Laparoscopic surgery principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Laparoscopic surgery principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Laparoscopic surgery principles US Medical PG Question 1: A research scientist attempts to understand the influence of carbon dioxide content in blood on its oxygen binding. The scientist adds carbon dioxide to dog blood and measures the uptake of oxygen in the blood versus oxygen pressure in the peripheral tissue. He notes in one dog that with the addition of carbon dioxide with a pressure of 90 mmHg, the oxygen pressure in the peripheral tissue rose from 26 to 33 mmHg. How can this phenomenon be explained?
- A. High partial pressure of CO2 in tissues decreases peripheral blood volume
- B. Binding of O2 to hemoglobin in lungs drives release of CO2 from hemoglobin
- C. High partial pressure of CO2 in tissues causes alkalemia, which is necessary for O2 unloading
- D. High partial pressure of CO2 in tissues facilitates O2 unloading in peripheral tissues (Correct Answer)
- E. The sum of the partial pressures of CO2 and O2 cannot exceed a known threshold in blood
Laparoscopic surgery principles Explanation: **High partial pressure of CO2 in tissues facilitates O2 unloading in peripheral tissues**
- An increase in **PCO2** leads to a decrease in pH (acidosis) in the tissues, which **decreases hemoglobin's affinity for oxygen**, promoting oxygen release.
- This phenomenon is known as the **Bohr effect**, where an acidic environment (from CO2) shifts the oxygen dissociation curve to the right, enhancing O2 unloading to meet tissue metabolic demands.
*High partial pressure of CO2 in tissues decreases peripheral blood volume*
- **Increased CO2** generally causes vasodilation in peripheral tissues, which would lead to an **increase**, not a decrease, in peripheral blood flow.
- Decreased blood volume is typically associated with conditions like hypovolemia or intense vasoconstriction, not elevated tissue CO2.
*Binding of O2 to hemoglobin in lungs drives release of CO2 from hemoglobin*
- This statement describes the **Haldane effect**, which occurs primarily in the lungs, where oxygen binding to hemoglobin facilitates the release of CO2.
- While true, it does not explain the **increased oxygen pressure in peripheral tissue** observed with added CO2, which is related to O2 unloading.
*High partial pressure of CO2 in tissues causes alkalemia, which is necessary for O2 unloading*
- High **PCO2** in tissues leads to the formation of carbonic acid and H+ ions, resulting in a **decrease in pH (acidosis)**, not alkalemia.
- **Acidosis** facilitates O2 unloading (Bohr effect), whereas alkalemia would increase hemoglobin's affinity for O2, inhibiting unloading.
*The sum of the partial pressures of CO2 and O2 cannot exceed a known threshold in blood*
- There is **no fixed threshold** for the sum of partial pressures of CO2 and O2 in the blood; these gases are independently regulated and their partial pressures fluctuate with metabolic activity.
- The partial pressure of a gas reflects its concentration and does not have an upper limit when considering the sum of different gases.
Laparoscopic surgery principles US Medical PG Question 2: A 67-year-old woman has fallen from the second story level of her home while hanging laundry. She was brought to the emergency department immediately and presented with severe abdominal pain. The patient is anxious, and her hands and feet feel very cold to the touch. There is no evidence of bone fractures, superficial skin wounds, or a foreign body penetration. Her blood pressure is 102/67 mm Hg, respirations are 19/min, pulse is 87/min, and temperature is 36.7°C (98.0°F). Her abdominal exam reveals rigidity and severe tenderness. A Foley catheter and nasogastric tube are inserted. The central venous pressure (CVP) is 5 cm H2O. The medical history is significant for hypertension. Which of the following is best indicated for the evaluation of this patient?
- A. X-Ray
- B. Ultrasound
- C. Peritoneal lavage
- D. CT scan (Correct Answer)
- E. Diagnostic laparotomy
Laparoscopic surgery principles Explanation: ***CT scan***
- A **CT scan of the abdomen and pelvis** is the most indicated imaging modality for evaluating blunt abdominal trauma due to its high sensitivity and specificity in detecting solid organ injuries, free fluid, and active bleeding.
- Given the patient's severe abdominal pain, rigidity, and tenderness after a significant fall, a CT scan will provide detailed anatomical information crucial for guiding further management.
