Hydrocephalus diagnosis and shunt procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hydrocephalus diagnosis and shunt procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 1: A 25-year-old man with no significant past medical history is brought in by ambulance after a witnessed seizure at home. On physical exam, temperature is 102.3 deg F (39.1 deg C), blood pressure is 90/62 mmHg, pulse is 118/min, and respirations are 25/min. He is unable to touch his chin to his chest and spontaneously flexes his hips with passive neck flexion. Appropriate empiric treatment is begun. CT head is unremarkable, and a lumbar puncture sample is obtained. Gram stain of the cerebrospinal fluid (CSF) reveals gram-positive diplococci. Which of the following would you expect to see on CSF studies?
- A. Elevated opening pressure, elevated protein, normal glucose
- B. Normal opening pressure, normal protein, normal glucose
- C. Elevated opening pressure, elevated protein, elevated glucose
- D. Normal opening pressure, elevated protein, normal glucose
- E. Elevated opening pressure, elevated protein, low glucose (Correct Answer)
Hydrocephalus diagnosis and shunt procedures Explanation: ***Elevated opening pressure, elevated protein, low glucose***
- **Bacterial meningitis** typically presents with an **elevated opening pressure** due to inflammation and increased intracranial pressure.
- The inflammatory response leads to increased vascular permeability, causing **elevated protein** in the CSF and **low glucose** due to bacterial consumption.
*Elevated opening pressure, elevated protein, normal glucose*
- While **elevated opening pressure** and **elevated protein** can be seen in inflammatory conditions, **normal CSF glucose** is more characteristic of viral meningitis or non-infectious inflammatory conditions, not bacterial.
- In bacterial meningitis, bacteria metabolize glucose, leading to a **decreased CSF glucose level**.
*Normal opening pressure, normal protein, normal glucose*
- This profile is typical for a **normal CSF study** or certain chronic neurological conditions, not acute bacterial meningitis.
- The patient's severe symptoms, including fever, seizure, and meningismus, contradict a normal CSF profile.
*Elevated opening pressure, elevated protein, elevated glucose*
- While **elevated opening pressure** and **elevated protein** can occur, **elevated CSF glucose** is inconsistent with any common form of meningitis.
- An elevated CSF glucose is rare and would suggest systemic hyperglycemia without impaired glucose transport into the CSF.
*Normal opening pressure, elevated protein, normal glucose*
- A **normal opening pressure** would be unusual in a patient with bacterial meningitis, given the inflammation and potential for increased intracranial pressure.
- While **elevated protein** and **normal glucose** can occur in certain conditions (e.g., Guillain-Barré syndrome), it does not fit the clinical picture of acute bacterial meningitis with fever and meningismus.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 2: A 53-year-old man is brought to the emergency department for confusion. He was in his usual state of health until about 3 hours ago when he tried to use his sandwich to turn off the TV. He also complained to his wife that he had a severe headache. Past medical history is notable for hypertension, which has been difficult to control on multiple medications. His temperature is 36.7°C (98°F), the pulse is 70/min, and the blood pressure is 206/132 mm Hg. On physical exam he is alert and oriented only to himself, repeating over and over that his head hurts. The physical exam is otherwise unremarkable and his neurologic exam is nonfocal. The noncontrast CT scan of the patient's head is shown and reveals an acute intraparenchymal hemorrhage in the basal ganglia. Which of the following diagnostic tests would be most helpful in determining the underlying cause of this patient's hemorrhage?
- A. Lumbar puncture
- B. Electroencephalogram (EEG)
- C. MRI of the brain
- D. CT angiography of the neck
- E. CT angiography of the brain (Correct Answer)
Hydrocephalus diagnosis and shunt procedures Explanation: ***CT angiography of the brain***
- Following identification of an **intracerebral hemorrhage** on noncontrast CT, **CT angiography (CTA) of the brain** is the most appropriate next diagnostic test to identify underlying vascular abnormalities such as **arteriovenous malformations (AVMs)**, **aneurysms**, **dural arteriovenous fistulas**, or **moyamoya disease**.
