Patient selection for minimally invasive approaches US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Patient selection for minimally invasive approaches. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
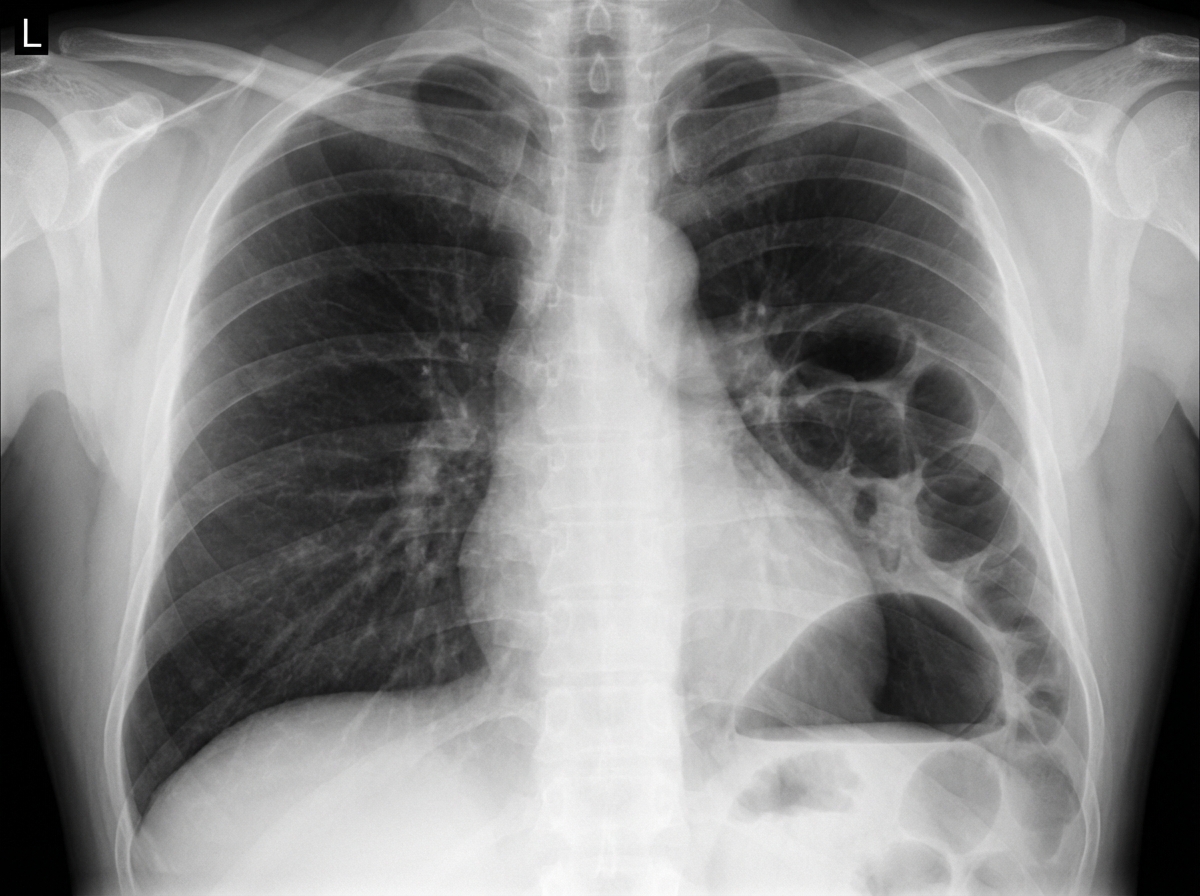
Patient selection for minimally invasive approaches US Medical PG Question 1: A 28-year-old man is brought to the emergency department with shortness of breath and chest pain, 35 minutes after he was involved in a high-speed motor vehicle collision. He was the helmeted driver of a scooter hit by a truck. On arrival, he is alert and oriented with a Glasgow Coma Scale rating of 14. His temperature is 37.3°C (99.1°F), pulse is 103/min, respirations are 33/min and blood pressure is 132/88 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 94%. Examination shows multiple abrasions over his abdomen and extremities. There is a 2.5-cm (1-in) laceration on the left side of the chest. There are decreased breath sounds over the left base. Cardiac examination shows no abnormalities. The abdomen is soft and there is tenderness to palpation over the left upper quadrant. Bowel sounds are normal. His hemoglobin concentration is 13.6 g/dL, leukocyte count is 9,110/mm3, and platelet count is 190,000/mm3. A chest x-ray is shown. Which of the following is the most likely diagnosis?
