Craniotomy indications and techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Craniotomy indications and techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Craniotomy indications and techniques US Medical PG Question 1: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Craniotomy indications and techniques Explanation: ***Prions***
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
Craniotomy indications and techniques US Medical PG Question 2: A 68-year-old man is brought to the emergency department because of a severe headache, nausea, and vomiting for 30 minutes. Forty-five minutes ago, he fell and struck his head, resulting in loss of consciousness for 1 minute. After regaining consciousness, he felt well for 15 minutes before the headache began. On arrival, the patient becomes rigid and his eyes deviate to the right; he is incontinent of urine. Intravenous lorazepam is administered and the rigidity resolves. Which of the following is the most likely cause of the patient's condition?
- A. Rupture of bridging veins
- B. Cerebrospinal fluid production/absorption mismatch
- C. Acute insufficiency of cerebral blood flow
- D. Bleeding between dura mater and skull (Correct Answer)
- E. Intracerebral hemorrhage
Craniotomy indications and techniques Explanation: ***Bleeding between dura mater and skull***
- The classic presentation of an **epidural hematoma** includes a brief **loss of consciousness** followed by a **lucent interval** (patient feeling well) and then rapid neurological deterioration with symptoms like **severe headache**, **nausea**, **vomiting**, and **seizures** due to increasing intracranial pressure.
- This type of bleeding is typically arterial, usually from the **middle meningeal artery**, and occurs between the dura mater and the inner table of the skull.
*Rupture of bridging veins*
- This describes a **subdural hematoma**, which usually results in a more gradual onset of symptoms due to slower venous bleeding, often over days to weeks.
- While a fall can cause it, the rapid deterioration after a lucid interval is less typical for a subdural hematoma.
*Cerebrospinal fluid production/absorption mismatch*
- This mechanism is associated with conditions like **hydrocephalus** or **idiopathic intracranial hypertension**, which typically present with a more gradual onset of symptoms such as chronic headache, visual changes, or gait disturbances.
- It does not account for an acute traumatic event, loss of consciousness, and rapid deterioration seen in this patient.
*Acute insufficiency of cerebral blood flow*
- This typically refers to an **ischemic stroke** or **transient ischemic attack (TIA)**, where symptoms arise from a lack of oxygenated blood to brain regions.
- While it can cause neurological deficits, the history of head trauma, lucid interval, and rapid progression to severe symptoms and seizures points away from a primary ischemic event.
*Intracerebral hemorrhage*
- This involves bleeding within the **brain parenchyma** itself, which can present acutely with headache, vomiting, and neurological deficits.
- However, the distinct **lucid interval** following initial loss of consciousness, as described, is much more characteristic of an **epidural hematoma** rather than bleeding directly into the brain tissue.
Craniotomy indications and techniques US Medical PG Question 3: Four days after being hospitalized, intubated, and mechanically ventilated, a 30-year-old man has no cough response during tracheal suctioning. He was involved in a motor vehicle collision and was obtunded on arrival in the emergency department. The ventilator is at a FiO2 of 100%, tidal volume is 920 mL, and positive end-expiratory pressure is 5 cm H2O. He is currently receiving vasopressors. His vital signs are within normal limits. The pupils are dilated and nonreactive to light. Corneal, gag, and oculovestibular reflexes are absent. There is no facial or upper extremity response to painful stimuli; the lower extremities show a triple flexion response to painful stimuli. Serum concentrations of electrolytes, urea, creatinine, and glucose are within the reference range. Arterial blood gas shows:
pH 7.45
pCO2 41 mm Hg
pO2 99 mm Hg
O2 saturation 99%
Two days ago, a CT scan of the head showed a left intracerebral hemorrhage with mass effect. The apnea test is positive. There are no known family members, advanced directives, or individuals with power of attorney. Which of the following is the most appropriate next step in management?
