Spinal surgery fundamentals US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Spinal surgery fundamentals. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Spinal surgery fundamentals US Medical PG Question 1: A 65-year-old woman comes to the physician for the evaluation of sharp, stabbing pain in the lower back for 3 weeks. The pain radiates to the back of her right leg and is worse at night. She reports decreased sensation around her buttocks and inner thighs. During the last several days, she has had trouble urinating. Three years ago, she was diagnosed with breast cancer and was treated with lumpectomy and radiation. Her only medication is anastrozole. Her temperature is 37°C (98.6°F), pulse is 80/min, respirations are 12/min, and blood pressure is 130/70 mm Hg. Neurologic examination shows 4/5 strength in the left lower extremity and 2/5 strength in her right lower extremity. Knee and ankle reflexes are 1+ on the right. The resting anal sphincter tone is normal but the squeeze tone is reduced. Which of the following is the most likely diagnosis?
- A. Anterior spinal cord syndrome
- B. Cauda equina syndrome (Correct Answer)
- C. Conus medullaris syndrome
- D. Central cord syndrome
- E. Brown-sequard syndrome
Spinal surgery fundamentals Explanation: ***Cauda equina syndrome***
- The patient's presentation with **severe low back pain**, **saddle anesthesia** (decreased sensation around buttocks and inner thighs), **bladder dysfunction** (trouble urinating), and **motor weakness** in the lower extremities is highly indicative of cauda equina syndrome. This can be caused by **spinal metastases** from her breast cancer.
- The **reduced squeeze tone** of the anal sphincter, despite normal resting tone, further supports the diagnosis, indicating dysfunction of the sacral nerve roots which are compressed in cauda equina syndrome.
*Anterior spinal cord syndrome*
- This syndrome typically presents with **motor paralysis**, loss of **pain** and **temperature** sensation below the lesion, but preservation of **proprioception** and **vibration sense**.
- It does not typically cause **saddle anesthesia** or **bladder dysfunction** to the extent seen in this patient.
*Conus medullaris syndrome*
- Conus medullaris syndrome involves the lower part of the spinal cord (T12-L2) and typically presents with **symmetric motor weakness**, **early onset bladder and bowel dysfunction**, and often **perianal numbness**.
- While there is bladder dysfunction, the described **asymmetric weakness** and prominent **radicular pain** radiating down one leg are more characteristic of cauda equina syndrome, which affects nerve roots rather than the spinal cord itself.
*Central cord syndrome*
- This syndrome usually results from hyperextension injuries and leads to **greater motor impairment in the upper extremities** than in the lower extremities.
- It is often associated with a **'shawl-like' distribution** of sensory loss and does not typically present with the same severe lower extremity weakness, saddle anesthesia, or bladder dysfunction as seen in this patient.
*Brown-Sequard syndrome*
- This syndrome is characterized by **hemisection of the spinal cord**, resulting in **ipsilateral motor paralysis** and loss of **proprioception and vibration sensation** below the level of the lesion.
- It also causes **contralateral loss of pain and temperature sensation** starting a few segments below the lesion, which does not match the patient's symptoms of bilateral sensory and motor deficits with saddle anesthesia.
