Neurosurgery Basics

On this page
🧠 The Neurosurgeon's Foundation: Mastering the Cranial Command Center
Neurosurgery demands more than steady hands-it requires three-dimensional anatomical mastery, strategic corridor selection through unforgiving tissue, and split-second judgment where millimeters separate cure from catastrophe. You'll build from foundational neuroanatomy through surgical approaches, decision frameworks, microsurgical techniques, complication recognition, and integrated practice patterns that transform theoretical knowledge into operative confidence. This lesson equips you to think like a neurosurgeon: anticipating risks, choosing optimal paths, and understanding why each maneuver matters when operating on humanity's most complex organ.

📌 Remember: SCALP layers from superficial to deep - Skin, Connective tissue, Aponeurosis, Loose areolar tissue, Pericranium. The loose areolar layer contains the dangerous scalp vessels that can cause 500-1000mL blood loss if not controlled.
The cranial vault operates as a rigid container following the Monro-Kellie doctrine - total intracranial volume remains constant at approximately 1400-1500mL. This includes brain tissue (80%), cerebrospinal fluid (10%), and blood (10%). Any increase in one component must be compensated by decrease in others, or intracranial pressure rises exponentially.
- Cranial Anatomy Mastery
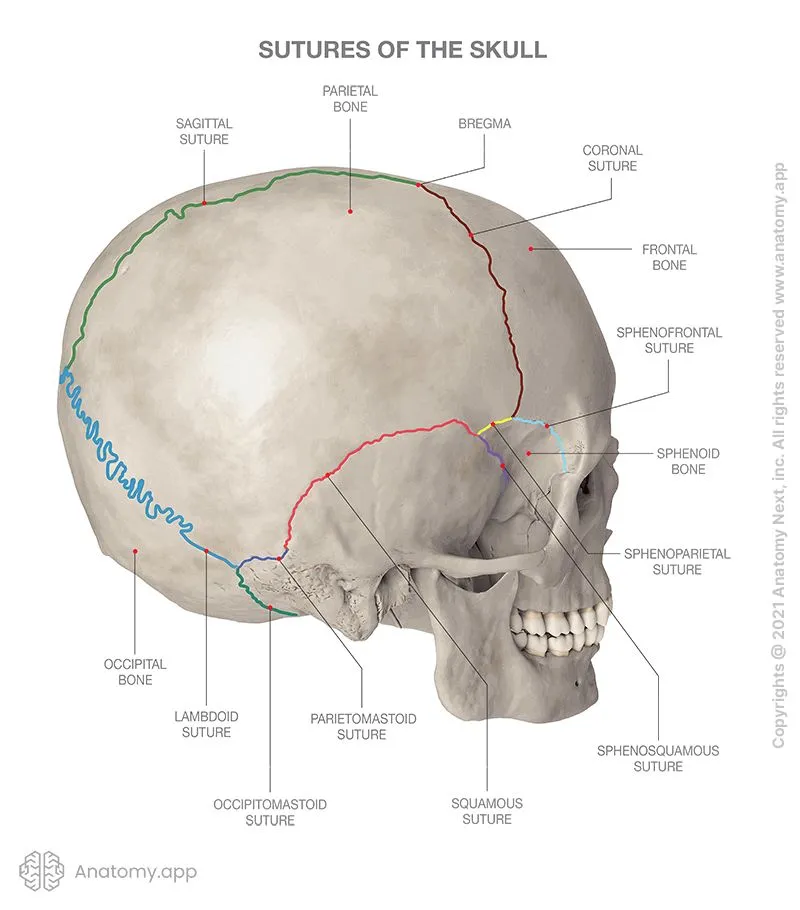
- Frontal bone: Houses frontal sinuses, 15-20mm thick at glabella
- Parietal bones: Thinnest at 3-4mm near temporal lines
- Temporal bone: Pterion - weakest skull point, 2-3mm thick
- Middle meningeal artery groove lies 2cm superior to zygomatic arch
- Temporal muscle attachment spans 8-10cm vertically
- Occipital bone: Inion landmark for posterior fossa approaches
⭐ Clinical Pearl: The pterion lies 4cm superior and 3cm posterior to the lateral orbital rim. This H-shaped suture junction overlies the middle meningeal artery in 85% of patients, making it the classic epidural hematoma location.
