Lumbar puncture technique and indications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lumbar puncture technique and indications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lumbar puncture technique and indications US Medical PG Question 1: A 22-year-old female is brought to the emergency department by her roommate with a one day history of fever and malaise. She did not feel well after class the previous night and has been in her room since then. She has not been eating or drinking due to severe nausea. Her roommate checked on her one hour ago and was alarmed to find a fever of 102°F (38.9°C). On physical exam temperature is 103°F (40°C), blood pressure is 110/66 mmHg, pulse is 110/min, respirations are 23/min, and pulse oximetry is 98% on room air. She refuses to move her neck and has a rash on her trunk. You perform a lumbar puncture and the CSF analysis is shown below.
Appearance: Cloudy
Opening pressure: 180 mm H2O
WBC count: 150 cells/µL (93% PMN)
Glucose level: < 40 mg/dL
Protein level: 50 mg/dL
Gram stain: gram-negative diplococci
Based on this patient's clinical presentation, which of the following should most likely be administered?
- A. Ceftriaxone (Correct Answer)
- B. Dexamethasone
- C. Rifampin
- D. Acyclovir
- E. Erythromycin
Lumbar puncture technique and indications Explanation: ***Ceftriaxone***
- The patient presents with classic signs of **bacterial meningitis** (fever, neck stiffness, rash, altered mental status) and CSF analysis confirms, showing **cloudy appearance**, **elevated opening pressure**, **high WBC count with PMN predominance**, **low glucose**, and **gram-negative diplococci** on Gram stain, typical for *Neisseria meningitidis*.
- **Ceftriaxone** is a third-generation cephalosporin, a first-line antibiotic for treating bacterial meningitis, particularly effective against *Neisseria meningitidis*.
*Dexamethasone*
- While **dexamethasone** can be used as an adjunct in bacterial meningitis, particularly when caused by *Streptococcus pneumoniae*, it's administered *before or with* the first dose of antibiotics to mitigate inflammation.
- It is not the primary treatment to *eradicate* the infection and is less critical than immediate antibiotic therapy.
*Rifampin*
- **Rifampin** is primarily used for chemoprophylaxis in close contacts of individuals with meningococcal meningitis, or as part of a multi-drug regimen for tuberculosis.
- It is not the recommended first-line monotherapy for acute bacterial meningitis.
*Acyclovir*
- **Acyclovir** is an antiviral medication used to treat herpes simplex virus (HSV) meningitis or encephalitis.
- The CSF analysis showing **gram-negative diplococci** clearly indicates a bacterial etiology, not viral, making acyclovir inappropriate.
*Erythromycin*
- **Erythromycin** is a macrolide antibiotic with a narrower spectrum of activity and is not typically used as first-line treatment for bacterial meningitis, especially not for *Neisseria meningitidis*.
- Its use is often limited by resistance and side effects compared to third-generation cephalosporins.
Lumbar puncture technique and indications US Medical PG Question 2: A 25-year-old man comes to the physician for severe back pain. He describes the pain as shooting and stabbing. On a 10-point scale, he rates the pain as a 9 to 10. The pain started after he lifted a heavy box at work; he works at a supermarket and recently switched from being a cashier to a storekeeper. The patient appears to be in severe distress. Vital signs are within normal limits. On physical examination, the spine is nontender without paravertebral muscle spasms. Range of motion is normal. A straight-leg raise test is negative. After the physical examination has been completed, the patient asks for a letter to his employer attesting to his inability to work as a storekeeper. Which of the following is the most appropriate response?
- A. “Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”
- B. You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing.
- C. I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job. (Correct Answer)
- D. The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional.
- E. The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy.
Lumbar puncture technique and indications Explanation: ***"I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job."***
- This response acknowledges the patient's reported discomfort while gently highlighting the **discrepancy between symptoms and objective findings**, which is crucial in cases of suspected **somatoform or functional pain**.
- It also opens communication about potential **psychosocial stressors** related to his job change, which could be contributing to his symptoms, without dismissing his pain or making a premature diagnosis.
*"You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing."*
- While this option correctly identifies the lack of physical findings, it can be perceived as dismissive of the patient's pain, potentially damaging the **physician-patient relationship**.
