Stereotactic procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Stereotactic procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Stereotactic procedures US Medical PG Question 1: A 50-year-old man comes to the physician because of gradually worsening rhythmic movements of his right hand for the past 5 months. His symptoms worsen when he is in a meeting and he is concerned that people are noticing it more frequently. There is no personal or family history of serious illness, but the patient recalls that his father developed bobbing of the head in older age. He takes no medications. Neurological examination shows a tremor of the right hand when the limbs are relaxed. When the patient is asked to move his arm the tremor decreases. He has reduced arm swing while walking. Which of the following is the most appropriate pharmacotherapy?
- A. Trihexyphenidyl
- B. Propranolol
- C. Clonazepam
- D. Donepezil
- E. Levodopa/carbidopa (Correct Answer)
Stereotactic procedures Explanation: ***Levodopa/carbidopa***
- The patient's symptoms (gradually worsening rhythmic movements, **resting tremor** which improves with action, reduced arm swing, and possible family history of head bobbing/tremor) are highly suggestive of **Parkinson's disease**.
- **Levodopa/carbidopa** is the most effective medication for symptomatic treatment of Parkinson's disease, particularly for motor symptoms like tremor, bradykinesia, and rigidity.
*Trihexyphenidyl*
- This is an **anticholinergic** medication that can be used to treat tremor in Parkinson's disease, but it is generally less effective than levodopa and has more side effects, especially in older patients (e.g., confusion, dry mouth, blurred vision).
- It is typically considered for younger patients with prominent tremor rather than older individuals or those with a broader range of motor symptoms.
*Propranolol*
- **Propranolol** is a beta-blocker primarily used to treat **essential tremor**, a condition characterized by an action or postural tremor that improves with alcohol and often has a strong family history.
- The patient's tremor is a **resting tremor** that decreases with action, making essential tremor less likely.
*Clonazepam*
- **Clonazepam** is a benzodiazepine that is used to treat various conditions, including anxiety, seizures, and some movement disorders (e.g., restless legs syndrome, clonus).
- It is not a primary treatment for Parkinson's disease tremor and would not address the other motor symptoms like reduced arm swing.
*Donepezil*
- **Donepezil** is an **acetylcholinesterase inhibitor** used to treat the cognitive symptoms of Alzheimer's disease and other dementias.
- It has no role in the treatment of the motor symptoms of Parkinson's disease.
Stereotactic procedures US Medical PG Question 2: A 48-year-old man presents to the ER with a sudden-onset, severe headache. He is vomiting and appears confused. His wife, who accompanied him, says that he has not had any trauma, and that the patient has no relevant family history. He undergoes a non-contrast head CT that shows blood between the arachnoid and pia mater. What is the most likely complication from this condition?
- A. Hemorrhagic shock
- B. Arterial Vasospasm (Correct Answer)
- C. Renal failure
- D. Bacterial Meningitis
- E. Blindness
Stereotactic procedures Explanation: **Arterial Vasospasm**
- **Arterial vasospasm** is a major delayed complication of **subarachnoid hemorrhage (SAH)**, typically occurring 3-14 days after the initial bleed.
- The presence of blood products in the subarachnoid space can irritate cerebral arteries, leading to their narrowing and subsequent **delayed cerebral ischemia** or infarction.
*Hemorrhagic shock*
- **Subarachnoid hemorrhage (SAH)** typically involves bleeding within the confines of the skull, which is usually not extensive enough to cause systemic **hypovolemia** or **hemorrhagic shock**.
- **Hemorrhagic shock** would require significant external blood loss or internal bleeding into a large body cavity, which is not characteristic of an isolated SAH.
*Renal failure*
- **Renal failure** is not a direct or common complication of **subarachnoid hemorrhage (SAH)**.
- While systemic complications can sometimes arise in critically ill patients, there is no direct pathophysiological link between SAH and primary kidney injury.
