Spinal cord injury management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Spinal cord injury management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Spinal cord injury management US Medical PG Question 1: A 16-year-old girl is brought to the emergency room with hyperextension of the cervical spine caused by a trampoline injury. After ruling out the possibility of hemorrhagic shock, she is diagnosed with quadriplegia with neurogenic shock. The physical examination is most likely to reveal which of the following constellation of findings?
- A. Pulse: 110/min; blood pressure: 88/50 mm Hg; respirations: 26/min; normal rectal tone on digital rectal examination (DRE); normal muscle power and sensations in the limbs
- B. Pulse: 116/min; blood pressure: 80/40 mm Hg; respirations: 16/min; loss of rectal tone on DRE; reduced muscle power and absence of sensations in the limbs
- C. Pulse: 54/min; blood pressure: 88/44 mm Hg; respirations: 26/min; increased rectal tone on DRE; normal muscle power and sensations in the limbs
- D. Pulse: 99/min; blood pressure: 188/90 mm Hg; respirations: 33/min; loss of rectal tone on DRE; reduced muscle power and absence of sensations in the limbs
- E. Pulse: 56/min; blood pressure: 88/40 mm Hg; respirations: 22/min; loss of rectal tone on DRE; reduced muscle power and absence of sensations in the limbs (Correct Answer)
Spinal cord injury management Explanation: **Pulse: 56/min; blood pressure: 88/40 mm Hg; respirations: 22/min; loss of rectal tone on DRE; reduced muscle power and absence of sensations in the limbs**
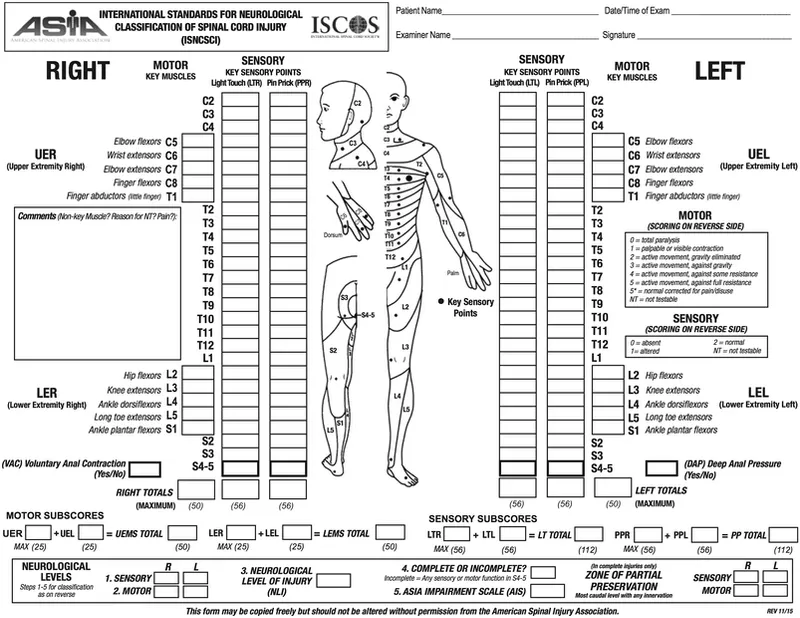
- **Neurogenic shock** is characterized by **bradycardia** and **hypotension** due to the loss of sympathetic tone below the level of the injury, so a pulse of 56/min and blood pressure of 88/40 mm Hg are consistent findings.
- **Quadriplegia** indicates significant neurological dysfunction with **loss of muscle power and sensation** in all four limbs, and loss of **rectal tone** is a key indicator of spinal cord injury.
*Pulse: 110/min; blood pressure: 88/50 mm Hg; respirations: 26/min; normal rectal tone on digital rectal examination (DRE); normal muscle power and sensations in the limbs*
- This option presents **tachycardia** (pulse 110/min), which is inconsistent with the **bradycardia** expected in neurogenic shock.
- **Normal rectal tone**, muscle power, and sensation are directly contradictory to a diagnosis of quadriplegia and spinal cord injury.
*Pulse: 116/min; blood pressure: 80/40 mm Hg; respirations: 16/min; loss of rectal tone on DRE; reduced muscle power and absence of sensations in the limbs*
- The **tachycardia** (pulse 116/min) in this option is not characteristic of **neurogenic shock**, which presents with bradycardia.