| Surgical Approach | Bone Thickness | Key Vessels | Complication Rate | Recovery Time | Functional Risk |
|---|---|---|---|---|---|
| Pterional | 2-3mm | MMA, superficial temporal | 8-12% | 4-6 weeks | <5% motor |
| Frontal | 15-20mm | Anterior cerebral | 5-8% | 3-4 weeks | <2% cognitive |
| Parietal | 6-8mm | Posterior cerebral | 10-15% | 5-7 weeks | 8-12% sensory |
| Occipital | 12-15mm | Posterior inferior cerebellar | 15-20% | 6-8 weeks | 20-25% visual |
| Temporal | 3-4mm | Middle cerebral | 12-18% | 4-6 weeks | 15-20% speech |
💡 Master This: The middle meningeal artery runs in a groove on the inner temporal bone, branching into anterior and posterior divisions at the pterion. Anterior division supplies 60% of temporal-parietal dura, explaining why 85% of epidural hematomas occur in this region.
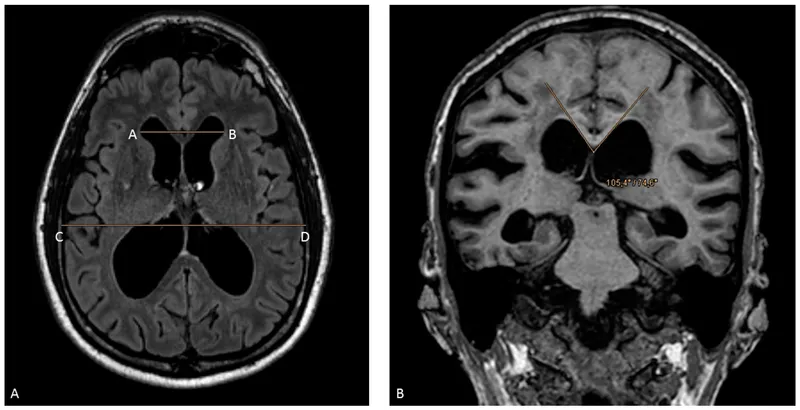
Understanding the ventricular system provides the foundation for hydrocephalus management and CSF diversion procedures. Total CSF volume measures 120-150mL in adults, with production rate of 20-25mL/hour (480-600mL/day). The choroid plexus produces 70% of CSF, while ependymal surfaces contribute 30%.
📌 Remember: LAMP for ventricular anatomy - Lateral ventricles (largest), Aqueduct of Sylvius (narrowest at 1-2mm), Monro foramina (connect lateral to third), Posterior fossa (fourth ventricle). Obstruction at any point causes upstream dilation.
Connect these anatomical foundations through surgical approaches to understand how neurosurgeons access different brain regions safely.
🧠 The Neurosurgeon's Foundation: Mastering the Cranial Command Center
⚔️ Surgical Corridors: The Neurosurgeon's Roadmap to Brain Access
📌 Remember: SAFE principles for craniotomy - Scalp incision behind hairline, Avoid crossing major vessels, Flap base toward vascular supply, Expose 2cm beyond lesion margins. Scalp blood flow averages 200-300mL/min/100g, requiring meticulous hemostasis.
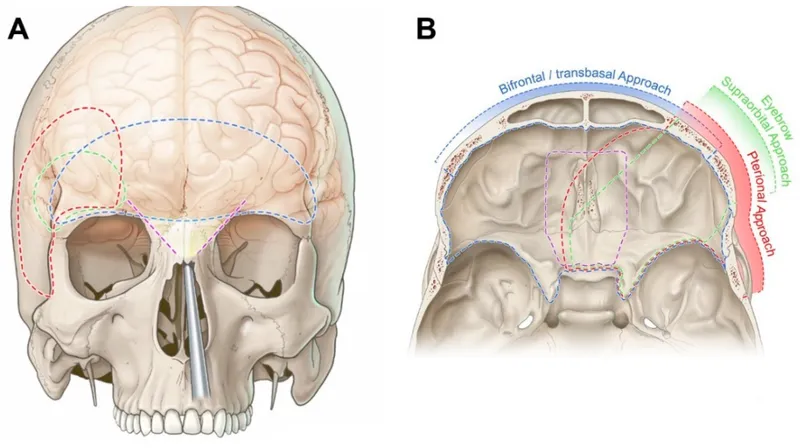
The pterional approach serves as the workhorse of neurosurgery, providing access to anterior circulation aneurysms, middle cerebral artery territory, and suprasellar region. This approach requires understanding the Sylvian fissure anatomy and sphenoid wing removal techniques.