Spinal surgery fundamentals US Medical PG Question 2: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Spinal surgery fundamentals Explanation: ***Prions***
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
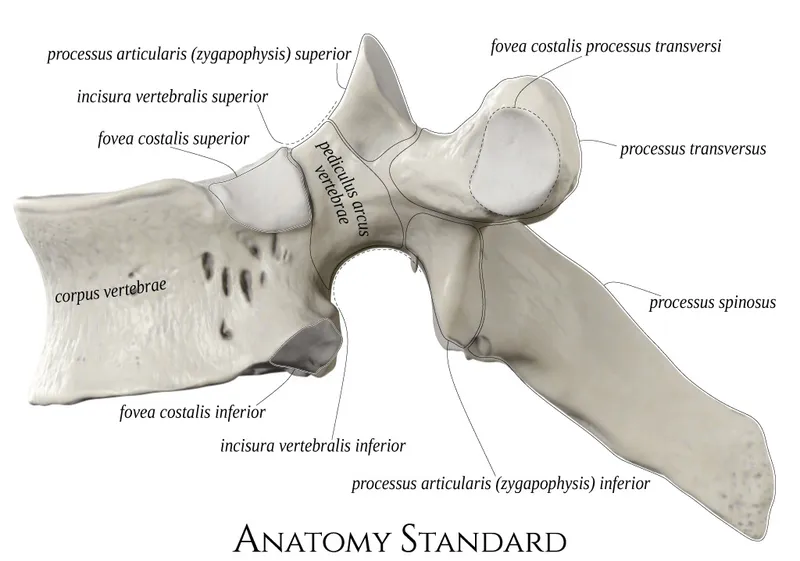
Spinal surgery fundamentals US Medical PG Question 3: A 65-year-old woman with osteoarthritis comes to the physician because of severe lower back and left leg pain. She has chronic lower back pain that is usually well-controlled with ibuprofen, but 3 hours ago her back pain acutely worsened after she picked up her 3-year-old granddaughter. The pain radiates from her lower back over her left outer thigh and knee towards the top of her big toe. Physical examination shows a diminished Achilles reflex on the left side. Muscle strength is 5/5 in all extremities and there are no sensory deficits. Steroid injection into which of the following anatomical locations is most likely to relieve her symptoms?
- A. Subarachnoid space
- B. Inferior facet joint
- C. Intervertebral disc
- D. Intervertebral foramen (Correct Answer)
- E. Subdural space
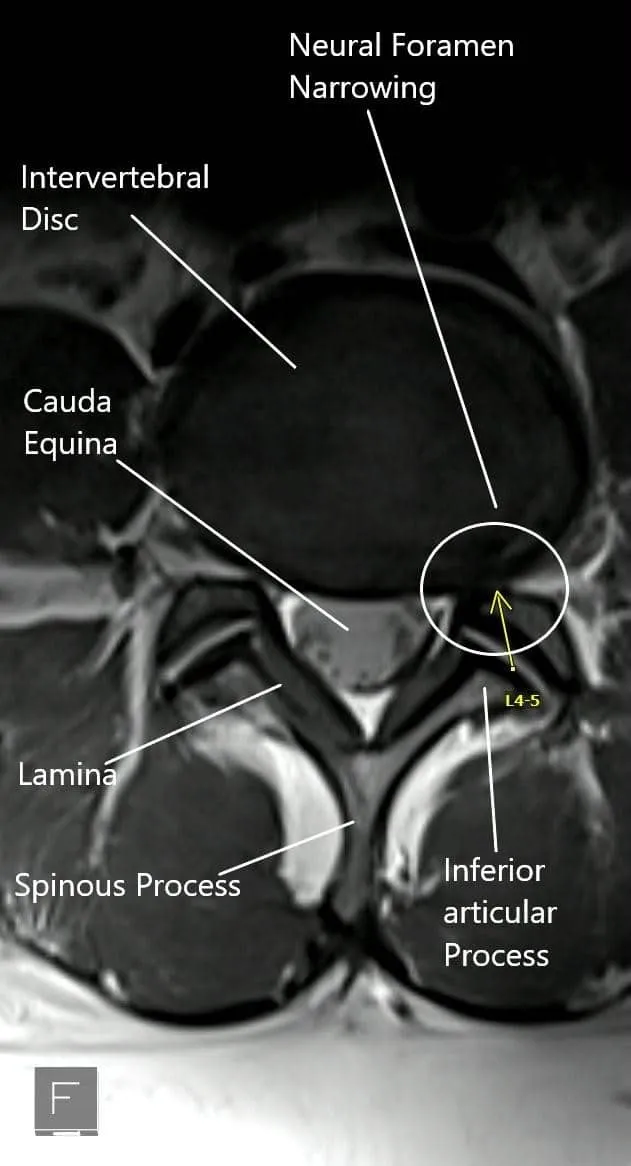
Spinal surgery fundamentals Explanation: ***Intervertebral foramen***
- The patient's symptoms, including **radiating lower back and left leg pain** with a diminished **posterior tibial reflex**, are classic for **radiculopathy** due to **spinal nerve root compression**.