- While loss of rectal tone, reduced muscle power, and absence of sensations are consistent with quadriplegia, the vital signs do not fully align with neurogenic shock.
*Pulse: 54/min; blood pressure: 88/44 mm Hg; respirations: 26/min; increased rectal tone on DRE; normal muscle power and sensations in the limbs*
- **Increased rectal tone** and normal muscle power/sensations are inconsistent with **quadriplegia** and spinal cord injury, where loss of function is expected.
- While bradycardia and hypotension are present, these neurological findings contradict the core diagnosis.
*Pulse: 99/min; blood pressure: 188/90 mm Hg; respirations: 33/min; loss of rectal tone on DRE; reduced muscle power and absence of sensations in the limbs*
- This option describes **hypertension** (188/90 mmHg), which is not characteristic of **neurogenic shock**, where **hypotension** is a prominent feature.
- **Tachycardia** (pulse 99/min) is also inconsistent with the bradycardia seen in neurogenic shock.
Spinal cord injury management US Medical PG Question 2: A 44-year-old man is brought to the emergency department 25 minutes after falling off the roof of a house. He was cleaning the roof when he slipped and fell. He did not lose consciousness and does not have any nausea. On arrival, he is alert and oriented and has a cervical collar on his neck. His pulse is 96/min, respirations are 18/min, and blood pressure is 118/78 mm Hg. Examination shows multiple bruises over the forehead and right cheek. The pupils are equal and reactive to light. There is a 2-cm laceration below the right ear. Bilateral ear canals show no abnormalities. The right wrist is swollen and tender; range of motion is limited by pain. The lungs are clear to auscultation. There is no midline cervical spine tenderness. There is tenderness along the 2nd and 3rd ribs on the right side. The abdomen is soft and nontender. Neurologic examination shows no focal findings. Two peripheral venous catheters are placed. Which of the following is the most appropriate next step in management?
- A. CT scan of the cervical spine (Correct Answer)
- B. Focused Assessment with Sonography in Trauma
- C. X-ray of the neck
- D. X-ray of the chest
- E. X-ray of the right wrist
Spinal cord injury management Explanation: ***CT scan of the cervical spine***
- This patient suffered a significant fall from a height, which is a **high-risk mechanism of injury** for cervical spine trauma, even without immediate neurologic deficits or midline tenderness.
- Due to the high-energy trauma and the potential for severe consequences from an unstable cervical spine injury, a **CT scan** is the preferred imaging modality as it offers superior detail compared to plain X-rays, especially in complex anatomy.
- The patient is **hemodynamically stable** with a benign abdominal exam, and the cervical collar is already in place, indicating that spinal precautions are the immediate priority before any further movement or transfers.
*Focused Assessment with Sonography in Trauma (FAST)*
- FAST exam is primarily used to detect **free fluid (hemorrhage)** in the pericardial, perihepatic, perisplenic, and pelvic spaces in trauma patients.
- While important in trauma evaluation, this patient is **hemodynamically stable** (normal blood pressure, normal pulse) with a **soft, nontender abdomen**, making urgent FAST less critical than clearing the cervical spine.
- The primary concern in a patient with a significant fall mechanism and cervical collar in place is ruling out **cervical spine instability** before further interventions or movement.
*X-ray of the neck*
- While an X-ray can assess the cervical spine, a **CT scan** is generally superior for detecting subtle fractures, ligamentous injuries, and malalignments, especially in patients with high-energy trauma.
- Given the patient's mechanism of injury, an X-ray might miss critical injuries that a CT would identify, leading to potential delays in diagnosis and treatment.
*X-ray of the chest*
- A chest X-ray would be appropriate to assess the patient's **rib fractures** and potential associated injuries like pneumothorax or hemothorax.
- However, the most immediate life-threatening injury in this context, after airway and breathing are secured, is an unstable cervical spine injury, which takes precedence in a stable patient with high-risk mechanism.
*X-ray of the right wrist*
- An X-ray of the right wrist is indicated to evaluate the **swollen and tender wrist** for a fracture or dislocation.
- While important for comprehensive trauma management, it is not the most immediate or life-threatening concern compared to potential cervical spine injury from a high-impact fall.
Spinal cord injury management US Medical PG Question 3: A 51-year-old woman comes to the physician because of progressively worsening lower back pain. The pain radiates down the right leg to the lateral side of the foot. She has had no trauma, urinary incontinence, or fever. An MRI of the lumbar spine shows disc degeneration and herniation at the level of L5–S1. Which of the following is the most likely finding on physical examination?