- A. Ethics committee consultation (Correct Answer)
- B. Remove the ventilator
- C. Court order for further management
- D. Repeat CT scan of the head
- E. Cerebral angiography
Craniotomy indications and techniques Explanation: ***Ethics committee consultation***
- The patient meets criteria for **brain death**, but there are no family members or advance directives to guide end-of-life decisions. An **ethics committee consultation** is essential to navigate the complex legal and ethical implications of withdrawing life support in such a situation.
- The committee can provide guidance on hospital policies, relevant laws, and ethical principles to ensure a decision that respects the patient's presumed wishes and societal values, especially given the absence of surrogates.
*Remove the ventilator*
- While the patient appears to meet the criteria for **brain death**, premature withdrawal of the ventilator without proper legal and ethical guidance is inappropriate, especially given the lack of identified next of kin or advance directives.
- A formal process, including definitive declaration of brain death by two separate physicians and addressing legal and ethical considerations, must precede such an action.
*Court order for further management*
- A court order might be necessary if there are intractable disagreements among stakeholders or if brain death cannot be definitively declared. However, an **ethics committee consult** is typically the initial step to resolve complex cases lacking surrogate decision-makers before escalating to legal action.
- Seeking a court order is a more extreme measure usually reserved when internal hospital mechanisms and ethical consultations fail to provide a clear path forward.
*Repeat CT scan of the head*
- A repeat CT scan would typically be performed to assess changes in the intracerebral hemorrhage or mass effect if there were signs of ongoing neurological deterioration that might be reversible, or to guide surgical intervention.
- However, in this patient, the clinical picture, including absent brainstem reflexes and a positive apnea test indicating **brain death**, suggests that further imaging for diagnostic purposes related to hemorrhage progression is unlikely to alter the prognosis or management related to end-of-life decisions.
*Cerebral angiography*
- **Cerebral angiography** is used to assess cerebral blood flow and can be a confirmatory test for brain death if clinical examination and apnea testing are inconclusive, especially in cases where sedative medications might confound the clinical picture.
- In this case, the comprehensive clinical examination and positive apnea test strongly suggest brain death, making angiography unnecessary at this stage, particularly without surrogate decision-makers.
Craniotomy indications and techniques US Medical PG Question 4: A six-month-old male presents to the pediatrician for a well-child visit. The patient’s mother is concerned about the patient’s vision because he often turns his head to the right. She has begun trying to correct the head turn and places him on his back with his head turned in the opposite direction to sleep, but she has not noticed any improvement. She is not certain about when the head turning began and denies any recent fever. She reports that the patient fell off the bed yesterday but was easily soothed afterwards. The patient is otherwise doing well and is beginning to try a variety of solid foods. The patient is sleeping well at night. He is beginning to babble and can sit with support. The patient was born at 37 weeks gestation via cesarean delivery for breech positioning. On physical exam, the patient’s head is turned to the right and tilted to the left. There is some minor bruising on the posterior aspect of the head and over the sternocleidomastoid. He has no ocular abnormalities and is able to focus on his mother from across the room. Which of the following is the best next step in management?
- A. Neck radiograph
- B. Direct laryngoscopy
- C. Reassurance and follow-up in one month
- D. Referral to ophthalmology
- E. Referral to physical therapy (Correct Answer)
Craniotomy indications and techniques Explanation: ***Referral to physical therapy***
- The infant presents with a persistent head turn and tilt, consistent with **congenital muscular torticollis**, which is often associated with breech presentation. **Physical therapy** is the primary treatment to stretch the sternocleidomastoid muscle and improve range of motion.
- The minor bruising on the sternocleidomastoid could be due to parental attempts to reposition the head and the recent fall, but the underlying issue of torticollis requires therapeutic intervention.
*Neck radiograph*
- While a neck radiograph might be considered if **skeletal abnormalities** are suspected, the clinical presentation strongly suggests muscular torticollis, not a spinal bone issue.
- There are no red flags for **osseous cervical spine anomalies** such as neurological deficits, significant trauma, or suspicion of congenital vertebral malformations, making this initial step less appropriate.
