Endoscopic procedures overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Endoscopic procedures overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Endoscopic procedures overview US Medical PG Question 1: A 62-year-old man comes to the office complaining of dysphagia that started 4-5 months ago. He reports that he initially had difficulty swallowing only solid foods. More recently, he has noticed some trouble swallowing liquids. The patient also complains of fatigue, a chronic cough that worsens at night, and burning chest pain that occurs after he eats. He says that he has used over-the-counter antacids for "years" with mild relief. He denies any change in diet, but says he has "gone down a pant size or 2." The patient has hypertension and hyperlipidemia. He takes amlodipine and atorvastatin. He smoked 1 pack of cigarettes a day for 12 years while in the military but quit 35 years ago. He drinks 1-2 beers on the weekend while he is golfing with his friends. His diet consists mostly of pasta, pizza, and steak. The patient's temperature is 98°F (36.7°C), blood pressure is 143/91 mmHg, and pulse is 80/min. His BMI is 32 kg/m^2. Physical examination reveals an obese man in no acute distress. No masses or enlarged lymph nodes are appreciated upon palpation of the neck. Cardiopulmonary examination is unremarkable. An endoscopy is performed, which identifies a lower esophageal mass. Which of the following is the most likely diagnosis?
- A. Nutcracker esophagus
- B. Plummer-Vinson syndrome
- C. Small cell carcinoma
- D. Adenocarcinoma (Correct Answer)
- E. Squamous cell carcinoma
Endoscopic procedures overview Explanation: ***Adenocarcinoma***
- The patient's history of **dysphagia progressing from solids to liquids**, **weight loss**, and **long-standing GERD symptoms** (chronic cough, burning chest pain, use of antacids for years) are highly suggestive of **esophageal adenocarcinoma**, especially given the endoscopic finding of a **lower esophageal mass**.
- **Risk factors** present include **obesity** (BMI 32 kg/m²), **chronic GERD**, and a remote history of smoking, which contribute to the development of **Barrett's esophagus**, a precursor to adenocarcinoma.
- Adenocarcinoma typically arises in the **distal/lower esophagus** due to chronic acid reflux.
*Nutcracker esophagus*
- Characterized by **high-amplitude peristaltic contractions** of the esophagus, primarily causing **chest pain** and **dysphagia**.
- It is a **motility disorder**, not a structural lesion, and does not present with **progressive dysphagia from solids to liquids**, **weight loss**, or an **esophageal mass** on endoscopy.
*Plummer-Vinson syndrome*
- A rare condition characterized by the triad of **iron deficiency anemia**, **dysphagia**, and **esophageal webs** (typically in the upper esophagus).
- While it causes dysphagia, it does not present with an **esophageal mass**, **weight loss**, or a history of long-standing GERD.
- More common in middle-aged women and associated with increased risk of squamous cell carcinoma.
*Small cell carcinoma*
- **Small cell carcinoma** is primarily a type of **lung cancer**, although it can rarely occur in the esophagus.
- Esophageal small cell carcinoma is **very aggressive** and usually presents with symptoms similar to other esophageal cancers but is **much less common** than adenocarcinoma or squamous cell carcinoma in the esophagus.
*Squamous cell carcinoma*
- **Squamous cell carcinoma** of the esophagus is strongly associated with **smoking** and **alcohol use**, and typically arises in the **upper or middle esophagus**.
- While the patient has a remote smoking history, his **long-standing GERD**, **obesity**, and **lower esophageal mass** location make **adenocarcinoma** the more probable diagnosis, as adenocarcinoma arises from **Barrett's esophagus** in the distal esophagus due to chronic reflux.
Endoscopic procedures overview US Medical PG Question 2: A 4-year-old boy presents to the emergency department after his parents found him drinking blue liquid out of an unlabeled bottle in the garage. They have no idea what was in the bottle and are concerned for his health. They have brought the bottle with them to the emergency department. The child's past medical history is not remarkable, and he is currently not taking any medications. The patient's vitals are within normal limits for his age. Physical exam reveals a crying child who is drooling. A radiograph is performed, and the child's vitals are closely monitored. It is determined that the blue liquid is a strong alkali. Which of the following is the best next step in management?