*X-Ray*
- An **X-ray** is useful for detecting bone fractures, but it has limited utility in assessing soft tissue and organ injuries within the abdomen.
- It would not effectively visualize internal bleeding or organ damage, which are primary concerns in this patient given the mechanism of injury and symptoms.
*Ultrasound*
- An **ultrasound (FAST exam)** is effective for rapid detection of free fluid in the abdomen (indicating bleeding or fluid leakage) and can be done at the bedside.
- However, it is operator-dependent and less sensitive than CT for identifying specific organ injuries, retroperitoneal hematomas, or the source of bleeding.
*Peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** is an invasive procedure primarily used to detect intra-abdominal bleeding in hemodynamically unstable patients, but it has largely been replaced by ultrasound and CT in stable patients.
- While it can detect blood, it is less specific for identifying the source of bleeding and does not provide anatomical detail, and carries risks of complications like bowel perforation.
*Diagnostic laparotomy*
- **Diagnostic laparotomy** is a surgical procedure to directly visualize abdominal contents and is indicated in cases of clear signs of peritonitis, hemodynamic instability with confirmed intra-abdominal bleeding, or evisceration.
- It is an invasive intervention and would not be the initial diagnostic step in a hemodynamically stable patient without clear indication for immediate surgery.
Laparoscopic surgery principles US Medical PG Question 3: A 27-year-old man is brought to the emergency department after a motor vehicle accident. He was the unrestrained driver in a head on collision. The patient is responding incoherently and is complaining of being in pain. He has several large lacerations and has been impaled with a piece of metal. IV access is unable to be obtained and a FAST exam is performed. His temperature is 98.2°F (36.8°C), blood pressure is 90/48 mmHg, pulse is 150/min, respirations are 13/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Reattempt intravenous access
- B. Obtain intraosseous access (Correct Answer)
- C. Place a central line
- D. Administer oral fluids
- E. Exploratory laparotomy
Laparoscopic surgery principles Explanation: ***Obtain intraosseous access***
- The patient is in **hypotensive shock** (BP 90/48 mmHg, HR 150/min) after a severe trauma, and **IV access cannot be obtained**. **Intraosseous (IO) access** provides a rapid and reliable route for fluid and medication administration in emergent situations when peripheral IV access is difficult or impossible.
- While central line placement is also a viable option, **IO access is generally faster and easier to establish** in an emergency setting by a wide range of providers, making it the **best initial step** when peripheral IV fails.
*Reattempt intravenous access*
- Although obtaining IV access is critical, the question states that it "is unable to be obtained," implying initial attempts have failed or are proving too difficult/time-consuming given the patient's critical state.
- Persisting with repeated attempts risks significant delay in resuscitation, which is detrimental for a patient in shock.
*Place a central line*
- A central line provides reliable access for fluid and medication, but its placement is generally **more time-consuming** and technically challenging than IO access, especially in an agitated, unstable patient in a chaotic emergency setting.
- The immediate priority is rapid access for fluids to address the patient's shock, for which IO is superior in terms of speed of establishment.
*Administer oral fluids*
- The patient is **unstable**, **incoherently responding**, and likely has significant internal injuries given the mechanism of injury (head-on collision, impalement).
- Oral fluids would be **ineffective** and potentially dangerous (risk of aspiration) in this critical, hemodynamically unstable patient who requires immediate intravenous fluid resuscitation.
*Exploratory laparotomy*
- While the patient likely has significant internal injuries requiring surgical intervention (impalement, hypovolemic shock), an **exploratory laparotomy** is a definitive treatment step, not the *best next step in management* for immediate resuscitation.
- **Hemodynamic stabilization** with fluid resuscitation must occur *before* or *simultaneously with* definitive surgical intervention to improve survival chances.