- A. Pneumothorax
- B. Phrenic nerve palsy
- C. Esophageal perforation
- D. Diaphragmatic rupture (Correct Answer)
- E. Diaphragmatic eventration
Patient selection for minimally invasive approaches Explanation: ***Diaphragmatic rupture***
- The patient's history of **high-speed motor vehicle collision**, **shortness of breath**, **chest pain**, **decreased breath sounds at the left base**, and **abdominal tenderness in the left upper quadrant** (suggesting possible visceral herniation) are all highly consistent with a diaphragmatic rupture.
- A **chest X-ray** showing an elevated hemidiaphragm, abnormal bowel gas patterns in the chest, or gastric bubble in the thoracic cavity would further support this diagnosis, given the clinical context.
*Pneumothorax*
- While a **pneumothorax** can cause sudden shortness of breath and chest pain and decreased breath sounds, the presence of **left upper quadrant abdominal tenderness** and the mechanism of injury make diaphragmatic rupture more likely as the primary diagnosis.
- A pneumothorax would typically present with a collapsed lung on chest X-ray but would not explain the abdominal symptoms.
*Phrenic nerve palsy*
- **Phrenic nerve palsy** typically causes paralysis of the diaphragm, leading to respiratory compromise and an elevated hemidiaphragm on imaging, but it's usually **atraumatic** or a complication of surgery, not acute trauma.
- It would not explain the acute onset of pain and tenderness after a high-speed collision.
*Esophageal perforation*
- **Esophageal perforation** would cause severe chest pain, often radiating to the back, and can lead to mediastinitis, but it is less likely to present with decreased breath sounds at the base and left upper quadrant tenderness.
- A history of significant **vomiting** or **instrumentation** is often associated with esophageal perforation, which is absent here.
*Diaphragmatic eventration*
- **Diaphragmatic eventration** is a congenital thinning of the diaphragm leading to its elevation, but it is a **chronic condition** and would not present acutely after a high-speed collision.
- It is typically asymptomatic or causes chronic respiratory symptoms, not acute traumatic symptoms.
Patient selection for minimally invasive approaches US Medical PG Question 2: A 62-year-old man comes to the physician in May for a routine health maintenance examination. He feels well. He underwent a right inguinal hernia repair 6 months ago. He has hypertension and type 2 diabetes mellitus. There is no family history of serious illness. Current medications include metformin, sitagliptin, enalapril, and metoprolol. He received the zoster vaccine 1 year ago. He received the PPSV23 vaccine 4 years ago. His last colonoscopy was 7 years ago and was normal. He smoked a pack of cigarettes a day for 20 years but quit 17 years ago. He drinks two to three alcoholic beverages on weekends. He is allergic to amoxicillin. He is scheduled to visit Australia and New Zealand in 2 weeks to celebrate his 25th wedding anniversary. He appears healthy. Vital signs are within normal limits. An S4 is heard at the apex. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate recommendation at this time?
- A. Colonoscopy
- B. Influenza vaccine (Correct Answer)
- C. Pneumococcal conjugate vaccine 13
- D. Cardiac stress test
- E. Abdominal ultrasound
Patient selection for minimally invasive approaches Explanation: ***Influenza vaccine***
- Current guidelines recommend annual **influenza vaccination** for all adults, particularly those over 60 years old and those with chronic medical conditions like diabetes and hypertension.
- **Critical timing consideration**: The patient is traveling to Australia and New Zealand (Southern Hemisphere) in 2 weeks, where it will be **winter season** (May-September) with peak influenza activity.
- He is a **high-risk patient** (age >60, diabetes, hypertension, cardiovascular disease) who should receive influenza vaccine before travel to areas experiencing influenza season.
- This is the **most appropriate and time-sensitive recommendation** at this visit.
