Cerebral aneurysm management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cerebral aneurysm management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cerebral aneurysm management US Medical PG Question 1: A 21-year-old man presents to the emergency department after sustaining a stab wound to the neck at a local farmer's market. The patient is otherwise healthy and is complaining of pain. The patient is able to offer the history himself. His temperature is 97.6°F (36.4°C), blood pressure is 120/84 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam demonstrates a 3 cm laceration 1 cm inferior to the mastoid process on the right side. The patient's breath sounds are clear and he is protecting his airway. No stridor or difficulty breathing is noted. Which of the following is the most appropriate next step in the management of this patient?
- A. Observation and blood pressure monitoring
- B. Intubation
- C. CT angiogram (Correct Answer)
- D. Surgical exploration
Cerebral aneurysm management Explanation: ***CT angiogram***
- A **CT angiogram (CTA)** is the most appropriate next step given the location of the stab wound, which is close to vital neurovascular structures, particularly the **carotid and vertebral arteries**.
- CTA is a **non-invasive** and rapid imaging modality that can effectively rule out or confirm vascular injuries, guide further management, and avoid unnecessary surgical exploration.
*Observation and blood pressure monitoring*
- While initial observation is important, relying solely on it for a penetration injury near major vessels is **insufficient** and could lead to delayed diagnosis of potentially life-threatening vascular damage.
- Although the patient is currently **hemodynamically stable**, vascular injuries can present with delayed symptoms and require more definitive diagnostic evaluation.
*Intubation*
- The patient has no signs of airway compromise, such as **stridor, difficulty breathing, or impaired oxygenation**.
- **Prophylactic intubation** is not indicated as it carries risks and is only performed when there is an immediate or impending threat to the airway.
*Surgical exploration*
- **Surgical exploration** is an invasive procedure and should be reserved for cases where there is clear evidence of vascular injury or when less invasive diagnostics like CTA are unavailable or inconclusive.
- In a stable patient, **non-invasive imaging** should precede surgery unless there are hard signs of vascular compromise (e.g., pulsatile bleeding, expanding hematoma, thrill/bruit).