- A. Administration of a diluent
- B. Gastrografin swallow and endoscopy (Correct Answer)
- C. Administration of a weak acid
- D. Charcoal
- E. Ipecac
Endoscopic procedures overview Explanation: ***Gastrografin swallow and endoscopy***
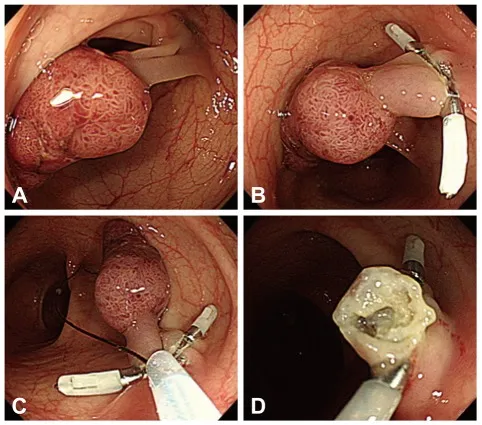
- **Endoscopy within 12-24 hours** is the gold standard for evaluating caustic ingestions, allowing direct visualization of mucosal injury and grading of severity to guide management.
- A **Gastrografin swallow** (water-soluble contrast study) may be considered if esophageal perforation is suspected, though it is not routinely performed in all cases; CT imaging is often preferred for perforation assessment.
- The key intervention is **endoscopy**, which should not be delayed beyond 24 hours to avoid missing the optimal window for assessment before granulation tissue forms.
*Administration of a diluent*
- Administering a diluent is **contraindicated** when there are signs of esophageal injury such as drooling, as it can worsen inflammation, induce vomiting, or lead to perforation.
- Dilution may also cause vomiting which re-exposes the esophagus to the caustic substance, causing additional injury.
*Administration of a weak acid*
- Neutralizing a strong alkali with a weak acid is **not recommended** due to the exothermic reaction this causes, generating heat and worsening tissue damage.
- The precise amount of acid needed for safe neutralization cannot be reliably determined, making this approach dangerous.
*Charcoal*
- **Activated charcoal** does not bind to strong alkalis or acids and is therefore not indicated for caustic ingestions.
- It may also impede endoscopic visualization, delaying definitive diagnosis and management.
*Ipecac*
- **Syrup of ipecac** induces vomiting and is **contraindicated** in caustic ingestions because it causes re-exposure of the esophagus to the corrosive substance, increasing mucosal damage.
- Vomiting also carries significant risk of aspiration into the lungs, which can cause severe respiratory complications.
Endoscopic procedures overview US Medical PG Question 3: A 28-year-old graduate student visits the university health clinic for 3-weeks of epigastric pain that worsens with meals, associated with retrosternal pain, early satiety, and bloating. She denies vomiting blood or blood in her stool. She has been consuming large volumes of caffeinated-drinks and fast-food for a month, as she has been studying for her tests. Her family and personal history are unremarkable with no history of gastrointestinal cancer. Her vital signs are within normal limits. Physical examination is only positive for a mild epigastric tenderness. Which of the following is the most appropriate approach in this case?
- A. Treatment with metoclopramide
- B. Upper endoscopy
- C. Fecal antigen testing for Helicobacter pylori (Correct Answer)
- D. Treatment with omeprazole
- E. Barium swallow radiograph
Endoscopic procedures overview Explanation: ***Fecal antigen testing for Helicobacter pylori***
- The patient presents with **dyspeptic symptoms** (epigastric pain, early satiety, bloating) and no **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia).
- Given her age (< 60 years) and lack of alarm symptoms, a "test-and-treat" strategy for **Helicobacter pylori** is recommended, with fecal antigen testing being a non-invasive and accurate option.