- A. Difficulty walking on heels
- B. Exaggerated patellar tendon reflex
- C. Diminished sensation of the anus and genitalia
- D. Diminished sensation of the anterior lateral thigh
- E. Weak Achilles tendon reflex (Correct Answer)
Spinal cord injury management Explanation: ***Weak Achilles tendon reflex***
- A herniated disc at **L5-S1** typically compresses the **S1 nerve root**, which is responsible for the **Achilles tendon reflex**.
- **S1 radiculopathy** presents with weakness in plantarflexion, diminished or absent Achilles reflex, and sensory loss in the **lateral foot** (matching the patient's symptoms).
*Difficulty walking on heels*
- Difficulty walking on heels (**dorsiflexion weakness**) is primarily associated with **L4-L5 disc herniation** compressing the **L5 nerve root**.
- This symptom indicates **L5 radiculopathy**, which affects the tibialis anterior muscle, not S1.
*Exaggerated patellar tendon reflex*
- An exaggerated patellar tendon reflex (**hyperreflexia**) indicates an **upper motor neuron lesion** or spinal cord compression above the lumbar region.
- A disc herniation at **L5-S1** causes a **lower motor neuron lesion** with diminished reflexes, not hyperreflexia.
*Diminished sensation of the anus and genitalia*
- This symptom, along with urinary incontinence and saddle anesthesia, is characteristic of **cauda equina syndrome**, a surgical emergency.
- The patient lacks urinary incontinence and the specific unilateral pain pattern points to isolated **S1 radiculopathy**, not cauda equina syndrome.
*Diminished sensation of the anterior lateral thigh*
- Sensory loss in the **anterior lateral thigh** is associated with compression of the **lateral femoral cutaneous nerve** or **L2-L4 nerve roots**.
- This pattern is not consistent with **L5-S1 disc herniation**, which causes sensory changes in the lateral foot and posterior leg.
Spinal cord injury management US Medical PG Question 4: A 65-year-old man presents to the emergency department for sudden weakness. He was doing mechanical work on his car where he acutely developed right-leg weakness and fell to the ground. He is accompanied by his wife, who said that this has never happened before. He was last seen neurologically normal approximately 2 hours prior to presentation. His past medical history is significant for hypertension and type II diabetes. His temperature is 98.8°F (37.1°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. Neurological exam reveals that he is having trouble speaking and has profound weakness of his right upper and lower extremity. Which of the following is the best next step in management?
- A. Thrombolytics
- B. Noncontrast head CT (Correct Answer)
- C. CT angiogram
- D. MRI of the head
- E. Aspirin
Spinal cord injury management Explanation: ***Noncontrast head CT***
- A **noncontrast head CT** is the most crucial initial step in managing acute stroke symptoms because it can rapidly rule out an **intracranial hemorrhage**.
- Distinguishing between ischemic stroke and hemorrhagic stroke is critical, as the management strategies are vastly different and administering thrombolytics in the presence of hemorrhage can be fatal.
*Thrombolytics*
- **Thrombolytics** can only be administered after an **intracranial hemorrhage** has been excluded via noncontrast head CT.
- Administering thrombolytics without imaging could worsen a hemorrhagic stroke, causing significant harm or death.
*CT angiogram*
- A **CT angiogram** is used to identify large vessel occlusions in ischemic stroke and is typically performed after a noncontrast CT rules out hemorrhage.
- This imaging is crucial for determining eligibility for **endovascular thrombectomy** but is not the very first diagnostic step.
*MRI of the head*
- An **MRI of the head** is more sensitive for detecting acute ischemic changes but takes longer to perform and is often not readily available in the acute emergency setting.
- It is not the initial imaging of choice for ruling out hemorrhage due to its longer acquisition time compared to CT.
*Aspirin*
- **Aspirin** is indicated for acute ischemic stroke but should only be given after an **intracranial hemorrhage** has been ruled out.
- Like thrombolytics, aspirin could exacerbate a hemorrhagic stroke and is thus deferred until initial imaging is complete.