Cerebral aneurysm management US Medical PG Question 2: A 52-year-old woman is brought to the emergency department for a severe, sudden-onset headache, light-sensitivity, and neck stiffness that began 30 minutes ago. A CT scan of the head shows hyperdensity between the arachnoid mater and the pia mater. The patient undergoes an endovascular procedure. One week later, she falls as she is returning from the bathroom. Neurologic examination shows 3/5 strength in the right lower extremity and 5/5 in the left lower extremity. Treatment with which of the following drugs is most likely to have prevented the patient's current condition?
- A. Fosphenytoin
- B. Nitroglycerin
- C. Enalapril
- D. Fresh frozen plasma
- E. Nimodipine (Correct Answer)
Cerebral aneurysm management Explanation: ***Nimodipine***
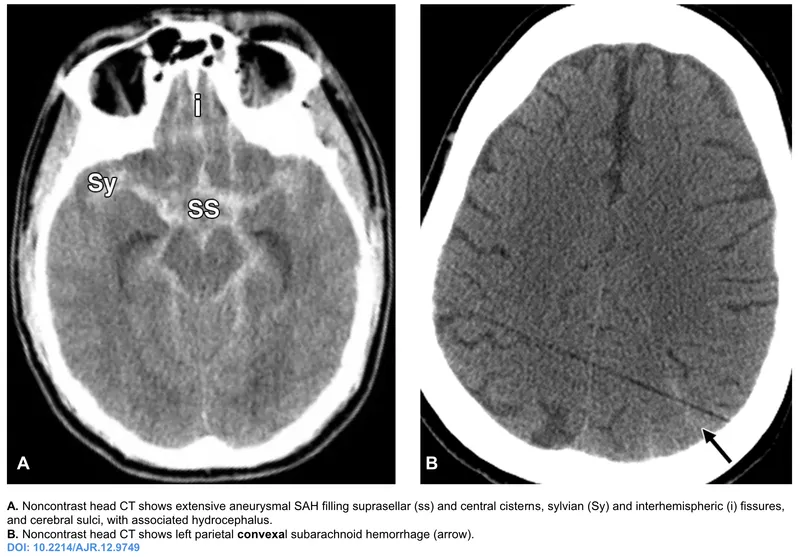
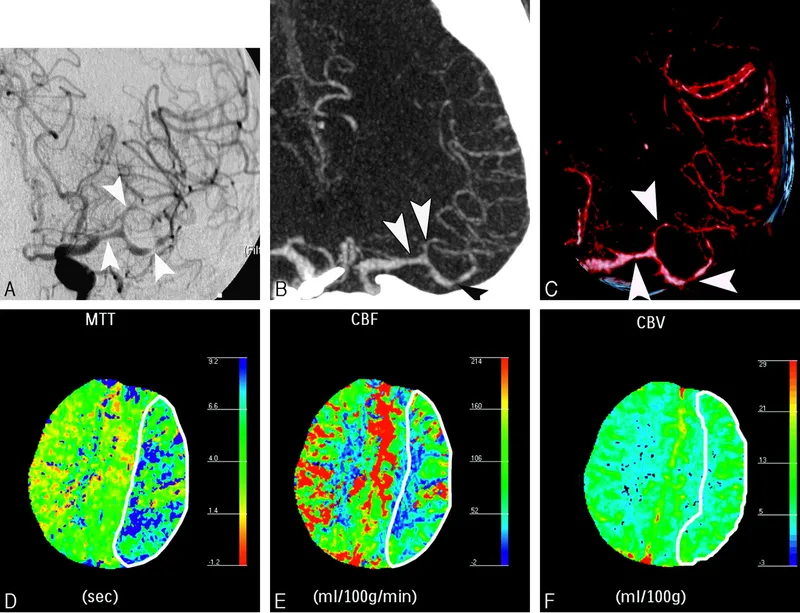
- The patient experienced a **subarachnoid hemorrhage (SAH)**, indicated by the sudden-onset severe headache, neck stiffness, light sensitivity, and hyperdensity between the arachnoid and pia mater on CT scan.
- **Nimodipine**, a calcium channel blocker, is used to prevent **cerebral vasospasm** following SAH, which can lead to delayed cerebral ischemia and focal neurological deficits like the patient's new right lower extremity weakness.
*Fosphenytoin*
- **Fosphenytoin** is an **anticonvulsant** used to treat or prevent seizures.
- While seizures can occur after SAH, there is no mention of seizure activity in this patient, and fosphenytoin would not prevent **vasospasm-induced ischemia**.
*Nitroglycerin*
- **Nitroglycerin** is a potent **vasodilator** primarily used to treat angina and heart failure.
- It rapidly lowers blood pressure and would not be used to prevent cerebral vasospasm after SAH, and could potentially worsen cerebral perfusion if blood pressure drops too low.
*Enalapril*
- **Enalapril** is an **ACE inhibitor** used to treat hypertension and heart failure.
- It is a long-acting antihypertensive and is not indicated for the prevention of **cerebral vasospasm** after SAH.
*Fresh frozen plasma*
- **Fresh frozen plasma (FFP)** is used to replace clotting factors in patients with coagulopathies or significant bleeding.
- While SAH involves bleeding, FFP would be used to reverse anticoagulant effects or treat a severe clotting factor deficiency, not to prevent **delayed ischemic deficits** from vasospasm.