*Treatment with metoclopramide*
- Metoclopramide is a **prokinetic agent** used for conditions like gastroparesis, not primarily for initial management of undiagnosed dyspepsia.
- While she has early satiety, the primary approach should be to rule out common causes of dyspepsia like **H. pylori** before considering symptomatic treatments for motility issues.
*Upper endoscopy*
- An **upper endoscopy** is indicated if the patient is older (typically > 60 years) or has **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia, persistent vomiting).
- This 28-year-old patient lacks any alarm symptoms and is below the age threshold for an immediate endoscopic evaluation for dyspepsia.
*Treatment with omeprazole*
- While a **proton pump inhibitor (PPI)** like omeprazole can treat dyspeptic symptoms, it is not the most appropriate *initial* approach without first testing for **H. pylori**.
- Empiric PPI therapy can **mask H. pylori infection**, potentially delaying appropriate eradication therapy if the test-and-treat strategy is not followed.
*Barium swallow radiograph*
- A **barium swallow** is primarily used to evaluate structural abnormalities of the **esophagus**, such as strictures, diverticula, or achalasia, and is less effective for diagnosing mucosal diseases of the stomach or duodenum.
- It is not the preferred diagnostic test for evaluating dyspepsia or identifying **H. pylori** infection.
Endoscopic procedures overview US Medical PG Question 4: A 66-year-old man was referred for endoscopic evaluation due to iron deficiency anemia. He has had anorexia and weight loss for two months. Three years ago, the patient had coronary artery bypass grafting and aortic mechanical valve replacement. He has a 12-year history of diabetes mellitus and hypertension. He takes warfarin, lisinopril, amlodipine, metformin, aspirin, and carvedilol. His blood pressure is 115/65 mm Hg, pulse is 68/min, respirations are 14/min, temperature is 36.8°C (98.2°F), and blood glucose is 220 mg/dL. Conjunctivae are pale. Heart examination reveals a metallic click just before the carotid pulse. Which of the following is the most appropriate switch in this patient’s drug therapy before the endoscopy?
- A. Metformin to empagliflozin
- B. Aspirin to clopidogrel
- C. Lisinopril to losartan
- D. Warfarin to heparin (Correct Answer)
- E. Amlodipine to diltiazem
Endoscopic procedures overview Explanation: ***Warfarin to heparin***
- The patient is on **warfarin** due to his **mechanical aortic valve**, which increases his risk of bleeding during endoscopy.
- Switching to **heparin (bridging therapy)** allows for a shorter half-life and easier reversal if bleeding occurs, making it safer for the procedure.
*Metformin to empagliflozin*
- This change in **antidiabetic medication** does not address the immediate concern of bleeding risk for endoscopy.
- **Empagliflozin** can cause **euglycemic diabetic ketoacidosis** and its benefits related to cardiovascular outcomes are long term, not relevant to peri-procedural management.
*Aspirin to clopidogrel*
- Both **aspirin** and **clopidogrel** are **antiplatelet agents** that increase bleeding risk.
- Switching from one to the other does not mitigate the bleeding risk for endoscopy; often, one or both are held before such procedures if possible.
*Lisinopril to losartan*
- Both **lisinopril** and **losartan** are **antihypertensive medications** (ACE inhibitor and ARB, respectively) with similar effects on blood pressure.
- This change would not impact the **bleeding risk** or the need for peri-procedural anticoagulation management.
*Amlodipine to diltiazem*
- Both **amlodipine** and **diltiazem** are **calcium channel blockers** used for hypertension and angina.
- While they have different mechanisms, switching between them does not address the immediate safety concern of **bleeding risk** during endoscopy.
Endoscopic procedures overview US Medical PG Question 5: A 45-year-old man undergoes elective vasectomy for permanent contraception. The procedure is performed under local anesthesia. There are no intra-operative complications and he is discharged home with ibuprofen for post-operative pain. This patient is at increased risk for which of the following complications?