- Steroid injection into the intervertebral foramen, where the **nerve root exits the spinal canal**, is directly targeting the site of inflammation and compression, thus being most likely to relieve symptoms.
*Subarachnoid space*
- An injection into the **subarachnoid space** (intrathecal injection) is typically used for **spinal anesthesia** or to administer medications for widespread CNS conditions, not focal nerve root compression.
- While it contains CSF and nerve roots, it is not the most precise or appropriate location for an injection aimed at isolated radicular pain.
*Inferior facet joint*
- The **facet joints** are involved in **axial back pain**, usually worse with extension, and do not typically cause radicular symptoms radiating down the leg to the big toe with a specific dermatomal and myotomal distribution like L5 or S1.
- An injection here would target facet joint arthritis, which presents differently from the described radiculopathy.
*Intervertebral disc*
- An injection into the **intervertebral disc** (discography or disc annuloplasty) is generally a diagnostic procedure to identify pain originating from the disc or a treatment for discogenic pain, which is usually axial and not radicular.
- Injecting steroids directly into the disc is not a standard treatment for nerve root compression.
*Subdural space*
- The **subdural space** is a potential space between the dura mater and arachnoid mater; injections into this space are rarely performed therapeutically and carry significant risks without clear benefit for radiculopathy.
- An inadvertent subdural injection during an epidural procedure can lead to complications such as a **subdural hematoma** or paralysis.
Spinal surgery fundamentals US Medical PG Question 4: A 36-year-old man is seen in the emergency department for back pain that has been getting progressively worse over the last 4 days. Upon further questioning, he also notes that he has been having a tingling and burning sensation rising up from his feet to his knees bilaterally. The patient states he is having difficulty urinating and having bowel movements over the last several days. His temperature is 97.4°F (36.3°C), blood pressure is 122/80 mmHg, pulse is 85/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for weak leg flexion bilaterally along with decreased anal sphincter tone. Which of the following is the best next step in management?
- A. Emergency surgery
- B. CT
- C. Pulmonary function tests
- D. Lumbar puncture
- E. MRI (Correct Answer)
Spinal surgery fundamentals Explanation: ***MRI***
- The patient's symptoms (back pain, ascending paresthesias, bladder/bowel dysfunction, and decreased anal sphincter tone) are highly suggestive of **cauda equina syndrome**. An **MRI of the spine** is the gold standard for diagnosing this condition, as it can visualize the spinal cord and nerve roots directly.
- Early diagnosis and intervention with MRI are crucial to prevent **permanent neurological deficits** in cauda equina syndrome.
*Emergency surgery*
- While emergency surgery might be the next step *after* diagnosis, it is **not the initial diagnostic step**. The cause of the cauda equina syndrome (e.g., disc herniation, tumor) must first be identified.
- Performing surgery without proper imaging could lead to operating on the wrong level or for the wrong pathology.
*CT*
- A **CT scan** can provide information about bony structures but is generally **inferior to MRI** for visualizing soft tissue structures like the spinal cord, nerve roots, and intervertebral discs, which are critical in cauda equina syndrome.
- It may miss subtle compressions or pathologies of the nerve roots.
*Pulmonary function tests*
- **Pulmonary function tests** are used to assess lung function and are **irrelevant** to the patient's acute neurological symptoms and back pain.
- This test would not provide any diagnostic information for suspected cauda equina syndrome.
*Lumbar puncture*
- A **lumbar puncture** is primarily used to analyze cerebrospinal fluid for conditions like infection or inflammation (e.g., meningitis, Guillain-Barré syndrome).