Cerebral aneurysm management US Medical PG Question 3: A 60-year-old male is admitted to the ICU for severe hypertension complicated by a headache. The patient has a past medical history of insulin-controlled diabetes, hypertension, and hyperlipidemia. He smokes 2 packs of cigarettes per day. He states that he forgot to take his medications yesterday and started getting a headache about one hour ago. His vitals on admission are the following: blood pressure of 160/110 mmHg, pulse 95/min, temperature 98.6 deg F (37.2 deg C), and respirations 20/min. On exam, the patient has an audible abdominal bruit. After administration of antihypertensive medications, the patient has a blood pressure of 178/120 mmHg. The patient reports his headache has increased to a 10/10 pain level, that he has trouble seeing, and he can't move his extremities. After stabilizing the patient, what is the best next step to diagnose the patient's condition?
- A. Doppler ultrasound of the carotids
- B. CT head with intravenous contrast
- C. MRI head without intravenous contrast
- D. CT head without intravenous contrast (Correct Answer)
- E. MRI head with intravenous contrast
Cerebral aneurysm management Explanation: ***CT head without intravenous contrast***
- The sudden onset of severe headache, visual disturbances, and neurological deficits (inability to move extremities), coupled with uncontrolled severe hypertension despite initial treatment, is highly suggestive of an **intracranial pathology**, most likely a **hemorrhagic stroke**.
- A **non-contrast CT scan of the head** is the **gold standard** for rapidly identifying acute intracranial hemorrhage, as it can be performed quickly and is readily available in emergency settings.
*Doppler ultrasound of the carotids*
- This test is primarily used to evaluate **carotid artery stenosis** due to atherosclerosis, which can lead to ischemic stroke.
- While the patient has risk factors for atherosclerosis, his acute presentation with severe central neurological symptoms points more towards an acute intracranial event rather than carotid disease.
*CT head with intravenous contrast*
- While a contrast CT can be useful for identifying tumors, abscesses, or vascular malformations, it is **contraindicated in the initial assessment of acute stroke** if an intracranial hemorrhage is suspected.
- Contrast can sometimes obscure subtle bleeds or complicate the interpretation of acute hemorrhage, and it also carries a risk of **contrast-induced nephropathy**, especially in a patient with diabetes.
*MRI head without intravenous contrast*
- An MRI provides superior soft tissue resolution compared to CT and is excellent for detecting ischemic strokes in later stages, as well as subtle hemorrhages, tumors, and other conditions.
- However, it is **less available, takes longer to perform**, and is often not the first choice in an acute neurological emergency where time is critical, particularly when differentiating between ischemic and hemorrhagic stroke.
*MRI head with intravenous contrast*
- Similar to a contrast CT, an MRI with contrast is generally **not the initial imaging choice for acute stroke** due to time constraints and the need to quickly rule out hemorrhage before considering contrast administration.
- Contrast agents for MRI, such as gadolinium, have their own risks, including **nephrogenic systemic fibrosis** in patients with renal impairment, which is a concern in a diabetic patient.
Cerebral aneurysm management US Medical PG Question 4: A 69-year-old male presents to the emergency department for slurred speech and an inability to use his right arm which occurred while he was eating dinner. The patient arrived at the emergency department within one hour. A CT scan was performed of the head and did not reveal any signs of hemorrhage. The patient is given thrombolytics and is then managed on the neurology floor. Three days later, the patient is recovering and is stable. He seems depressed but is doing well with his symptoms gradually improving as compared to his initial presentation. The patient complains of neck pain that has worsened slowly over the past few days for which he is being given ibuprofen. Laboratory values are ordered and return as indicated below:
Serum:
Na+: 130 mEq/L
K+: 3.7 mEq/L
Cl-: 100 mEq/L
HCO3-: 24 mEq/L
Urea nitrogen: 7 mg/dL
Glucose: 70 mg/dL
Creatinine: 0.9 mg/dL
Ca2+: 9.7 mg/dL
Urine:
Appearance: dark
Glucose: negative
WBC: 0/hpf
Bacterial: none
Na+: 320 mEq/L/24 hours
His temperature is 99.5°F (37.5°C), pulse is 95/min, blood pressure is 129/70 mmHg, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Demeclocycline
- B. Fluid restriction (Correct Answer)
- C. Oral salt tablets
- D. Continue conservative management
- E. Conivaptan
Cerebral aneurysm management Explanation: ***Fluid restriction***
- The patient presents with **hyponatremia** (Na+ 130 mEq/L) and elevated urine sodium (320 mEq/L/24 hours) in the setting of recent stroke and possible SIADH (**Syndrome of Inappropriate Antidiuretic Hormone secretion**).
