Intracranial pressure management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Intracranial pressure management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Intracranial pressure management US Medical PG Question 1: A 67-year-old man presents to the emergency department for a headache. The patient states his symptoms started thirty minutes ago. He states he experienced a sudden and severe headache while painting his house, causing him to fall off the ladder and hit his head. He has also experienced two episodes of vomiting and difficulty walking since the fall. The patient has a past medical history of hypertension, obesity, and atrial fibrillation. His current medications include lisinopril, rivaroxaban, atorvastatin, and metformin. His temperature is 99.5°F (37.5°C), blood pressure is 150/105 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. On physical exam, the patient localizes his headache to the back of his head. Cardiac exam reveals a normal rate and rhythm. Pulmonary exam reveals minor bibasilar crackles. Neurological exam is notable for minor weakness of the muscles of facial expression. Examination of cranial nerve three reveals a notable nystagmus. Heel to shin exam is abnormal bilaterally. The patient's gait is notably ataxic. A non-contrast CT scan of the head is currently pending. Which of the following is the most likely diagnosis?
- A. Pontine hemorrhage
- B. Cerebellar hemorrhage (Correct Answer)
- C. Subarachnoid hemorrhage
- D. Thalamic hemorrhage
- E. Subdural hematoma
Intracranial pressure management Explanation: ***Cerebellar hemorrhage***
- The sudden onset of a **severe headache**, localized to the back of the head, combined with **ataxia**, nystagmus, and minor facial weakness, in a patient on **anticoagulation** (rivaroxaban) for atrial fibrillation, strongly suggests a cerebellar hemorrhage.
- **Vomiting** and **difficulty walking** are common symptoms due to the cerebellar involvement and increased intracranial pressure.
*Pontine hemorrhage*
- Pontine hemorrhages typically present with **quadriplegia**, profound **coma**, and **pinpoint pupils**, which are not observed in this patient.
- While it can cause sudden headache and vomiting, the specific neurological deficits (ataxia, nystagmus, mild facial weakness) are less characteristic of a pontine lesion.
*Subarachnoid hemorrhage*
- Characterized by a **"thunderclap" headache** (sudden and severe), often described as the "worst headache of my life," and can cause focal neurological deficits depending on the location of rupture.
- While the sudden onset and severity fit, the specific cerebellar signs (**nystagmus**, **ataxia**, posterior headache) point more directly to a cerebellar lesion, and the fall causing head trauma suggests a hemorrhage within the brain parenchyma.
*Thalamic hemorrhage*
- Thalamic hemorrhages commonly present with **contralateral hemisensory loss**, hemiparesis, and sometimes pupillary abnormalities.
- The patient's presentation with prominent **ataxia**, nystagmus, and posterior headache is less typical for a thalamic hemorrhage.
*Subdural hematoma*
- Subdural hematomas usually result from **trauma** and can have a more **insidious onset** (especially chronic subdural hematomas in elderly or anticoagulated patients).
- While the fall might suggest this, the acute onset of severe headache and the specific neurological signs like **ataxia** and nystagmus are more indicative of an intraparenchymal hemorrhage (like cerebellar) rather than a subdural collection compressing the brain surface.
Intracranial pressure management US Medical PG Question 2: A 60-year-old male is admitted to the ICU for severe hypertension complicated by a headache. The patient has a past medical history of insulin-controlled diabetes, hypertension, and hyperlipidemia. He smokes 2 packs of cigarettes per day. He states that he forgot to take his medications yesterday and started getting a headache about one hour ago. His vitals on admission are the following: blood pressure of 160/110 mmHg, pulse 95/min, temperature 98.6 deg F (37.2 deg C), and respirations 20/min. On exam, the patient has an audible abdominal bruit. After administration of antihypertensive medications, the patient has a blood pressure of 178/120 mmHg. The patient reports his headache has increased to a 10/10 pain level, that he has trouble seeing, and he can't move his extremities. After stabilizing the patient, what is the best next step to diagnose the patient's condition?
- A. Doppler ultrasound of the carotids
- B. CT head with intravenous contrast
- C. MRI head without intravenous contrast
- D. CT head without intravenous contrast (Correct Answer)
- E. MRI head with intravenous contrast
Intracranial pressure management Explanation: ***CT head without intravenous contrast***
- The sudden onset of severe headache, visual disturbances, and neurological deficits (inability to move extremities), coupled with uncontrolled severe hypertension despite initial treatment, is highly suggestive of an **intracranial pathology**, most likely a **hemorrhagic stroke**.