*Direct laryngoscopy*
- This procedure is used to examine the **larynx and vocal cords** and is irrelevant to the presented symptoms of head turn and tilt.
- There is no mention of **stridor, dysphagia, or respiratory distress** that would warrant a direct laryngoscopy.
*Reassurance and follow-up in one month*
- Although torticollis can sometimes resolve spontaneously, the persistent nature of the head turn, parental concern, and potential for **developmental delays** if left untreated make simple reassurance inappropriate.
- Delaying intervention could lead to **facial asymmetry, plagiocephaly**, or impaired motor development.
*Referral to ophthalmology*
- Ocular abnormalities can cause a compensatory head turn (**ocular torticollis**), however, the patient's eyes are described as normal, and he is able to focus, making a primary ophthalmological problem unlikely.
- The presence of bruising over the sternocleidomastoid points more towards a **musculoskeletal origin** rather than ocular.
Craniotomy indications and techniques US Medical PG Question 5: A 78-year-old man is brought in to the emergency department by ambulance after his wife noticed that he began slurring his speech and had developed facial asymmetry during dinner approximately 30 minutes ago. His past medical history is remarkable for hypertension and diabetes. His temperature is 99.1°F (37.3°C), blood pressure is 154/99 mmHg, pulse is 89/min, respirations are 12/min, and oxygen saturation is 98% on room air. Neurologic exam reveals right upper and lower extremity weakness and an asymmetric smile. Which of the following is the next best step in management?
- A. Alteplase
- B. MRI brain
- C. CT head (Correct Answer)
- D. Aspirin
- E. CTA head
Craniotomy indications and techniques Explanation: ***CT head***
- A **non-contrast CT head** is the immediate priority to differentiate between ischemic and hemorrhagic stroke, which is critical for guiding subsequent treatment decisions.
- Given the patient's acute neurological deficits (slurred speech, facial asymmetry, weakness) and vascular risk factors (hypertension, diabetes), **stroke is highly suspected**, and identifying intracerebral hemorrhage is crucial before considering thrombolytic therapy.
*Alteplase*
- **Alteplase** (tPA) is a thrombolytic agent used for acute ischemic stroke, but its administration is **contraindicated in hemorrhagic stroke**.
- Initiating alteplase without first ruling out hemorrhage with a CT scan could lead to catastrophic bleeding.
*MRI brain*
- While an **MRI brain** can provide more detailed imaging of stroke, it is typically **not the initial imaging modality** in the emergency setting due to longer acquisition times and limited availability, especially when emergent differentiation between ischemic and hemorrhagic stroke is needed.
- Its use is usually reserved for cases where the CT is inconclusive or for later evaluation.
*Aspirin*
- **Aspirin** is an antiplatelet agent used in the management of ischemic stroke, but it should **not be given until a hemorrhagic stroke has been ruled out** via CT head.
- Administering aspirin in the context of an intracerebral hemorrhage could worsen bleeding.
*CTA head*
- A **CT angiography (CTA) head** is used to visualize the cerebral vasculature and identify large vessel occlusions, which can guide thrombectomy decisions in ischemic stroke.
- However, performing a **non-contrast CT head is a prerequisite** to rule out hemorrhage before proceeding with CTA or any other advanced imaging or therapeutic interventions.
Craniotomy indications and techniques US Medical PG Question 6: Which change in CSF production most directly affects intracranial pressure?
- A. Decreased arachnoid granulation function
- B. Increased choroid plexus blood flow
- C. Decreased carbonic anhydrase activity (Correct Answer)
- D. Increased osmotic gradient
Craniotomy indications and techniques Explanation: ***Decreased carbonic anhydrase activity***
- The **choroid plexus** produces CSF primarily through an active secretion process involving carbonic anhydrase.
- Decreased activity of this enzyme directly reduces the formation of **bicarbonate ions** and **protons (H+)**, which are crucial for the active transport of Na+ and Cl- into the CSF, thereby lowering CSF production and subsequently **intracranial pressure**.