Laparoscopic surgery principles US Medical PG Question 4: A 41-year-old man is admitted to the emergency room after being struck in the abdomen by a large cement plate while transporting it. On initial assessment by paramedics at the scene, his blood pressure was 110/80 mm Hg, heart rate 85/min, with no signs of respiratory distress. On admission, the patient is alert but in distress. He complains of severe, diffuse, abdominal pain and severe weakness. Vital signs are now: blood pressure 90/50 mm Hg, heart rate 96/min, respiratory rate 19/min, temperature 37.4℃ (99.3℉), and oxygen saturation of 95% on room air. His lungs are clear on auscultation. The cardiac exam is significant for a narrow pulse pressure. Abdominal examination reveals a large bruise over the epigastric and periumbilical regions. The abdomen is distended and there is diffuse tenderness to palpation with rebound and guarding, worst in the epigastric region. There is hyperresonance to percussion in the epigastric region and absence of hepatic dullness in the right upper quadrant. Aspiration of the nasogastric tube reveals bloody contents. Focused assessment with sonography for trauma (FAST) shows free fluid in the pelvic region. Evaluation of the perisplenic and perihepatic regions is impossible due to the presence of free air. Aggressive intravenous fluid resuscitation is administered but fails to improve upon the patient’s hemodynamics. Which of the following is the next best step in management?
- A. Emergency laparoscopy
- B. Abdominal ultrasound
- C. Diagnostic peritoneal lavage (DPL)
- D. Emergency laparotomy (Correct Answer)
- E. CT scan
Laparoscopic surgery principles Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** unresponsive to fluid resuscitation, coupled with clear signs of **perforation** (hyperresonance, absent hepatic dullness, free air on FAST limited view). This clinical picture is a direct indication for immediate surgical intervention.
- The presence of bloody nasogastric tube contents, diffuse tenderness with rebound and guarding, and a history of significant blunt trauma further support the need for urgent exploratory **laparotomy** to identify and repair the source of injury.
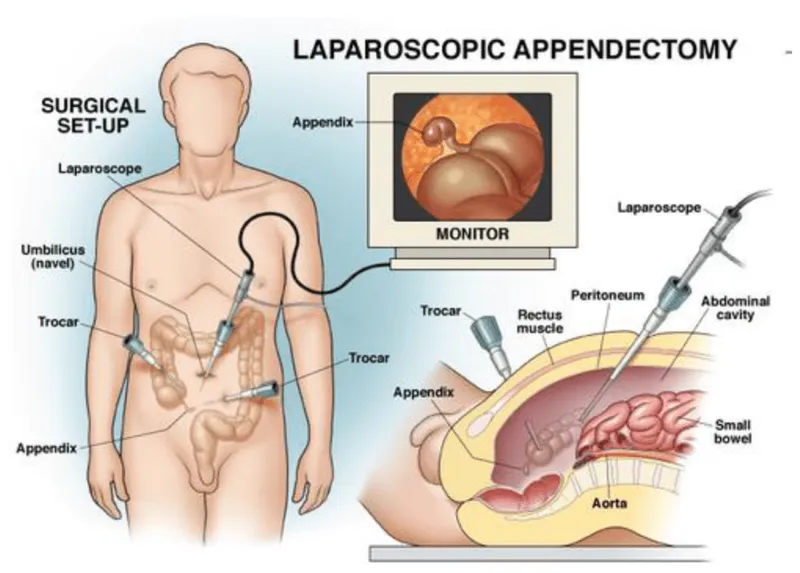
*Emergency laparoscopy*
- While laparoscopy can be used for abdominal exploration, it is **contraindicated in hemodynamically unstable patients** due to the need for pneumoperitoneum, which can further compromise cardiovascular stability.
- In cases of suspected visceral perforation with extensive free air and massive bleeding, **laparoscopy may be technically challenging** and less efficient than open laparotomy for rapid control of hemorrhage and contamination.
*Abdominal ultrasound*
- An abdominal ultrasound (**FAST exam**) has already been partially performed, revealing free fluid and raising suspicion of free air, making further ultrasound redundant.
- While useful for initial trauma assessment, an ultrasound **cannot definitively rule out all abdominal injuries**, especially hollow viscus perforations or retroperitoneal hematomas, and is insufficient for unstable patients with clear signs of peritonitis.
*Diagnostic peritoneal lavage (DPL)*
- **DPL is largely replaced by FAST and CT scans** in most trauma centers, especially given the availability of imaging.
- Although it can detect intraperitoneal bleeding or perforation, it is an **invasive procedure** with potential complications and would only confirm what is already strongly suspected clinically; it does not address the need for immediate therapeutic intervention in an unstable patient.