- While this patient has severe hypertension (a common cause of basal ganglia hemorrhage), CTA should still be performed to rule out secondary causes, particularly in patients under 70 years old or those with atypical features.
- CTA can be performed rapidly in the acute setting and has high sensitivity for detecting vascular lesions that may require specific treatment.
*MRI of the brain*
- MRI with specialized sequences (GRE, SWI, FLAIR) can provide detailed information about **chronic microhemorrhages**, **cerebral amyloid angiopathy**, **underlying tumors**, or **cavernomas**.
- However, MRI is typically performed **after CTA** in the workup of intracerebral hemorrhage, not as the immediate next step.
- MRI is less readily available in the acute setting and takes longer to perform than CTA.
*CT angiography of the neck*
- This test visualizes the **carotid and vertebral arteries** in the neck to detect **stenosis**, **dissection**, or **atherosclerotic disease**.
- It is not directly useful for identifying the cause of an **intraparenchymal hemorrhage** within the brain substance itself.
*Lumbar puncture*
- Lumbar puncture analyzes **cerebrospinal fluid (CSF)** and is primarily used for suspected **subarachnoid hemorrhage** (when CT is negative), **meningitis**, or **encephalitis**.
- It is **contraindicated** in patients with significant intraparenchymal hemorrhage due to risk of herniation from increased intracranial pressure.
*Electroencephalogram (EEG)*
- EEG measures **electrical activity in the brain** and is used to diagnose **seizure disorders** or evaluate altered mental status from metabolic or epileptic causes.
- While confusion can result from seizures, the primary pathology is the **intracerebral hemorrhage** identified on CT, which EEG cannot diagnose or characterize.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 3: A 75-year-old female presents to your office with her daughter. The patient states that she feels perfectly well and that she does not know why she is present. The daughter states that over the last several years, the patient has become forgetful and recently forgot her grandchild's name, along with the groceries she was supposed to buy. She was also found lost 10 miles away from her house last week. The daughter also states that the patient has had urinary incontinence over the last few months and has been seeing little children in the morning that are not present. The patient denies any recent falls. Her vitals are normal and her physical exam does not reveal any focal neurological deficits. Her mini-mental status exam is scored 22/30. What is the most accurate test for this patient?
- A. CT angiography of head
- B. CT scan of head
- C. Lumbar puncture
- D. MRI scan of head (Correct Answer)
- E. PET scan of head
Hydrocephalus diagnosis and shunt procedures Explanation: ***MRI scan of head***
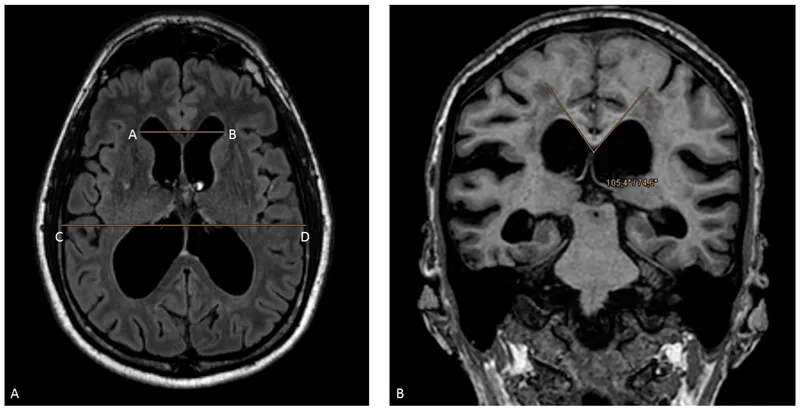
- An MRI scan of the head is the **most accurate initial test** to evaluate cognitive decline and rule out structural/reversible causes of dementia.
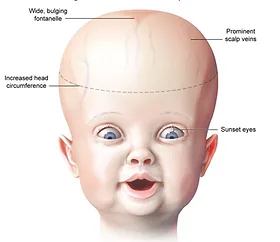
- This patient's presentation includes **progressive memory loss, disorientation, urinary incontinence, and visual hallucinations** - suggestive of **Lewy Body Dementia (LBD)** or potentially **Normal Pressure Hydrocephalus (NPH)**, though gait disturbance (a key NPH feature) is notably absent.