- **Fluid restriction** is the initial and most crucial step in managing euvolemic hyponatremia due to SIADH, reducing water intake to allow the kidney to excrete excess water and correct serum sodium.
*Demeclocycline*
- **Demeclocycline** is a tetracycline derivative that inhibits the action of ADH on renal tubules, used in chronic or refractory cases of SIADH.
- It is *not* the first-line treatment for acute, moderate hyponatremia, especially when fluid restriction has not yet been attempted.
*Oral salt tablets*
- **Oral salt tablets** would increase the solute load but would also draw water, potentially worsening hyponatremia if unrestricted fluid intake persists in SIADH.
- This intervention is generally not appropriate for **euvolemic hyponatremia** where the primary issue is excess free water.
*Continue conservative management*
- With a sodium level of 130 mEq/L, this is considered **mild to moderate hyponatremia** and requires active intervention to prevent potential neurological complications.
- Simply continuing conservative management without addressing the underlying **hyponatremia** or its cause would be inadequate and potentially harmful.
*Conivaptan*
- **Conivaptan** is an ADH receptor antagonist that can be used for persistent or significant hyponatremia in SIADH.
- It is typically reserved for more severe or refractory cases of hyponatremia and is usually administered intravenously, making it less suitable as a first-line outpatient management strategy.
Cerebral aneurysm management US Medical PG Question 5: A 52-year-old man is brought to the emergency department with a 2-hour history of severe, sudden-onset generalized headache. He has since developed nausea and has had one episode of vomiting. The symptoms began while he was at home watching television. Six days ago, he experienced a severe headache that resolved without treatment. He has hypertension and hyperlipidemia. The patient has smoked two packs of cigarettes daily for 30 years. His current medications include lisinopril-hydrochlorothiazide and simvastatin. His temperature is 38.1°C (100.6°F), pulse is 82/min, respirations are 16/min, and blood pressure is 162/98 mm Hg. The pupils are equal, round, and reactive to light. Fundoscopic examination shows no swelling of the optic discs. Cranial nerves II–XII are intact. He has no focal motor or sensory deficits. Finger-to-nose and heel-to-shin testing are normal. A CT scan of the head shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Obtain an MRI scan of the head
- B. Repeat CT scan in 24 hours
- C. Administer 100% oxygen and intranasal sumatriptan
- D. Place ventriculoperitoneal shunt
- E. Obtain a lumbar puncture (Correct Answer)
Cerebral aneurysm management Explanation: ***Obtain a lumbar puncture***
- The sudden onset of a "thunderclap" headache, especially if severe and generalized, is highly suspicious for **subarachnoid hemorrhage (SAH)**, even with a normal CT scan. An earlier, resolving headache ( sentinel headache) further supports this.
- A **lumbar puncture (LP)** is the gold standard for diagnosing SAH when a CT scan is negative, as it can detect **xanthochromia** (yellowish discoloration of CSF due to bilirubin degradation of red blood cells), indicating prior bleeding.
*Obtain an MRI scan of the head*
- While an MRI can detect SAH, especially in later stages, it is **less sensitive than LP** for acute SAH, particularly within the first few hours or if the bleed is small.
- MRI is generally reserved for situations where a CT scan is normal and LP is equivocal or contraindicated, or to investigate other potential causes of headache like lesions or thrombosis.
*Repeat CT scan in 24 hours*
- Repeating the CT scan in 24 hours is **not the most appropriate immediate action** as it will delay definitive diagnosis of SAH, which is a medical emergency requiring prompt management.