- A **non-contrast CT scan of the head** is the **gold standard** for rapidly identifying acute intracranial hemorrhage, as it can be performed quickly and is readily available in emergency settings.
*Doppler ultrasound of the carotids*
- This test is primarily used to evaluate **carotid artery stenosis** due to atherosclerosis, which can lead to ischemic stroke.
- While the patient has risk factors for atherosclerosis, his acute presentation with severe central neurological symptoms points more towards an acute intracranial event rather than carotid disease.
*CT head with intravenous contrast*
- While a contrast CT can be useful for identifying tumors, abscesses, or vascular malformations, it is **contraindicated in the initial assessment of acute stroke** if an intracranial hemorrhage is suspected.
- Contrast can sometimes obscure subtle bleeds or complicate the interpretation of acute hemorrhage, and it also carries a risk of **contrast-induced nephropathy**, especially in a patient with diabetes.
*MRI head without intravenous contrast*
- An MRI provides superior soft tissue resolution compared to CT and is excellent for detecting ischemic strokes in later stages, as well as subtle hemorrhages, tumors, and other conditions.
- However, it is **less available, takes longer to perform**, and is often not the first choice in an acute neurological emergency where time is critical, particularly when differentiating between ischemic and hemorrhagic stroke.
*MRI head with intravenous contrast*
- Similar to a contrast CT, an MRI with contrast is generally **not the initial imaging choice for acute stroke** due to time constraints and the need to quickly rule out hemorrhage before considering contrast administration.
- Contrast agents for MRI, such as gadolinium, have their own risks, including **nephrogenic systemic fibrosis** in patients with renal impairment, which is a concern in a diabetic patient.
Intracranial pressure management US Medical PG Question 3: Which change in CSF production most directly affects intracranial pressure?
- A. Decreased arachnoid granulation function
- B. Increased choroid plexus blood flow
- C. Decreased carbonic anhydrase activity (Correct Answer)
- D. Increased osmotic gradient
Intracranial pressure management Explanation: ***Decreased carbonic anhydrase activity***
- The **choroid plexus** produces CSF primarily through an active secretion process involving carbonic anhydrase.
- Decreased activity of this enzyme directly reduces the formation of **bicarbonate ions** and **protons (H+)**, which are crucial for the active transport of Na+ and Cl- into the CSF, thereby lowering CSF production and subsequently **intracranial pressure**.
*Decreased arachnoid granulation function*
- This change would lead to a **decreased reabsorption** of CSF, which would *increase* intracranial pressure, not directly affect production to lower it.
- Arachnoid granulations are responsible for the **resorption of CSF** into the venous system.
*Increased choroid plexus blood flow*
- While increased blood flow could potentially increase the delivery of substrates for CSF production, it is **not the most direct or primary determinant** of CSF production rate.
- CSF production is predominantly an **active secretory process**, not a passive filtration process dependent solely on blood flow.
*Increased osmotic gradient*
- An increased osmotic gradient, if referring to a higher osmolality in the CSF compared to plasma, would tend to **draw water into the CSF**, potentially *increasing* CSF volume and intracranial pressure.
- If referring to a gradient drawing water *out* of the CSF, it would *decrease* intracranial pressure but is not a primary mechanism of CSF production regulation.
Intracranial pressure management US Medical PG Question 4: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Intracranial pressure management Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
Intracranial pressure management US Medical PG Question 5: A 27-year-old man presents to the emergency department after being hit by a car while riding his bike. The patient was brought in with his airway intact, vitals stable, and with a C-collar on. Physical exam is notable for bruising over the patient’s head and a confused man with a Glasgow coma scale of 11. It is noticed that the patient has a very irregular pattern of breathing. Repeat vitals demonstrate his temperature is 97.5°F (36.4°C), blood pressure is 172/102 mmHg, pulse is 55/min, respirations are 22/min and irregular, and oxygen saturation is 94% on room air. Which of the following interventions are most likely to improve this patient's vital signs?
