may require specific treatment.
*MRI of the brain*
- MRI with specialized sequences (GRE, SWI, FLAIR) can provide detailed information about **chronic microhemorrhages**, **cerebral amyloid angiopathy**, **underlying tumors**, or **cavernomas**.
- However, MRI is typically performed **after CTA** in the workup of intracerebral hemorrhage, not as the immediate next step.
- MRI is less readily available in the acute setting and takes longer to perform than CTA.
*CT angiography of the neck*
- This test visualizes the **carotid and vertebral arteries** in the neck to detect **stenosis**, **dissection**, or **atherosclerotic disease**.
- It is not directly useful for identifying the cause of an **intraparenchymal hemorrhage** within the brain substance itself.
*Lumbar puncture*
- Lumbar puncture analyzes **cerebrospinal fluid (CSF)** and is primarily used for suspected **subarachnoid hemorrhage** (when CT is negative), **meningitis**, or **encephalitis**.
- It is **contraindicated** in patients with significant intraparenchymal hemorrhage due to risk of herniation from increased intracranial pressure.
*Electroencephalogram (EEG)*
- EEG measures **electrical activity in the brain** and is used to diagnose **seizure disorders** or evaluate altered mental status from metabolic or epileptic causes.
- While confusion can result from seizures, the primary pathology is the **intracerebral hemorrhage** identified on CT, which EEG cannot diagnose or characterize.
Subdural and epidural hematoma management US Medical PG Question 6: A 2-month-old boy is brought to the emergency room by his mother who reports he has appeared lethargic for the past 3 hours. She reports that she left the patient with a new nanny this morning, and he was behaving normally. When she got home in the afternoon, the patient seemed lethargic and would not breastfeed as usual. At birth, the child had an Apgar score of 8/9 and weighed 2.8 kg (6.1 lb). Growth has been in the 90th percentile, and the patient has been meeting all developmental milestones. There is no significant past medical history, and vaccinations are up-to-date. On physical examination, the patient does not seem arousable. Ophthalmologic examination shows retinal hemorrhages. Which of the following findings would most likely be expected on a noncontrast CT scan of the head?
- A. Lens-shaped hematoma
- B. Cortical atrophy
- C. Crescent-shaped hematoma (Correct Answer)
- D. Blood in the basal cisterns
- E. Multiple cortical and subcortical infarcts
Subdural and epidural hematoma management Explanation: ***Crescent-shaped hematoma***
- The clinical presentation with **lethargy**, a history of being with a **new caregiver**, and **retinal hemorrhages** strongly suggests **abusive head trauma** (shaken baby syndrome).
- This typically results in a **subdural hematoma**, which appears as a **crescent-shaped collection of blood** on a noncontrast CT scan, reflecting bleeding into the potential space between the dura mater and arachnoid mater.
*Lens-shaped hematoma*
- A **lens-shaped (biconvex) hematoma** on CT is characteristic of an **epidural hematoma**, which typically results from a **skull fracture** tearing a meningeal artery.
- While head trauma is present, the specific findings (retinal hemorrhages, lack of skull fracture mention, and mechanism of shaking) are more consistent with subdural rather than epidural bleeding.
*Cortical atrophy*
- **Cortical atrophy** refers to the shrinking of brain tissue and is typically seen in chronic conditions like **neurodegenerative diseases** or **long-standing severe malnutrition**.
- It does not explain the acute onset of lethargy and retinal hemorrhages immediately following a potential traumatic event in an otherwise healthy infant.
*Blood in the basal cisterns*
- **Blood in the basal cisterns** is characteristic of **subarachnoid hemorrhage**, which can be caused by ruptured aneurysms (rare in infants), arteriovenous malformations, or severe trauma.
- While abusive head trauma can sometimes cause subarachnoid bleeding, the primary finding in shaken baby syndrome is usually subdural hemorrhage, and retinal hemorrhages specifically point towards the shearing forces causing subdural bleeding.
*Multiple cortical and subcortical infarcts*
- **Multiple cortical and subcortical infarcts** indicate areas of brain tissue death due to **interrupted blood supply**, as seen in severe stroke or vasculitis.
- This is not the primary or most likely finding in abusive head trauma, though severe head trauma can sometimes lead to secondary ischemic injury due to increased intracranial pressure or vascular disruption.