- Pterional Approach Mastery
- Skin incision: Starts 1cm anterior to tragus, curves behind hairline
- Bone removal: 4x5cm craniotomy centered on pterion
- Sphenoid wing: Remove 15-20mm to expose middle cerebral artery
- Lesser wing removal exposes optic nerve and carotid artery
- Greater wing removal provides temporal lobe access
- Sylvian fissure: Split arachnoid to access M1-M2 junction
⭐ Clinical Pearl: The sphenoid ridge must be drilled flush with the anterior clinoid process to achieve adequate exposure. Inadequate bone removal accounts for 40-50% of approach-related complications, forcing excessive brain retraction.
| Approach Type | Exposure Area | Bone Removal | Surgery Time | Complication Rate | Functional Outcome |
|---|---|---|---|---|---|
| Pterional | 25-30cm² | 4x5cm | 3-4 hours | 8-12% | >90% good |
| Frontal | 20-25cm² | 5x6cm | 2-3 hours | 5-8% | >95% good |
| Parietal | 15-20cm² | 4x4cm | 2-3 hours | 10-15% | 85-90% good |
| Occipital | 12-15cm² | 3x4cm | 2-3 hours | 15-20% | 75-85% good |
| Temporal | 18-22cm² | 4x5cm | 3-4 hours | 12-18% | 80-85% good |
💡 Master This: The asterion (junction of parietal, temporal, and occipital bones) lies directly over the sigmoid sinus in 90% of patients. A 3x4cm craniotomy centered 1cm medial to asterion provides optimal cerebellopontine angle exposure while avoiding sinus injury.
Endoscopic approaches revolutionize neurosurgery by utilizing natural corridors and minimally invasive techniques. Endonasal endoscopy accesses pituitary, skull base, and ventricular pathology through nostril entry points, avoiding external incisions entirely.
- Endoscopic Technique Advantages
- Endonasal: Access sella, clivus, anterior skull base
- Intraventricular: Reach third ventricle, pineal region, posterior third ventricle
- Transcallosal: Approach interhemispheric lesions without cortical incision
- Visualization: HD cameras with ×10-20 magnification
- Instruments: 2-3mm diameter tools with articulating tips
- Recovery: 50-70% faster than open approaches
📌 Remember: NOSE for endonasal anatomy - Nasal septum (midline reference), Olfactory apparatus (preserve in upper 1/3), Sphenoid sinus (surgical corridor), Ethmoid air cells (remove for access). CSF leak risk increases to 15-20% with extended approaches.
Understanding surgical approaches enables recognition of approach-related complications and anatomical limitations that influence surgical decision-making.
⚔️ Surgical Corridors: The Neurosurgeon's Roadmap to Brain Access
🎯 Surgical Decision Matrix: When Steel Meets Brain
📌 Remember: HITS criteria for emergency craniotomy - Hematoma volume >30mL, Intracranial pressure >20mmHg, Temporal herniation signs, Severe midline shift >5mm. These findings mandate immediate surgical intervention within 60-90 minutes.
Traumatic brain injury represents the most common neurosurgical emergency, with clear surgical thresholds based on imaging findings and clinical presentation. The Brain Trauma Foundation guidelines provide evidence-based decision algorithms.