- MRI provides detailed visualization of **brain atrophy patterns**, **ventricular enlargement** (for NPH), **white matter lesions** (vascular dementia), **hippocampal atrophy** (Alzheimer's), and excludes other reversible causes like **subdural hematoma, tumor, or stroke**.
- **Must be performed first** before any invasive procedures like lumbar puncture.
*CT scan of head*
- A CT scan is useful for acute conditions like **hemorrhage, stroke, or mass lesions**, but it is **significantly less sensitive** than MRI for detecting subtle changes critical for dementia diagnosis.
- Cannot adequately visualize **cortical atrophy, hippocampal volume loss, or subtle white matter changes** that help differentiate dementia subtypes.
- While faster and more accessible, it is not the "most accurate" test for cognitive decline evaluation.
*CT angiography of head*
- CT angiography specifically visualizes **blood vessels** to detect **aneurysms, stenoses, or vascular malformations**.
- While vascular disease can contribute to dementia, this test does not evaluate the **brain parenchyma** or structural changes necessary for diagnosing neurodegenerative conditions.
- Not indicated as the initial test for cognitive impairment without focal vascular symptoms.
*Lumbar puncture*
- Lumbar puncture analyzes **cerebrospinal fluid (CSF)** for biomarkers (**amyloid-beta, tau, alpha-synuclein**), infection, or inflammation.
- It is an **invasive procedure** that should only be performed **after neuroimaging** to rule out increased intracranial pressure, hydrocephalus, or mass lesions.
- While useful for confirming specific dementia diagnoses (e.g., Alzheimer's or LBD biomarkers), it is a **second-line test**, not the initial most accurate diagnostic study.
*PET scan of head*
- PET imaging (FDG-PET or amyloid-PET) measures **metabolic activity** or **specific protein deposits** and is highly specific for certain dementias like **Alzheimer's disease** or **Frontotemporal dementia**.
- It is typically a **specialized second-line test** used after structural imaging when the diagnosis remains unclear.
- **More expensive and less available** than MRI, and not necessary as the initial most accurate test for broad cognitive impairment evaluation.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 4: A 5-year-old girl is brought to the emergency department after drinking a bottle of drain cleaner. It is unknown how much the child drank. She has a past medical history of Down syndrome and obesity. The patient's vitals are unremarkable. Physical exam is notable for a child in no acute distress. She is tolerating her oral secretions and interactive. Inspection of the oropharynx is unremarkable. Which of the following is appropriate management of this patient?
- A. Dilute hydrochloric acid
- B. Polyethylene glycol
- C. Observation
- D. Intubation
- E. Endoscopy (Correct Answer)
Hydrocephalus diagnosis and shunt procedures Explanation: ***Endoscopy***
- Due to the **inherent danger of caustic ingestion**, regardless of initial symptoms, **esophagogastroduodenoscopy (EGD)** is the gold standard for assessing the extent and severity of injury to the upper gastrointestinal tract. This procedure is crucial within the first 12-24 hours to guide further management.
- While the patient is asymptomatic, **caustic injuries** can progress and develop into strictures or perforations even without immediate obvious symptoms, making direct visualization essential.
*Dilute hydrochloric acid*
- **Neutralizing alkalis with acids** (or vice-versa) is contraindicated as it can cause an **exothermic reaction**, leading to further thermal injury and worsening the damage.
- Chemical neutralization can also produce gas, which increases the **risk of esophageal perforation**.
*Polyethylene glycol*
- **Polyethylene glycol (PEG)** is an osmotic laxative used for **bowel preparation** or as a treatment for constipation but has no role in the management of caustic ingestion.
- It would not remove the caustic substance from the esophagus or stomach, nor would it mitigate the chemical damage.
*Observation*
- Despite being asymptomatic initially, **caustic ingestions** can lead to delayed and severe complications such as **stricture formation**, perforation, and mediastinitis.