- Suggesting regular meetings without a clear plan for addressing his immediate concerns or exploring underlying issues might not be the most effective initial approach.
*“Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”*
- This response would **validate the patient's claim of severe pain** without objective evidence, potentially reinforcing illness behavior and avoiding addressing the underlying issue.
- Providing a doctor's note for inability to work without a clear diagnostic basis or understanding of the pain's origin is **medically inappropriate** and could set a precedent for future such requests.
*"The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional."*
- Directly labeling the problem as "psychological" can be **stigmatizing and alienating** to the patient, leading to distrust and resistance to care.
- While a psychological component might be present, immediately referring to mental health without further exploration of the patient's situation or current stressors is premature and lacks empathy.
*"The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy."*
- Similar to the previous option, explicitly stating a "psychological problem" can be **stigmatizing**.
- Jumping directly to recommending **cognitive-behavioral therapy (CBT)** without a comprehensive discussion and patient buy-in is premature and may lead to non-compliance.
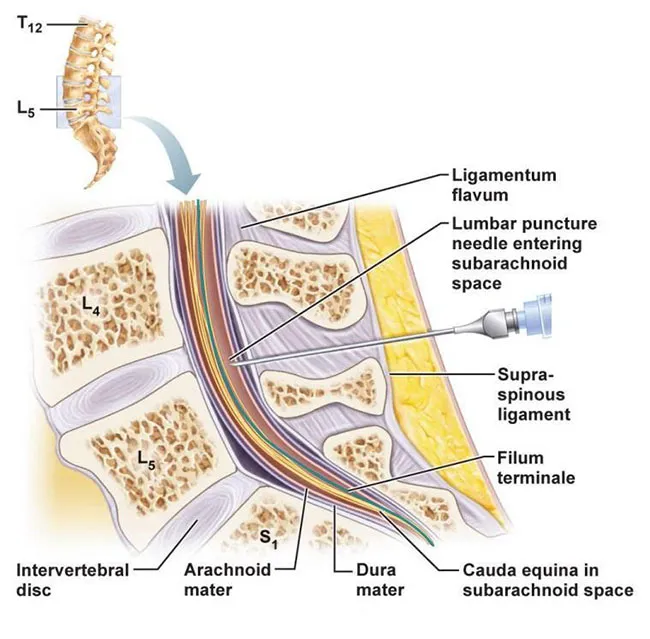
Lumbar puncture technique and indications US Medical PG Question 3: A 26-year-old female with AIDS (CD4 count: 47) presents to the emergency department in severe pain. She states that over the past week she has been fatigued and has had a progressively worse headache and fever. These symptoms have failed to remit leading her to seek care in the ED. A lumbar puncture is performed which demonstrates an opening pressure of 285 mm H2O, increased lymphocytes, elevated protein, and decreased glucose. The emergency physician subsequently initiates treatment with IV amphotericin B and PO flucytosine. What additional treatment in the acute setting may be warranted in this patient?
- A. Serial lumbar punctures (Correct Answer)
- B. Fluconazole
- C. Mannitol
- D. Chloramphenicol
- E. Acetazolamide
Lumbar puncture technique and indications Explanation: **Serial lumbar punctures**
- The elevated opening pressure (285 mm H2O) indicates **increased intracranial pressure (ICP)**, which is common in cryptococcal meningitis and can be life-threatening.
- Serial lumbar punctures can help to **reduce ICP** and relieve symptoms, improving outcomes in patients with cryptococcal meningitis.
*Fluconazole*
- Fluconazole is used for **maintenance therapy** to prevent relapse after the acute phase of cryptococcal meningitis has been controlled.
- It is generally **not recommended for initial acute treatment** in severe cases due to its fungistatic nature, making it less effective than the combination of amphotericin B and flucytosine.
*Mannitol*
- Mannitol is an **osmotic diuretic** sometimes used to acutely *reduce* ICP in cases of cerebral edema.
- While effective in some situations, it is **not the primary treatment for increased ICP** in cryptococcal meningitis, where repeated LPs are preferred to remove infected CSF and directly reduce pressure.
*Chloramphenicol*
- Chloramphenicol is an **antibiotic** primarily used to treat bacterial infections, not fungal infections.
- It has **no role in the treatment of fungal meningitis** caused by *Cryptococcus neoformans*.