Spinal cord injury management US Medical PG Question 5: A 22-year-old man is brought to the emergency department after he was impaled by a metal rod during a work accident. The rod went into his back around the level of T9 but was removed before arrival. He has no past medical history and does not take any medications. On physical examination, he has significant muscle weakness in his entire left lower body. He also exhibits impaired vibration and proprioception in his left leg as well as loss of pain and temperature sensation in his right leg. Which of the following sections of the spinal cord was most likely damaged in this patient?
- A. Posterior cord
- B. Anterior cord
- C. Left hemicord (Correct Answer)
- D. Central cord
- E. Right hemicord
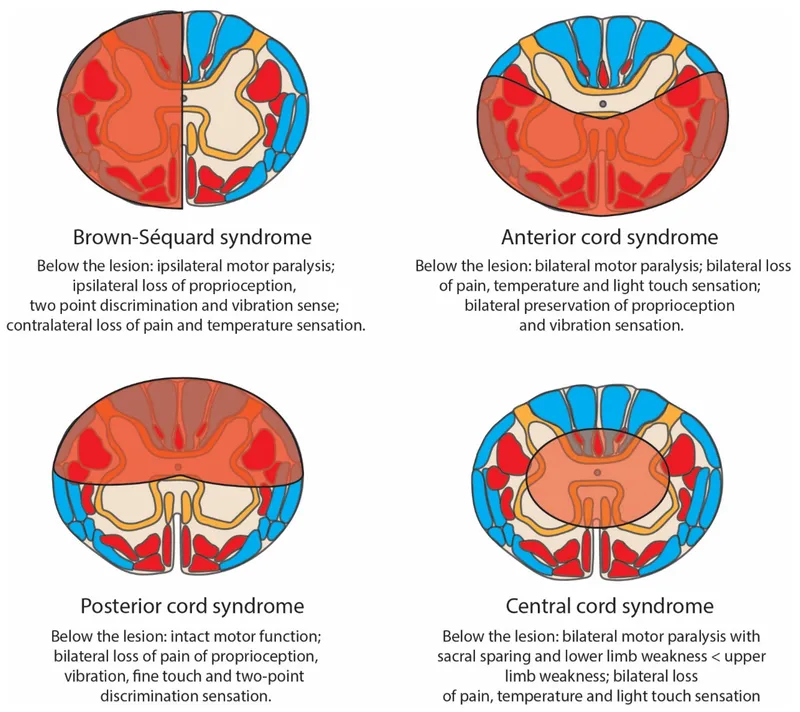
Spinal cord injury management Explanation: ***Left hemicord***
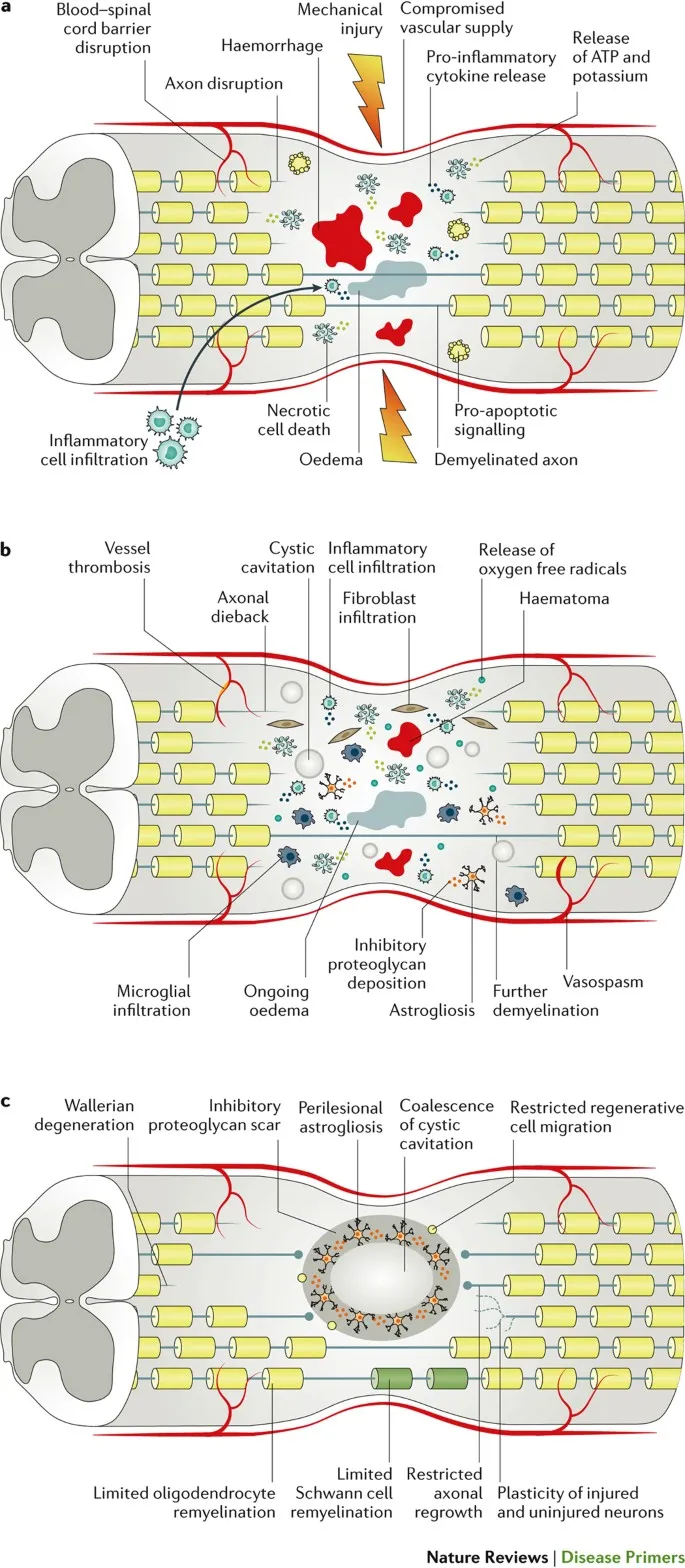
- The combination of **ipsilateral motor weakness** and **loss of vibration/proprioception** (damage to the **corticospinal tract** and **dorsal column**) along with **contralateral loss of pain/temperature** (damage to the **spinothalamic tract**) is the classic presentation of **Brown-Séquard syndrome**, which results from a lesion affecting one side (hemicord) of the spinal cord.
- The injury at **T9** is consistent with lower body symptoms, as tracts for the legs would be affected at this level.
*Posterior cord*
- Damage to the **posterior cord** primarily affects the **dorsal columns**, leading to **ipsilateral loss of vibration and proprioception**.
- It would not explain the **ipsilateral motor weakness** or the **contralateral loss of pain and temperature sensation**.
*Anterior cord*
- **Anterior cord syndrome** typically presents with **bilateral loss of motor function** (due to damage to the corticospinal tracts) and **bilateral loss of pain and temperature sensation** (due to damage to the spinothalamic tracts).
- **Vibration and proprioception** are usually preserved because the dorsal columns are spared.