*Decreased arachnoid granulation function*
- This change would lead to a **decreased reabsorption** of CSF, which would *increase* intracranial pressure, not directly affect production to lower it.
- Arachnoid granulations are responsible for the **resorption of CSF** into the venous system.
*Increased choroid plexus blood flow*
- While increased blood flow could potentially increase the delivery of substrates for CSF production, it is **not the most direct or primary determinant** of CSF production rate.
- CSF production is predominantly an **active secretory process**, not a passive filtration process dependent solely on blood flow.
*Increased osmotic gradient*
- An increased osmotic gradient, if referring to a higher osmolality in the CSF compared to plasma, would tend to **draw water into the CSF**, potentially *increasing* CSF volume and intracranial pressure.
- If referring to a gradient drawing water *out* of the CSF, it would *decrease* intracranial pressure but is not a primary mechanism of CSF production regulation.
Craniotomy indications and techniques US Medical PG Question 7: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Craniotomy indications and techniques Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
Craniotomy indications and techniques US Medical PG Question 8: A 48-year-old woman is brought to the emergency department because of a 1-hour history of sudden-onset headache associated with nausea and vomiting. The patient reports she was sitting at her desk when the headache began. The headache is global and radiates to her neck. She has hypertension. She has smoked one pack of cigarettes daily for the last 10 years. She drinks alcohol occasionally. Her father had a stroke at the age 58 years. Current medications include hydrochlorothiazide. She is in severe distress. She is alert and oriented to person, place, and time. Her temperature is 38.2°C (100.8°F), pulse is 89/min, respirations are 19/min, and blood pressure is 150/90 mm Hg. Cardiopulmonary examination shows no abnormalities. Cranial nerves II–XII are intact. She has no focal motor or sensory deficits. She flexes her hips and knees when her neck is flexed while lying in a supine position. A CT scan of the head is shown. Which of the following is the most appropriate intervention?
- A. Perform burr hole surgery
- B. Administer intravenous alteplase
- C. Administer intravenous vancomycin and ceftriaxone
- D. Perform surgical clipping (Correct Answer)
- E. Perform decompressive craniectomy
Craniotomy indications and techniques Explanation: ***Perform surgical clipping***
- The clinical presentation of **sudden-onset severe headache** ("thunderclap headache"), **nausea, vomiting, neck stiffness (positive Brudzinski's sign)**, and the CT scan showing **blood in the subarachnoid space** strongly indicate a **subarachnoid hemorrhage (SAH)** from a ruptured cerebral aneurysm.
- Definitive treatment requires **securing the aneurysm** to prevent **rebleeding**, which carries 40-50% mortality. Modern management includes **endovascular coiling** (first-line for most cases) or **surgical clipping**.
- **Surgical clipping** involves placing a metal clip across the aneurysm neck to exclude it from circulation. It remains the preferred approach for certain aneurysm locations (MCA), wide-necked aneurysms, or when accompanied by hematoma requiring evacuation.
- Among the options provided, surgical clipping is the only definitive intervention that secures the ruptured aneurysm.
*Perform burr hole surgery*
- **Burr hole surgery** is used for draining **subdural hematomas** or accessing the brain for procedures like biopsy or external ventricular drain placement.
- While burr holes may be needed for complications of SAH (e.g., hydrocephalus requiring EVD), this is not the primary intervention for securing the ruptured aneurysm itself.
*Administer intravenous alteplase*
- **Alteplase** (tPA) is a **thrombolytic agent** used for **acute ischemic stroke** within 4.5 hours of symptom onset.
- Administering thrombolytics in **hemorrhagic stroke** (like SAH) is **absolutely contraindicated** as it would worsen bleeding and cause catastrophic neurological deterioration or death.
*Administer intravenous vancomycin and ceftriaxone*
- **Vancomycin and ceftriaxone** treat **bacterial meningitis**, which can present with headache, fever, and meningeal signs.