- TBI Surgical Indications
- Epidural hematoma: Volume >30mL regardless of GCS
- Subdural hematoma: Thickness >10mm or midline shift >5mm
- Intracerebral hemorrhage: Volume >50mL in non-eloquent areas
- GCS decline of ≥2 points from admission
- Pupillary changes indicating herniation
- ICP monitoring showing sustained >20mmHg
⭐ Clinical Pearl: The ABC/2 method rapidly estimates hematoma volume on CT: A (largest diameter) × B (perpendicular diameter) × C (slice thickness × number of slices) ÷ 2. Volumes >30mL predict poor outcome without surgery in 85% of cases.
| Pathology Type | Volume Threshold | Midline Shift | GCS Threshold | Surgery Urgency | Outcome Prediction |
|---|---|---|---|---|---|
| Epidural | >30mL | Any shift | Any GCS | <2 hours | 90% good if early |
| Subdural | >40mL | >5mm | <13 | <4 hours | 60% good if early |
| Intracerebral | >50mL | >10mm | <12 | <6 hours | 40% good if early |
| Cerebellar | >15mL | >3mm | Any decline | <1 hour | 70% good if early |
| Contusion | >25mL | >5mm | <10 | <8 hours | 50% good if early |
💡 Master This: Normal pressure hydrocephalus presents with the classic Hakim triad: gait disturbance (85% of patients), cognitive decline (60%), and urinary incontinence (40%). Lumbar puncture with 30-50mL CSF removal predicts shunt responsiveness in 70-80% of cases.
Brain tumor surgery depends on histological diagnosis, location, patient age, and functional status. Gross total resection improves survival in low-grade gliomas by 2-3 years compared to subtotal resection.
- Tumor Surgery Decision Factors
- Location: Eloquent areas limit resection extent
- Size: Tumors >6cm require staged procedures
- Histology: High-grade lesions need aggressive resection
- Intraoperative monitoring reduces permanent deficits to <5%
- Awake craniotomy enables language mapping in dominant hemisphere
- Fluorescence guidance increases gross total resection rates by 20-30%
📌 Remember: SMART tumor surgery principles - Safety first (preserve function), Maximal safe resection, Adjuvant therapy planning, Rapid pathological diagnosis, Team-based approach. Extent of resection correlates directly with survival in 85% of tumor types.
Understanding surgical indications enables rapid decision-making and appropriate patient counseling regarding risks, benefits, and expected outcomes.
🎯 Surgical Decision Matrix: When Steel Meets Brain
🔬 Precision Techniques: The Microsurgeon's Arsenal
📌 Remember: MICRO principles for microsurgery - Magnification ×6-40, Illumination coaxial LED, Coagulation bipolar only, Retraction minimal force, Orientation constant reference. Hand tremor amplifies ×10-20 under magnification, requiring arm rests and controlled movements.
Microsurgical technique forms the foundation of modern neurosurgery, enabling precise dissection of neurovascular structures while minimizing tissue trauma. Operating microscopes provide stereoscopic vision with variable magnification and coaxial illumination.
- Microsurgical Equipment Mastery
- Microscope: ×6-40 magnification with 400mm working distance
- Instruments: 0.5-2mm tips with micro-serrations
- Sutures: 8-0 to 11-0 nylon or polypropylene
- Needle diameter: 50-100 micrometers for vessel anastomosis
- Suture strength: 0.5-2 pounds tensile strength
- Knot security: 6-8 throws for permanent closure
⭐ Clinical Pearl: Bipolar coagulation at 15-25 watts provides precise hemostasis without thermal spread beyond 1-2mm. Monopolar cautery causes 5-10mm thermal damage and should never be used near neural tissue or major vessels.
| Technique Type | Magnification | Instrument Size | Precision Level | Complication Rate | Learning Curve |
|---|---|---|---|---|---|
| Microsurgery | ×10-25 | 0.5-1mm | ±0.1mm | <5% | 200+ cases |
| Endoscopy | ×5-15 | 2-3mm | ±0.5mm | 8-12% | 100+ cases |
| Stereotactic | ×1-5 | 1-2mm | ±1mm | 3-8% | 50+ cases |
| Open Surgery | ×2-6 | 3-5mm | ±2mm | 10-15% | 300+ cases |
| Robotic | ×10-20 | 1-2mm | ±0.2mm | 5-10% | 150+ cases |
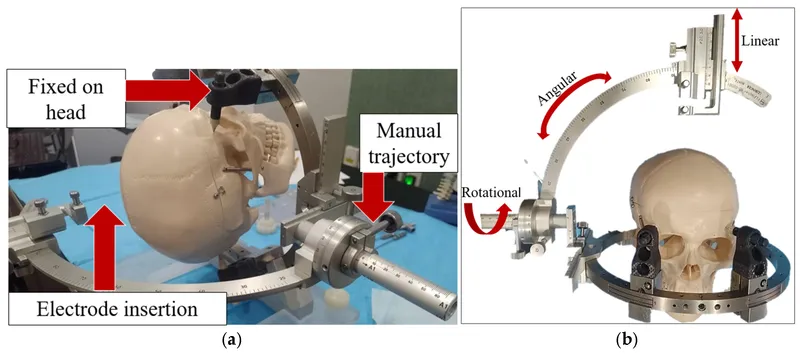
💡 Master This: Stereotactic coordinates use the anterior commissure-posterior commissure line as reference, with accuracy of ±1-2mm in 95% of cases. Frame-based systems achieve ±0.5mm accuracy, while frameless systems reach ±1-2mm precision.