*Central cord*
- **Central cord syndrome** most commonly results from hyperextension injuries, particularly in the cervical spine, affecting the central gray matter.
- It typically causes greater **weakness in the upper extremities** than the lower extremities and a variable sensory loss, often in a **"cape-like" distribution**.
*Right hemicord*
- A **right hemicord** lesion would cause **right-sided motor weakness** and **loss of vibration/proprioception**, along with **left-sided loss of pain/temperature sensation**.
- The patient's symptoms are on the **left side for motor/proprioception** and the **right side for pain/temperature**, indicating a left hemicord lesion.
Spinal cord injury management US Medical PG Question 6: A previously healthy 44-year-old man is brought by his coworkers to the emergency department 45 minutes after he became light-headed and collapsed while working in the boiler room of a factory. He did not lose consciousness. His coworkers report that 30 minutes prior to collapsing, he told them he was nauseous and had a headache. The patient appears sweaty and lethargic. He is not oriented to time, place, or person. The patient’s vital signs are as follows: temperature 41°C (105.8°F); heart rate 133/min; respiratory rate 22/min; and blood pressure 90/52 mm Hg. Examination shows equal and reactive pupils. Deep tendon reflexes are 2+ bilaterally. His neck is supple. A 0.9% saline infusion is administered. A urinary catheter is inserted and dark brown urine is collected. The patient’s laboratory test results are as follows:
Laboratory test
Blood
Hemoglobin 15 g/dL
Leukocyte count 18,000/mm3
Platelet count 51,000/mm3
Serum
Na+ 149 mEq/L
K+ 5.0 mEq/L
Cl- 98 mEq/L
Urea nitrogen 42 mg/dL
Glucose 88 mg/dL
Creatinine 1.8 mg/dL
Aspartate aminotransferase (AST, GOT) 210
Alanine aminotransferase (ALT, GPT) 250
Creatine kinase 86,000 U/mL
Which of the following is the most appropriate next step in patient management?