*Bacterial Meningitis*
- The presence of blood in the **subarachnoid space** can cause a **chemical meningitis** due to irritation, mimicking some symptoms of bacterial meningitis.
- However, it does not typically predispose to **bacterial infection** unless there's an iatrogenic cause (e.g., lumbar puncture contamination).
*Blindness*
- While damage to the **optic nerves** or visual pathways can occur with severe neurological events or increased intracranial pressure, **blindness** is not a common or direct complication specifically arising from the bleed itself or its immediate sequelae in SAH.
- Visual disturbances are possible due to elevated **intracranial pressure** or specific anatomical lesion, but not primary blindness.
Stereotactic procedures US Medical PG Question 3: A 78-year-old man is brought in to the emergency department by ambulance after his wife noticed that he began slurring his speech and had developed facial asymmetry during dinner approximately 30 minutes ago. His past medical history is remarkable for hypertension and diabetes. His temperature is 99.1°F (37.3°C), blood pressure is 154/99 mmHg, pulse is 89/min, respirations are 12/min, and oxygen saturation is 98% on room air. Neurologic exam reveals right upper and lower extremity weakness and an asymmetric smile. Which of the following is the next best step in management?
- A. Alteplase
- B. MRI brain
- C. CT head (Correct Answer)
- D. Aspirin
- E. CTA head
Stereotactic procedures Explanation: ***CT head***
- A **non-contrast CT head** is the immediate priority to differentiate between ischemic and hemorrhagic stroke, which is critical for guiding subsequent treatment decisions.
- Given the patient's acute neurological deficits (slurred speech, facial asymmetry, weakness) and vascular risk factors (hypertension, diabetes), **stroke is highly suspected**, and identifying intracerebral hemorrhage is crucial before considering thrombolytic therapy.
*Alteplase*
- **Alteplase** (tPA) is a thrombolytic agent used for acute ischemic stroke, but its administration is **contraindicated in hemorrhagic stroke**.
- Initiating alteplase without first ruling out hemorrhage with a CT scan could lead to catastrophic bleeding.
*MRI brain*
- While an **MRI brain** can provide more detailed imaging of stroke, it is typically **not the initial imaging modality** in the emergency setting due to longer acquisition times and limited availability, especially when emergent differentiation between ischemic and hemorrhagic stroke is needed.
- Its use is usually reserved for cases where the CT is inconclusive or for later evaluation.
*Aspirin*
- **Aspirin** is an antiplatelet agent used in the management of ischemic stroke, but it should **not be given until a hemorrhagic stroke has been ruled out** via CT head.
- Administering aspirin in the context of an intracerebral hemorrhage could worsen bleeding.
*CTA head*
- A **CT angiography (CTA) head** is used to visualize the cerebral vasculature and identify large vessel occlusions, which can guide thrombectomy decisions in ischemic stroke.
- However, performing a **non-contrast CT head is a prerequisite** to rule out hemorrhage before proceeding with CTA or any other advanced imaging or therapeutic interventions.
Stereotactic procedures US Medical PG Question 4: A 62-year-old man is brought to the emergency department by his wife because she thinks he has had a stroke. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He has smoked 1 pack of cigarettes per day for the past 35 years. His blood pressure is 162/95 mm Hg. A CT scan of the brain shows a lacunar stroke involving the left subthalamic nucleus. The patient most likely presented with which of the following findings on physical examination?
- A. Cogwheel rigidity
- B. Dystonia
- C. Hemispatial agnosia
- D. Vertical gaze palsy
- E. Hemiballismus (Correct Answer)
Stereotactic procedures Explanation: ***Hemiballismus***
- A lacunar stroke in the **subthalamic nucleus (STN)** typically causes **hemiballismus**, which is characterized by wild, involuntary, large-amplitude flinging movements on one side of the body.
- The STN is part of the **basal ganglia circuit** and its damage leads to disinhibition of the thalamus, resulting in hyperkinetic movements.