- A. Head elevation, sedation, hypertonic saline, hypoventilation
- B. Lower head, sedation, hypertonic saline, hypoventilation
- C. Head elevation, sedation, mannitol, hyperventilation (Correct Answer)
- D. Head elevation, norepinephrine, mannitol, hyperventilation
- E. Lower head, sedation, hypertonic saline, hyperventilation
Intracranial pressure management Explanation: ***Head elevation, sedation, mannitol, hyperventilation***
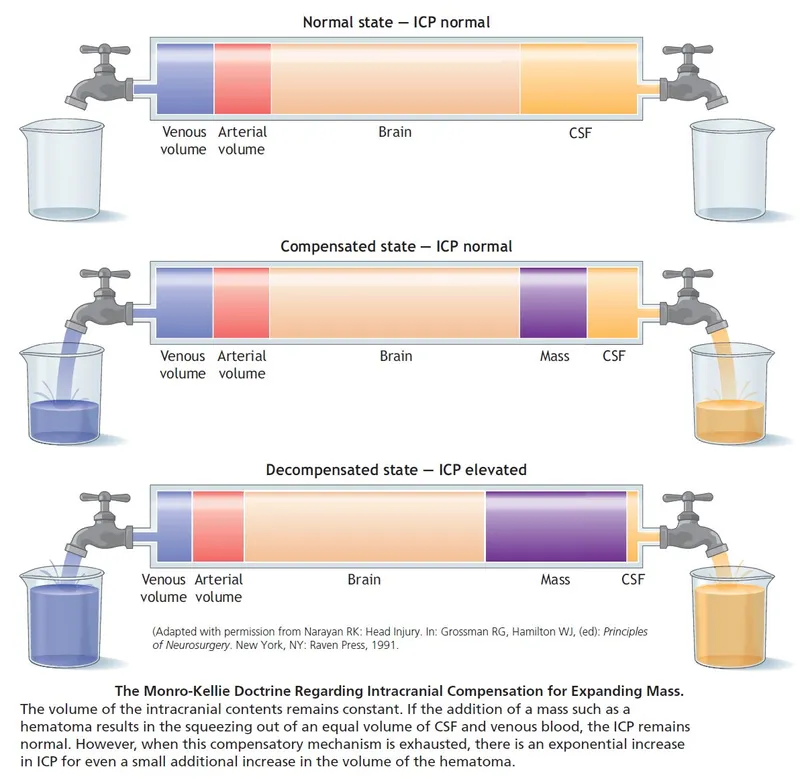
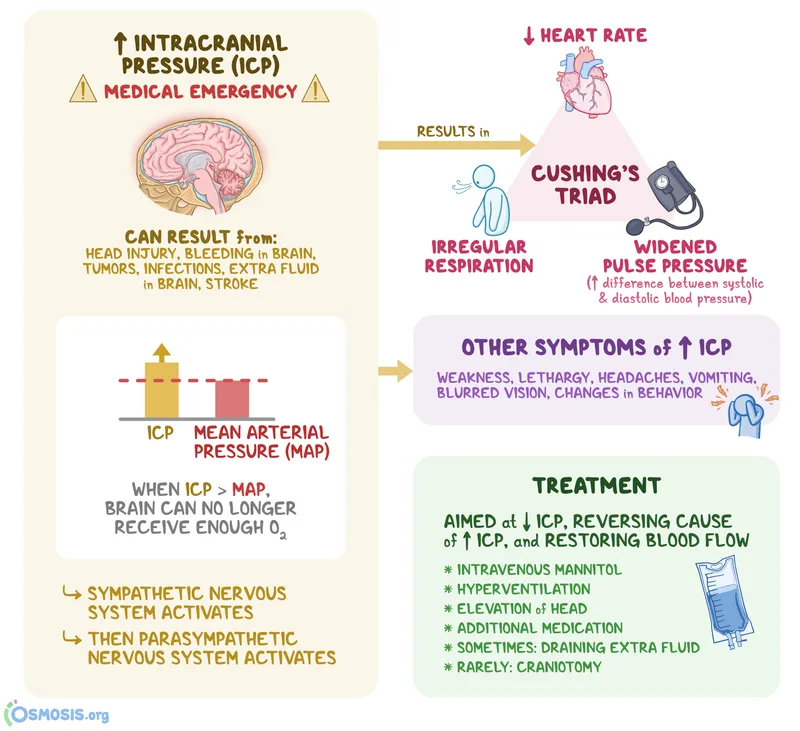
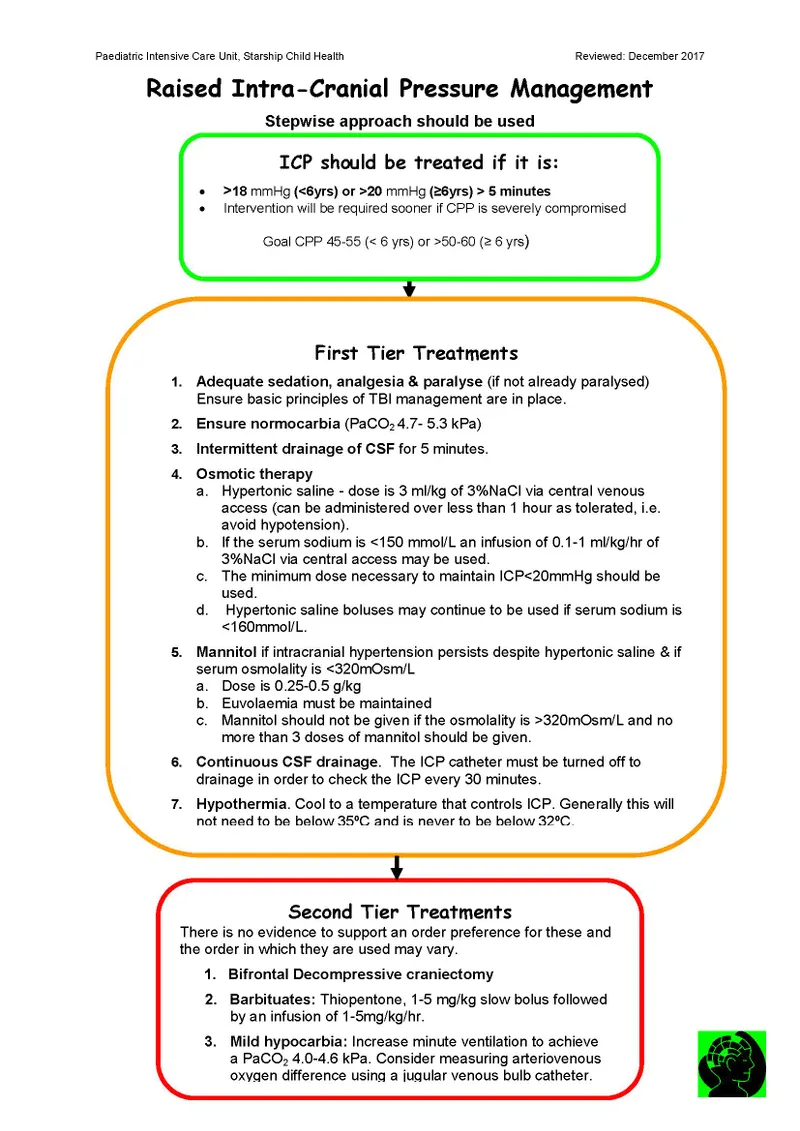
- This patient presents with signs of **increased intracranial pressure (ICP)**, indicated by **Cushing's triad** (hypertension, bradycardia, irregular respirations) and a decreased Glasgow Coma Scale (GCS) after head trauma. **Head elevation** to 30 degrees promotes venous outflow from the brain, reducing ICP.
- **Sedation** lowers metabolic demand and reduces agitation, which can otherwise increase ICP. **Mannitol** is an osmotic diuretic that rapidly draws fluid from the brain, decreasing cerebral edema. **Hyperventilation** temporarily reduces ICP by causing cerebral vasoconstriction through decreased pCO2.
*Head elevation, sedation, hypertonic saline, hypoventilation*