- While Guillain-Barré can cause ascending paralysis, the prominent back pain, bowel/bladder dysfunction, and decreased anal sphincter tone make **cauda equina syndrome** a more likely diagnosis, for which LP is not the primary diagnostic tool.
Spinal surgery fundamentals US Medical PG Question 5: A 35-year-old man who suffered a motor vehicle accident 3 months ago presents to the office for a neurological evaluation. He has no significant past medical history and takes no current medications. He has a family history of coronary artery disease in his father and Alzheimer’s disease in his mother. On physical examination, his blood pressure is 110/60 mm Hg, the pulse is 85/min, the temperature is 37.0°C (98.6°F), and the respiratory rate is 20/min. Neurological examination is suggestive of a lesion in the anterior spinal artery that affects the anterior two-thirds of the spinal cord, which is later confirmed with angiography. Which of the following exam findings would have suggested this diagnosis?
- A. Loss of vibratory sense below the level of the lesion
- B. Loss of pain and temperature sensation above the level of the lesion
- C. Negative plantar extensor response in his lower limbs
- D. Flaccid paralysis on the right side
- E. Preserved pressure sensation (Correct Answer)
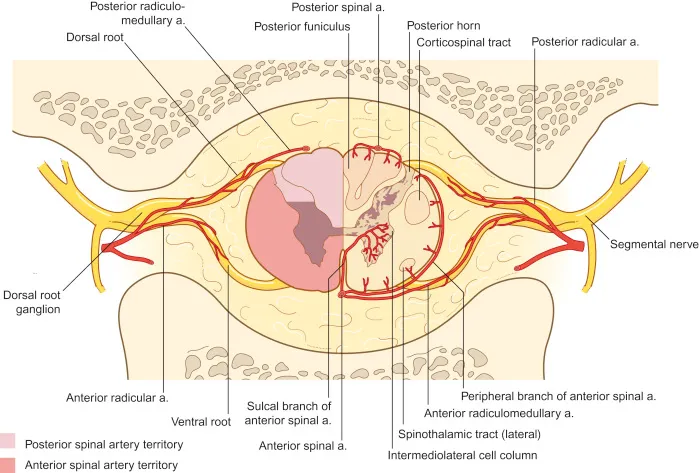
Spinal surgery fundamentals Explanation: ***Preserved pressure sensation***
- **Anterior spinal artery** occlusion affects the **spinothalamic tracts** (pain and temperature) and **corticospinal tracts** (motor function), but spares the **dorsal columns**.
- The **dorsal columns** carry **vibration, proprioception, and discriminative (fine) touch and pressure sensation**, which would therefore be preserved.
- While crude touch/pressure via the anterior spinothalamic tract may be impaired, the preservation of dorsal column function allows for intact discriminative pressure sensation, distinguishing this from other cord syndromes.
*Loss of vibratory sense below the level of the lesion*
- **Vibratory sense** is carried by the **dorsal columns**, which are typically spared in **anterior spinal artery syndromes** as they are supplied by the posterior spinal arteries.
- Loss of vibratory sense would suggest involvement of the posterior part of the spinal cord, inconsistent with an anterior spinal artery lesion.
*Loss of pain and temperature sensation above the level of the lesion*
- **Anterior spinal artery syndrome** causes loss of **pain and temperature sensation** *below* the level of the lesion, as the spinothalamic tracts are affected in the anterior cord.
- Sensation *above* the lesion level should be intact, as those pathways have already ascended past the lesion.
*Negative plantar extensor response in his lower limbs*
- A **negative plantar extensor response** (normal plantar reflex) indicates the toes curl downwards, which is the normal response.
- Lesions of the **corticospinal tract**, such as in anterior spinal artery syndrome, typically cause a **positive Babinski sign** (extensor plantar response), where the big toe extends upwards, indicating upper motor neuron damage.
*Flaccid paralysis on the right side*
- **Anterior spinal artery syndrome** causes **bilateral motor deficits** due to involvement of both **corticospinal tracts** in the anterior cord.
- While initial presentation can be **flaccid paralysis** due to spinal shock below the level of the lesion, it is typically **bilateral**, not unilateral, and evolves to **spastic paralysis** over time.