*CT scan*
- A CT scan would be the imaging modality of choice for a **hemodynamically stable** patient with blunt abdominal trauma.
- However, performing a CT scan on an **unstable patient** would unnecessarily delay definitive surgical management, which is critical given the signs of ongoing internal bleeding and likely perforation.
Laparoscopic surgery principles US Medical PG Question 5: A 27-year-old man presents to the emergency department after being stabbed. The patient was robbed at a local pizza parlor and was stabbed over 10 times with a large kitchen knife with an estimated 7 inch blade in the ventral abdomen. His temperature is 97.6°F (36.4°C), blood pressure is 74/54 mmHg, pulse is 180/min, respirations are 19/min, and oxygen saturation is 98% on room air. The patient is intubated and given blood products and vasopressors. Physical exam is notable for multiple stab wounds over the patient's abdomen inferior to the nipple line. Which of the following is the best next step in management?
- A. Exploratory laparotomy (Correct Answer)
- B. Diagnostic peritoneal lavage
- C. CT scan of the abdomen and pelvis
- D. Exploratory laparoscopy
- E. FAST exam
Laparoscopic surgery principles Explanation: ***Exploratory laparotomy***
- The patient presents with **multiple stab wounds** to the abdomen and signs of **hemorrhagic shock** (BP 74/54 mmHg, HR 180/min), which are clear indications for immediate surgical intervention.
- An exploratory laparotomy allows for direct visualization and repair of internal injuries, which is critical in this life-threatening situation.
*Diagnostic peritoneal lavage*
- While DPL can detect intra-abdominal bleeding, it is an **invasive procedure** and may delay definitive treatment in a hemodynamically unstable patient with obvious penetrating trauma.
- It is **less specific** than a laparotomy for identifying the exact location and nature of injuries, and it has largely been replaced by imaging studies or direct surgical exploration in unstable patients.
*CT scan of the abdomen and pelvis*
- A CT scan requires a **hemodynamically stable** patient and time for scanning and interpretation, which this patient does not have.
- Delaying definitive treatment for imaging in a patient with severe shock could lead to worse outcomes.
*Exploratory laparoscopy*
- Although less invasive, laparoscopy can be time-consuming and may not be feasible or safe in a patient with **profound hemorrhagic shock** and extensive injuries, especially if major vascular or visceral damage is suspected.
- Conversion to a **laparotomy** is often necessary in cases of significant injury, making immediate open exploration more efficient.
*FAST exam*
- A FAST exam can rapidly detect free fluid in the abdomen, suggesting internal bleeding, but it does **not provide specific information** about the source or extent of the injuries.
- While useful in the initial assessment, a positive FAST exam in a hemodynamically unstable patient with penetrating trauma directly points to the need for immediate surgical intervention, not further diagnostic delay.
Laparoscopic surgery principles US Medical PG Question 6: A 45-year-old man undergoes elective vasectomy for permanent contraception. The procedure is performed under local anesthesia. There are no intra-operative complications and he is discharged home with ibuprofen for post-operative pain. This patient is at increased risk for which of the following complications?
- A. Prostatitis
- B. Seminoma
- C. Testicular torsion
- D. Sperm granuloma (Correct Answer)
- E. Inguinal hernia
Laparoscopic surgery principles Explanation: **Sperm granuloma**
- A **sperm granuloma** can occur after vasectomy due to the extravasation of sperm from the severed vas deferens, leading to a foreign body granulomatous reaction.
- This complication presents as a **palpable, tender nodule** at the vasectomy site and is a relatively common long-term issue.
*Prostatitis*
- **Prostatitis** is an inflammation of the prostate gland, and there is no direct mechanistic link or increased risk following a vasectomy.
- It is typically caused by bacterial infection or non-infectious inflammatory processes, unrelated to the **vas deferens** ligation.
*Seminoma*
- **Seminoma** is a type of testicular germ cell tumor, and extensive research has shown no increased risk of developing testicular cancer after vasectomy.
- The procedure does not alter the cellular processes or environment within the testicles that predispose to germ cell tumor formation.
*Testicular torsion*
- **Testicular torsion** is a urological emergency involving the twisting of the spermatic cord, which cuts off blood supply to the testis.