- **Asymptomatic presentation** does not rule out significant internal injury, particularly because the full extent of the ingestion is unknown, making observation alone an unsafe approach.
*Intubation*
- While airway compromise is a potential complication of caustic ingestion, the patient is currently in no acute distress and is tolerating oral secretions, indicating a **patent airway**.
- **Prophylactic intubation** is not indicated at this stage unless there are signs of respiratory distress, stridor, or significant oropharyngeal edema.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 5: A 52-year-old woman is accompanied by her husband to the emergency department with a severe occipital headache that started suddenly an hour ago. She is drowsy but able to answer the physician's questions. She describes it as the worst headache she has ever had, 9/10 in intensity. The husband says it was initially localized to the occiput but has now spread all over her head and she also complained of a generalized heaviness. She took an ibuprofen without experiencing any relief. She also complains of blurry vision and nausea and had 1 episode of vomiting. She denies a recent history of fever, chills, numbness, or seizures. Her past medical history is significant for hypertension controlled with lisinopril and metoprolol. On examination, she is drowsy but oriented. Papilledema is seen on ophthalmoscopy. Neck flexion is difficult and painful. The rest of the exam is unremarkable. Her blood pressure is 160/100 mm Hg, heart rate is 100/min, and temperature is 37.0°C (98.6°F). The ECG, cardiac enzymes, and laboratory studies are normal. Lumbar puncture results are as follows:
Opening pressure 210 mm H2O
RBC 50/mm3, numbers steady over 4 test tubes
Cell count 5/mm3
Glucose 60 mg/dL
Proteins 100 mg/dL
The patient is admitted to the ICU for further management. Which of the following is the most likely pathophysiology based on her history and CSF findings?
- A. Rupture of the communicating branches of the cerebral arteries (Correct Answer)
- B. Intracerebral bleed
- C. Viral infection of the brain parenchyma
- D. Bacterial infection of the meninges
- E. Trauma during lumbar puncture
Hydrocephalus diagnosis and shunt procedures Explanation: ***Rupture of the communicating branches of the cerebral arteries***
- This presentation, with a **sudden-onset, severe occipital headache ("thunderclap headache")**, meningeal irritation (stiff neck), blurry vision, papilledema, and elevated intracranial pressure (high opening pressure, nausea, vomiting), is highly classic for a **subarachnoid hemorrhage (SAH)**.
- The **CSF findings** of grossly bloody fluid with consistent red blood cells (RBCs) across multiple tubes (indicating true hemorrhage, not traumatic tap), elevated protein, and normal glucose are diagnostic of SAH. The most common cause of spontaneous SAH is the rupture of a **saccular (berry) aneurysm**, frequently found in the communicating branches of cerebral arteries.
*Intracerebral bleed*
- While an intracerebral bleed can cause severe headache and neurological deficits, it typically presents with **focal neurological signs** corresponding to the brain region affected by the hematoma.
- Classic CSF findings in an intracerebral bleed, unless it ruptures into the ventricles or subarachnoid space, would generally be **acellular or mildly pleocytic**, not overtly bloody with high RBC counts.
*Viral infection of the brain parenchyma*
- **Viral encephalitis** would typically present with fever, altered mental status, and often focal neurological deficits or seizures.
- CSF findings for viral encephalitis would show **lymphocytic pleocytosis**, mildly elevated protein, and normal glucose, not significant RBCs.
*Bacterial infection of the meninges*
- **Bacterial meningitis** is characterized by fever, neck stiffness, and altered mental status. The headache is usually progressive, not thunderclap.
- CSF analysis would typically show **neutrophilic pleocytosis**, markedly elevated protein, **low glucose**, and often visible bacteria on gram stain, unlike this patient's findings.
*Trauma during lumbar puncture*
- A **traumatic lumbar puncture** can cause blood in the CSF, but the RBC count would typically **decrease progressively** in subsequent tubes as less contaminated fluid is collected.