*Acetazolamide*
- Acetazolamide is a **carbonic anhydrase inhibitor** that can reduce CSF production, thereby *reducing* ICP.
- While it can be used in some cases of elevated ICP, routine use in cryptococcal meningitis is **not standard practice**, and serial LPs are generally the preferred method for managing dangerously high ICP in this context due to their immediate efficacy.
Lumbar puncture technique and indications US Medical PG Question 4: A 26-year-old G1P0 woman at 40 weeks estimated gestational age presents after experiencing labor pains. Pregnancy has been uncomplicated so far. Rupture of membranes occurs, and a transvaginal delivery is performed under epidural anesthesia, and the baby is delivered alive and healthy. The patient voids a few hours after the delivery and complains of mild irritation at the injection site on her back. On the second day, she complains of a severe headache over the back of her head. The headache is associated with pain and stiffness in the neck. Her headache is aggravated by sitting up or standing and relieved by lying down. The pain is relieved slightly by acetaminophen and ibuprofen. The patient is afebrile. Her vital signs include: pulse 100/min, respiratory rate 18/min, and blood pressure 128/84 mm Hg. Which of the following statements is the most accurate regarding this patient’s condition?
- A. A blockage of CSF is the cause of this patient’s headache
- B. An infection is present at the epidural injection site
- C. This patient’s condition can resolve on its own (Correct Answer)
- D. Excessive bed rest will worsen this patient’s condition
- E. Immediate intervention is required
Lumbar puncture technique and indications Explanation: ***This patient’s condition can resolve on its own***
- The symptoms describe a **post-dural puncture headache (PDPH)**, a common complication of epidural anesthesia, which is often **self-limiting** within days to weeks.
- Initial management involves conservative measures like bed rest, hydration, and analgesics, as many cases resolve without specific interventions.
*A blockage of CSF is the cause of this patient’s headache*
- PDPH is caused by a **leakage of cerebrospinal fluid (CSF)** through the dura mater, leading to **intracranial hypotension**, not a blockage of CSF flow.
- The leakage reduces CSF pressure, causing the brain to sag when upright, stretching pain-sensitive structures like meninges and blood vessels.
*An infection is present at the site of epidural injection site*
- While localized irritation is mentioned, there are no signs of infection such as **fever**, **erythema**, or **purulent discharge** at the injection site, making infection less likely.
- The headache characteristics (positional, severe, neck stiffness) are classic for PDPH, not typically seen in local epidural infections, which would also present with systemic signs.
*Excessive bed rest will worsen this patient’s condition*
- **Bed rest** typically **improves** the symptoms of PDPH by reducing the gravitational pull on the intracranial structures, thereby alleviating the headache.
- Prolonged bed rest is generally recommended in the acute phase, often combined with hydration and caffeine, to help manage symptoms, not worsen them.
*Immediate intervention is required*
- While severe PDPH can be debilitating, immediate invasive intervention (like an **epidural blood patch**) is usually reserved for cases that are **severe and refractory to conservative management** after 24-48 hours.
- Many patients experience spontaneous resolution or significant improvement with conservative measures, making immediate invasive intervention typically unnecessary.
Lumbar puncture technique and indications US Medical PG Question 5: A 77-year-old man with a history of hypertension and a 46 pack-year smoking history presents to the emergency department from an extended care facility with acute onset of headache, nausea, vomiting, and neck pain which started 6 hours ago and has persisted since. He is alert, but his baseline level of consciousness is slightly diminished per the nursing home staff. His temperature is 99.0°F (37.2°C), blood pressure is 164/94 mmHg, pulse is 90/min, respirations are 16/min, and oxygen saturation is 98% on room air. The patient's neurological exam is unremarkable with cranial nerves II-XII grossly intact and with stable gait with a walker. He is immediately sent for a head CT which is normal. What is the most appropriate next step in management?
- A. Ultrasound
- B. Lumbar puncture (Correct Answer)
- C. Alteplase
- D. Ibuprofen, acetaminophen, metoclopramide, and diphenhydramine
- E. MRI
Lumbar puncture technique and indications Explanation: ***Lumbar puncture***
- The patient's symptoms (acute severe headache, nausea, vomiting, neck pain) and risk factors (hypertension, smoking history) are highly suggestive of a **subarachnoid hemorrhage (SAH)**, even with a normal initial **non-contrast head CT**.