- A. Dantrolene
- B. Acetaminophen therapy
- C. Hemodialysis
- D. Ice water immersion (Correct Answer)
- E. Evaporative cooling
Spinal cord injury management Explanation: ***Ice water immersion***
- This patient presents with signs and symptoms consistent with **heat stroke**, including high body temperature (41°C), altered mental status, and a history of working in a hot environment (boiler room). **Rapid aggressive cooling** is the most critical immediate intervention to prevent organ damage.
- **Ice water immersion** is the fastest and most effective cooling method for heat stroke, aiming to reduce core body temperature to less than 39°C (102.2°F) within 30 minutes.
*Dantrolene*
- **Dantrolene** is primarily used to treat **malignant hyperthermia** and **neuroleptic malignant syndrome**, conditions caused by abnormal calcium release in muscle cells, not environmental heat exposure.
- While both conditions involve hyperthermia, the underlying pathophysiology and triggers are different from heat stroke.
*Acetaminophen therapy*
- **Acetaminophen** is an antipyretic that works by inhibiting prostaglandin synthesis in the central nervous system, affecting the hypothalamic thermoregulatory center.
- It is **ineffective** for the hyperthermia seen in heat stroke, which is due to a failure of thermoregulation rather than an altered hypothalamic set point, and could potentially worsen liver injury.
*Hemodialysis*
- **Hemodialysis** is indicated for severe **renal failure**, drug overdose, or certain electrolyte imbalances. Although this patient has acute kidney injury (elevated BUN and creatinine, dark urine suggestive of rhabdomyolysis), aggressive cooling is the immediate life-saving intervention for heat stroke.
- While renal support might be necessary later if kidney injury progresses, it is not the most appropriate *initial* next step for hyperthermia and altered mental status.
*Evaporative cooling*
- **Evaporative cooling** (e.g., spraying with lukewarm water and using fans) is a cooling method that can be effective, particularly in environments with low humidity.
- However, for severe heat stroke with a temperature as high as 41°C, **ice water immersion** provides a more rapid and aggressive temperature reduction, which is crucial for improving outcomes.
Spinal cord injury management US Medical PG Question 7: A 61-year-old man is found dead in his home after his neighbors became concerned when they did not see him for several days. The man was described as a "recluse" who lived alone and mostly kept to himself. Medical records reveal that he had not seen a physician in over a decade. He had a known history of vascular disease including hypertension, hyperlipidemia, and diabetes mellitus. He did not take any medications for these conditions. An autopsy is performed to identify the cause of death. Although it is determined that the patient suffered from a massive cerebrovascular accident as the cause of death, an incidental finding of a tumor arising from the spinal cord meninges is noted. The tumor significantly compresses the left anterolateral lower thoracic spinal cord. The right side of the spinal cord and the posterior spinal cord appear normal. Which of the following would most likely be impaired due to this lesion?
- A. Pain sensation from the right side of the body (Correct Answer)
- B. Proprioceptive sensation from the left side of the body
- C. Temperature sensation from the left side of the body
- D. Pressure sensation from the left side of the body
- E. Vibratory sensation from the right side of the body
Spinal cord injury management Explanation: ***Pain sensation from the right side of the body***
- Compression of the **left anterolateral lower thoracic spinal cord** would affect the **spinothalamic tract** on that side. The spinothalamic tract carries **pain and temperature** sensations from the **contralateral** side of the body.
- Since the fibers decussate (cross over) at the level of the spinal cord entry, a lesion on the left side of the cord would impair pain sensation from the right side of the body.
*Proprioceptive sensation from the left side of the body*
- Proprioception is carried by the **dorsal columns**, which are located in the posterior part of the spinal cord and decussate in the brainstem.
- The lesion is described as affecting the **anterolateral** left spinal cord, and the posterior cord is noted as normal, making this unlikely.
*Temperature sensation from the left side of the body*
- Temperature sensation is carried by the **spinothalamic tract**, similar to pain.
- This tract decussates at the level of entry into the spinal cord, so a lesion on the left anterolateral cord would impair temperature sensation from the **contralateral (right)** side, not the ipsilateral (left) side.