*Colonoscopy*
- The patient had a normal colonoscopy 7 years ago; current guidelines suggest a repeat colonoscopy every **10 years** for average-risk individuals.
- There are no new symptoms, family history, or risk factors that would necessitate an earlier repeat colonoscopy at this time.
*Pneumococcal conjugate vaccine 13*
- The patient received **PPSV23** four years ago at approximately age 58.
- Per **current CDC guidelines (2019+)**, PCV13 is **no longer routinely recommended** for immunocompetent adults ≥65 years old.
- PPSV23 alone is now the standard recommendation for adults ≥65, which this patient has already received.
- PCV13 may be considered through **shared decision-making** in specific circumstances, but is not a routine or urgent recommendation.
*Cardiac stress test*
- Although the patient has risk factors for cardiovascular disease (hypertension, diabetes, former smoker) and an **S4 heart sound** (indicating **left ventricular hypertrophy**), he is asymptomatic.
- Routine **screening stress tests** are not recommended for asymptomatic individuals without signs of active cardiac ischemia.
*Abdominal ultrasound*
- There are **no symptoms** or specific indications (e.g., abdominal aortic aneurysm screening criteria not met - would need age 65-75 with smoking history).
- The patient is 62 years old and quit smoking 17 years ago, so AAA screening criteria are not yet met.
- Routine screening abdominal ultrasounds are not indicated.
Patient selection for minimally invasive approaches US Medical PG Question 3: A 27-year-old man presents to the emergency department after being stabbed. The patient was robbed at a local pizza parlor and was stabbed over 10 times with a large kitchen knife with an estimated 7 inch blade in the ventral abdomen. His temperature is 97.6°F (36.4°C), blood pressure is 74/54 mmHg, pulse is 180/min, respirations are 19/min, and oxygen saturation is 98% on room air. The patient is intubated and given blood products and vasopressors. Physical exam is notable for multiple stab wounds over the patient's abdomen inferior to the nipple line. Which of the following is the best next step in management?
- A. Exploratory laparotomy (Correct Answer)
- B. Diagnostic peritoneal lavage
- C. CT scan of the abdomen and pelvis
- D. Exploratory laparoscopy
- E. FAST exam
Patient selection for minimally invasive approaches Explanation: ***Exploratory laparotomy***
- The patient presents with **multiple stab wounds** to the abdomen and signs of **hemorrhagic shock** (BP 74/54 mmHg, HR 180/min), which are clear indications for immediate surgical intervention.
- An exploratory laparotomy allows for direct visualization and repair of internal injuries, which is critical in this life-threatening situation.
*Diagnostic peritoneal lavage*
- While DPL can detect intra-abdominal bleeding, it is an **invasive procedure** and may delay definitive treatment in a hemodynamically unstable patient with obvious penetrating trauma.
- It is **less specific** than a laparotomy for identifying the exact location and nature of injuries, and it has largely been replaced by imaging studies or direct surgical exploration in unstable patients.
*CT scan of the abdomen and pelvis*
- A CT scan requires a **hemodynamically stable** patient and time for scanning and interpretation, which this patient does not have.
- Delaying definitive treatment for imaging in a patient with severe shock could lead to worse outcomes.
*Exploratory laparoscopy*
- Although less invasive, laparoscopy can be time-consuming and may not be feasible or safe in a patient with **profound hemorrhagic shock** and extensive injuries, especially if major vascular or visceral damage is suspected.
- Conversion to a **laparotomy** is often necessary in cases of significant injury, making immediate open exploration more efficient.
*FAST exam*
- A FAST exam can rapidly detect free fluid in the abdomen, suggesting internal bleeding, but it does **not provide specific information** about the source or extent of the injuries.
- While useful in the initial assessment, a positive FAST exam in a hemodynamically unstable patient with penetrating trauma directly points to the need for immediate surgical intervention, not further diagnostic delay.