Subdural and epidural hematoma management US Medical PG Question 7: A 52-year-old woman is accompanied by her husband to the emergency department with a severe occipital headache that started suddenly an hour ago. She is drowsy but able to answer the physician's questions. She describes it as the worst headache she has ever had, 9/10 in intensity. The husband says it was initially localized to the occiput but has now spread all over her head and she also complained of a generalized heaviness. She took an ibuprofen without experiencing any relief. She also complains of blurry vision and nausea and had 1 episode of vomiting. She denies a recent history of fever, chills, numbness, or seizures. Her past medical history is significant for hypertension controlled with lisinopril and metoprolol. On examination, she is drowsy but oriented. Papilledema is seen on ophthalmoscopy. Neck flexion is difficult and painful. The rest of the exam is unremarkable. Her blood pressure is 160/100 mm Hg, heart rate is 100/min, and temperature is 37.0°C (98.6°F). The ECG, cardiac enzymes, and laboratory studies are normal. Lumbar puncture results are as follows:
Opening pressure 210 mm H2O
RBC 50/mm3, numbers steady over 4 test tubes
Cell count 5/mm3
Glucose 60 mg/dL
Proteins 100 mg/dL
The patient is admitted to the ICU for further management. Which of the following is the most likely pathophysiology based on her history and CSF findings?
- A. Rupture of the communicating branches of the cerebral arteries (Correct Answer)
- B. Intracerebral bleed
- C. Viral infection of the brain parenchyma
- D. Bacterial infection of the meninges
- E. Trauma during lumbar puncture
Subdural and epidural hematoma management Explanation: ***Rupture of the communicating branches of the cerebral arteries***
- This presentation, with a **sudden-onset, severe occipital headache ("thunderclap headache")**, meningeal irritation (stiff neck), blurry vision, papilledema, and elevated intracranial pressure (high opening pressure, nausea, vomiting), is highly classic for a **subarachnoid hemorrhage (SAH)**.
- The **CSF findings** of grossly bloody fluid with consistent red blood cells (RBCs) across multiple tubes (indicating true hemorrhage, not traumatic tap), elevated protein, and normal glucose are diagnostic of SAH. The most common cause of spontaneous SAH is the rupture of a **saccular (berry) aneurysm**, frequently found in the communicating branches of cerebral arteries.
*Intracerebral bleed*
- While an intracerebral bleed can cause severe headache and neurological deficits, it typically presents with **focal neurological signs** corresponding to the brain region affected by the hematoma.
- Classic CSF findings in an intracerebral bleed, unless it ruptures into the ventricles or subarachnoid space, would generally be **acellular or mildly pleocytic**, not overtly bloody with high RBC counts.
*Viral infection of the brain parenchyma*
- **Viral encephalitis** would typically present with fever, altered mental status, and often focal neurological deficits or seizures.
- CSF findings for viral encephalitis would show **lymphocytic pleocytosis**, mildly elevated protein, and normal glucose, not significant RBCs.
*Bacterial infection of the meninges*
- **Bacterial meningitis** is characterized by fever, neck stiffness, and altered mental status. The headache is usually progressive, not thunderclap.
- CSF analysis would typically show **neutrophilic pleocytosis**, markedly elevated protein, **low glucose**, and often visible bacteria on gram stain, unlike this patient's findings.
*Trauma during lumbar puncture*
- A **traumatic lumbar puncture** can cause blood in the CSF, but the RBC count would typically **decrease progressively** in subsequent tubes as less contaminated fluid is collected.
- The presence of **xanthochromia** (not explicitly mentioned but usually present in SAH after several hours) and the clinical presentation of a thunderclap headache, papilledema, and meningeal signs prior to the LP make a traumatic tap unlikely as the primary pathology.
Subdural and epidural hematoma management US Medical PG Question 8: A 23-year-old man presents with a blunt force injury to the head from a baseball bat. He is currently unconscious, although his friends say he was awake and speaking with them en route to the hospital. He has no significant past medical history and takes no current medications. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 165/85 mm Hg, pulse 50/min, and respiratory rate 19/min. On physical examination, there is a blunt force injury to the left temporoparietal region approximately 10.1–12.7 cm (4–5 in) in diameter. There is anisocoria of the left pupil, which is unresponsive to light. The patient is intubated and fluid resuscitation is initiated. A noncontrast computed tomography (CT) scan of the head is acquired and shown in the exhibit (see image). Which of the following is the most appropriate medical treatment for this patient?