- This condition is not associated with vasectomy; it typically occurs due to an anatomical abnormality (e.g., **bell-clapper deformity**) or trauma.
*Inguinal hernia*
- An **inguinal hernia** is a protrusion of abdominal contents through a weakness in the abdominal wall, specifically in the inguinal canal.
- Vasectomy is a superficial procedure that does not involve manipulating or weakening the abdominal wall in a way that would increase the risk of an inguinal hernia.
Laparoscopic surgery principles US Medical PG Question 7: A 63-year-old man is brought to the emergency department, 30 minutes after being involved in a high-speed motor vehicle collision. He is obtunded on arrival. He is intubated and mechanical ventilation is begun. The ventilator is set at a FiO2 of 60%, tidal volume of 440 mL, and positive end-expiratory pressure of 4 cm H2O. On the third day of intubation, his temperature is 37.3°C (99.1°F), pulse is 91/min, and blood pressure is 103/60 mm Hg. There are decreased breath sounds over the left lung base. Cardiac examination shows no abnormalities. The abdomen is soft and not distended. Arterial blood gas analysis shows:
pH 7.49
pCO2 29 mm Hg
pO2 73 mm Hg
HCO3- 20 mEq/L
O2 saturation 89%
Monitoring shows a sudden increase in the plateau airway pressure. An x-ray of the chest shows deepening of the costophrenic angle on the left side. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Administer levofloxacin
- C. Close observation
- D. Increase the PEEP
- E. Insertion of a chest tube (Correct Answer)
Laparoscopic surgery principles Explanation: ***Insertion of a chest tube***
- The sudden increase in **plateau airway pressure**, decreased breath sounds over the left lung base, worsening hypoxemia (O2 sat 89%) despite high FiO2, and **deepening of the costophrenic angle on the left side** indicate a **traumatic hemothorax**.
- Deepening of the costophrenic angle on chest X-ray is a classic sign of **pleural fluid accumulation** (hemothorax or pleural effusion), not pneumothorax.
- In a trauma patient (high-speed motor vehicle collision) on day 3 of mechanical ventilation, this represents a **delayed hemothorax** requiring immediate drainage.
- **Chest tube insertion** is the definitive management to evacuate blood, re-expand the lung, and improve ventilation and oxygenation.
*CT scan of the chest*
- While CT scan would provide detailed anatomical information, the clinical presentation with sudden respiratory decompensation and clear chest X-ray findings of hemothorax requires **immediate intervention**.
- Delaying treatment to obtain CT imaging in an unstable ventilated patient could worsen hypoxemia and lead to cardiovascular compromise.
- CT scan may be obtained later if needed to evaluate for ongoing bleeding or other injuries.
*Administer levofloxacin*
- Antibiotics would be appropriate for **pneumonia or empyema**, but the patient has no clear signs of infection (afebrile at 37.3°C, acute presentation over hours not days).
- The primary problem is **mechanical compression** from pleural fluid accumulation, not infection.
- Antibiotics do not address the life-threatening respiratory compromise from hemothorax.
*Close observation*
- Close observation is inappropriate given the acute deterioration with increased plateau pressures and worsening hypoxemia.
- The patient requires urgent intervention to prevent further respiratory failure and potential cardiovascular collapse.
- Expectant management would be negligent in this clinical scenario.
*Increase the PEEP*
- Increasing **Positive End-Expiratory Pressure (PEEP)** would worsen the situation by increasing intrathoracic pressure against an already compressed lung.
- Higher PEEP could impair venous return, decrease cardiac output, and potentially convert a simple hemothorax to a tension physiology.
- PEEP adjustments do not address the underlying problem of pleural space fluid accumulation requiring drainage.
Laparoscopic surgery principles US Medical PG Question 8: A 30-year-old male gang member is brought to the emergency room with a gunshot wound to the abdomen. The patient was intubated and taken for an exploratory laparotomy, which found peritoneal hemorrhage and injury to the small bowel. He required 5 units of blood during this procedure. Following the operation, the patient was sedated and remained on a ventilator in the surgical intensive care unit (SICU). The next day, a central line is placed and the patient is started on total parenteral nutrition. Which of the following complications is most likely in this patient?