- A **lumbar puncture (LP)** is the next critical diagnostic step to detect **xanthochromia** (due to bilirubin degradation from red blood cells) or elevated red blood cell count in the cerebrospinal fluid (CSF), which would confirm SAH.
- CT has approximately **95% sensitivity in the first 6 hours**, but sensitivity decreases over time, making LP essential when clinical suspicion remains high.
*Ultrasound*
- **Ultrasound** is not a standard diagnostic tool for acute neurological symptoms like severe headache or suspected SAH.
- It is primarily used for evaluating soft tissues, abdominal organs, and vascular structures like carotid arteries, but offers limited utility for intracranial bleeding.
*Alteplase*
- **Alteplase** (tissue plasminogen activator, tPA) is a thrombolytic agent used in acute ischemic stroke, characterized by focal neurological deficits due to arterial occlusion.
- Administering alteplase in the setting of headache and neck pain without focal deficits, while SAH is suspected, could be fatal as it would worsen bleeding.
*Ibuprofen, acetaminophen, metoclopramide, and diphenhydramine*
- This combination of medications is used for **symptomatic relief** of headache and nausea but does not address the underlying potentially life-threatening cause.
- Treating symptoms without a definitive diagnosis in suspected SAH could lead to delayed intervention and worse outcomes.
*MRI*
- While **MRI with specific sequences (FLAIR, GRE, SWI)** has high sensitivity for detecting SAH and is increasingly used in clinical practice, **lumbar puncture remains the traditional and most widely recommended next step** after a negative CT in suspected SAH.
- LP directly detects **xanthochromia** (present 6-12 hours after bleeding) and RBCs in CSF, providing definitive evidence of SAH.
- MRI may not always be readily available in the emergency setting, takes longer to perform, and requires patient stability and cooperation.
- For standardized exams, **LP is the classic correct answer** when CT is negative but clinical suspicion for SAH remains high.
Lumbar puncture technique and indications US Medical PG Question 6: A 56-year-old woman presents with sudden-onset severe headache, nausea, vomiting, and neck pain for the past 90 minutes. She describes her headache as a ‘thunderclap’, followed quickly by severe neck pain and stiffness, nausea and vomiting. She denies any loss of consciousness, seizure, or similar symptoms in the past. Her past medical history is significant for an episode 6 months ago where she suddenly had trouble putting weight on her right leg, which resolved within hours. The patient denies any history of smoking, alcohol or recreational drug use. On physical examination, the patient has significant nuchal rigidity. Her muscle strength in the lower extremities is 4/5 on the right and 5/5 on the left. The remainder of the physical examination is unremarkable. A noncontrast CT scan of the head is normal. Which of the following is the next best step in the management of this patient?
- A. Diffusion-weighted magnetic resonance imaging of the brain
- B. IV tPA
- C. Placement of a ventriculoperitoneal (VP) shunt
- D. T1/T2 MRI of the head
- E. Lumbar puncture (Correct Answer)
Lumbar puncture technique and indications Explanation: ***Lumbar puncture***
- A **thunderclap headache**, nuchal rigidity, nausea, and vomiting despite a normal noncontrast CT scan, is highly suspicious for **subarachnoid hemorrhage (SAH)**. A lumbar puncture is the next diagnostic step to look for **xanthochromia** or **red blood cells** in the cerebrospinal fluid.
- The previous episode of transient leg weakness could indicate a prior **warning leak** from an **aneurysm**, increasing the suspicion for SAH.
*Diffusion-weighted magnetic resonance imaging of the brain*
- This imaging is primarily used to detect **acute ischemic stroke**, which presents differently.
- While helpful for ischemic events, it is **not the primary diagnostic test** for suspected SAH after a normal CT.
*IV tPA*
- **Intravenous tissue plasminogen activator (IV tPA)** is a thrombolytic used in acute ischemic stroke, characterized by focal neurological deficits.
- It is **contraindicated** in SAH due to the significant risk of exacerbating intracranial bleeding.
*Placement of a ventriculoperitoneal (VP) shunt*
- A **VP shunt** is a surgical procedure to drain excess cerebrospinal fluid, typically used to treat **hydrocephalus**.