Intraoperative monitoring preserves neurological function during high-risk procedures by providing real-time feedback about neural pathway integrity. Motor evoked potentials and somatosensory evoked potentials detect impending injury before permanent damage occurs.
- Neuromonitoring Applications
- Motor evoked potentials: Monitor corticospinal tract integrity
- Somatosensory evoked potentials: Assess dorsal column function
- Brainstem auditory evoked potentials: Protect hearing during CPA surgery
- Amplitude reduction >50% indicates neural compromise
- Latency increase >10% suggests ischemic changes
- Signal loss requires immediate intervention within 5-10 minutes
📌 Remember: ALARM criteria for neuromonitoring changes - Amplitude drop >50%, Latency increase >10%, Absent responses, Repetitive stimulation failure, Morphology changes. These findings mandate immediate surgical pause and intervention.
Awake craniotomy enables real-time functional testing during tumor resection in eloquent brain areas. Language mapping and motor testing guide resection boundaries to maximize tumor removal while preserving function.
Understanding precision techniques enables appropriate case selection and realistic outcome expectations for complex neurosurgical procedures.
🔬 Precision Techniques: The Microsurgeon's Arsenal
⚠️ Complication Mastery: Navigating Neurosurgical Hazards
Complication prevention begins with thorough preoperative planning, appropriate case selection, and meticulous surgical technique. Understanding complication patterns enables early recognition and prompt intervention to optimize outcomes.
📌 Remember: STOP protocol for intraoperative bleeding - Stop all activity, Tamponade with cottonoids, Obtain proximal control, Precise hemostasis with bipolar. Uncontrolled bleeding accounts for 40-50% of intraoperative deaths in neurosurgery.
Hemorrhagic complications represent the most immediate threat to patient safety, with mortality rates of 15-25% when major vessel injury occurs. Rapid recognition and systematic response determine patient survival.
- Hemorrhage Management Hierarchy
- Immediate: Direct pressure with cottonoids or patties
- Proximal control: Temporary clips on feeding vessels
- Definitive repair: Primary suture or patch grafts
- Blood loss >500mL requires immediate transfusion
- Systolic pressure maintain >90mmHg for cerebral perfusion
- Hematocrit keep >25% for adequate oxygen delivery
⭐ Clinical Pearl: Venous bleeding appears dark red and continuous, while arterial bleeding shows bright red and pulsatile flow. Venous injuries respond to gentle pressure and patient positioning, while arterial injuries require immediate surgical repair.
| Complication Type | Incidence Rate | Mortality Risk | Permanent Deficit | Prevention Strategy | Treatment Response |
|---|---|---|---|---|---|
| Major Hemorrhage | 3-8% | 15-25% | 30-40% | Gentle technique | Emergency repair |
| Infection | 5-12% | 2-5% | 10-20% | Sterile technique | Antibiotics |
| Seizures | 15-25% | <1% | 5-10% | Prophylactic AEDs | Medication |
| CSF Leak | 8-15% | <1% | <5% | Watertight closure | Surgical repair |
| Stroke | 2-5% | 10-20% | 60-80% | Gentle retraction | Medical management |
💡 Master This: Post-op neurological decline follows the HIPS pattern - Hematoma (40%), Infection (20%), Pneumocephalus (15%), Seizures (25%). Immediate CT scan identifies surgical emergencies requiring urgent intervention.