- While a repeat CT might show subtle changes, an LP is a more sensitive and direct method to confirm or rule out SAH in this clinical scenario.
*Administer 100% oxygen and intranasal sumatriptan*
- This treatment is appropriate for **cluster headaches** or **migraine**, which typically have a different presentation (e.g., specific aura, unilateral pain, autonomic symptoms for cluster headache).
- Given the high suspicion for SAH, administering these medications would delay proper diagnosis and management, which could be life-threatening.
*Place ventriculoperitoneal shunt*
- A ventriculoperitoneal shunt is used to treat **hydrocephalus**, a condition characterized by excessive CSF accumulation in the brain.
- There are no clinical signs or symptoms (e.g., papilledema, altered mental status with focal neurological deficits) in this patient to suggest hydrocephalus requiring immediate shunting.
Cerebral aneurysm management US Medical PG Question 6: A 56-year-old woman presents with sudden-onset severe headache, nausea, vomiting, and neck pain for the past 90 minutes. She describes her headache as a ‘thunderclap’, followed quickly by severe neck pain and stiffness, nausea and vomiting. She denies any loss of consciousness, seizure, or similar symptoms in the past. Her past medical history is significant for an episode 6 months ago where she suddenly had trouble putting weight on her right leg, which resolved within hours. The patient denies any history of smoking, alcohol or recreational drug use. On physical examination, the patient has significant nuchal rigidity. Her muscle strength in the lower extremities is 4/5 on the right and 5/5 on the left. The remainder of the physical examination is unremarkable. A noncontrast CT scan of the head is normal. Which of the following is the next best step in the management of this patient?
- A. Diffusion-weighted magnetic resonance imaging of the brain
- B. IV tPA
- C. Placement of a ventriculoperitoneal (VP) shunt
- D. T1/T2 MRI of the head
- E. Lumbar puncture (Correct Answer)
Cerebral aneurysm management Explanation: ***Lumbar puncture***
- A **thunderclap headache**, nuchal rigidity, nausea, and vomiting despite a normal noncontrast CT scan, is highly suspicious for **subarachnoid hemorrhage (SAH)**. A lumbar puncture is the next diagnostic step to look for **xanthochromia** or **red blood cells** in the cerebrospinal fluid.
- The previous episode of transient leg weakness could indicate a prior **warning leak** from an **aneurysm**, increasing the suspicion for SAH.
*Diffusion-weighted magnetic resonance imaging of the brain*
- This imaging is primarily used to detect **acute ischemic stroke**, which presents differently.
- While helpful for ischemic events, it is **not the primary diagnostic test** for suspected SAH after a normal CT.
*IV tPA*
- **Intravenous tissue plasminogen activator (IV tPA)** is a thrombolytic used in acute ischemic stroke, characterized by focal neurological deficits.
- It is **contraindicated** in SAH due to the significant risk of exacerbating intracranial bleeding.
*Placement of a ventriculoperitoneal (VP) shunt*
- A **VP shunt** is a surgical procedure to drain excess cerebrospinal fluid, typically used to treat **hydrocephalus**.
- This is a treatment for a complication (hydrocephalus) that may arise from SAH, but it is **not the initial diagnostic or management step** for an acute SAH.
*T1/T2 MRI of the head*
- While MRI can detect SAH, especially if performed with specific sequences (FLAIR), a **lumbar puncture is more sensitive for detecting SAH** when a CT scan is negative and clinical suspicion remains high.
- MRI is generally less accessible and more time-consuming than lumbar puncture in an emergency setting for suspected SAH.