- A. Placement of a ventriculoperitoneal (VP) shunt
- B. Acetazolamide
- C. Placing the head of the bed at 0 degrees
- D. Maintain a PaCO2 of 24 mm Hg
- E. Mannitol (Correct Answer)
Subdural and epidural hematoma management Explanation: ***Mannitol***
- The patient presents with classic signs of **epidural hematoma** (lucid interval, ipsilateral pupillary dilation, contralateral hemiparesis), and the CT scan confirms a large, biconvex hemorrhage compressing the brain.
- **Mannitol** is an osmotic diuretic used to rapidly **reduce intracranial pressure (ICP)** by drawing water from the brain into the vasculature, which can be life-saving in cases of acute brain herniation.
*Placement of a ventriculoperitoneal (VP) shunt*
- A VP shunt is used for long-term management of **hydrocephalus** due to impaired CSF absorption or flow, not for acute, traumatic hemorrhage and mass effect.
- Placing a shunt would not address the immediate, life-threatening mass effect from the epidural hematoma.
*Acetazolamide*
- **Acetazolamide** is a carbonic anhydrase inhibitor that reduces CSF production, primarily used for conditions like chronic **idiopathic intracranial hypertension** (pseudotumor cerebri) or hydrocephalus.
- It is not an effective treatment for the rapid reduction of ICP in the setting of acute intracranial hemorrhage and mass effect.
*Placing the head of the bed at 0 degrees*
- Keeping the head of the bed flat (at 0 degrees) is generally discouraged in patients with **elevated ICP** as it can worsen cerebral venous outflow and increase ICP.
- Elevating the head of the bed to **30 degrees** is standard practice to promote venous drainage and reduce ICP.
*Maintain a PaCO2 of 24 mm Hg*
- While **hyperventilation** to lower PaCO2 can cause cerebral vasoconstriction and reduce ICP, maintaining a PaCO2 as low as 24 mm Hg (severe hyperventilation) is typically reserved for **brief periods** in severe, refractory ICP elevation.
- Prolonged severe hyperventilation can lead to **cerebral ischemia** due to excessive vasoconstriction and is generally not the first-line or sustained management strategy.
Subdural and epidural hematoma management US Medical PG Question 9: A 77-year-old man is brought to the emergency department by his wife because of headache, nausea, and vomiting for 24 hours. His wife says that over the past 2 weeks, he has been more irritable and has had trouble remembering to do routine errands. Two weeks ago, he fell during a skiing accident but did not lose consciousness. He has coronary artery disease and hypertension. He has smoked one pack of cigarettes daily for 50 years. He has had 2 glasses of wine daily since his retirement 10 years ago. Current medications include atenolol, enalapril, furosemide, atorvastatin, and aspirin. He appears acutely ill. He is oriented to person but not to place or time. His temperature is 37°C (98.6°F), pulse is 99/min, respirations are 16/min, and blood pressure is 160/90 mm Hg. During the examination, he is uncooperative and unable to answer questions. Deep tendon reflexes are 4+ on the left and 2+ on the right. Babinski's sign is present on the left. There is mild weakness of the left iliopsoas and hamstring muscles. A CT scan of the head without contrast shows a high-density, 15-mm crescentic collection across the right hemispheric convexity. Which of the following is the most appropriate next step in the management of this patient?
- A. Recombinant tissue plasminogen activator administration
- B. Obtain an Electroencephalography
- C. Obtain an MRI of the head
- D. Surgical evacuation (Correct Answer)
- E. Observation
Subdural and epidural hematoma management Explanation: ***Surgical evacuation***
- The CT scan reveals a **high-density, crescentic collection**, strongly indicative of an **acute subdural hematoma**, which is causing significant neurological deficits and mass effect (e.g., increased intracranial pressure symptoms like headache, nausea, vomiting, and altered mental status, and focal neurological signs).
- Given the patient's **acute neurological decline**, significant mass effect from the 15-mm hematoma, and age, prompt **surgical evacuation** is the definitive treatment to relieve pressure and prevent further brain injury.
*Recombinant tissue plasminogen activator administration*
- **tPA** is indicated for **acute ischemic stroke**, not hemorrhagic stroke or subdural hematoma. Administering tPA in this context would be harmful, potentially worsening the hemorrhage.