Infection prevention requires strict sterile technique, appropriate antibiotic prophylaxis, and meticulous wound care. Surgical site infections occur in 5-12% of craniotomies, with higher rates in contaminated cases.
- Infection Prevention Protocol
- Preoperative: Chlorhexidine skin prep, cefazolin 2g IV within 60 minutes
- Intraoperative: Sterile technique, irrigation with antibiotic solution
- Postoperative: Wound monitoring, early mobilization, glucose control
- Deep infections require surgical debridement within 24-48 hours
- Superficial infections respond to oral antibiotics in 80-90%
- Meningitis develops in 2-5% of craniotomies, requiring IV antibiotics
📌 Remember: WASH principles for infection prevention - Wound care protocols, Antibiotic prophylaxis, Sterile technique, Hand hygiene compliance. Infection rates correlate directly with operative time (+2% per hour) and blood loss (+1% per 100mL).
Seizure prophylaxis prevents early postoperative seizures in high-risk patients, particularly those with cortical incisions or tumor surgery. Phenytoin or levetiracetam reduce seizure incidence from 25-30% to 8-12%.
Understanding complication patterns enables proactive management and improved patient outcomes through early recognition and prompt intervention.
⚠️ Complication Mastery: Navigating Neurosurgical Hazards
🔗 Advanced Integration: The Neurosurgical Ecosystem
Modern neurosurgery operates within complex healthcare systems that demand seamless integration between surgical teams, intensive care units, rehabilitation services, and outpatient follow-up. Understanding these interconnections optimizes patient outcomes across the entire care continuum.
📌 Remember: TEAMS approach to neurosurgical care - Team-based decisions, Evidence-based protocols, Advanced monitoring, Multidisciplinary rounds, Systematic follow-up. Team communication failures account for 60-70% of preventable complications in neurosurgery.
Perioperative management extends far beyond the operating room, encompassing preoperative optimization, intraoperative monitoring, and postoperative critical care. Enhanced recovery protocols reduce hospital length of stay by 20-30% while improving patient satisfaction.
- Integrated Care Pathways
- Preoperative: Medical optimization, anesthesia consultation, family education
- Intraoperative: Neuromonitoring, blood conservation, temperature management
- Postoperative: ICU protocols, early mobilization, rehabilitation planning
- ICU monitoring duration averages 24-48 hours for routine craniotomies
- Neurological assessments every 1-2 hours for first 24 hours
- Rehabilitation begins within 24-48 hours when medically stable
⭐ Clinical Pearl: Fast-track protocols in neurosurgery reduce ICU stay from 3-5 days to 1-2 days through standardized pathways, early extubation, and aggressive mobilization. Patient selection criteria include GCS ≥13, minimal brain swelling, and stable vital signs.
| Care Phase | Duration | Key Metrics | Monitoring Frequency | Complication Risk | Resource Intensity |
|---|---|---|---|---|---|
| Preoperative | 1-7 days | Medical clearance | Daily assessment | 5-10% | Low |
| Intraoperative | 2-8 hours | Vital signs, neuro | Continuous | 15-25% | Very High |
| ICU Phase | 1-5 days | ICP, GCS, vitals | Hourly | 20-30% | High |
| Ward Phase | 3-7 days | Neurological exam | Every 4-6 hours | 10-15% | Moderate |
| Rehabilitation | 2-12 weeks | Functional status | Weekly | 5-10% | Moderate |
💡 Master This: Intraoperative MRI changes surgical strategy in 25-30% of tumor cases, enabling real-time assessment of resection completeness. Navigation accuracy improves from ±3-5mm to ±1-2mm with updated imaging during surgery.
Quality improvement initiatives focus on standardized protocols, outcome measurement, and continuous improvement cycles. National databases track complication rates, functional outcomes, and patient satisfaction across multiple institutions.
- Quality Metrics Integration
- Process measures: Antibiotic timing, DVT prophylaxis, glucose control
- Outcome measures: Mortality rates, functional status, readmission rates
- Patient experience: Pain scores, communication ratings, discharge planning
- Mortality rates for elective craniotomy average 1-3%
- Functional independence at 6 months ranges 70-85%
- Patient satisfaction scores correlate with communication quality
📌 Remember: PDSA cycles for quality improvement - Plan interventions, Do implementation, Study results, Act on findings. Continuous improvement reduces complication rates by 15-25% over 2-3 year periods.