- The presence of **xanthochromia** (not explicitly mentioned but usually present in SAH after several hours) and the clinical presentation of a thunderclap headache, papilledema, and meningeal signs prior to the LP make a traumatic tap unlikely as the primary pathology.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 6: A 4-year-old boy is brought to the physician because of a progressive headache and neck pain for 2 weeks. During this period, he has had multiple episodes of dizziness and tingling sensations in his arms and hands. A year ago, he underwent closed reduction of a dislocated shoulder that he suffered after a fall. He underwent surgical removal of a sac-like protuberance on his lower back, soon after being born. His temperature is 36.7°C (98°F), pulse is 80/min, and blood pressure is 100/80 mm Hg. His neck is supple. Neurological examination shows sensorineural hearing loss bilaterally and normal gross motor function. Fundoscopy reveals bilateral optic disk swelling. An MRI of the brain is shown. Which of the following is the most likely cause of this patient's symptoms?
- A. Brachial plexus injury
- B. Vestibular schwannoma
- C. Chiari II malformation (Correct Answer)
- D. Medulloblastoma
- E. Intraventricular hemorrhage
Hydrocephalus diagnosis and shunt procedures Explanation: ***Chiari II malformation***
- The patient's history of surgical removal of a "sac-like protuberance" on his lower back soon after birth suggests a **myelomeningocele**, which is strongly associated with Chiari II malformation.
- Symptoms like progressive headache, neck pain, dizziness, tingling in arms/hands, bilateral optic disk swelling (indicating **increased intracranial pressure**), and sensorineural hearing loss are consistent with brainstem and cranial nerve compression common in Chiari II.
*Brachial plexus injury*
- This typically presents with acute, localized weakness, numbness, or pain in the arm and hand **due to nerve damage**, often following trauma like a dislocated shoulder.
- It would not explain the **progressive headache**, optic disc swelling, or the patient's congenital history of a lower back malformation.
*Vestibular schwannoma*
- This tumor primarily affects the **vestibulocochlear nerve (CN VIII)**, causing **unilateral hearing loss**, tinnitus, and balance issues.
- It would not typically present with bilateral hearing loss, increased intracranial pressure symptoms (like optic disc swelling), or be linked to a congenital spinal defect.
*Medulloblastoma*
- While a **medulloblastoma** can cause symptoms of increased intracranial pressure (headache, optic disc swelling) and sometimes dizziness, it is a **malignant brain tumor**.
- It does not explain the patient's history of a congenital spinal defect (myelomeningocele) or the specific tingling sensations in the arms and hands in the context of brainstem compression.
*Intraventricular hemorrhage*
- This usually occurs in **neonates, especially premature infants**, and presents with acute neurological deficits, apnea, bradycardia, or seizures.
- It is unlikely to present as progressive headache and neck pain in a 4-year-old and does not account for the congenital spinal defect or chronic symptoms.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 7: A 56-year-old male with a history of hepatitis C cirrhosis status post TIPS procedure is brought in by his wife to the emergency department because he has been acting disoriented, slurring his speech, and sleeping throughout the day. On arrival the patient is afebrile and his vital signs are pulse is 87/min, blood pressure is 137/93 mmHg, and respirations are 12/min with shallow breaths. Examination reveals a jaundiced male who appears older than stated age. Abdominal exam is positive for a fluid wave and shifting dullness to percussion. You note enlarged breasts, decreased facial hair, 3+ patellar reflexes bilaterally, and the following in the upper extremity (Image A). Paracentesis reveals ascitic fluid with neutrophil counts of < 100 cells/mcL. Serum creatinine is 1.0 and BUN is 15. Which of the following is the next best step in management?
- A. Administer neomycin and glucose
- B. IV albumin and antibiotic therapy with cefotaxime
- C. Administer rifaximin and glucose
- D. Administer lactulose (Correct Answer)
- E. Liver transplantation
Hydrocephalus diagnosis and shunt procedures Explanation: ***Administer lactulose***
- The patient exhibits classic symptoms of **hepatic encephalopathy** (disorientation, slurred speech, somnolence, asterixis as demonstrated by Image A), combined with findings consistent with **cirrhosis** (jaundice, ascites, gynecomastia, decreased facial hair, history of hepatitis C and TIPS).