- While **head elevation**, **sedation**, and **hypertonic saline** (an alternative osmotic agent to mannitol) are appropriate for ICP management, **hypoventilation** would increase pCO2, causing cerebral vasodilation and worsening ICP.
- The combination of effective and ineffective ICP-reducing strategies makes this an incorrect option.
*Lower head, sedation, hypertonic saline, hypoventilation*
- **Lowering the head** would impede venous drainage from the brain and increase ICP, which is detrimental in this scenario.
- As mentioned, **hypoventilation** is contraindicated as it exacerbates cerebral edema and elevated ICP.
*Head elevation, norepinephrine, mannitol, hyperventilation*
- While **head elevation**, **mannitol**, and **hyperventilation** are appropriate, **norepinephrine** is primarily used to treat hypotension and maintain cerebral perfusion pressure (CPP) if blood pressure is dangerously low.
- In this case, the patient is hypertensive (**blood pressure 172/102 mmHg**), so norepinephrine would further increase blood pressure and ICP.
*Lower head, sedation, hypertonic saline, hyperventilation*
- **Lowering the head** is contraindicated as it directly increases ICP by hindering venous outflow from the brain.
- Although **sedation**, **hypertonic saline**, and **hyperventilation** are useful for ICP control, the incorrect positioning makes this option less suitable.