- This is a treatment for a complication (hydrocephalus) that may arise from SAH, but it is **not the initial diagnostic or management step** for an acute SAH.
*T1/T2 MRI of the head*
- While MRI can detect SAH, especially if performed with specific sequences (FLAIR), a **lumbar puncture is more sensitive for detecting SAH** when a CT scan is negative and clinical suspicion remains high.
- MRI is generally less accessible and more time-consuming than lumbar puncture in an emergency setting for suspected SAH.
Lumbar puncture technique and indications US Medical PG Question 7: A 48-year-old woman is brought to the emergency department because of a 1-hour history of sudden-onset headache associated with nausea and vomiting. The patient reports she was sitting at her desk when the headache began. The headache is global and radiates to her neck. She has hypertension. She has smoked one pack of cigarettes daily for the last 10 years. She drinks alcohol occasionally. Her father had a stroke at the age 58 years. Current medications include hydrochlorothiazide. She is in severe distress. She is alert and oriented to person, place, and time. Her temperature is 38.2°C (100.8°F), pulse is 89/min, respirations are 19/min, and blood pressure is 150/90 mm Hg. Cardiopulmonary examination shows no abnormalities. Cranial nerves II–XII are intact. She has no focal motor or sensory deficits. She flexes her hips and knees when her neck is flexed while lying in a supine position. A CT scan of the head is shown. Which of the following is the most appropriate intervention?
- A. Perform burr hole surgery
- B. Administer intravenous alteplase
- C. Administer intravenous vancomycin and ceftriaxone
- D. Perform surgical clipping (Correct Answer)
- E. Perform decompressive craniectomy
Lumbar puncture technique and indications Explanation: ***Perform surgical clipping***
- The clinical presentation of **sudden-onset severe headache** ("thunderclap headache"), **nausea, vomiting, neck stiffness (positive Brudzinski's sign)**, and the CT scan showing **blood in the subarachnoid space** strongly indicate a **subarachnoid hemorrhage (SAH)** from a ruptured cerebral aneurysm.
- Definitive treatment requires **securing the aneurysm** to prevent **rebleeding**, which carries 40-50% mortality. Modern management includes **endovascular coiling** (first-line for most cases) or **surgical clipping**.
- **Surgical clipping** involves placing a metal clip across the aneurysm neck to exclude it from circulation. It remains the preferred approach for certain aneurysm locations (MCA), wide-necked aneurysms, or when accompanied by hematoma requiring evacuation.
- Among the options provided, surgical clipping is the only definitive intervention that secures the ruptured aneurysm.
*Perform burr hole surgery*
- **Burr hole surgery** is used for draining **subdural hematomas** or accessing the brain for procedures like biopsy or external ventricular drain placement.
- While burr holes may be needed for complications of SAH (e.g., hydrocephalus requiring EVD), this is not the primary intervention for securing the ruptured aneurysm itself.
*Administer intravenous alteplase*
- **Alteplase** (tPA) is a **thrombolytic agent** used for **acute ischemic stroke** within 4.5 hours of symptom onset.
- Administering thrombolytics in **hemorrhagic stroke** (like SAH) is **absolutely contraindicated** as it would worsen bleeding and cause catastrophic neurological deterioration or death.
*Administer intravenous vancomycin and ceftriaxone*
- **Vancomycin and ceftriaxone** treat **bacterial meningitis**, which can present with headache, fever, and meningeal signs.
- Although the patient has low-grade fever (likely from blood irritating meninges, not infection) and neck stiffness, the **sudden-onset thunderclap headache** and **CT findings of SAH** make ruptured aneurysm the diagnosis, not meningitis. The fever in SAH is typically from aseptic meningeal irritation.
*Perform decompressive craniectomy*
- **Decompressive craniectomy** removes skull bone to relieve **elevated intracranial pressure** from massive brain swelling (severe TBI, malignant MCA infarction).
- While SAH can cause elevated ICP, craniectomy does not secure the aneurysm. The immediate priority is preventing **rebleeding** by securing the aneurysm source, not managing secondary complications.