- A. Prostatitis
- B. Seminoma
- C. Testicular torsion
- D. Sperm granuloma (Correct Answer)
- E. Inguinal hernia
Endoscopic procedures overview Explanation: **Sperm granuloma**
- A **sperm granuloma** can occur after vasectomy due to the extravasation of sperm from the severed vas deferens, leading to a foreign body granulomatous reaction.
- This complication presents as a **palpable, tender nodule** at the vasectomy site and is a relatively common long-term issue.
*Prostatitis*
- **Prostatitis** is an inflammation of the prostate gland, and there is no direct mechanistic link or increased risk following a vasectomy.
- It is typically caused by bacterial infection or non-infectious inflammatory processes, unrelated to the **vas deferens** ligation.
*Seminoma*
- **Seminoma** is a type of testicular germ cell tumor, and extensive research has shown no increased risk of developing testicular cancer after vasectomy.
- The procedure does not alter the cellular processes or environment within the testicles that predispose to germ cell tumor formation.
*Testicular torsion*
- **Testicular torsion** is a urological emergency involving the twisting of the spermatic cord, which cuts off blood supply to the testis.
- This condition is not associated with vasectomy; it typically occurs due to an anatomical abnormality (e.g., **bell-clapper deformity**) or trauma.
*Inguinal hernia*
- An **inguinal hernia** is a protrusion of abdominal contents through a weakness in the abdominal wall, specifically in the inguinal canal.
- Vasectomy is a superficial procedure that does not involve manipulating or weakening the abdominal wall in a way that would increase the risk of an inguinal hernia.
Endoscopic procedures overview US Medical PG Question 6: A 55-year-old man presents to his primary care physician for trouble swallowing. The patient claims that he used to struggle when eating food if he did not chew it thoroughly, but now he occasionally struggles with liquids as well. He also complains of a retrosternal burning sensation whenever he eats. He also claims that he feels his throat burns when he lays down or goes to bed. Otherwise, the patient has no other complaints. The patient has a past medical history of obesity, diabetes, constipation, and anxiety. His current medications include insulin, metformin, and lisinopril. On review of systems, the patient endorses a 5 pound weight loss recently. The patient has a 22 pack-year smoking history and drinks alcohol with dinner. His temperature is 99.5°F (37.5°C), blood pressure is 177/98 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note an overweight man in no current distress. Abdominal exam is within normal limits. Which of the following is the best next step in management?
- A. Endoscopy (Correct Answer)
- B. Omeprazole trial
- C. Manometry
- D. Barium swallow
- E. CT scan
Endoscopic procedures overview Explanation: ***Endoscopy***
- The patient presents with **dysphagia to solids and liquids**, significant for **recent weight loss**, and a **history of smoking**, all of which are **alarm symptoms** necessitating an upper endoscopy to rule out malignancy.
- While he has **GERD symptoms** as well (retrosternal burning), the presence of alarm features mandates a direct investigation of the upper GI tract rather than empirical treatment.
*Omeprazole trial*
- An empirical trial of **PPIs** like omeprazole is appropriate for classic GERD symptoms without alarm features.
- However, **dysphagia to solids and liquids with associated weight loss**, especially in a patient with a significant **smoking history**, are alarm symptoms that require direct visualization via endoscopy, not just symptom management.
*Manometry*
- **Esophageal manometry** is used to evaluate the motility of the esophagus and diagnose conditions like achalasia or esophageal spasm.
- While the patient has dysphagia, **alarm symptoms (weight loss, smoking history)** raise concern for mechanical obstruction or malignancy, which should be investigated before motility disorders.
*Barium swallow*
- A **barium swallow** can identify structural abnormalities like strictures, masses, or webs, and also assess motility.