- The patient's CT scan clearly shows a **hemorrhagic lesion**, not an ischemic event.
*Obtain an Electroencephalography*
- **EEG** is primarily used to evaluate **seizure disorders** or certain types of encephalopathy. While the patient has altered mental status, the primary issue identified on CT is a subdural hematoma requiring immediate intervention.
- EEG would not provide information relevant to the immediate management of an **acute subdural hematoma**.
*Obtain an MRI of the head*
- An **MRI** can provide more detailed imaging, but in the context of an **acute subdural hematoma** with significant neurological compromise, it would delay crucial and time-sensitive surgical intervention.
- The **CT scan** has already provided sufficient diagnostic information to warrant immediate surgical planning.
*Observation*
- **Observation** is not appropriate for a patient with a rapidly expanding **acute subdural hematoma** causing significant neurological deficits and a 15-mm collection, especially given the patient's age and clinical presentation.
- Delaying treatment would likely lead to further neurological deterioration, **herniation**, and potentially death.
Subdural and epidural hematoma management US Medical PG Question 10: A 47-year-old man is admitted to the emergency room after a fight in which he was hit in the head with a hammer. The witnesses say that the patient initially lost consciousness, but regained consciousness by the time emergency services arrived. On admission, the patient complained of a diffuse headache. He opened his eyes spontaneously, was verbally responsive, albeit confused, and was able to follow commands. He could not elevate his left hand and leg. He did not remember the events prior to the loss of consciousness and had difficulty remembering information, such as the names of nurses or doctors. His airway was not compromised. The vital signs are as follows: blood pressure, 180/100 mm Hg; heart rate, 59/min; respiratory rate, 12/min; temperature 37.0℃ (98.6℉); and SaO2, 96% on room air. The examination revealed bruising in the right frontotemporal region. The pupils are round, equal, and show a poor response to light. The neurologic examination shows hyperreflexia and decreased power in the left upper and lower limbs. There is questionable nuchal rigidity, but no Kernig and Brudzinski signs. The CT scan is shown in the image. Which of the following options is recommended for this patient?
- A. Lumbar puncture
- B. Decompressive craniectomy
- C. Administration of levetiracetam
- D. Administration of methylprednisolone
- E. Surgical evacuation of the clots (Correct Answer)
Subdural and epidural hematoma management Explanation: ***Surgical evacuation of the clots***
- The CT scan image shows a **biconvex (lenticular) hyperdensity** consistent with an **epidural hematoma (EDH)**, which typically results from arterial bleeding (often from the **middle meningeal artery**). This patient's **"lucid interval"** (initial loss of consciousness, regain consciousness, then deterioration) is classic for EDH.
- Given the patient's neurological deterioration (left-sided weakness, pupillary changes, confusion, memory issues) and signs of increased intracranial pressure (hypertension, bradycardia - part of Cushing's triad), urgent surgical evacuation of the hematoma is indicated to relieve pressure and prevent herniation.
*Lumbar puncture*
- A lumbar puncture is **contraindicated** in the setting of suspected or confirmed **increased intracranial pressure (ICP)**, as it can precipitate **cerebral herniation**.
- The CT scan clearly demonstrates a space-occupying lesion, making a lumbar puncture unnecessary and potentially dangerous.
*Decompressive craniectomy*
- While decompressive craniectomy is a neurosurgical procedure used to reduce ICP, it is generally considered when other measures have failed or in cases of **diffuse brain swelling** or large **intracerebral hematomas** not amenable to simple evacuation.
- In this case of a localized epidural hematoma with a clear surgical target, direct evacuation is the primary and most effective intervention.
*Administration of levetiracetam*
- Levetiracetam is an **anticonvulsant** used to prevent seizures. While seizures can occur after traumatic brain injury, there is no indication that the patient is currently seizing.
- Prophylactic anticonvulsants are sometimes used in severe TBI, but addressing the life-threatening hematoma takes **precedence** over seizure prophylaxis.
*Administration of methylprednisolone*
- **Corticosteroids** like methylprednisolone are generally **contraindicated** in traumatic brain injury (TBI) as studies have shown **worse outcomes** and increased mortality.
- They are primarily used for their **anti-inflammatory effects** in conditions like spinal cord injury or vasogenic edema from tumors, not for acute head trauma with hematoma.
More Subdural and epidural hematoma management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.