- Although the patient has low-grade fever (likely from blood irritating meninges, not infection) and neck stiffness, the **sudden-onset thunderclap headache** and **CT findings of SAH** make ruptured aneurysm the diagnosis, not meningitis. The fever in SAH is typically from aseptic meningeal irritation.
*Perform decompressive craniectomy*
- **Decompressive craniectomy** removes skull bone to relieve **elevated intracranial pressure** from massive brain swelling (severe TBI, malignant MCA infarction).
- While SAH can cause elevated ICP, craniectomy does not secure the aneurysm. The immediate priority is preventing **rebleeding** by securing the aneurysm source, not managing secondary complications.
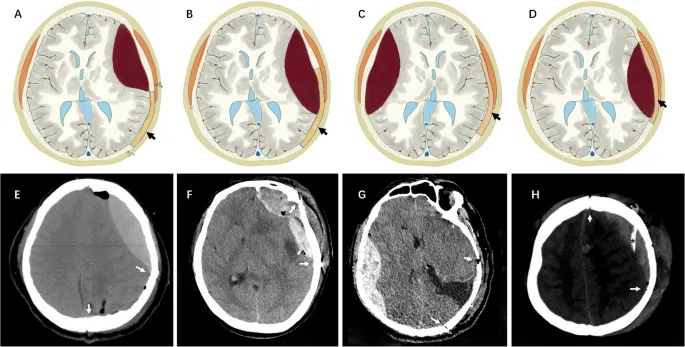
Craniotomy indications and techniques US Medical PG Question 9: A 47-year-old man is admitted to the emergency room after a fight in which he was hit in the head with a hammer. The witnesses say that the patient initially lost consciousness, but regained consciousness by the time emergency services arrived. On admission, the patient complained of a diffuse headache. He opened his eyes spontaneously, was verbally responsive, albeit confused, and was able to follow commands. He could not elevate his left hand and leg. He did not remember the events prior to the loss of consciousness and had difficulty remembering information, such as the names of nurses or doctors. His airway was not compromised. The vital signs are as follows: blood pressure, 180/100 mm Hg; heart rate, 59/min; respiratory rate, 12/min; temperature 37.0℃ (98.6℉); and SaO2, 96% on room air. The examination revealed bruising in the right frontotemporal region. The pupils are round, equal, and show a poor response to light. The neurologic examination shows hyperreflexia and decreased power in the left upper and lower limbs. There is questionable nuchal rigidity, but no Kernig and Brudzinski signs. The CT scan is shown in the image. Which of the following options is recommended for this patient?
- A. Lumbar puncture
- B. Decompressive craniectomy
- C. Administration of levetiracetam
- D. Administration of methylprednisolone
- E. Surgical evacuation of the clots (Correct Answer)
Craniotomy indications and techniques Explanation: ***Surgical evacuation of the clots***
- The CT scan image shows a **biconvex (lenticular) hyperdensity** consistent with an **epidural hematoma (EDH)**, which typically results from arterial bleeding (often from the **middle meningeal artery**). This patient's **"lucid interval"** (initial loss of consciousness, regain consciousness, then deterioration) is classic for EDH.
- Given the patient's neurological deterioration (left-sided weakness, pupillary changes, confusion, memory issues) and signs of increased intracranial pressure (hypertension, bradycardia - part of Cushing's triad), urgent surgical evacuation of the hematoma is indicated to relieve pressure and prevent herniation.
*Lumbar puncture*
- A lumbar puncture is **contraindicated** in the setting of suspected or confirmed **increased intracranial pressure (ICP)**, as it can precipitate **cerebral herniation**.
- The CT scan clearly demonstrates a space-occupying lesion, making a lumbar puncture unnecessary and potentially dangerous.
*Decompressive craniectomy*
- While decompressive craniectomy is a neurosurgical procedure used to reduce ICP, it is generally considered when other measures have failed or in cases of **diffuse brain swelling** or large **intracerebral hematomas** not amenable to simple evacuation.