- However, in the context of alarm symptoms, a **barium swallow is less sensitive** for detecting subtle mucosal changes or early malignancy compared to endoscopy, and any positive findings would still prompt an endoscopy.
*CT scan*
- A **CT scan of the chest and abdomen** is useful for assessing extraluminal pathology, mediastinal involvement, or distant metastases.
- While it may eventually be part of staging if a malignancy is found, the **initial investigation for esophageal symptoms and alarm features** focuses on direct luminal visualization with endoscopy to identify the primary pathology.
Endoscopic procedures overview US Medical PG Question 7: A 65-year-old African-American man presents to your office with dysphagia. He reports that he has found it progressively more difficult to swallow food over the past year. At the time of presentation, he is able to eat only soup. Social history is significant for asbestos exposure, multiple daily drinks of hard alcohol, and a 70 pack-year smoking history. What would you most expect to see on an esophageal biopsy of this patient?
- A. Esophageal varices
- B. Ferruginous bodies
- C. Keratin nests and pearls (Correct Answer)
- D. Glandular metaplasia
- E. Mucosal abrasions
Endoscopic procedures overview Explanation: ***Keratin nests and pearls***
- This patient's significant **smoking history** and **alcohol consumption** are major risk factors for **esophageal squamous cell carcinoma**, which is characterized microscopically by **keratin nests and pearls** on biopsy.
- The progressive **dysphagia** (difficulty swallowing) over a year, especially progressing to difficulty with solids, is a classic symptom of **esophageal cancer**.
*Esophageal varices*
- Esophageal varices are typically caused by **portal hypertension**, most commonly due to cirrhosis from chronic alcohol abuse.
- While alcohol abuse is present, varices would present with **hematemesis** or melena due to rupture, not progressive dysphagia as the primary symptom.
*Ferruginous bodies*
- These are indicative of **asbestos exposure** in the lungs, typically seen in conditions like asbestosis or mesothelioma.
- They are found in the **lungs**, not in the esophagus, although asbestos exposure is noted in the history.
*Glandular metaplasia*
- **Glandular metaplasia** of the esophagus, also known as **Barrett's esophagus**, is a precursor to **esophageal adenocarcinoma**.
- This typically results from chronic **gastroesophageal reflux disease (GERD)** symptoms, which are not mentioned in this patient.
*Mucosal abrasions*
- Mucosal abrasions would suggest trauma or inflammation but would not explain the **progressive, obstructive dysphagia** over a year.
- Abrasions are generally acute findings and not consistent with the underlying pathology suggested by this patient's long history and risk factors.
Endoscopic procedures overview US Medical PG Question 8: A 56-year-old man is brought to the emergency department after 4 hours of severe abdominal pain with an increase in its intensity over the last hour. His personal history is relevant for peptic ulcer disease and H. pylori infection that is being treated with clarithromycin triple therapy. Upon admission his vital signs are as follows: pulse of 120/min, a respiratory rate of 20/min, body temperature of 39°C (102.2°F), and blood pressure of 90/50 mm Hg. Physical examination reveals significant tenderness over the abdomen. A chest radiograph taken when the patient was standing erect is shown. Which of the following is the next best step in the management of this patient?
- A. Abdominal ultrasound
- B. Emergency abdominal surgery (Correct Answer)
- C. Abdominal computed tomography
- D. Nasogastric tube placement followed by gastric lavage
- E. Emergency endoscopy
Endoscopic procedures overview Explanation: ***Emergency abdominal surgery***
- The chest radiograph shows **free air under the diaphragm** (pneumoperitoneum), confirming a visceral perforation. The patient's severe abdominal pain, fever, tachycardia, and hypotension indicate **septic shock** secondary to peritonitis, necessitating immediate surgical intervention.
- Delaying surgery for further diagnostic tests (like CT or ultrasound) or less invasive procedures would be detrimental given the patient's **hemodynamic instability** and clear evidence of perforation.