*Cogwheel rigidity*
- This is a feature of **Parkinson's disease**, resulting from damage to the **substantia nigra** affecting dopamine production, not typically a direct result of a lacunar stroke in the subthalamic nucleus.
- It is characterized by a jerky resistance to passive movement in a limb.
*Dystonia*
- Characterized by sustained or repetitive muscle contractions resulting in **twisting and repetitive movements** or abnormal fixed postures.
- While basal ganglia dysfunction can cause dystonia, it's a broader term, and **hemiballismus** is a more specific and classic presentation of STN lesions.
*Hemispatial agnosia*
- Refers to a deficit in attention to one side of space, most commonly associated with lesions in the **non-dominant (right) parietal lobe**.
- This is distinct from the motor symptoms expected from a subthalamic nucleus lesion.
*Vertical gaze palsy*
- Commonly associated with lesions in the **midbrain**, particularly the **dorsal midbrain syndrome (Parinaud syndrome)**.
- This is not a typical presentation of a lacunar stroke specifically involving the subthalamic nucleus.
Stereotactic procedures US Medical PG Question 5: A 26-year-old man is brought to the emergency department by ambulance after being involved in a motor vehicle collision. He does not open his eyes on command or respond to verbal cues. A CT scan of the head shows a hyperdense fluid collection in the right medial temporal lobe with medial displacement of the uncus and parahippocampal gyrus of the temporal lobe. Which of the following cranial nerves is most likely to be injured as a result of this patient's lesion?
- A. Vagus
- B. Facial
- C. Oculomotor (Correct Answer)
- D. Abducens
- E. Trigeminal
Stereotactic procedures Explanation: ***Oculomotor***
- The description of **medial displacement of the uncus and parahippocampal gyrus** (uncus herniation) compresses the **oculomotor nerve (CN III)** as it passes between the posterior cerebral and superior cerebellar arteries.
- Compression of the oculomotor nerve leads to a **dilated pupil** (due to parasympathetic fiber involvement) and **down-and-out deviation of the eye** (due to paralysis of extraocular muscles it innervates).
*Vagus*
- The vagus nerve (CN X) is deep within the skull and brainstem, far from the temporal lobe, and is not directly affected by uncal herniation.
- Injury to the vagus nerve typically presents with dysphagia, hoarseness, or cardiac arrhythmias, symptoms not indicated here.
*Facial*
- The facial nerve (CN VII) exits the brainstem at the pontomedullary junction and is located more superiorly and laterally than the structures involved in uncal herniation.
- Damage to the facial nerve causes facial muscle weakness or paralysis, which is not the primary concern with uncal herniation.
*Abducens*
- The abducens nerve (CN VI) is a long, slender nerve that can be affected by **generalized increases in intracranial pressure**, but is less commonly directly compressed by an uncal herniation itself.
- Injury to the abducens nerve causes **lateral rectus muscle paralysis**, leading to medial deviation of the eye, whereas uncal herniation typically affects the oculomotor nerve.
*Trigeminal*
- The trigeminal nerve (CN V) exits the pons and is located superior to the tentorial notch and medial temporal lobe, making it unlikely to be directly compressed by uncal herniation.
- Injury to the trigeminal nerve causes sensory loss in the face or weakness of the muscles of mastication, which are not consistent with the described lesion.
Stereotactic procedures US Medical PG Question 6: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Stereotactic procedures Explanation: ***Mesolimbic pathway***
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Stereotactic procedures US Medical PG Question 7: A 76-year-old man is brought to his geriatrician by his daughter, who reports that he has been "losing his memory." While the patient previously performed all household duties by himself, he has recently had several bills that were unpaid. He also called his daughter on several occasions after getting lost while driving and having "accidents" before getting to the toilet. On exam, the patient is conversant and alert to person, place, and time, though his gait is wide-based and slow. Which of the following diagnostic procedures would be most appropriate to confirm the suspected diagnosis in this patient?