Cerebral aneurysm management US Medical PG Question 7: A 48-year-old woman is brought to the emergency department because of a 1-hour history of sudden-onset headache associated with nausea and vomiting. The patient reports she was sitting at her desk when the headache began. The headache is global and radiates to her neck. She has hypertension. She has smoked one pack of cigarettes daily for the last 10 years. She drinks alcohol occasionally. Her father had a stroke at the age 58 years. Current medications include hydrochlorothiazide. She is in severe distress. She is alert and oriented to person, place, and time. Her temperature is 38.2°C (100.8°F), pulse is 89/min, respirations are 19/min, and blood pressure is 150/90 mm Hg. Cardiopulmonary examination shows no abnormalities. Cranial nerves II–XII are intact. She has no focal motor or sensory deficits. She flexes her hips and knees when her neck is flexed while lying in a supine position. A CT scan of the head is shown. Which of the following is the most appropriate intervention?
- A. Perform burr hole surgery
- B. Administer intravenous alteplase
- C. Administer intravenous vancomycin and ceftriaxone
- D. Perform surgical clipping (Correct Answer)
- E. Perform decompressive craniectomy
Cerebral aneurysm management Explanation: ***Perform surgical clipping***
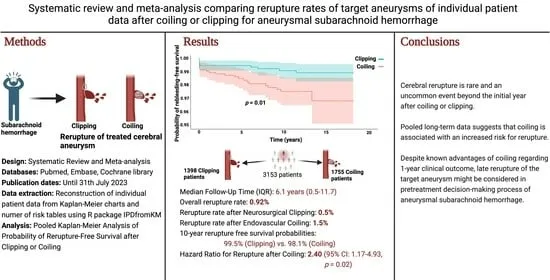
- The clinical presentation of **sudden-onset severe headache** ("thunderclap headache"), **nausea, vomiting, neck stiffness (positive Brudzinski's sign)**, and the CT scan showing **blood in the subarachnoid space** strongly indicate a **subarachnoid hemorrhage (SAH)** from a ruptured cerebral aneurysm.
- Definitive treatment requires **securing the aneurysm** to prevent **rebleeding**, which carries 40-50% mortality. Modern management includes **endovascular coiling** (first-line for most cases) or **surgical clipping**.
- **Surgical clipping** involves placing a metal clip across the aneurysm neck to exclude it from circulation. It remains the preferred approach for certain aneurysm locations (MCA), wide-necked aneurysms, or when accompanied by hematoma requiring evacuation.
- Among the options provided, surgical clipping is the only definitive intervention that secures the ruptured aneurysm.
*Perform burr hole surgery*
- **Burr hole surgery** is used for draining **subdural hematomas** or accessing the brain for procedures like biopsy or external ventricular drain placement.
- While burr holes may be needed for complications of SAH (e.g., hydrocephalus requiring EVD), this is not the primary intervention for securing the ruptured aneurysm itself.
*Administer intravenous alteplase*
- **Alteplase** (tPA) is a **thrombolytic agent** used for **acute ischemic stroke** within 4.5 hours of symptom onset.
- Administering thrombolytics in **hemorrhagic stroke** (like SAH) is **absolutely contraindicated** as it would worsen bleeding and cause catastrophic neurological deterioration or death.
*Administer intravenous vancomycin and ceftriaxone*
- **Vancomycin and ceftriaxone** treat **bacterial meningitis**, which can present with headache, fever, and meningeal signs.
- Although the patient has low-grade fever (likely from blood irritating meninges, not infection) and neck stiffness, the **sudden-onset thunderclap headache** and **CT findings of SAH** make ruptured aneurysm the diagnosis, not meningitis. The fever in SAH is typically from aseptic meningeal irritation.
*Perform decompressive craniectomy*
- **Decompressive craniectomy** removes skull bone to relieve **elevated intracranial pressure** from massive brain swelling (severe TBI, malignant MCA infarction).
- While SAH can cause elevated ICP, craniectomy does not secure the aneurysm. The immediate priority is preventing **rebleeding** by securing the aneurysm source, not managing secondary complications.