- **Lactulose** is the first-line treatment for hepatic encephalopathy as it acidifies the colon, promoting the conversion of ammonia (a neurotoxin) to ammonium, which is then trapped and excreted in the feces.
*Administer neomycin and glucose*
- **Neomycin** is an antibiotic that can reduce ammonia-producing bacteria in the gut but is generally considered a second-line agent due to potential side effects like **ototoxicity** and **nephrotoxicity**.
- **Glucose** administration is not a primary treatment for hepatic encephalopathy; it would only be indicated if the patient were hypoglycemic, which is not suggested by the clinical picture.
*IV albumin and antibiotic therapy with cefotaxime*
- **IV albumin** is primarily used in **spontaneous bacterial peritonitis (SBP)** to prevent hepatorenal syndrome, and the paracentesis finding of < 100 cells/mcL neutrophils suggests SBP is unlikely.
- **Cefotaxime** is an appropriate antibiotic for **SBP**, but the patient's presentation is more consistent with hepatic encephalopathy, not an active infection.
*Administer rifaximin and glucose*
- **Rifaximin** is a non-absorbable antibiotic used to reduce ammonia-producing bacteria in the gut, often as an add-on or alternative to lactulose for maintenance therapy or in cases unresponsive to lactulose alone. It is not generally the initial monotherapy for an acute, severe encephalopathy episode.
- As mentioned, **glucose** is not a primary treatment for hepatic encephalopathy.
*Liver transplantation*
- **Liver transplantation** is a definitive treatment for end-stage liver disease, but it is not the **next best step** for acute management of hepatic encephalopathy.
- The immediate priority is to address the acute encephalopathy episode pharmacologically before considering long-term solutions like transplantation, which has a complex workup and waiting list.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 8: A 9-year-old girl is admitted to the hospital with a one-day history of acute abdominal pain and vomiting. She also has a two-day history of fever, headache, and neck pain. Her immunizations are up-to-date. She is confused and oriented only to place and person. Her temperature is 39.7°C (103.5°F), pulse is 148/min, blood pressure is 90/50 mm Hg, and respiratory rate is 28/min. Cervical range of motion is limited by pain. The remainder of the neurologic examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.9 g/dL
Leukocyte count 44,000/mm3
Serum
pH 7.33
Na+ 130 mEq/L
Cl- 108 mEq/L
K+ 6.1 mEq/L
HCO3- 20 mEq/L
Urea nitrogen 34 mg/dL
Glucose 180 mg/dL
Creatinine 2.4 mg/dL
Urine ketones negative
A CT scan of the head shows enhancement of the arachnoid and pia mater. Cerebrospinal fluid analysis shows a leukocyte count of 3,400/μL (90% neutrophils), a glucose concentration of 50 mg/dL, protein concentration of 81 mg/dL, and no erythrocytes. Gram stain of the CSF shows gram-negative diplococci. This patient is at increased risk for which of the following complications?
- A. Vesicular skin eruptions
- B. Adrenal hemorrhage (Correct Answer)
- C. Pancreatitis
- D. Temporal lobe inflammation
- E. Deep neck abscess
Hydrocephalus diagnosis and shunt procedures Explanation: **Adrenal hemorrhage**
- The clinical picture of **fever, acute abdominal pain, confusion, hypotension, and a high WBC count (44,000/mm³)**, along with **Gram-negative diplococci in CSF**, indicates **meningococcal meningitis with sepsis**. This rapidly progressive infection by *Neisseria meningitidis* can lead to **Waterhouse-Friderichsen syndrome**, characterized by **adrenal hemorrhage** and profound shock.
- The **elevated potassium (6.1 mEq/L)** and **hyponatremia (130 mEq/L)** are consistent with **adrenal insufficiency** resulting from adrenal hemorrhage.
*Vesicular skin eruptions*
- **Vesicular skin eruptions** are characteristic of viral infections such as **herpes simplex virus (HSV)** or **varicella-zoster virus**, which would present differently (e.g., HSV encephalitis often causes temporal lobe involvement).