- A. Warfarin
- B. Donepezil
- C. Carbidopa/Levodopa
- D. Memantine
- E. Lumbar puncture (Correct Answer)
Stereotactic procedures Explanation: ***Lumbar puncture***
- The patient's symptoms of **cognitive decline**, **gait disturbance**, and **urinary incontinence** (losing control before reaching the toilet) represent the classic triad of **Normal Pressure Hydrocephalus (NPH)**.
- **Lumbar puncture** with removal of CSF (30-50 mL) serves as both a **diagnostic and therapeutic test** (tap test); transient improvement in symptoms, especially gait, strongly supports the diagnosis of NPH.
- This is the only **diagnostic procedure** among the options; the others are medications/treatments.
*Warfarin*
- This is an **anticoagulant medication** (not a diagnostic procedure) used to prevent blood clots in atrial fibrillation or venous thromboembolism.
- Has no role in diagnosing or treating NPH, which involves CSF dynamics, not coagulation.
*Donepezil*
- **Donepezil** is an **acetylcholinesterase inhibitor medication** (not a diagnostic procedure) used to treat Alzheimer's disease symptoms.
- While the patient has cognitive decline, the classic NPH triad (cognitive, gait, incontinence) distinguishes this from typical Alzheimer's dementia.
- This is a treatment option, not a diagnostic test.
*Carbidopa/Levodopa*
- This **medication combination** (not a diagnostic procedure) is the primary treatment for **Parkinson's disease**, replacing dopamine.
- While Parkinson's causes gait issues, it doesn't typically present with this specific triad, and parkinsonian gait differs from NPH's magnetic/apraxic gait.
- This is a treatment, not a diagnostic procedure.
*Memantine*
- **Memantine** is an **NMDA receptor antagonist medication** (not a diagnostic procedure) used in moderate to severe Alzheimer's disease.
- Like donepezil, this treats dementia symptoms but is not a diagnostic test for NPH.
Stereotactic procedures US Medical PG Question 8: A 58-year-old woman is brought to the emergency department for shortness of breath and chest pain. Pulmonary angiography shows a large saddle embolus in the pulmonary arteries. Emergency drug therapy is administered and she is admitted to the hospital for observation. A follow-up CT scan of the chest shortly after admission shows that the thrombus has disappeared. Five hours later, the patient is found to be lethargic with slurred speech. Physical examination shows decreased consciousness, dysarthria, and optic disc swelling bilaterally. Which of the following is the most likely cause of her neurological symptoms?
- A. Acute metabolic encephalopathy
- B. Embolic cerebrovascular accident
- C. Idiopathic intracranial hypertension
- D. Intracerebral hemorrhage (Correct Answer)
- E. Drug-induced hypotension
Stereotactic procedures Explanation: ***Intracerebral hemorrhage***
- The patient was treated for a **saddle pulmonary embolism** with drug therapy (likely thrombolytics). This type of therapy carries a significant risk of **intracerebral hemorrhage**, especially in older patients or those with underlying risks. The sudden onset of neurological symptoms, including decreased consciousness, dysarthria, and **bilateral optic disc swelling** (indicating increased intracranial pressure), five hours after receiving thrombolytic therapy, is highly suspicious for a hemorrhagic stroke.
- The rapid dissolution of the pulmonary thrombus followed by new neurological deficits strongly suggests a side effect of aggressive anticoagulation or thrombolysis.
*Acute metabolic encephalopathy*
- While metabolic encephalopathy can cause decreased consciousness and lethargy, it typically does not present with focal neurological signs like **dysarthria** or **optic disc swelling** indicating increased intracranial pressure.
- The rapid onset immediately following thrombolytic treatment for a significant thromboembolic event points away from a primary metabolic cause.