Patient selection for minimally invasive approaches US Medical PG Question 4: A 68-year-old man comes to the physician because of recurrent episodes of nausea and abdominal discomfort for the past 4 months. The discomfort is located in the upper abdomen and sometimes occurs after eating, especially after a big meal. He has tried to go for a walk after dinner to help with digestion, but his complaints have only increased. For the past 3 weeks he has also had symptoms while climbing the stairs to his apartment. He has type 2 diabetes mellitus, hypertension, and stage 2 peripheral arterial disease. He has smoked one pack of cigarettes daily for the past 45 years. He drinks one to two beers daily and occasionally more on weekends. His current medications include metformin, enalapril, and aspirin. He is 168 cm (5 ft 6 in) tall and weighs 126 kg (278 lb); BMI is 45 kg/m2. His temperature is 36.4°C (97.5°F), pulse is 78/min, and blood pressure is 148/86 mm Hg. On physical examination, the abdomen is soft and nontender with no organomegaly. Foot pulses are absent bilaterally. An ECG shows no abnormalities. Which of the following is the most appropriate next step in diagnosis?
- A. CT scan of the abdomen
- B. Abdominal ultrasonography of the right upper quadrant
- C. Esophagogastroduodenoscopy
- D. Hydrogen breath test
- E. Cardiac stress test (Correct Answer)
Patient selection for minimally invasive approaches Explanation: ***Cardiac stress test***
- The patient's **epigastric discomfort** that is exacerbated by exertion (walking, climbing stairs) and presents with several **cardiovascular risk factors** (obesity, type 2 diabetes mellitus, hypertension, smoking, peripheral arterial disease) strongly suggests **ischemic heart disease** as the cause of his abdominal symptoms.
- A **cardiac stress test** is the most appropriate next step to evaluate for **exercise-induced myocardial ischemia**, which can manifest as referred pain to the epigastrium (angina equivalent).
- This patient has a high pretest probability of coronary artery disease, making functional cardiac testing essential before pursuing other diagnostic workup.
*CT scan of the abdomen*
- A CT scan of the abdomen would be indicated for evaluating structural abnormalities of abdominal organs, but the **exertional nature** of the patient's symptoms makes **cardiac ischemia** a more pressing concern.
- While it could rule out other abdominal pathologies, it would not address the likely cardiac origin of his symptoms.
*Abdominal ultrasonography of the right upper quadrant*
- Abdominal ultrasonography is used to evaluate organs like the **gallbladder, liver, and pancreas** for conditions such as **cholelithiasis or cholecystitis**.
- The patient's symptoms are more consistent with **exertional pain** rather than typical biliary colic, making cardiac evaluation a higher priority.
*Esophagogastroduodenoscopy*
- An **EGD** is used to visualize the **esophagus, stomach, and duodenum** to diagnose conditions like **peptic ulcer disease, esophagitis, or gastritis**.
- While **upper GI symptoms** are present, the exacerbation with exertion shifts the focus away from primary gastrointestinal pathology toward cardiac causes.
*Hydrogen breath test*
- A **hydrogen breath test** is primarily used to diagnose **small intestinal bacterial overgrowth (SIBO)** or **carbohydrate malabsorption** (e.g., lactose intolerance).
- The patient's symptoms are not classic for SIBO or malabsorption, and the **exertional component** makes this a less probable diagnosis.
Patient selection for minimally invasive approaches US Medical PG Question 5: A 25-year-old woman presents to a physician for a new patient physical exam. Aside from occasional shin splints, she has a relatively unremarkable medical history. She takes oral contraceptive pills as scheduled and a multivitamin daily. She reports no known drug allergies. All of her age appropriate immunizations are up to date. Her periods have been regular, occurring once every 28 to 30 days with normal flow. She is sexually active with two partners, who use condoms routinely. She works as a cashier at the local grocery store. Her mother has diabetes and coronary artery disease, and her father passed away at age 45 after being diagnosed with colon cancer at age 40. Her grand-aunt underwent bilateral mastectomies after being diagnosed with breast cancer at age 60. Her physical exam is unremarkable. Which of the following is the best recommendation for this patient?
- A. Colonoscopy in 10 years
- B. Mammogram now
- C. Pap smear now
- D. Pap smear in 5 years
- E. HPV DNA testing now (Correct Answer)
Patient selection for minimally invasive approaches Explanation: ***HPV DNA testing now***
- This 25-year-old patient is due for cervical cancer screening and this is the best recommendation.
- **ACOG (2021)** recommends **primary HPV testing every 5 years** for women aged 25-65 as the preferred screening method.