Intracranial pressure management US Medical PG Question 6: A 48-year-old woman is brought to the emergency department because of a 1-hour history of sudden-onset headache associated with nausea and vomiting. The patient reports she was sitting at her desk when the headache began. The headache is global and radiates to her neck. She has hypertension. She has smoked one pack of cigarettes daily for the last 10 years. She drinks alcohol occasionally. Her father had a stroke at the age 58 years. Current medications include hydrochlorothiazide. She is in severe distress. She is alert and oriented to person, place, and time. Her temperature is 38.2°C (100.8°F), pulse is 89/min, respirations are 19/min, and blood pressure is 150/90 mm Hg. Cardiopulmonary examination shows no abnormalities. Cranial nerves II–XII are intact. She has no focal motor or sensory deficits. She flexes her hips and knees when her neck is flexed while lying in a supine position. A CT scan of the head is shown. Which of the following is the most appropriate intervention?
- A. Perform burr hole surgery
- B. Administer intravenous alteplase
- C. Administer intravenous vancomycin and ceftriaxone
- D. Perform surgical clipping (Correct Answer)
- E. Perform decompressive craniectomy
Intracranial pressure management Explanation: ***Perform surgical clipping***
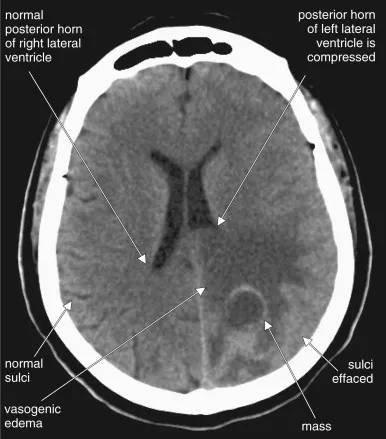
- The clinical presentation of **sudden-onset severe headache** ("thunderclap headache"), **nausea, vomiting, neck stiffness (positive Brudzinski's sign)**, and the CT scan showing **blood in the subarachnoid space** strongly indicate a **subarachnoid hemorrhage (SAH)** from a ruptured cerebral aneurysm.
- Definitive treatment requires **securing the aneurysm** to prevent **rebleeding**, which carries 40-50% mortality. Modern management includes **endovascular coiling** (first-line for most cases) or **surgical clipping**.
- **Surgical clipping** involves placing a metal clip across the aneurysm neck to exclude it from circulation. It remains the preferred approach for certain aneurysm locations (MCA), wide-necked aneurysms, or when accompanied by hematoma requiring evacuation.
- Among the options provided, surgical clipping is the only definitive intervention that secures the ruptured aneurysm.
*Perform burr hole surgery*
- **Burr hole surgery** is used for draining **subdural hematomas** or accessing the brain for procedures like biopsy or external ventricular drain placement.
- While burr holes may be needed for complications of SAH (e.g., hydrocephalus requiring EVD), this is not the primary intervention for securing the ruptured aneurysm itself.
*Administer intravenous alteplase*
- **Alteplase** (tPA) is a **thrombolytic agent** used for **acute ischemic stroke** within 4.5 hours of symptom onset.
- Administering thrombolytics in **hemorrhagic stroke** (like SAH) is **absolutely contraindicated** as it would worsen bleeding and cause catastrophic neurological deterioration or death.
*Administer intravenous vancomycin and ceftriaxone*
- **Vancomycin and ceftriaxone** treat **bacterial meningitis**, which can present with headache, fever, and meningeal signs.
- Although the patient has low-grade fever (likely from blood irritating meninges, not infection) and neck stiffness, the **sudden-onset thunderclap headache** and **CT findings of SAH** make ruptured aneurysm the diagnosis, not meningitis. The fever in SAH is typically from aseptic meningeal irritation.
*Perform decompressive craniectomy*
- **Decompressive craniectomy** removes skull bone to relieve **elevated intracranial pressure** from massive brain swelling (severe TBI, malignant MCA infarction).
- While SAH can cause elevated ICP, craniectomy does not secure the aneurysm. The immediate priority is preventing **rebleeding** by securing the aneurysm source, not managing secondary complications.