*Abdominal ultrasound*
- While an ultrasound could detect fluid collections or sometimes free air, it is **less sensitive** than an upright chest radiograph for detecting pneumoperitoneum and cannot provide the same level of detail as CT for localizing a perforation.
- In a hemodynamically unstable patient with clear signs of peritonitis and pneumoperitoneum, performing an ultrasound would **delay definitive treatment**.
*Abdominal computed tomography*
- An abdominal CT scan is excellent for detecting subtle perforations, localizing them, and assessing associated complications. However, in this patient, the **upright chest radiograph already clearly shows pneumoperitoneum**, and the patient is **hemodynamically unstable**.
- Transporting an unstable patient to CT and waiting for the scan results would **waste critical time** and increase morbidity and mortality in the setting of ongoing septic shock.
*Nasogastric tube placement followed by gastric lavage*
- **Nasogastric tube placement** is appropriate for gastric decompression in cases of suspected obstruction or ileus, but it does not address a perforation. **Gastric lavage** is indicated for specific intoxications or gastrointestinal bleeding, neither of which is the primary concern here.
- This procedure would **not treat the underlying perforation** or the resulting peritonitis and septic shock.
*Emergency endoscopy*
- While an endoscopy can diagnose and sometimes treat upper gastrointestinal perforations (especially iatrogenic ones), it is typically **contraindicated in cases of suspected free perforation** due to the risk of exacerbating the pneumoperitoneum and further contamination.
- In an unstable patient with clear pneumoperitoneum and peritonitis, **surgery is the definitive treatment**, not endoscopy.
Endoscopic procedures overview US Medical PG Question 9: A 55-year-old man comes to the physician because of heartburn for the past 2 years. He has no chest pain, dysphagia, weight loss, or fever. He has no history of any serious illnesses. He takes omeprazole daily. Vital signs are within normal limits. Body mass index (BMI) is 34 kg/m2. Physical exam shows no abnormalities. An endoscopic image of the lower esophageal sphincter is shown. Which of the following is the most important next step in management?
- A. Endoscopic mucosal ablation therapy
- B. Esophagectomy
- C. High-dose pantoprazole
- D. Multiple endoscopic biopsies (Correct Answer)
- E. Laparoscopic Nissen fundoplication
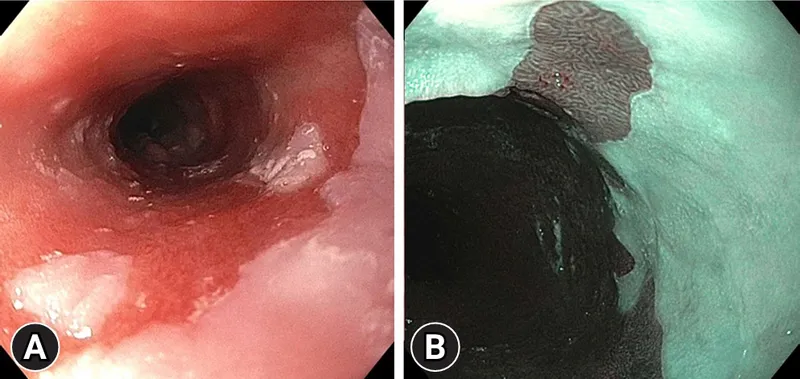
Endoscopic procedures overview Explanation: ***Multiple endoscopic biopsies***
- The endoscopic image likely shows **Barrett's esophagus**, characterized by metaplastic columnar epithelium. This condition is a precursor to **esophageal adenocarcinoma**.
- **Biopsies** are crucial to assess for the presence and grade of **dysplasia**, which dictates further management strategies.
*Endoscopic mucosal ablation therapy*
- This therapy is typically reserved for patients with **high-grade dysplasia** or **intramucosal carcinoma** in Barrett's esophagus, after diagnosis has been confirmed by biopsy.
- It would be premature to consider ablation without a definitive histological diagnosis of dysplasia.