- Although USPSTF guidelines recommend starting HPV testing at age 30, ACOG's updated guidelines support initiating primary HPV testing at age 25, making this the most current evidence-based recommendation.
- Given she is presenting for a new patient physical and cervical cancer screening is due now, initiating HPV testing is appropriate.
*Colonoscopy in 10 years*
- While the patient's father was diagnosed with colon cancer at age 40, this option is **incorrectly timed**.
- Guidelines recommend screening beginning at age 40 OR 10 years before the youngest affected first-degree relative's diagnosis (age 30 for this patient), whichever comes first.
- Since this patient is 25, she would need colonoscopy at age 30 (in 5 years), not in 10 years (age 35).
- However, cervical cancer screening is the more immediate priority right now.
*Mammogram now*
- The patient's grand-aunt had breast cancer at age 60, but this is a **second-degree relative** with late-onset disease.
- This does not meet criteria for early mammography screening at age 25.
- Routine mammography typically begins at age 40 (per ACOG) or age 50 (per USPSTF), unless there is a strong family history in first-degree relatives or genetic mutations (BRCA1/2).
*Pap smear now*
- Pap smear (cytology) is an acceptable screening option for cervical cancer.
- **USPSTF (2018)** recommends cytology alone every 3 years for women ages 21-29, or starting HPV-based testing at age 30.
- However, **ACOG (2021)** supports primary HPV testing starting at age 25 as the preferred method.
- While Pap smear now would not be incorrect, HPV DNA testing is the preferred and more current guideline-based approach for this age group.
*Pap smear in 5 years*
- This represents inappropriate delay in initiating cervical cancer screening.
- Screening should begin now, not be deferred for 5 years.
- The 5-year interval applies to primary HPV testing once initiated, not to delaying the start of screening.
Patient selection for minimally invasive approaches US Medical PG Question 6: A 32-year-old man is brought to the emergency department after a skiing accident. The patient had been skiing down the mountain when he collided with another skier who had stopped suddenly in front of him. He is alert but complaining of pain in his chest and abdomen. He has a past medical history of intravenous drug use and peptic ulcer disease. He is a current smoker. His temperature is 97.4°F (36.3°C), blood pressure is 77/53 mmHg, pulse is 127/min, and respirations are 13/min. He has a GCS of 15 and bilateral shallow breath sounds. His abdomen is soft and distended with bruising over the epigastrium. He is moving all four extremities and has scattered lacerations on his face. His skin is cool and delayed capillary refill is present. Two large-bore IVs are placed in his antecubital fossa, and he is given 2L of normal saline. His FAST exam reveals fluid in Morison's pouch. Following the 2L normal saline, his temperature is 97.5°F (36.4°C), blood pressure is 97/62 mmHg, pulse is 115/min, and respirations are 12/min.
Which of the following is the best next step in management?
- A. Diagnostic peritoneal lavage
- B. Emergency laparotomy (Correct Answer)
- C. Upper gastrointestinal endoscopy
- D. Close observation
- E. Diagnostic laparoscopy
Patient selection for minimally invasive approaches Explanation: ***Emergency laparotomy***
- The patient remains **hemodynamically unstable** (BP 97/62 mmHg, HR 115/min after 2L IV fluids) with evidence of **intra-abdominal fluid on FAST exam** (fluid in Morison's pouch).
- This clinical picture indicates active intra-abdominal hemorrhage requiring **immediate surgical intervention** to identify and control the source of bleeding.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has largely been replaced by the focused abdominal sonography for trauma (FAST) exam and CT scans.
- While it can detect intra-abdominal bleeding, it is **invasive** and would delay definitive treatment in a hemodynamically unstable patient with positive FAST.
*Upper gastrointestinal endoscopy*
- This procedure is primarily for diagnosing and treating **upper gastrointestinal bleeding** or mucosal abnormalities.
- It is **not indicated** for evaluating traumatic intra-abdominal hemorrhage or hemodynamic instability following blunt abdominal trauma.
*Close observation*
- Close observation is appropriate for **hemodynamically stable patients** with blunt abdominal trauma and minor injuries or equivocal findings.