- In this case of a localized epidural hematoma with a clear surgical target, direct evacuation is the primary and most effective intervention.
*Administration of levetiracetam*
- Levetiracetam is an **anticonvulsant** used to prevent seizures. While seizures can occur after traumatic brain injury, there is no indication that the patient is currently seizing.
- Prophylactic anticonvulsants are sometimes used in severe TBI, but addressing the life-threatening hematoma takes **precedence** over seizure prophylaxis.
*Administration of methylprednisolone*
- **Corticosteroids** like methylprednisolone are generally **contraindicated** in traumatic brain injury (TBI) as studies have shown **worse outcomes** and increased mortality.
- They are primarily used for their **anti-inflammatory effects** in conditions like spinal cord injury or vasogenic edema from tumors, not for acute head trauma with hematoma.
Craniotomy indications and techniques US Medical PG Question 10: A 77-year-old man is brought to the emergency department by his wife because of headache, nausea, and vomiting for 24 hours. His wife says that over the past 2 weeks, he has been more irritable and has had trouble remembering to do routine errands. Two weeks ago, he fell during a skiing accident but did not lose consciousness. He has coronary artery disease and hypertension. He has smoked one pack of cigarettes daily for 50 years. He has had 2 glasses of wine daily since his retirement 10 years ago. Current medications include atenolol, enalapril, furosemide, atorvastatin, and aspirin. He appears acutely ill. He is oriented to person but not to place or time. His temperature is 37°C (98.6°F), pulse is 99/min, respirations are 16/min, and blood pressure is 160/90 mm Hg. During the examination, he is uncooperative and unable to answer questions. Deep tendon reflexes are 4+ on the left and 2+ on the right. Babinski's sign is present on the left. There is mild weakness of the left iliopsoas and hamstring muscles. A CT scan of the head without contrast shows a high-density, 15-mm crescentic collection across the right hemispheric convexity. Which of the following is the most appropriate next step in the management of this patient?
- A. Recombinant tissue plasminogen activator administration
- B. Obtain an Electroencephalography
- C. Obtain an MRI of the head
- D. Surgical evacuation (Correct Answer)
- E. Observation
Craniotomy indications and techniques Explanation: ***Surgical evacuation***
- The CT scan reveals a **high-density, crescentic collection**, strongly indicative of an **acute subdural hematoma**, which is causing significant neurological deficits and mass effect (e.g., increased intracranial pressure symptoms like headache, nausea, vomiting, and altered mental status, and focal neurological signs).
- Given the patient's **acute neurological decline**, significant mass effect from the 15-mm hematoma, and age, prompt **surgical evacuation** is the definitive treatment to relieve pressure and prevent further brain injury.
*Recombinant tissue plasminogen activator administration*
- **tPA** is indicated for **acute ischemic stroke**, not hemorrhagic stroke or subdural hematoma. Administering tPA in this context would be harmful, potentially worsening the hemorrhage.
- The patient's CT scan clearly shows a **hemorrhagic lesion**, not an ischemic event.
*Obtain an Electroencephalography*
- **EEG** is primarily used to evaluate **seizure disorders** or certain types of encephalopathy. While the patient has altered mental status, the primary issue identified on CT is a subdural hematoma requiring immediate intervention.
- EEG would not provide information relevant to the immediate management of an **acute subdural hematoma**.
*Obtain an MRI of the head*
- An **MRI** can provide more detailed imaging, but in the context of an **acute subdural hematoma** with significant neurological compromise, it would delay crucial and time-sensitive surgical intervention.
- The **CT scan** has already provided sufficient diagnostic information to warrant immediate surgical planning.
*Observation*
- **Observation** is not appropriate for a patient with a rapidly expanding **acute subdural hematoma** causing significant neurological deficits and a 15-mm collection, especially given the patient's age and clinical presentation.
- Delaying treatment would likely lead to further neurological deterioration, **herniation**, and potentially death.
More Craniotomy indications and techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.