*Esophagectomy*
- **Esophagectomy** is a major surgical procedure reserved for advanced esophageal cancer or high-grade dysplasia refractory to endoscopic therapies.
- It is an overly aggressive and inappropriate initial step without histological confirmation and assessment of dysplasia or cancer.
*High-dose pantoprazole*
- While proton pump inhibitors (PPIs) like pantoprazole are used to manage GERD symptoms and may help prevent progression of Barrett's esophagus, this patient is already on omeprazole daily.
- Simply increasing the dose of PPI does not address the need for **histological evaluation** of the abnormal-appearing mucosa for dysplasia or cancer.
*Laparoscopic Nissen fundoplication*
- This surgical procedure aims to strengthen the lower esophageal sphincter to treat severe GERD when medical management fails.
- While it addresses reflux, it does not directly evaluate or treat the potential **precancerous changes** in the esophageal lining seen on endoscopy, making biopsies a more immediate and critical next step.
Endoscopic procedures overview US Medical PG Question 10: A 50-year-old male presents to the emergency with abdominal pain. He reports he has had abdominal pain associated with meals for several months and has been taking over the counter antacids as needed, but experienced significant worsening pain one hour ago in the epigastric region. The patient reports the pain radiating to his shoulders. Vital signs are T 38, HR 120, BP 100/60, RR 18, SpO2 98%. Physical exam reveals diffuse abdominal rigidity with rebound tenderness. Auscultation reveals hypoactive bowel sounds. Which of the following is the next best step in management?
- A. Admission and observation
- B. Chest radiograph
- C. 12 lead electrocardiogram
- D. Abdominal CT scan (Correct Answer)
- E. Abdominal ultrasound
Endoscopic procedures overview Explanation: ***Abdominal CT scan***
- This patient presents with classic signs of a **perforated peptic ulcer**: sudden severe epigastric pain radiating to the shoulders (diaphragmatic irritation), fever, tachycardia, hypotension, and peritoneal signs (rigid abdomen with rebound tenderness).
- While the patient shows signs of **early shock** (BP 100/60, HR 120), he is **conscious and maintaining adequate oxygenation** (SpO2 98%), making him stable enough for rapid CT imaging.
- **Abdominal CT scan** is the **most sensitive and specific** test for detecting free air, identifying the location of perforation, and assessing for complications (abscess, contained perforation).
- CT provides **critical surgical planning information** about the extent and location of perforation, which can guide the surgical approach.
- This should be followed by **immediate surgical consultation** and preparation for emergency laparotomy.
*Chest radiograph*
- While an **upright chest X-ray** can detect free air under the diaphragm (pneumoperitoneum), it has **lower sensitivity** (70-80%) compared to CT scan (>95%).
- In a patient who is stable enough for imaging, **CT is preferred** as it provides more information for surgical planning.
- Chest X-ray would be the appropriate choice only if **CT is unavailable** or if the patient is **too unstable** to be transported to the CT scanner.
*Admission and observation*
- This patient has **acute peritonitis** from a likely perforated viscus, which is a **surgical emergency** requiring operative intervention.
- Observation would be inappropriate and dangerous, leading to **septic shock**, **multi-organ failure**, and death.
*12 lead electrocardiogram*
- While epigastric pain can sometimes be cardiac in origin, the **peritoneal signs** (rigid abdomen, rebound tenderness, hypoactive bowel sounds) clearly indicate an **intra-abdominal pathology**.
- The pain radiation to **both shoulders** (Kehr's sign) suggests diaphragmatic irritation from intraperitoneal air or fluid, not cardiac ischemia.
*Abdominal ultrasound*
- Ultrasound is useful for evaluating **solid organ injury**, **free fluid**, and conditions like **cholecystitis** or **appendicitis**.
- However, it is **poor at detecting free air** due to bowel gas artifact and has limited sensitivity for perforated viscus.
- It would not provide adequate information for this surgical emergency.
More Endoscopic procedures overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.