- This patient's persistent hypotension, tachycardia, and positive FAST findings rule out observation as a safe or appropriate next step.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a minimally invasive surgical procedure used to evaluate the abdominal cavity.
- While it can be diagnostic, it is generally **contraindicated in hemodynamically unstable patients** as it can prolong the time to definitive hemorrhage control if a major injury is found.
Patient selection for minimally invasive approaches US Medical PG Question 7: A 68-year-old man comes to the emergency department because of sudden onset abdominal pain for 6 hours. On a 10-point scale, he rates the pain as a 8 to 9. The abdominal pain is worst in the right upper quadrant. He has atrial fibrillation and hyperlipidemia. His temperature is 38.7° C (101.7°F), pulse is 110/min, and blood pressure is 146/86 mm Hg. The patient appears acutely ill. Physical examination shows a distended abdomen and tenderness to palpation in all quadrants with guarding, but no rebound. Murphy's sign is positive. Right upper quadrant ultrasound shows thickening of the gallbladder wall, sludging in the gallbladder, and pericolic fat stranding. He is admitted for acute cholecystitis and grants permission for cholecystectomy. His wife is his healthcare power of attorney (POA), but she is out of town on a business trip. He is accompanied today by his brother. After induction and anesthesia, the surgeon removes the gallbladder but also finds a portion of the small intestine is necrotic due to a large thromboembolism occluding a branch of the superior mesenteric artery. The treatment is additional surgery with small bowel resection and thromboendarterectomy. Which of the following is the most appropriate next step in management?
- A. Decrease the patient's sedation until he is able to give consent
- B. Contact the patient's healthcare POA to consent
- C. Proceed with additional surgery without obtaining consent (Correct Answer)
- D. Ask the patient's brother in the waiting room to consent
- E. Close the patient and obtain re-consent for a second operation
Patient selection for minimally invasive approaches Explanation: ***Proceed with additional surgery without obtaining consent***
- In an **emergency situation** where immediate intervention is required to save a patient's life or prevent serious harm, and the patient **lacks capacity** to consent, explicit consent for additional necessary procedures is not required. The surgeon can proceed based on the principle of **implied consent** in emergencies.
- The discovery of **necrotic small bowel due to thromboembolism** is a life-threatening condition requiring urgent surgical intervention in an already sedated patient, making it an emergency.
*Decrease the patient's sedation until he is able to give consent*
- Decreasing sedation to obtain consent in this critical situation would cause a **dangerous delay** in treating a life-threatening condition (bowel necrosis) and could lead to worsening outcomes or death.
- The patient is **acutely ill** and likely in a state where he cannot grasp information and make decisions, even with reduced sedation, thus true informed consent would be difficult to obtain quickly.
*Contact the patient's healthcare POA to consent*
- Contacting the POA who is out of town would introduce **significant and potentially fatal delays** in treating a rapidly progressing, life-threatening condition.
- While POAs are crucial for non-emergent decision-making, the **principle of preserving life** takes precedence in an acute emergency when a delay would cause irreversible harm.
*Ask the patient's brother in the waiting room to consent*
- The brother is **not the designated healthcare POA** and there is no indication he has legal authority to make medical decisions for the patient.
- Relying on a non-POA family member for consent in an emergency, when the patient's legally appointed surrogate is known, is generally **not the appropriate first step** unless no other option exists and the brother can confirm the patient's wishes from prior discussions, which is not stated.
*Close the patient and obtain re-consent for a second operation*
- Closing the patient and then re-opening for another surgery would expose the patient to **two separate anesthetic events and surgical procedures**, significantly increasing morbidity and mortality risks compared to continuous surgery.
- This option would also introduce an **unacceptable delay** in addressing the acute bowel necrosis, which requires immediate intervention.
Patient selection for minimally invasive approaches US Medical PG Question 8: A 63-year-old man undergoes workup for nocturnal dyspnea and what he describes as a "choking" sensation while sleeping. He also endorses fatigue and dyspnea on exertion. Physical exam reveals a normal S1, loud P2, and a neck circumference of 17 inches (43 cm) (normal < 14 inches (< 35 cm)). His temperature is 98.8°F (37°C), blood pressure is 128/82 mmHg, pulse is 86/min, and respirations are 19/min. He undergoes spirometry, which is unrevealing, and polysomnography, which shows 16 hypopneic and apneic events per hour. Mean pulmonary arterial pressure is 30 mmHg. Which of the following complications is this patient most at risk for?