Intracranial pressure management US Medical PG Question 7: A 50-year-old woman presents with a severe headache and vomiting. She says that symptoms onset after attending a wine tasting at the local winery. She says that her headache is mostly at the back of her head and that she has been nauseous and vomited twice. Past medical history is significant for depression diagnosed 20 years ago but now well-controlled with medication. She also has significant vitamin D deficiency. Current medications are phenelzine and a vitamin D supplement. The patient denies any smoking history, alcohol or recreational drug use. On physical examination, the patient is diaphoretic. Her pupils are dilated. Which of the following is most likely to be elevated in this patient?
- A. Blood pressure (Correct Answer)
- B. Temperature
- C. Creatine phosphokinase
- D. Aspartate aminotransferase
- E. Serum creatinine
Intracranial pressure management Explanation: ***Blood pressure***
- The patient is taking **phenelzine**, a **monoamine oxidase inhibitor (MAOI)**. Consuming **tyramine-rich foods**, such as **wine** and fermented products, while on an MAOI can trigger a **hypertensive crisis**.
- Symptoms like severe headache (especially occipital), vomiting, diaphoresis, and dilated pupils are consistent with a **hypertensive crisis** induced by a **tyramine reaction**.
*Temperature*
- While fever can accompany a hypertensive crisis, it is not the most direct or consistently elevated vital sign in this specific scenario, which primarily describes symptoms related to **vasoconstriction** and **sympathetic overactivity**.
- Other conditions like **neuroleptic malignant syndrome** or **serotonin syndrome** are more typically associated with prominent hyperthermia, but the clinical picture here points more strongly to a tyramine reaction.
*Creatine phosphokinase*
- An elevated **creatine phosphokinase (CPK)** often indicates **muscle damage** or **rhabdomyolysis**. While severe hypertensive crises can sometimes lead to organ damage, CPK elevation is not a primary or immediate expected finding.
- This is more commonly elevated in conditions like **malignant hyperthermia**, **rhabdomyolysis**, or **myocardial infarction**, none of which are directly suggested by the initial presentation.
*Aspartate aminotransferase*
- **Aspartate aminotransferase (AST)** is an enzyme primarily associated with **liver damage**, although it can also be elevated in muscle or cardiac injury. There is no information in the vignette to suggest liver pathology.
- While severe organ damage can occur in prolonged or extreme hypertensive crises, **AST elevation** is not an immediate or characteristic feature of an acute **tyramine reaction**.
*Serum creatinine*
- **Serum creatinine** is a marker of **kidney function**. While kidney injury can occur in severe, prolonged hypertension, it is not an immediate finding expected during the acute onset of a **hypertensive crisis** from a tyramine reaction.
- There is no clinical information provided that would directly indicate immediate and significant renal impairment in this acute setting.
Intracranial pressure management US Medical PG Question 8: A 62-year-old man is brought to the emergency department after his wife found him unresponsive 1 hour ago. He had fallen from a flight of stairs the previous evening. Four years ago, he underwent a mitral valve replacement. He has hypertension and coronary artery disease. Current medications include aspirin, warfarin, enalapril, metoprolol, and atorvastatin. On arrival, he is unconscious. His temperature is 37.3°C (99.1°F), pulse is 59/min, respirations are 7/min and irregular, and blood pressure is 200/102 mm Hg. The right pupil is 5 mm and fixed. The left pupil is 4 mm and reactive to light. There is extension of the extremities to painful stimuli. The lungs are clear to auscultation. Cardiac examination shows a systolic click. The abdomen is soft and nontender. He is intubated and mechanically ventilated. A mannitol infusion is begun. A noncontrast CT scan of the brain shows a 6-cm subdural hematoma on the right side with an 18-mm midline shift. Which of the following is the most likely early sequela of this patient's current condition?