*Pressure sensation from the left side of the body*
- **Crude touch and pressure** are partially carried by the **spinothalamic tract** and partially by the **dorsal columns**.
- Impairment of pressure sensation on the left side would primarily indicate damage to the ipsilateral dorsal column pathway or significant bilateral spinothalamic involvement, neither of which is consistent with an isolated left anterolateral lesion affecting ipsilateral sensation.
*Vibratory sensation from the right side of the body*
- Vibratory sensation is carried by the **dorsal columns**, which are in the posterior spinal cord and decussate in the medulla oblongata.
- The lesion is in the **anterolateral** left spinal cord, and the posterior cord is noted as normal, making this an unlikely finding.
Spinal cord injury management US Medical PG Question 8: A 22-year-old man is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which he was the unrestrained driver. After extrication, he had severe neck pain and was unable to move his arms and legs. On arrival, he is lethargic and cannot provide a history. Hospital records show that eight months ago, he underwent an open reduction and internal fixation of the right humerus. His neck is immobilized in a cervical collar. Intravenous fluids are being administered. His pulse is 64/min, respirations are 8/min and irregular, and blood pressure is 104/64 mm Hg. Examination shows multiple bruises over the chest, abdomen, and extremities. There is flaccid paralysis and absent reflexes in all extremities. Sensory examination shows decreased sensation below the shoulders. Cardiopulmonary examination shows no abnormalities. The abdomen is soft. There is swelling of the right ankle and right knee. Squeezing of the glans penis does not produce anal sphincter contraction. A focused assessment with sonography for trauma shows no abnormalities. He is intubated and mechanically ventilated. Which of the following is the most appropriate next step in management?
- A. Cervical x-ray
- B. CT of the head
- C. Intravenous dexamethasone therapy
- D. MRI of the spine (Correct Answer)
- E. Placement of Foley catheter
Spinal cord injury management Explanation: **MRI of the spine**
- The patient presents with clear signs of a **spinal cord injury** (flaccid paralysis, absent reflexes, decreased sensation below the shoulders, severe neck pain after trauma). **MRI** is the most sensitive and specific imaging modality to visualize soft tissue injuries, including the spinal cord, ligaments, and disc herniations, which are crucial for diagnosing and guiding treatment for a spinal cord injury.
- Given the patient's **hemodynamic stability** after initial resuscitation and intubation, and the suspicion of spinal cord injury, a thorough evaluation with MRI is the next appropriate step to delineate the extent and location of the injury.
*Cervical x-ray*
- While cervical X-rays are often performed in trauma cases, they have **limited sensitivity** for detecting all spinal injuries, especially soft tissue damage, ligamentous injuries, or non-displaced fractures.
- In a patient with clear neurological deficits suggesting spinal cord involvement, X-rays alone are **insufficient** for a definitive diagnosis and treatment planning.
*CT of the head*
- A CT scan of the head would be appropriate if there were signs of a **head injury**, such as focal neurological deficits suggestive of intracranial pathology, or a change in mental status not fully explained by other injuries.
- In this case, the predominant neurological signs point to a **spinal cord injury** rather than a primary head injury, making head CT a lower priority at this stage.
*Intravenous dexamethasone therapy*
- The use of high-dose corticosteroids like dexamethasone for acute spinal cord injury is **controversial** and its routine use is **not recommended** by current guidelines due to a lack of clear benefit and potential for harm.
- Imaging to characterize the injury is a more urgent and appropriate step before considering any pharmacological interventions for spinal cord protection.
*Placement of Foley catheter*
- While a **Foley catheter** will likely be needed for this patient to manage neurogenic bladder dysfunction that often accompanies spinal cord injury, it is a supportive measure.
- It does not address the immediate diagnostic need to characterize the spinal cord injury, which is paramount for guiding surgical or medical management and preventing further damage.
Spinal cord injury management US Medical PG Question 9: A 22-year-old man is rushed to the emergency department after a motor vehicle accident. The patient states that he feels weakness and numbness in both of his legs. He also reports pain in his lower back. His airway, breathing, and circulation is intact, and he is conversational. Neurologic exam is significant for bilateral lower extremity flaccid paralysis and impaired pain and temperature sensation up to T10-T11 with normal vibration sense. A computerized tomography scan of the spine is performed which shows a vertebral burst fracture of the vertebral body at the level of T11. Which of the following findings is most likely present in this patient?