- A. Left ventricular failure
- B. Right ventricular failure (Correct Answer)
- C. Pulmonary embolism
- D. Aspiration pneumonia
- E. Chronic obstructive pulmonary disease
Patient selection for minimally invasive approaches Explanation: ***Right ventricular failure***
- The patient's symptoms (nocturnal dyspnea, choking sensation, fatigue, exertional dyspnea), risk factors (large neck circumference), and polysomnography results (16 hypopneic/apneic events/hour) are consistent with **obstructive sleep apnea (OSA)**.
- OSA leads to **chronic intermittent hypoxia** and hypercapnia, causing **pulmonary vasoconstriction** and increased pulmonary arterial pressure (mean PAP 30 mmHg), which can result in **pulmonary hypertension** and eventually **right ventricular failure**.
*Left ventricular failure*
- While OSA can exacerbate cardiovascular conditions, the primary cardiac complication directly resulting from ongoing pulmonary hypertension due to OSA is typically right-sided, not primarily left-sided, failure.
- There are no specific findings in the description (e.g., S3 gallop, crackles) that strongly point to left ventricular dysfunction as the most immediate and direct complication.
*Pulmonary embolism*
- Although obesity (suggested by large neck circumference) is a risk factor for pulmonary embolism, there are no acute symptoms (e.g., sudden onset dyspnea, pleuritic chest pain, hemoptysis) or signs (e.g., tachycardia, hypoxemia) to suggest a pulmonary embolism.
- The patient's symptoms are chronic and related to sleep-disordered breathing and pulmonary hypertension.
*Aspiration pneumonia*
- While a "choking" sensation could potentially lead to aspiration, there's no evidence of infection (e.g., fever, productive cough, crackles) or recurrent aspiration events.
- The primary respiratory pathology is clearly defined by the polysomnography and elevated pulmonary pressures.
*Chronic obstructive pulmonary disease*
- Spirometry was reported as "unrevealing," which rules out significant airflow limitation characteristic of COPD.
- The patient's symptoms are more indicative of sleep-disordered breathing and its cardiovascular consequences rather than an intrinsic obstructive lung disease like COPD.
Patient selection for minimally invasive approaches US Medical PG Question 9: A 45-year-old woman comes to the emergency department complaining of abdominal pain for the past day. The pain is situated in the right upper quadrant, colicky, 8/10, and radiates to the tip of the right shoulder with no aggravating or relieving factors. The pain is associated with nausea but no vomiting. She tried to take over-the-counter antacids which relieved her pain to a certain extent, but not entirely. She does not smoke cigarettes or drink alcohol. She has no past medical illness. Her father died of pancreatic cancer at the age of 75, and her mother has diabetes controlled with medications. Temperature is 38°C (100.4°F), blood pressure is 125/89 mm Hg, pulse is 104/min, respiratory rate is 20/min, and BMI is 29 kg/m2. On abdominal examination, her abdomen is tender to shallow and deep palpation of the right upper quadrant.
Laboratory test
Complete blood count
Hemoglobin 13 g/dL
WBC 15,500/mm3
Platelets 145,000/mm3
Basic metabolic panel
Serum Na+ 137 mEq/L
Serum K+ 3.6 mEq/L
Serum Cl- 95 mEq/L
Serum HCO3- 25 mEq/L
BUN 10 mg/dL
Serum creatinine 0.8 mg/dL
Liver function test
Total bilirubin 1.3 mg/dL
AST 52 U/L
ALT 60 U/L
Ultrasonography of the abdomen shows normal findings. What is the best next step in management of this patient?
- A. Emergency cholecystectomy
- B. CT scan
- C. Reassurance and close follow up
- D. Cholescintigraphy (Correct Answer)
- E. Percutaneous cholecystostomy
Patient selection for minimally invasive approaches Explanation: ***Cholescintigraphy***
- The patient presents with **right upper quadrant pain**, fever, **leukocytosis**, and elevated liver enzymes, pointing towards **acute cholecystitis**. Despite a normal ultrasound, cholescintigraphy (HIDA scan) is the gold standard for diagnosing acute cholecystitis when imaging is equivocal.