*Embolic cerebrovascular accident*
- An embolic stroke could cause similar neurological symptoms, but the history of massive thrombolysis for a pulmonary embolism makes **hemorrhage** a more immediate concern given the treatment. Additionally, an embolic stroke would not typically cause **bilateral optic disc swelling** so rapidly.
- While theoretically possible if a paradoxical embolism occurred (e.g., via a patent foramen ovale), the administration of powerful anticoagulants/thrombolytics makes hemorrhage the more probable complication.
*Idiopathic intracranial hypertension*
- This condition is characterized by **increased intracranial pressure without an identifiable cause** and primarily affects young, obese women. It typically presents with chronic headaches and visual disturbances, but rarely acute neurological deterioration with decreased consciousness or dysarthria.
- The acute, post-treatment onset of symptoms is inconsistent with the chronic nature of idiopathic intracranial hypertension.
*Drug-induced hypotension*
- Severe hypotension could lead to global cerebral hypoperfusion and altered mental status, but it usually causes more generalized symptoms, and is less likely to produce focal neurological signs like **dysarthria** or **bilateral optic disc swelling** within such a short timeframe as the primary cause.
- While hypotension can be a side effect of some drugs, the specific constellation of symptoms, particularly the optic disc swelling, points more directly towards an acute intracranial event like hemorrhage.
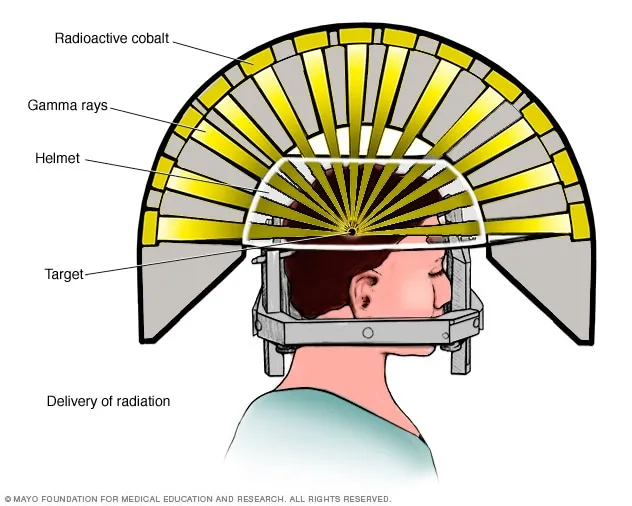
Stereotactic procedures US Medical PG Question 9: The patient is admitted to the hospital. A stereotactic brain biopsy of the suspicious lesion is performed that shows many large lymphocytes with irregular nuclei. Which of the following is the most appropriate treatment?
- A. Methotrexate (Correct Answer)
- B. Pyrimethamine and sulfadiazine
- C. Intrathecal glucocorticoids
- D. Surgical resection
- E. Temozolomide
Stereotactic procedures Explanation: ***Methotrexate***
- A brain biopsy showing **large lymphocytes with irregular nuclei** is highly suggestive of **primary central nervous system lymphoma (PCNSL)**. High-dose methotrexate is the cornerstone of PCNSL treatment due to its ability to cross the **blood-brain barrier** effectively.
- Methotrexate is a **folate antagonist** that inhibits DNA synthesis, making it effective against rapidly dividing cancer cells, including lymphoma cells in the brain.
*Pyrimethamine and sulfadiazine*
- This combination is the standard treatment for **cerebral toxoplasmosis**, an opportunistic infection often seen in immunocompromised patients, which can present as a brain lesion.
- However, the biopsy finding of **lymphoma cells** rules out toxoplasmosis as the primary diagnosis, making this treatment inappropriate.
*Intrathecal glucocorticoids*
- **Glucocorticoids** can be used to reduce **peritumoral edema** and provide symptomatic relief in PCNSL, but they are not a definitive treatment for the lymphoma itself.
- While sometimes used as an adjunct, high-dose glucocorticoids can induce **lymphoma cell apoptosis**, potentially confounding diagnostic biopsy results if administered before the biopsy.