- A. Intact vibration sense
- B. Bowel incontinence (Correct Answer)
- C. Flaccid paralysis at the level of the lesion
- D. Spasticity below the lesion
- E. Impaired proprioception sense
Spinal cord injury management Explanation: ***Bowel incontinence***
- The presented symptoms of acute **bilateral lower extremity flaccid paralysis**, **impaired pain and temperature sensation**, and a T11 **vertebral burst fracture** are highly indicative of **anterior cord syndrome**.
- **Anterior cord syndrome** characteristically involves damage to the **anterior two-thirds of the spinal cord**, affecting the **corticospinal tracts** (motor control), **spinothalamic tracts** (pain and temperature sensation), and the **autonomic fibers** that control bladder and bowel function, leading to **bowel and bladder dysfunction**.
*Intact vibration sense*
- The sensation of **vibration** and **proprioception** is carried by the **dorsal columns** (posterior part of the spinal cord), which are typically **spared** in **anterior cord syndrome**.
- Therefore, **intact vibration sense** is an expected finding, but the question asks for the **most likely finding** that represents a significant complication of the syndrome.
*Flaccid paralysis at the level of the lesion*
- While **flaccid paralysis** is present in the lower extremities, it occurs **below the level of the lesion** due to damage to the descending motor tracts (corticospinal tracts).
- Flaccid paralysis *at* the level of the lesion would typically involve damage to the **lower motor neurons** at that specific segment, which is not the primary feature described for a burst fracture causing **anterior cord syndrome**.
*Spasticity below the lesion*
- **Spasticity** typically develops much **later** in spinal cord injuries, after the initial phase of **spinal shock** resolves (usually weeks to months).
- In the acute phase following a significant spinal cord injury, **flaccid paralysis** is the more common finding below the lesion, reflecting spinal shock.
*Impaired proprioception sense*
- Similar to vibration sense, **proprioception** is primarily mediated by the **dorsal columns**, which are generally **spared** in **anterior cord syndrome**.
- Therefore, **proprioception** would likely be **intact**, not impaired, in this specific type of spinal cord injury.
Spinal cord injury management US Medical PG Question 10: A 20-year-old man presents to the family medicine clinic with left knee pain. He is the star running back for his college football team with a promising future in the sport. He states he injured his knee 2 days ago during the final game of the season while making a cutting move, where his foot was planted and rotated outward and his knee buckled inward. He admits to feeling a ‘pop’ and having immediate pain. He denies any locking, clicking, or giving way since the event. Physical examination reveals an antalgic gait with avoidance of active knee extension. His left knee demonstrates moderate, diffuse swelling and is very tender to palpation along the joint line. Which of the following structures is most likely damaged in this patient?
- A. Medial meniscus
- B. Anterior cruciate ligament (Correct Answer)
- C. Lateral meniscus
- D. Posterior cruciate ligament
- E. Medial collateral ligament
Spinal cord injury management Explanation: ***Anterior cruciate ligament***
- The mechanism of injury, described as a **cutting move** with the foot planted and knee buckled inward, is a classic non-contact mechanism for **ACL tears**.
- A palpable or audible **'pop'** at the time of injury, followed by immediate pain and swelling, is highly characteristic of an **ACL rupture**.
*Medial meniscus*
- While meniscal tears can cause pain and swelling along the joint line, the history of a **'pop' and immediate swelling** is more indicative of ligamentous injury.
- Absence of **locking or clicking** on the examination makes a primary meniscal tear less likely in this acute presentation.
*Lateral meniscus*
- The injury mechanism, an **external rotation force** on a planted foot, is less commonly associated with isolated lateral meniscal tears than with ACL or medial meniscal injuries.
- Similar to the medial meniscus, the lack of **locking or clicking** makes an isolated lateral meniscal tear less probable.
*Posterior cruciate ligament*
- PCL injuries typically result from a **direct blow to the anterior tibia** with the knee flexed or from a hyperextension injury, which is inconsistent with the described mechanism.
- A PCL injury would most likely present with **posterior laxity** on examination, rather than the general instability often associated with an ACL tear.
*Medial collateral ligament*
- MCL injuries result from a **valgus stress** to the knee, often without an audible 'pop' and usually causing localized pain on the medial side.
- While a valgus force can occur, the prominent **'pop' and immediate, diffuse swelling** are more consistent with an ACL injury than an isolated MCL sprain.
More Spinal cord injury management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.