- Cholescintigraphy can assess the **patency of the cystic duct**, which is often obstructed in acute cholecystitis, by observing whether the gallbladder fills with tracer.
*Emergency cholecystectomy*
- **Acute cholecystitis** usually requires cholecystectomy, but it's typically performed **after confirmation** of the diagnosis, often after a period of stabilization with antibiotics and fluids, not immediately as an emergency for this stable patient.
- There is no evidence of severe complications such as **gallbladder perforation** or gangrene that would necessitate immediate emergency surgery without further diagnostic confirmation.
*CT scan*
- A **CT scan** is not the primary imaging modality for acute cholecystitis as it is **less sensitive** than ultrasound or cholescintigraphy for detecting gallbladder inflammation and cystic duct obstruction.
- While CT can identify complications such as abscess formation or perforation, the initial diagnostic work-up should focus on confirming the inflammation of the gallbladder itself.
*Reassurance and close follow up*
- The patient's symptoms (severe **colicky pain**, fever, **leukocytosis**, elevated liver enzymes) indicate an **acute inflammatory process** requiring active medical management and diagnosis, not mere reassurance.
- Delaying appropriate diagnosis and treatment for acute cholecystitis can lead to severe complications like gallbladder perforation, sepsis, or cholangitis.
*Percutaneous cholecystostomy*
- **Percutaneous cholecystostomy** is generally reserved for patients with acute cholecystitis who are **too unstable for surgery**, or in cases where surgical risk is very high.
- The patient is hemodynamically stable and does not have contraindications for surgery, making a definitive surgical approach (after diagnosis) preferable over a temporizing measure.
Patient selection for minimally invasive approaches US Medical PG Question 10: A 32-year-old woman undergoes laparoscopic excision of ovarian endometrioma. During surgery with the patient in Trendelenburg position and pneumoperitoneum at 15 mmHg, the anesthesiologist notes peak airway pressures rising from 25 to 40 cmH2O, oxygen saturation dropping to 88%, and blood pressure decreasing. Apply the appropriate immediate intervention.
- A. Increase tidal volume and respiratory rate
- B. Increase FiO2 and administer fluid bolus only
- C. Release pneumoperitoneum and decrease Trendelenburg (Correct Answer)
- D. Administer bronchodilators for bronchospasm
- E. Check for endobronchial intubation and reposition tube
Patient selection for minimally invasive approaches Explanation: ***Release pneumoperitoneum and decrease Trendelenburg***
- High **peak airway pressures** (40 cmH2O), **hypoxemia**, and **hypotension** indicate severe physiological compromise from **pneumoperitoneum** and positioning.
- Releasing the gas and leveling the patient immediately facilitates **diaphragmatic descent**, increases **lung compliance**, and restores **venous return** to improve cardiac output.
*Increase tidal volume and respiratory rate*
- Increasing **tidal volume** in the presence of already high airway pressures significantly increases the risk of **barotrauma** and further cardiovascular collapse.
- This intervention does not address the mechanical cause of **diaphragmatic splinting** caused by the CO2 insufflation.
*Increase FiO2 and administer fluid bolus only*
- While oxygenation may temporarily improve, this fails to correct the **reduced functional residual capacity** caused by the **positive pressure** in the abdomen.
- Fluids may not compensate for the **inferior vena cava compression** if the source of high **intra-abdominal pressure** remains unchanged.
*Administer bronchodilators for bronchospasm*
- High airway pressures in laparoscopy are usually due to **decreased thoracic compliance**, not necessarily **bronchospasm**.
- The sudden drop in blood pressure suggests a hemodynamic/mechanical cause rather than an isolated **obstructive lung** pathology.
*Check for endobronchial intubation and reposition tube*
- While cephalad movement of the diaphragm can cause **endobronchial intubation**, it does not typically explain the systemic **hypotension** seen here.
- This step should follow the **immediate release** of abdominal pressure, which is the most life-threatening contributor to the current vitals.
More Patient selection for minimally invasive approaches US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.