Spinal surgery fundamentals US Medical PG Question 6: A 57-year-old woman presents to an outpatient clinic with lower extremity weakness and lower back pain. The patient says that her symptoms began 2 weeks ago when she was working in her garden and have progressively worsened to the extent she currently is unable to walk on her own. She describes the pain as sharp, severe and descending bilaterally from her lower back to her lateral ankles along the posterior surface of her thighs and legs. She also states that she has had several episodes of urinary incontinence for the past couple of days. The patient denies having any similar pain or incontinence in the past. No other significant past medical history. Current medications are alendronate 5 mg orally daily and a daily multivitamin. Her temperature is 37.0℃ (98.6℉), the blood pressure is 110/70 mm Hg, the pulse is 72/min, the respiratory rate is 15/min, and oxygen saturation is 99% on room air. On physical examination, the patient appears to be in significant distress. Strength is ⅗ in her thighs bilaterally and ⅖ in the legs bilaterally left greater than right. Muscle tone is decreased in the lower extremities. The patellar reflex is 1+ bilaterally and plantar reflex is 0+ bilaterally. Fine touch and pain and temperature sensation are decreased in the lower extremities bilaterally, left greater than right. Saddle anesthesia is present. Which of the following is the next, best step in the management of this patient?
- A. Outpatient management with a 3-day course of meloxicam and tolperisone and reassess
- B. Recommend non-emergent inpatient spinal manipulation program
- C. Outpatient management with a 3-day course of diclofenac and gabapentin and reassess
- D. Immediate transfer to the emergency department for management (Correct Answer)
- E. Outpatient management with 3 days of strict bed rest and reassess
Spinal surgery fundamentals Explanation: ***Immediate transfer to the emergency department for management***
- The patient presents with classic symptoms of **cauda equina syndrome**, including bilateral lower extremity weakness, severe sciatica, **urinary incontinence (new-onset)**, and **saddle anesthesia**. These constitute a **neurological emergency** requiring urgent evaluation and intervention.
- Cauda equina syndrome results from compression of the neural elements below the conus medullaris (typically L2-L5 and sacral nerve roots).
- **Immediate management** includes urgent **MRI of the lumbosacral spine** (gold standard for diagnosis) and **emergent neurosurgical consultation** for **surgical decompression within 48 hours** (ideally within 24 hours) to prevent permanent neurological deficits, including irreversible bladder/bowel dysfunction and paralysis.
*Outpatient management with a 3-day course of meloxicam and tolperisone and reassess*
- Administering **NSAIDs (meloxicam)** and **muscle relaxants (tolperisone)** for outpatient management would **delay critical care** for a rapidly progressing neurological emergency.
- This approach is inappropriate given the **acute onset of incontinence** and **saddle anesthesia**, which are red flags for cauda equina syndrome requiring immediate intervention.
*Recommend non-emergent inpatient spinal manipulation program*
- **Spinal manipulation** is absolutely **contraindicated** in cases of suspected cauda equina syndrome due to the risk of exacerbating spinal cord or nerve root compression.
- Such a program is designed for less severe, chronic back pain conditions, not for an **acute neurological emergency** with progressive deficits.
*Outpatient management with a 3-day course of diclofenac and gabapentin and reassess*
- While diclofenac (NSAID) and gabapentin (for neuropathic pain) can manage some back pain, they are **insufficient** for cauda equina syndrome, which requires **urgent diagnosis and surgical intervention**.
- Delaying definitive treatment for a few days to "reassess" would likely lead to **irreversible neurological damage**, including permanent bladder dysfunction and paralysis.
*Outpatient management with 3 days of strict bed rest and reassess*
- **Strict bed rest** is generally **not recommended** for acute low back pain and can often be detrimental, potentially leading to deconditioning.
- More importantly, it does nothing to address the underlying **spinal compression** causing the cauda equina syndrome and would lead to **critical delays** in care, risking permanent neurological sequelae.