Lumbar puncture technique and indications US Medical PG Question 8: A 62-year-old man is brought to the emergency department after his wife found him unresponsive 1 hour ago. He had fallen from a flight of stairs the previous evening. Four years ago, he underwent a mitral valve replacement. He has hypertension and coronary artery disease. Current medications include aspirin, warfarin, enalapril, metoprolol, and atorvastatin. On arrival, he is unconscious. His temperature is 37.3°C (99.1°F), pulse is 59/min, respirations are 7/min and irregular, and blood pressure is 200/102 mm Hg. The right pupil is 5 mm and fixed. The left pupil is 4 mm and reactive to light. There is extension of the extremities to painful stimuli. The lungs are clear to auscultation. Cardiac examination shows a systolic click. The abdomen is soft and nontender. He is intubated and mechanically ventilated. A mannitol infusion is begun. A noncontrast CT scan of the brain shows a 6-cm subdural hematoma on the right side with an 18-mm midline shift. Which of the following is the most likely early sequela of this patient's current condition?
- A. Multifocal myoclonus
- B. Right eye esotropia and elevation
- C. Bilateral lower limb paralysis
- D. Left-side facial nerve palsy
- E. Right-sided hemiplegia (Correct Answer)
Lumbar puncture technique and indications Explanation: ***Right-sided hemiplegia***
- The patient has a **right-sided subdural hematoma** causing **uncal herniation** with significant midline shift (18 mm).
- **Kernohan's notch phenomenon** is a false localizing sign where the contralateral cerebral peduncle (left side) is compressed against the edge of the tentorium cerebelli by the herniating brain.
- This contralateral peduncle compression paradoxically produces **ipsilateral hemiplegia** (same side as the lesion) - in this case, right-sided hemiplegia from a right-sided mass.
- This is an **early sequela** of severe herniation and represents a classic false localizing sign in neurosurgery.
*Multifocal myoclonus*
- This indicates widespread cortical irritability or **metabolic encephalopathy** (e.g., uremia, hypoxia, drug toxicity).
- Not a typical early focal sequela of subdural hematoma with uncal herniation.
- May occur later with diffuse hypoxic brain injury but is not the most likely early finding.
*Right eye esotropia and elevation*
- **Oculomotor nerve (CN III) palsy** causes the eye to be displaced "**down and out**" (exotropia and depression), not esotropia and elevation.
- The right fixed dilated pupil indicates CN III compression from uncal herniation, but this would cause lateral deviation and depression of the eye.
- The described eye position is inconsistent with CN III palsy.
*Bilateral lower limb paralysis*
- Would require **bilateral cerebral involvement** of motor cortices or **spinal cord injury**.
- A unilateral subdural hematoma, even with herniation, would not typically cause isolated bilateral lower limb paralysis as an early sequela.
- Not consistent with the focal nature of this injury.
*Left-side facial nerve palsy*
- While **contralateral hemiplegia** (left-sided weakness) would be expected from direct mass effect of a right-sided lesion, isolated facial nerve palsy is less likely.
- **Central facial palsy** (upper motor neuron) would affect the lower face and could occur contralaterally, but complete hemiplegia including the face would be more common than isolated CN VII palsy.
- Kernohan's notch phenomenon specifically affects the motor pathways in the cerebral peduncle, making ipsilateral hemiplegia the most characteristic early motor sequela.
Lumbar puncture technique and indications US Medical PG Question 9: A 48-year-old woman undergoes awake craniotomy for resection of a left frontal glioma near Broca's area. Intraoperatively, cortical mapping identifies eloquent tissue, but the tumor extends into functionally critical regions. The surgeon achieves 70% resection when the patient develops expressive aphasia during mapping. Frozen section shows low-grade astrocytoma. The family previously expressed desire for maximal resection. Evaluate the intraoperative decision-making.
- A. Use awake testing to define exact limits of safe resection
- B. Obtain family consultation intraoperatively about acceptable deficits
- C. Convert to asleep anesthesia and use anatomic landmarks for resection
- D. Continue resection since low-grade tumors justify aggressive surgery
- E. Stop resection to preserve language function (Correct Answer)
Lumbar puncture technique and indications Explanation: ***Stop resection to preserve language function***
- Development of **expressive aphasia** during mapping indicates the surgical margin has reached **eloquent cortex** (Broca's area), and proceeding further risks permanent neurological deficit.