- A. Multifocal myoclonus
- B. Right eye esotropia and elevation
- C. Bilateral lower limb paralysis
- D. Left-side facial nerve palsy
- E. Right-sided hemiplegia (Correct Answer)
Intracranial pressure management Explanation: ***Right-sided hemiplegia***
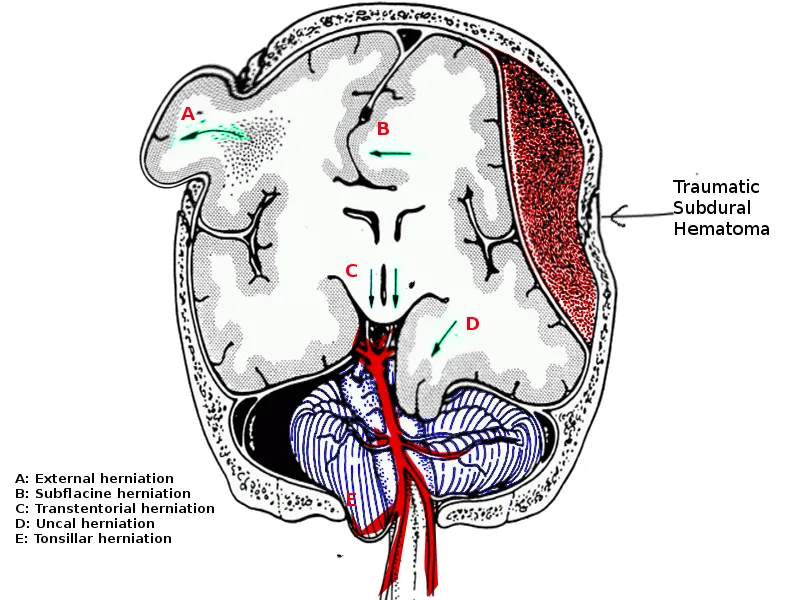
- The patient has a **right-sided subdural hematoma** causing **uncal herniation** with significant midline shift (18 mm).
- **Kernohan's notch phenomenon** is a false localizing sign where the contralateral cerebral peduncle (left side) is compressed against the edge of the tentorium cerebelli by the herniating brain.
- This contralateral peduncle compression paradoxically produces **ipsilateral hemiplegia** (same side as the lesion) - in this case, right-sided hemiplegia from a right-sided mass.
- This is an **early sequela** of severe herniation and represents a classic false localizing sign in neurosurgery.
*Multifocal myoclonus*
- This indicates widespread cortical irritability or **metabolic encephalopathy** (e.g., uremia, hypoxia, drug toxicity).
- Not a typical early focal sequela of subdural hematoma with uncal herniation.
- May occur later with diffuse hypoxic brain injury but is not the most likely early finding.
*Right eye esotropia and elevation*
- **Oculomotor nerve (CN III) palsy** causes the eye to be displaced "**down and out**" (exotropia and depression), not esotropia and elevation.
- The right fixed dilated pupil indicates CN III compression from uncal herniation, but this would cause lateral deviation and depression of the eye.
- The described eye position is inconsistent with CN III palsy.
*Bilateral lower limb paralysis*
- Would require **bilateral cerebral involvement** of motor cortices or **spinal cord injury**.
- A unilateral subdural hematoma, even with herniation, would not typically cause isolated bilateral lower limb paralysis as an early sequela.
- Not consistent with the focal nature of this injury.
*Left-side facial nerve palsy*
- While **contralateral hemiplegia** (left-sided weakness) would be expected from direct mass effect of a right-sided lesion, isolated facial nerve palsy is less likely.
- **Central facial palsy** (upper motor neuron) would affect the lower face and could occur contralaterally, but complete hemiplegia including the face would be more common than isolated CN VII palsy.
- Kernohan's notch phenomenon specifically affects the motor pathways in the cerebral peduncle, making ipsilateral hemiplegia the most characteristic early motor sequela.
Intracranial pressure management US Medical PG Question 9: A 17-year-old boy is brought to the emergency department by his brother after losing consciousness 1 hour ago. The brother reports that the patient was skateboarding outside when he fell on the ground and started to have generalized contractions. There was also some blood coming from his mouth. The contractions stopped after about 1 minute, but he remained unconscious for a few minutes afterward. He has never had a similar episode before. There is no personal or family history of serious illness. He does not smoke or drink alcohol. He does not use illicit drugs. He takes no medications. On arrival, he is confused and oriented only to person and place. He cannot recall what happened and reports diffuse muscle ache, headache, and fatigue. He appears pale. His temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 130/80 mm Hg. There is a small wound on the left side of the tongue. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference ranges. Toxicology screening is negative. An ECG shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Electroencephalography
- B. Lumbar puncture
- C. Lorazepam therapy
- D. Reassurance and follow-up
- E. CT scan of the head (Correct Answer)
Intracranial pressure management Explanation: ***CT scan of the head***
- Given the **first-time seizure** in an adolescent, especially with a history of head trauma (falling while skateboarding) and subsequent confusion, a **CT scan of the head** is crucial to rule out acute structural lesions like hemorrhage, mass, or edema.
- It is vital for identifying **life-threatening causes** of seizure that require immediate intervention, such as an **intracranial hematoma** or **mass lesion**, which could have been precipitated or exacerbated by the fall.