Spinal surgery fundamentals US Medical PG Question 7: A 38-year-old man comes to the physician for a follow-up examination. He has quadriparesis as a result of a burst fracture of the cervical spine that occurred after a fall from his roof 1 month ago. He has urinary and bowel incontinence. He appears malnourished. His temperature is 37.1°C (98.8°F), pulse is 88/min, and blood pressure is 104/60 mm Hg. Examination shows spasticity in all extremities. Muscle strength is decreased in proximal and distal muscle groups bilaterally. Deep tendon reflexes are 4+ bilaterally. Plantar reflex shows extensor response bilaterally. Sensation to pinprick and temperature is absent below the neck. Sensation to vibration, position, and light touch is normal bilaterally. Rectal tone is decreased. There is a 1-cm area of erythema over the sacrum. Which of the following is the most likely cause of this patient's symptoms?
- A. Hemi-transection of the spinal cord
- B. Cavitation within the spinal cord
- C. Injury to gray matter of the spinal cord
- D. Occlusion of the posterior spinal artery
- E. Damage to the anterior spinal artery (Correct Answer)
Spinal surgery fundamentals Explanation: ***Damage to the anterior spinal artery***
- This typically results in **anterior cord syndrome**, characterized by bilateral loss of pain and temperature sensation, motor function (quadriparesis), and autonomic dysfunction (bowel/bladder incontinence below the level of injury).
- The **preservation of posterior column functions** (vibration, proprioception, light touch) is a hallmark of anterior spinal artery ischemia, as the posterior columns are supplied by the posterior spinal arteries.
*Hemi-transection of the spinal cord*
- This describes **Brown-Séquard syndrome**, which involves ipsilateral loss of motor function, vibration, and proprioception, and contralateral loss of pain and temperature sensation.
- The patient's symptoms are inconsistent with Brown-Séquard syndrome due to the **bilateral presentation of motor and sensory deficits**.
*Cavitation within the spinal cord*
- This condition, known as **syringomyelia**, typically presents with a **cape-like distribution of pain and temperature loss** (due to central cord involvement affecting the decussating spinothalamic fibers).
- It would usually spare motor function initially and would not explain the sudden, severe quadriparesis and complete sensory loss described.
*Injury to gray matter of the spinal cord*
- Isolated gray matter injury, often seen in conditions like **central cord syndrome**, primarily affects the pain and temperature pathways and may cause upper extremity weakness.
- It would not explain the **complete loss of motor function and pain/temperature sensation below the neck** while preserving posterior column function.
*Occlusion of the posterior spinal artery*
- Occlusion of the posterior spinal artery would primarily affect the **dorsal columns**, leading to loss of vibration, proprioception, and light touch.
- This patient, however, has **preserved sensation to vibration, position, and light touch**, making posterior spinal artery occlusion unlikely.
Spinal surgery fundamentals US Medical PG Question 8: A 21-year-old man was involved in a motor vehicle accident and died. At autopsy, the patient demonstrated abnormally increased mobility at the neck. A section of cervical spinal cord at C6 was removed and processed into slides. Which of the following gross anatomic features is most likely true of this spinal cord level?
- A. Cuneate and gracilis fasciculi are present (Correct Answer)
- B. Least amount of white matter
- C. Prominent lateral horns
- D. Absence of gray matter enlargement
- E. Involvement with parasympathetic nervous system
Spinal surgery fundamentals Explanation: **Cuneate and gracilis fasciculi are present**
- At the **C6 level** of the spinal cord, both the **fasciculus gracilis** (carrying information from the lower body) and the **fasciculus cuneatus** (carrying information from the upper body) are present in the dorsal column.
- The fasciculus cuneatus typically appears at **T6 and above**, making it visible at C6.
*Least amount of white matter*
- The cervical spinal cord, particularly at C6, contains a **significant amount of white matter** because it carries all ascending and descending tracts to and from the brain, including those for the upper and lower limbs.
- The **sacral segments** typically have the least amount of white matter due to fewer tracts remaining.