- The principle of **"maximal safe resection"** prioritizes the preservation of **quality of life** and functional status over the total removal of a low-grade tumor.
*Use awake testing to define exact limits of safe resection*
- Awake testing and **cortical mapping** have already identified the limit by triggering aphasia; additional testing at that specific site is redundant and risks seizure or further injury.
- Once a **functional boundary** is identified via intraoperative monitoring, it serves as the definitive anatomical endpoint for the resection.
*Obtain family consultation intraoperatively about acceptable deficits*
- Surrogate decision-makers cannot provide **informed consent** for new, immediate neurological deficits in the middle of a procedure when the surgeon has reached a safety limit.
- The surgeon’s primary obligation is to maintain **patient safety** and adhere to the established surgical plan of functional preservation.
*Convert to asleep anesthesia and use anatomic landmarks for resection*
- Converting to **general anesthesia** would lose the benefit of **functional monitoring**, making any further resection near Broca's area extremely dangerous and blind to functional limits.
- **Anatomic landmarks** are often unreliable for predicting function due to **neuroplasticity** or tumor displacement, making mapping essential in this region.
*Continue resection since low-grade tumors justify aggressive surgery*
- While aggressive resection improves **progression-free survival**, the prognosis for **low-grade astrocytomas** is relatively long, making a permanent, devastating deficit like **aphasia** unacceptable.
- Aggressive surgery is only justified up to the **functional boundary**; crossing it violates the core surgical principle of avoiding non-recoverable morbidity.
Lumbar puncture technique and indications US Medical PG Question 10: A 25-year-old man with newly diagnosed glioblastoma multiforme undergoes gross total resection. Pathology confirms IDH-wild type, MGMT promoter unmethylated tumor. His parents want aggressive treatment, but oncology notes poor prognosis (median survival 12-15 months). The patient is engaged to be married and wants to prioritize quality of life. Radiation oncology recommends standard chemoradiation. Evaluate the most appropriate management approach considering prognostic factors and patient values.
- A. Clinical trial enrollment with experimental immunotherapy
- B. Palliative care referral with symptom management only
- C. Multidisciplinary meeting to align treatment with patient goals of care (Correct Answer)
- D. Standard Stupp protocol (radiation with concurrent and adjuvant temozolomide)
- E. Hypofractionated radiation alone to preserve quality of life
Lumbar puncture technique and indications Explanation: ***Multidisciplinary meeting to align treatment with patient goals of care***
- There is a significant conflict between the family's desire for **aggressive treatment** and the patient's focus on **quality of life**, necessitating a structured **shared decision-making** process.
- Given the poor prognosis of **IDH-wild type** and **MGMT-unmethylated** glioblastoma, a multidisciplinary approach ensures all specialists and the patient can reconcile medical options with personal life goals.
*Clinical trial enrollment with experimental immunotherapy*
- While a valid consideration for high-grade gliomas, it is not the immediate first step before establishing the overall **goals of care** with the patient.
- **Experimental therapies** often involve significant logistical burdens and side effects that may conflict with the patient's wish to prioritize his wedding and quality of life.
*Palliative care referral with symptom management only*
- Transitioning to **exclusive palliative care** may be premature as the patient is young, has had a gross total resection, and has not yet discussed potential lifespan-extending benefits of treatment.
- This approach ignores the possibility of combining radiation with supportive care to maintain **neurological function** and independence.
*Standard Stupp protocol (radiation with concurrent and adjuvant temozolomide)*
- The **Stupp protocol** is the standard of care, but its efficacy is significantly reduced in **MGMT-unmethylated** tumors because the tumor lacks the epigenetic silencing of the DNA repair enzyme.
- Proceeding with standard chemoradiation without highlighting the limited benefit and potential **toxicity** (fatigue, cytopenias) violates the patient's preference for quality-of-life-centered care.
*Hypofractionated radiation alone to preserve quality of life*
- **Hypofractionated radiation** is typically reserved for elderly patients or those with a poor **performance status**, rather than a fit 25-year-old.
- Selecting a treatment plan based solely on one factor before a comprehensive **multidisciplinary discussion** risks under-treating the patient or misaligning expectations.
More Lumbar puncture technique and indications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.