- A. Mesenteric ischemia
- B. Hypocalcemia
- C. Refeeding syndrome
- D. Sepsis (Correct Answer)
- E. Cholelithiasis
Laparoscopic surgery principles Explanation: ***Sepsis***
- This patient has undergone **major abdominal surgery** after a **gunshot wound**, which carries a high risk of **peritoneal contamination** and subsequent infection.
- He also has several risk factors for sepsis, including **intubation**, central line placement, and possibly prolonged ventilation, all of which increase the risk of nosocomial infections and subsequent sepsis.
*Mesenteric ischemia*
- While possible in critically ill patients, there is no direct evidence such as advanced age, atherosclerosis, or specific signs of **bowel ischemia** (e.g., severe abdominal pain disproportionate to exam, bloody diarrhea) presenting in this case.
- The initial injury was to the small bowel, but the current context points more to systemic complications rather than a focal vascular event.
*Hypocalcemia*
- Hypocalcemia can occur in critically ill patients due to various reasons, but it is not the *most likely* complication given the patient's presentation primarily focused on surgical trauma and subsequent interventions.
- Dilutional effects from massive transfusions or **citrate toxicity** could contribute to temporary hypocalcemia, but sepsis poses a more immediate and widespread threat.
*Refeeding syndrome*
- Refeeding syndrome occurs when severely malnourished patients are rapidly refed, leading to shifts in **electrolytes** (especially **phosphate**, potassium, magnesium).
- Although the patient is starting **total parenteral nutrition (TPN)**, there's no indication of prior severe malnutrition, making sepsis a more prominent immediate concern due to the gunshot wound and surgery.
*Cholelithiasis*
- **Cholelithiasis** (gallstones) can be a long-term complication of total parenteral nutrition (TPN) due to gallbladder stasis.
- However, it is unlikely to develop so acutely within a day of starting TPN and is thus not the most immediate or likely complication for this patient's acute critical state.
Laparoscopic surgery principles US Medical PG Question 9: A 25-year-old man presents with pain and a limited range of motion in his right shoulder. He is a collegiate baseball player and says he has not been playing for approx. 1 week because his shoulder hurts when he throws. He also noticed trouble raising his arm over his head. He describes the pain as moderate, dull, and aching in character and worse when he moves his arm above his shoulder or when he lays in bed on his side. He denies any recent acute trauma to the shoulder or other joint pain. The medical history is significant for asthma, which is managed medically. The current medications include albuterol inhaled and fluticasone. He reports a 5-year history of chewing tobacco but denies smoking, alcohol, or drug use. The temperature is 37.0°C (98.6°F); blood pressure is 110/85 mm Hg; pulse is 97/min; respiratory rate is 15/min, and oxygen saturation is 99% on room air. The physical examination is significant for tenderness to palpation on the anterolateral aspect of the right shoulder. The active range of motion on abduction of the right shoulder is decreased. The passive range of motion is intact. No swelling, warmth, or erythema is noted. The sensation is intact. The deep tendon reflexes are 2+ bilaterally. The peripheral pulses are 2+. The laboratory results are all within normal limits. A plain radiograph of the right shoulder shows no evidence of fracture or bone deformities. An MRI of the right shoulder shows increased T1 and T2 signals in the rotator cuff tendon. Which of the following is the best initial course of treatment for this patient?
- A. No further treatment is needed
- B. Acromioplasty
- C. Intra-articular corticosteroid injection
- D. NSAIDs and conservative measures (Correct Answer)
- E. Conservative measures (rest and ice)
Laparoscopic surgery principles Explanation: ***NSAIDs and conservative measures***
- The patient presents with symptoms and MRI findings consistent with **rotator cuff tendinitis**, common in overhead athletes. Initial treatment should focus on **reducing inflammation** and pain, and promoting healing.
- **NSAIDs** combined with conservative measures like **rest from inciting activities** and **ice application** are the mainstay of initial treatment for tendinitis, aiming to alleviate pain and improve function.
*No further treatment is needed*
- This option is incorrect because the patient is experiencing significant pain, limitation in his sport, and MRI findings of **tendinitis**, which warrants intervention.
- Doing nothing would likely lead to worsening symptoms and potentially chronic issues, especially given his athletic demands.