*Prominent lateral horns*
- **Lateral horns** are characteristic of the **thoracic and upper lumbar (T1-L2/L3)** spinal cord segments, where they house preganglionic sympathetic neurons.
- They are generally **absent or poorly developed** in the cervical spinal cord.
*Absence of gray matter enlargement*
- The **cervical enlargement** of the spinal cord, particularly pronounced from C4 to T1, contains an increased amount of gray matter to accommodate the innervation of the **upper limbs**.
- Therefore, the C6 level would show **significant gray matter enlargement**.
*Involvement with parasympathetic nervous system*
- The **parasympathetic nervous system** exits the spinal cord at the **sacral levels (S2-S4)** and as cranial nerves, not primarily from the cervical spinal cord through distinct horns.
- The cervical spinal cord is primarily associated with **somatic motor and sensory pathways** for the neck, shoulders, and upper limbs, and receives some sympathetic input, but is not where parasympathetic outflow predominantly originates.
Spinal surgery fundamentals US Medical PG Question 9: A 69-year-old male presents to the emergency room with back pain. He has a history of personality disorder and metastatic prostate cancer and was not a candidate for surgical resection. He began chemotherapy but discontinued due to unremitting nausea. He denies any bowel or bladder incontinence. He has never had pain like this before and is demanding morphine. The nurse administers IV morphine and he feels more comfortable. Vital signs are stable. On physical examination you note tenderness to palpation along the lower spine, weakness in the bilateral lower extremities, left greater than right. Neurological examination is also notable for hyporeflexia in the knee and ankle jerks bilaterally. You conduct a rectal examination, which reveals saddle anesthesia. Regarding this patient, what is the most likely diagnosis and the appropriate next step in management?
- A. The most likely diagnosis is cauda equina syndrome and the patient should be rushed to radiation
- B. The most likely diagnosis is conus medullaris syndrome and steroids should be started prior to MRI
- C. The most likely diagnosis is cauda equina syndrome and steroids should be started prior to MRI (Correct Answer)
- D. The most likely diagnosis is conus medullaris syndrome and steroids should be started after MRI
- E. The most likely diagnosis is cauda equina syndrome and steroids should be started after MRI
Spinal surgery fundamentals Explanation: ***The most likely diagnosis is cauda equina syndrome and steroids should be started prior to MRI***
- The patient's presentation with **back pain**, **bilateral lower extremity weakness** (left > right), **hyporeflexia**, and **saddle anesthesia** are classic signs of **cauda equina syndrome**. This is often caused by compression of the nerve roots below the spinal cord, commonly from metastasis in patients with a history of prostate cancer.
- Given the suspected **spinal cord compression** due to metastatic disease, initiating **high-dose corticosteroids** (like dexamethasone) before imaging is crucial to reduce edema around the spinal cord and preserve neurological function. An **urgent MRI** is the next step to confirm the diagnosis and localize the compression.
*The most likely diagnosis is cauda equina syndrome and the patient should be rushed to radiation*
- While **cauda equina syndrome** is the correct diagnosis, **radiation** is typically a definitive treatment modality for metastatic compression, not an immediate next step before confirming the extent and location of compression with imaging.
- **Corticosteroids** are the immediate priority to reduce swelling and improve neurological outcomes while awaiting definitive imaging and treatment planning.
*The most likely diagnosis is conus medullaris syndrome and steroids should be started prior to MRI*
- **Conus medullaris syndrome** typically presents with more symmetrical symptoms, often including early-onset **bladder and bowel dysfunction** and **hyperreflexia** (or mixed reflexes), which are not fully consistent with this patient's presentation of hyporeflexia and lack of incontinence.
- Although steroids would be appropriate for suspected compression before MRI for either syndrome, the specific symptom profile strongly favors cauda equina over conus.
*The most likely diagnosis is conus medullaris syndrome and steroids should be started after MRI*
- The patient's symptoms (weakness, hyporeflexia, saddle anesthesia) are more indicative of **cauda equina syndrome** rather than **conus medullaris syndrome** (which often involves hyperreflexia and earlier bowel/bladder dysfunction).