*Surgical resection*
- **Gross total resection** is generally not feasible or recommended for PCNSL because these tumors tend to be multifocal and deeply infiltrating, making complete removal difficult and often associated with significant neurological morbidity.
- The primary treatment for PCNSL is **chemotherapy** (especially high-dose methotrexate) and sometimes radiation, rather than surgery.
*Temozolomide*
- **Temozolomide** is an **oral alkylating agent** primarily used in the treatment of **glioblastoma multiforme** and anaplastic astrocytoma, as well as other high-grade gliomas.
- While it can cross the blood-brain barrier, it is not the primary or most effective chemotherapy for PCNSL, which responds better to methotrexate-based regimens.
Stereotactic procedures US Medical PG Question 10: A 77-year-old man is brought to the emergency department by his wife because of headache, nausea, and vomiting for 24 hours. His wife says that over the past 2 weeks, he has been more irritable and has had trouble remembering to do routine errands. Two weeks ago, he fell during a skiing accident but did not lose consciousness. He has coronary artery disease and hypertension. He has smoked one pack of cigarettes daily for 50 years. He has had 2 glasses of wine daily since his retirement 10 years ago. Current medications include atenolol, enalapril, furosemide, atorvastatin, and aspirin. He appears acutely ill. He is oriented to person but not to place or time. His temperature is 37°C (98.6°F), pulse is 99/min, respirations are 16/min, and blood pressure is 160/90 mm Hg. During the examination, he is uncooperative and unable to answer questions. Deep tendon reflexes are 4+ on the left and 2+ on the right. Babinski's sign is present on the left. There is mild weakness of the left iliopsoas and hamstring muscles. A CT scan of the head without contrast shows a high-density, 15-mm crescentic collection across the right hemispheric convexity. Which of the following is the most appropriate next step in the management of this patient?
- A. Recombinant tissue plasminogen activator administration
- B. Obtain an Electroencephalography
- C. Obtain an MRI of the head
- D. Surgical evacuation (Correct Answer)
- E. Observation
Stereotactic procedures Explanation: ***Surgical evacuation***
- The CT scan reveals a **high-density, crescentic collection**, strongly indicative of an **acute subdural hematoma**, which is causing significant neurological deficits and mass effect (e.g., increased intracranial pressure symptoms like headache, nausea, vomiting, and altered mental status, and focal neurological signs).
- Given the patient's **acute neurological decline**, significant mass effect from the 15-mm hematoma, and age, prompt **surgical evacuation** is the definitive treatment to relieve pressure and prevent further brain injury.
*Recombinant tissue plasminogen activator administration*
- **tPA** is indicated for **acute ischemic stroke**, not hemorrhagic stroke or subdural hematoma. Administering tPA in this context would be harmful, potentially worsening the hemorrhage.
- The patient's CT scan clearly shows a **hemorrhagic lesion**, not an ischemic event.
*Obtain an Electroencephalography*
- **EEG** is primarily used to evaluate **seizure disorders** or certain types of encephalopathy. While the patient has altered mental status, the primary issue identified on CT is a subdural hematoma requiring immediate intervention.
- EEG would not provide information relevant to the immediate management of an **acute subdural hematoma**.
*Obtain an MRI of the head*
- An **MRI** can provide more detailed imaging, but in the context of an **acute subdural hematoma** with significant neurological compromise, it would delay crucial and time-sensitive surgical intervention.
- The **CT scan** has already provided sufficient diagnostic information to warrant immediate surgical planning.
*Observation*
- **Observation** is not appropriate for a patient with a rapidly expanding **acute subdural hematoma** causing significant neurological deficits and a 15-mm collection, especially given the patient's age and clinical presentation.
- Delaying treatment would likely lead to further neurological deterioration, **herniation**, and potentially death.
More Stereotactic procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.