- While various infections can cause skin rashes, this specific presentation with extensive meningeal inflammation and septic shock points away from typical vesicular eruptions.
*Pancreatitis*
- **Pancreatitis** is characterized by severe epigastric pain radiating to the back, often with nausea and vomiting, and elevated lipase/amylase. While **abdominal pain** is present, other symptoms like **neck stiffness, confusion, and CSF findings of bacterial meningitis** are not typical for pancreatitis.
- There is no specific evidence, such as imaging findings or elevated pancreatic enzymes, to suggest pancreatitis in this case.
*Temporal lobe inflammation*
- **Temporal lobe inflammation** is a hallmark of **HSV encephalitis**, which often presents with seizures, bizarre behavior, and specific MRI findings in the temporal lobes. While a CT scan showed arachnoid and pia mater enhancement, this indicates **meningeal inflammation**, not specifically temporal lobe parenchymal inflammation (encephalitis).
- The presence of **Gram-negative diplococci in the CSF** strongly indicates bacterial meningitis, not viral encephalitis, making temporal lobe inflammation less likely.
*Deep neck abscess*
- A **deep neck abscess** would typically cause localized neck pain, swelling, dysphagia, and stridor, potentially with fever, but would not explain the widespread CNS symptoms (confusion, meningeal signs, CSF findings) or systemic signs of shock and coagulopathy seen here.
- While the patient has neck pain, it is due to **meningismus**, not a localized abscess, and there is no mention of local swelling or airway compromise.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 9: A 62-year-old man is brought to the emergency department after his wife found him unresponsive 1 hour ago. He had fallen from a flight of stairs the previous evening. Four years ago, he underwent a mitral valve replacement. He has hypertension and coronary artery disease. Current medications include aspirin, warfarin, enalapril, metoprolol, and atorvastatin. On arrival, he is unconscious. His temperature is 37.3°C (99.1°F), pulse is 59/min, respirations are 7/min and irregular, and blood pressure is 200/102 mm Hg. The right pupil is 5 mm and fixed. The left pupil is 4 mm and reactive to light. There is extension of the extremities to painful stimuli. The lungs are clear to auscultation. Cardiac examination shows a systolic click. The abdomen is soft and nontender. He is intubated and mechanically ventilated. A mannitol infusion is begun. A noncontrast CT scan of the brain shows a 6-cm subdural hematoma on the right side with an 18-mm midline shift. Which of the following is the most likely early sequela of this patient's current condition?
- A. Multifocal myoclonus
- B. Right eye esotropia and elevation
- C. Bilateral lower limb paralysis
- D. Left-side facial nerve palsy
- E. Right-sided hemiplegia (Correct Answer)
Hydrocephalus diagnosis and shunt procedures Explanation: ***Right-sided hemiplegia***
- The patient has a **right-sided subdural hematoma** causing **uncal herniation** with significant midline shift (18 mm).
- **Kernohan's notch phenomenon** is a false localizing sign where the contralateral cerebral peduncle (left side) is compressed against the edge of the tentorium cerebelli by the herniating brain.
- This contralateral peduncle compression paradoxically produces **ipsilateral hemiplegia** (same side as the lesion) - in this case, right-sided hemiplegia from a right-sided mass.
- This is an **early sequela** of severe herniation and represents a classic false localizing sign in neurosurgery.
*Multifocal myoclonus*
- This indicates widespread cortical irritability or **metabolic encephalopathy** (e.g., uremia, hypoxia, drug toxicity).
- Not a typical early focal sequela of subdural hematoma with uncal herniation.
- May occur later with diffuse hypoxic brain injury but is not the most likely early finding.
*Right eye esotropia and elevation*
- **Oculomotor nerve (CN III) palsy** causes the eye to be displaced "**down and out**" (exotropia and depression), not esotropia and elevation.
- The right fixed dilated pupil indicates CN III compression from uncal herniation, but this would cause lateral deviation and depression of the eye.