Cerebral aneurysm management US Medical PG Question 8: A 17-year-old boy is brought to the emergency department by his brother after losing consciousness 1 hour ago. The brother reports that the patient was skateboarding outside when he fell on the ground and started to have generalized contractions. There was also some blood coming from his mouth. The contractions stopped after about 1 minute, but he remained unconscious for a few minutes afterward. He has never had a similar episode before. There is no personal or family history of serious illness. He does not smoke or drink alcohol. He does not use illicit drugs. He takes no medications. On arrival, he is confused and oriented only to person and place. He cannot recall what happened and reports diffuse muscle ache, headache, and fatigue. He appears pale. His temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 130/80 mm Hg. There is a small wound on the left side of the tongue. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference ranges. Toxicology screening is negative. An ECG shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Electroencephalography
- B. Lumbar puncture
- C. Lorazepam therapy
- D. Reassurance and follow-up
- E. CT scan of the head (Correct Answer)
Cerebral aneurysm management Explanation: ***CT scan of the head***
- Given the **first-time seizure** in an adolescent, especially with a history of head trauma (falling while skateboarding) and subsequent confusion, a **CT scan of the head** is crucial to rule out acute structural lesions like hemorrhage, mass, or edema.
- It is vital for identifying **life-threatening causes** of seizure that require immediate intervention, such as an **intracranial hematoma** or **mass lesion**, which could have been precipitated or exacerbated by the fall.
*Electroencephalography*
- **EEG** is appropriate for later evaluation to diagnose and classify seizure disorders, but it is not the *most appropriate initial step* in the emergency setting for a first-time seizure with a possible traumatic etiology.
- An EEG might be normal shortly after a seizure, and it does not rule out acute structural brain pathology that requires urgent management.
*Lumbar puncture*
- A **lumbar puncture** is indicated if there's suspicion of meningoencephalitis (e.g., fever, nuchal rigidity, immunocompromised status), which are not prominent features in this patient.
- The patient's vital signs are stable, and there are no signs of infection, making this a less urgent initial diagnostic step compared to imaging.
*Lorazepam therapy*
- **Lorazepam** is a benzodiazepine used to terminate ongoing seizures (**status epilepticus**), but this patient's generalized contractions have already stopped.
- Administering lorazepam when the seizure has resolved is unnecessary and would only cause further sedation.
*Reassurance and follow-up*
- While reassurance is part of patient care, it is *insufficient* as the sole next step for a **first-time seizure** episode in an adolescent, especially with features suggesting a possible underlying acute cause.
- A thorough diagnostic workup, beginning with neuroimaging, is necessary to ensure there is no serious underlying pathology before considering discharge and follow-up.
Cerebral aneurysm management US Medical PG Question 9: A 48-year-old woman undergoes awake craniotomy for resection of a left frontal glioma near Broca's area. Intraoperatively, cortical mapping identifies eloquent tissue, but the tumor extends into functionally critical regions. The surgeon achieves 70% resection when the patient develops expressive aphasia during mapping. Frozen section shows low-grade astrocytoma. The family previously expressed desire for maximal resection. Evaluate the intraoperative decision-making.
- A. Use awake testing to define exact limits of safe resection
- B. Obtain family consultation intraoperatively about acceptable deficits
- C. Convert to asleep anesthesia and use anatomic landmarks for resection
- D. Continue resection since low-grade tumors justify aggressive surgery
- E. Stop resection to preserve language function (Correct Answer)
Cerebral aneurysm management Explanation: ***Stop resection to preserve language function***
- Development of **expressive aphasia** during mapping indicates the surgical margin has reached **eloquent cortex** (Broca's area), and proceeding further risks permanent neurological deficit.
- The principle of **"maximal safe resection"** prioritizes the preservation of **quality of life** and functional status over the total removal of a low-grade tumor.
*Use awake testing to define exact limits of safe resection*
- Awake testing and **cortical mapping** have already identified the limit by triggering aphasia; additional testing at that specific site is redundant and risks seizure or further injury.