*Electroencephalography*
- **EEG** is appropriate for later evaluation to diagnose and classify seizure disorders, but it is not the *most appropriate initial step* in the emergency setting for a first-time seizure with a possible traumatic etiology.
- An EEG might be normal shortly after a seizure, and it does not rule out acute structural brain pathology that requires urgent management.
*Lumbar puncture*
- A **lumbar puncture** is indicated if there's suspicion of meningoencephalitis (e.g., fever, nuchal rigidity, immunocompromised status), which are not prominent features in this patient.
- The patient's vital signs are stable, and there are no signs of infection, making this a less urgent initial diagnostic step compared to imaging.
*Lorazepam therapy*
- **Lorazepam** is a benzodiazepine used to terminate ongoing seizures (**status epilepticus**), but this patient's generalized contractions have already stopped.
- Administering lorazepam when the seizure has resolved is unnecessary and would only cause further sedation.
*Reassurance and follow-up*
- While reassurance is part of patient care, it is *insufficient* as the sole next step for a **first-time seizure** episode in an adolescent, especially with features suggesting a possible underlying acute cause.
- A thorough diagnostic workup, beginning with neuroimaging, is necessary to ensure there is no serious underlying pathology before considering discharge and follow-up.
Intracranial pressure management US Medical PG Question 10: A 47-year-old man is admitted to the emergency room after a fight in which he was hit in the head with a hammer. The witnesses say that the patient initially lost consciousness, but regained consciousness by the time emergency services arrived. On admission, the patient complained of a diffuse headache. He opened his eyes spontaneously, was verbally responsive, albeit confused, and was able to follow commands. He could not elevate his left hand and leg. He did not remember the events prior to the loss of consciousness and had difficulty remembering information, such as the names of nurses or doctors. His airway was not compromised. The vital signs are as follows: blood pressure, 180/100 mm Hg; heart rate, 59/min; respiratory rate, 12/min; temperature 37.0℃ (98.6℉); and SaO2, 96% on room air. The examination revealed bruising in the right frontotemporal region. The pupils are round, equal, and show a poor response to light. The neurologic examination shows hyperreflexia and decreased power in the left upper and lower limbs. There is questionable nuchal rigidity, but no Kernig and Brudzinski signs. The CT scan is shown in the image. Which of the following options is recommended for this patient?
- A. Lumbar puncture
- B. Decompressive craniectomy
- C. Administration of levetiracetam
- D. Administration of methylprednisolone
- E. Surgical evacuation of the clots (Correct Answer)
Intracranial pressure management Explanation: ***Surgical evacuation of the clots***
- The CT scan image shows a **biconvex (lenticular) hyperdensity** consistent with an **epidural hematoma (EDH)**, which typically results from arterial bleeding (often from the **middle meningeal artery**). This patient's **"lucid interval"** (initial loss of consciousness, regain consciousness, then deterioration) is classic for EDH.
- Given the patient's neurological deterioration (left-sided weakness, pupillary changes, confusion, memory issues) and signs of increased intracranial pressure (hypertension, bradycardia - part of Cushing's triad), urgent surgical evacuation of the hematoma is indicated to relieve pressure and prevent herniation.
*Lumbar puncture*
- A lumbar puncture is **contraindicated** in the setting of suspected or confirmed **increased intracranial pressure (ICP)**, as it can precipitate **cerebral herniation**.
- The CT scan clearly demonstrates a space-occupying lesion, making a lumbar puncture unnecessary and potentially dangerous.
*Decompressive craniectomy*
- While decompressive craniectomy is a neurosurgical procedure used to reduce ICP, it is generally considered when other measures have failed or in cases of **diffuse brain swelling** or large **intracerebral hematomas** not amenable to simple evacuation.
- In this case of a localized epidural hematoma with a clear surgical target, direct evacuation is the primary and most effective intervention.
*Administration of levetiracetam*
- Levetiracetam is an **anticonvulsant** used to prevent seizures. While seizures can occur after traumatic brain injury, there is no indication that the patient is currently seizing.
- Prophylactic anticonvulsants are sometimes used in severe TBI, but addressing the life-threatening hematoma takes **precedence** over seizure prophylaxis.
*Administration of methylprednisolone*
- **Corticosteroids** like methylprednisolone are generally **contraindicated** in traumatic brain injury (TBI) as studies have shown **worse outcomes** and increased mortality.
- They are primarily used for their **anti-inflammatory effects** in conditions like spinal cord injury or vasogenic edema from tumors, not for acute head trauma with hematoma.
More Intracranial pressure management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.