- The described eye position is inconsistent with CN III palsy.
*Bilateral lower limb paralysis*
- Would require **bilateral cerebral involvement** of motor cortices or **spinal cord injury**.
- A unilateral subdural hematoma, even with herniation, would not typically cause isolated bilateral lower limb paralysis as an early sequela.
- Not consistent with the focal nature of this injury.
*Left-side facial nerve palsy*
- While **contralateral hemiplegia** (left-sided weakness) would be expected from direct mass effect of a right-sided lesion, isolated facial nerve palsy is less likely.
- **Central facial palsy** (upper motor neuron) would affect the lower face and could occur contralaterally, but complete hemiplegia including the face would be more common than isolated CN VII palsy.
- Kernohan's notch phenomenon specifically affects the motor pathways in the cerebral peduncle, making ipsilateral hemiplegia the most characteristic early motor sequela.
Hydrocephalus diagnosis and shunt procedures US Medical PG Question 10: A 77-year-old man is brought to the emergency department by his wife because of headache, nausea, and vomiting for 24 hours. His wife says that over the past 2 weeks, he has been more irritable and has had trouble remembering to do routine errands. Two weeks ago, he fell during a skiing accident but did not lose consciousness. He has coronary artery disease and hypertension. He has smoked one pack of cigarettes daily for 50 years. He has had 2 glasses of wine daily since his retirement 10 years ago. Current medications include atenolol, enalapril, furosemide, atorvastatin, and aspirin. He appears acutely ill. He is oriented to person but not to place or time. His temperature is 37°C (98.6°F), pulse is 99/min, respirations are 16/min, and blood pressure is 160/90 mm Hg. During the examination, he is uncooperative and unable to answer questions. Deep tendon reflexes are 4+ on the left and 2+ on the right. Babinski's sign is present on the left. There is mild weakness of the left iliopsoas and hamstring muscles. A CT scan of the head without contrast shows a high-density, 15-mm crescentic collection across the right hemispheric convexity. Which of the following is the most appropriate next step in the management of this patient?
- A. Recombinant tissue plasminogen activator administration
- B. Obtain an Electroencephalography
- C. Obtain an MRI of the head
- D. Surgical evacuation (Correct Answer)
- E. Observation
Hydrocephalus diagnosis and shunt procedures Explanation: ***Surgical evacuation***
- The CT scan reveals a **high-density, crescentic collection**, strongly indicative of an **acute subdural hematoma**, which is causing significant neurological deficits and mass effect (e.g., increased intracranial pressure symptoms like headache, nausea, vomiting, and altered mental status, and focal neurological signs).
- Given the patient's **acute neurological decline**, significant mass effect from the 15-mm hematoma, and age, prompt **surgical evacuation** is the definitive treatment to relieve pressure and prevent further brain injury.
*Recombinant tissue plasminogen activator administration*
- **tPA** is indicated for **acute ischemic stroke**, not hemorrhagic stroke or subdural hematoma. Administering tPA in this context would be harmful, potentially worsening the hemorrhage.
- The patient's CT scan clearly shows a **hemorrhagic lesion**, not an ischemic event.
*Obtain an Electroencephalography*
- **EEG** is primarily used to evaluate **seizure disorders** or certain types of encephalopathy. While the patient has altered mental status, the primary issue identified on CT is a subdural hematoma requiring immediate intervention.
- EEG would not provide information relevant to the immediate management of an **acute subdural hematoma**.
*Obtain an MRI of the head*
- An **MRI** can provide more detailed imaging, but in the context of an **acute subdural hematoma** with significant neurological compromise, it would delay crucial and time-sensitive surgical intervention.
- The **CT scan** has already provided sufficient diagnostic information to warrant immediate surgical planning.
*Observation*
- **Observation** is not appropriate for a patient with a rapidly expanding **acute subdural hematoma** causing significant neurological deficits and a 15-mm collection, especially given the patient's age and clinical presentation.
- Delaying treatment would likely lead to further neurological deterioration, **herniation**, and potentially death.
More Hydrocephalus diagnosis and shunt procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.