Research integration drives innovation in neurosurgical techniques, device development, and outcome optimization. Clinical trials evaluate new technologies, surgical approaches, and adjuvant therapies to advance patient care.
Understanding system integration enables optimal resource utilization and coordinated care delivery that maximizes patient outcomes while minimizing healthcare costs.
🔗 Advanced Integration: The Neurosurgical Ecosystem
🎯 Clinical Mastery Arsenal: Your Neurosurgical Command Center
Clinical excellence in neurosurgery demands integration of anatomical knowledge, surgical technique, complication management, and system coordination into seamless patient care. These essential tools form your clinical command center for neurosurgical practice.
📌 Remember: MASTER neurosurgery essentials - Monitor vitals continuously, Assess neurological status hourly, Systematic approach to complications, Team communication protocols, Evidence-based decisions, Rapid intervention when indicated.
Essential Clinical Thresholds for immediate action:
- Critical Parameters
- ICP: >20mmHg sustained requires immediate intervention
- CPP: <60mmHg indicates inadequate brain perfusion
- GCS: Drop ≥2 points mandates urgent imaging
- Pupil changes: >2mm difference suggests herniation
- Blood pressure: SBP >180 or <90mmHg needs correction
- Temperature: >38.5°C increases metabolic demand by 10-15%
⭐ Clinical Pearl: The 20-60-15 Rule - ICP <20mmHg, CPP >60mmHg, GCS >15 represent optimal targets for neurosurgical patients. Deviation from any parameter increases mortality risk by 15-25%.
| Emergency Scenario | Recognition Time | Intervention Window | Success Rate | Key Actions | Outcome Predictors |
|---|---|---|---|---|---|
| Herniation | <5 minutes | <15 minutes | 60-70% | Mannitol, surgery | Pupil reactivity |
| Hemorrhage | <2 minutes | <10 minutes | 70-80% | Control, repair | Volume, location |
| Seizure | <1 minute | <5 minutes | 90-95% | Anticonvulsants | Duration, type |
| Hydrocephalus | <30 minutes | <2 hours | 85-90% | CSF drainage | Ventricular size |
| Infection | <6 hours | <24 hours | 75-85% | Antibiotics, surgery | Organism, timing |
Rapid Assessment Tools:
📌 Remember: FOUR Score for comatose patients - Eye response (0-4), Motor response (0-4), Brainstem reflexes (0-4), Respiration pattern (0-4). Total score ≤8 indicates poor prognosis, while ≥12 suggests good recovery potential.
Surgical Decision Matrix for common scenarios:
- Trauma Protocols
- Epidural: Any volume with neurological decline
- Subdural: >10mm thickness or >5mm midline shift
- Contusion: >25mL volume with mass effect
- Decompressive craniectomy: ICP >25mmHg refractory to medical management
- ICP monitoring: GCS ≤8 with abnormal CT
- Hypothermia: 32-34°C for refractory ICP elevation
⭐ Clinical Pearl: Time is brain in neurosurgical emergencies - every 30-minute delay in surgical intervention increases mortality by 5-10% and poor functional outcome by 15-20%.
Communication Templates for critical situations:
💡 Master This: SBAR communication for neurosurgical emergencies - Situation (patient status), Background (relevant history), Assessment (current findings), Recommendation (proposed action). Clear communication reduces medical errors by 40-50%.
These clinical tools provide immediate access to critical information and decision algorithms that optimize patient outcomes in high-pressure situations.
🎯 Clinical Mastery Arsenal: Your Neurosurgical Command Center
Practice Questions: Neurosurgery Basics
Test your understanding with these related questions
A 41-year-old woman is brought to the emergency department by ambulance because of a sudden onset severe headache. On presentation, the patient also says that she is not able to see well. Physical examination shows ptosis of the right eye with a dilated pupil that is deviated inferiorly and laterally. Based on the clinical presentation, neurosurgery is immediately consulted and the patient is taken for an early trans-sphenoidal surgical decompression. Which of the following will also most likely need to be supplemented in this patient?