*Acromioplasty*
- **Acromioplasty** is a surgical procedure typically reserved for cases of **subacromial impingement syndrome** that have failed extensive conservative management, or for larger, more symptomatic tears.
- The patient's presentation suggests **tendinitis** without clear evidence of chronic impingement or a full-thickness tear requiring immediate surgical intervention.
*Intra-articular corticosteroid injection*
- **Corticosteroid injections** can provide temporary pain relief but are generally reserved for cases that have failed conservative therapy with oral NSAIDs and physical therapy.
- They also carry risks like **tendon weakening** and potential for rupture, which is particularly concerning in an athlete with tendinitis.
*Conservative measures (rest and ice)*
- While **rest and ice** are crucial components of conservative management, this option is incomplete as it omits the important role of **NSAIDs** in managing the inflammatory component of tendinitis.
- Simply resting and icing might not be sufficient for adequate pain control and inflammation reduction in an active individual with this degree of symptoms.
Laparoscopic surgery principles US Medical PG Question 10: A 65-year-old man comes to the physician for evaluation of severe pain in his left shoulder for several days. He did not fall or injure his shoulder. He has a history of osteoarthritis of both knees that is well-controlled with indomethacin. He spends most of his time at a retirement facility and does not do any sports. There is no family history of serious illness. He has smoked one pack of cigarettes daily for 35 years. Vital signs are within normal limits. Physical examination shows tenderness of the greater tuberosity of the left humerus. There is no swelling or erythema. The patient is unable to slowly adduct his arm after it is passively abducted to 90 degrees. External rotation is limited by pain. Subacromial injection of lidocaine does not relieve his symptoms. An x-ray of the left shoulder shows sclerosis of the acromion and humeral head. Which of the following is the most appropriate next step in management?
- A. CT scan of the shoulder
- B. Reassurance
- C. Surgical fixation
- D. Biopsy of the humerus
- E. Musculoskeletal ultrasound (Correct Answer)
Laparoscopic surgery principles Explanation: ***Musculoskeletal ultrasound***
- The patient's symptoms (pain, inability to adduct arm after passive abduction to 90° - **positive drop arm sign**, limited external rotation, tenderness of the **greater tuberosity**) are highly suggestive of a **rotator cuff tear**.
- **Ultrasound** is a validated imaging modality for assessing soft tissue structures like tendons and can readily identify rotator cuff tears with high sensitivity and specificity.
- While **MRI is considered the gold standard** for rotator cuff evaluation, ultrasound is a reasonable initial imaging choice when available, especially given the failed diagnostic lidocaine injection pointing to structural pathology.
- Ultrasound can demonstrate the presence, size, and location of rotator cuff tears and guide further management decisions.
*CT scan of the shoulder*
- A **CT scan** is primarily used for evaluating **bony structures** and complex fractures, which are not the primary concern here given the symptoms pointing to soft tissue injury.
- While it can indirectly show rotator cuff pathology through secondary signs, it is **less sensitive** than ultrasound or MRI for direct visualization of tendon tears.
- The x-ray findings (sclerosis) already provide adequate bony detail for this clinical scenario.
*Reassurance*
- Given the severe, persistent pain, functional deficit (inability to adduct - **positive drop arm sign**), and specific physical exam findings, **reassurance alone** is inappropriate and would delay necessary diagnosis and intervention.
- The patient clearly has a significant underlying shoulder pathology requiring further investigation and likely treatment.
*Surgical fixation*
- **Surgical fixation** is a treatment, not a diagnostic step. It would only be considered after a definitive diagnosis, such as a severe rotator cuff tear, has been made with imaging confirmation.
- The immediate next step should be diagnostic imaging to confirm the nature, extent, and characteristics of the suspected injury.
*Biopsy of the humerus*
- A **biopsy of the humerus** would be indicated if there was suspicion of a bony tumor or infection, which is not suggested by the patient's presentation.
- The x-ray findings (sclerosis of acromion and humeral head) are consistent with chronic degenerative changes or impingement syndrome, not neoplastic or infectious processes.
- The clinical picture clearly points to a **soft tissue injury** rather than primary bone pathology requiring biopsy.
More Laparoscopic surgery principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.