- Once a **functional boundary** is identified via intraoperative monitoring, it serves as the definitive anatomical endpoint for the resection.
*Obtain family consultation intraoperatively about acceptable deficits*
- Surrogate decision-makers cannot provide **informed consent** for new, immediate neurological deficits in the middle of a procedure when the surgeon has reached a safety limit.
- The surgeon’s primary obligation is to maintain **patient safety** and adhere to the established surgical plan of functional preservation.
*Convert to asleep anesthesia and use anatomic landmarks for resection*
- Converting to **general anesthesia** would lose the benefit of **functional monitoring**, making any further resection near Broca's area extremely dangerous and blind to functional limits.
- **Anatomic landmarks** are often unreliable for predicting function due to **neuroplasticity** or tumor displacement, making mapping essential in this region.
*Continue resection since low-grade tumors justify aggressive surgery*
- While aggressive resection improves **progression-free survival**, the prognosis for **low-grade astrocytomas** is relatively long, making a permanent, devastating deficit like **aphasia** unacceptable.
- Aggressive surgery is only justified up to the **functional boundary**; crossing it violates the core surgical principle of avoiding non-recoverable morbidity.
Cerebral aneurysm management US Medical PG Question 10: A 25-year-old man with newly diagnosed glioblastoma multiforme undergoes gross total resection. Pathology confirms IDH-wild type, MGMT promoter unmethylated tumor. His parents want aggressive treatment, but oncology notes poor prognosis (median survival 12-15 months). The patient is engaged to be married and wants to prioritize quality of life. Radiation oncology recommends standard chemoradiation. Evaluate the most appropriate management approach considering prognostic factors and patient values.
- A. Clinical trial enrollment with experimental immunotherapy
- B. Palliative care referral with symptom management only
- C. Multidisciplinary meeting to align treatment with patient goals of care (Correct Answer)
- D. Standard Stupp protocol (radiation with concurrent and adjuvant temozolomide)
- E. Hypofractionated radiation alone to preserve quality of life
Cerebral aneurysm management Explanation: ***Multidisciplinary meeting to align treatment with patient goals of care***
- There is a significant conflict between the family's desire for **aggressive treatment** and the patient's focus on **quality of life**, necessitating a structured **shared decision-making** process.
- Given the poor prognosis of **IDH-wild type** and **MGMT-unmethylated** glioblastoma, a multidisciplinary approach ensures all specialists and the patient can reconcile medical options with personal life goals.
*Clinical trial enrollment with experimental immunotherapy*
- While a valid consideration for high-grade gliomas, it is not the immediate first step before establishing the overall **goals of care** with the patient.
- **Experimental therapies** often involve significant logistical burdens and side effects that may conflict with the patient's wish to prioritize his wedding and quality of life.
*Palliative care referral with symptom management only*
- Transitioning to **exclusive palliative care** may be premature as the patient is young, has had a gross total resection, and has not yet discussed potential lifespan-extending benefits of treatment.
- This approach ignores the possibility of combining radiation with supportive care to maintain **neurological function** and independence.
*Standard Stupp protocol (radiation with concurrent and adjuvant temozolomide)*
- The **Stupp protocol** is the standard of care, but its efficacy is significantly reduced in **MGMT-unmethylated** tumors because the tumor lacks the epigenetic silencing of the DNA repair enzyme.
- Proceeding with standard chemoradiation without highlighting the limited benefit and potential **toxicity** (fatigue, cytopenias) violates the patient's preference for quality-of-life-centered care.
*Hypofractionated radiation alone to preserve quality of life*
- **Hypofractionated radiation** is typically reserved for elderly patients or those with a poor **performance status**, rather than a fit 25-year-old.
- Selecting a treatment plan based solely on one factor before a comprehensive **multidisciplinary discussion** risks under-treating the patient or misaligning expectations.
More Cerebral aneurysm management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.