- Delaying **corticosteroids** until after the MRI in suspected spinal cord compression can lead to irreversible neurological damage, as they help reduce edema immediately.
*The most likely diagnosis is cauda equina syndrome and steroids should be started after MRI*
- While **cauda equina syndrome** is the correct diagnosis, waiting for an **MRI** before initiating **corticosteroids** would be a critical delay.
- **Early administration of steroids** is vital in cases of suspected spinal cord compression to reduce inflammation and preserve neurological function, even before definitive imaging.
Spinal surgery fundamentals US Medical PG Question 10: A 47-year-old man is admitted to the emergency room after a fight in which he was hit in the head with a hammer. The witnesses say that the patient initially lost consciousness, but regained consciousness by the time emergency services arrived. On admission, the patient complained of a diffuse headache. He opened his eyes spontaneously, was verbally responsive, albeit confused, and was able to follow commands. He could not elevate his left hand and leg. He did not remember the events prior to the loss of consciousness and had difficulty remembering information, such as the names of nurses or doctors. His airway was not compromised. The vital signs are as follows: blood pressure, 180/100 mm Hg; heart rate, 59/min; respiratory rate, 12/min; temperature 37.0℃ (98.6℉); and SaO2, 96% on room air. The examination revealed bruising in the right frontotemporal region. The pupils are round, equal, and show a poor response to light. The neurologic examination shows hyperreflexia and decreased power in the left upper and lower limbs. There is questionable nuchal rigidity, but no Kernig and Brudzinski signs. The CT scan is shown in the image. Which of the following options is recommended for this patient?
- A. Lumbar puncture
- B. Decompressive craniectomy
- C. Administration of levetiracetam
- D. Administration of methylprednisolone
- E. Surgical evacuation of the clots (Correct Answer)
Spinal surgery fundamentals Explanation: ***Surgical evacuation of the clots***
- The CT scan image shows a **biconvex (lenticular) hyperdensity** consistent with an **epidural hematoma (EDH)**, which typically results from arterial bleeding (often from the **middle meningeal artery**). This patient's **"lucid interval"** (initial loss of consciousness, regain consciousness, then deterioration) is classic for EDH.
- Given the patient's neurological deterioration (left-sided weakness, pupillary changes, confusion, memory issues) and signs of increased intracranial pressure (hypertension, bradycardia - part of Cushing's triad), urgent surgical evacuation of the hematoma is indicated to relieve pressure and prevent herniation.
*Lumbar puncture*
- A lumbar puncture is **contraindicated** in the setting of suspected or confirmed **increased intracranial pressure (ICP)**, as it can precipitate **cerebral herniation**.
- The CT scan clearly demonstrates a space-occupying lesion, making a lumbar puncture unnecessary and potentially dangerous.
*Decompressive craniectomy*
- While decompressive craniectomy is a neurosurgical procedure used to reduce ICP, it is generally considered when other measures have failed or in cases of **diffuse brain swelling** or large **intracerebral hematomas** not amenable to simple evacuation.
- In this case of a localized epidural hematoma with a clear surgical target, direct evacuation is the primary and most effective intervention.
*Administration of levetiracetam*
- Levetiracetam is an **anticonvulsant** used to prevent seizures. While seizures can occur after traumatic brain injury, there is no indication that the patient is currently seizing.
- Prophylactic anticonvulsants are sometimes used in severe TBI, but addressing the life-threatening hematoma takes **precedence** over seizure prophylaxis.
*Administration of methylprednisolone*
- **Corticosteroids** like methylprednisolone are generally **contraindicated** in traumatic brain injury (TBI) as studies have shown **worse outcomes** and increased mortality.
- They are primarily used for their **anti-inflammatory effects** in conditions like spinal cord injury or vasogenic edema from tumors, not for acute head trauma with hematoma.
More Spinal surgery fundamentals US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.