CO2 insufflation physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for CO2 insufflation physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
CO2 insufflation physiology US Medical PG Question 1: A 41-year-old man is admitted to the emergency room after being struck in the abdomen by a large cement plate while transporting it. On initial assessment by paramedics at the scene, his blood pressure was 110/80 mm Hg, heart rate 85/min, with no signs of respiratory distress. On admission, the patient is alert but in distress. He complains of severe, diffuse, abdominal pain and severe weakness. Vital signs are now: blood pressure 90/50 mm Hg, heart rate 96/min, respiratory rate 19/min, temperature 37.4℃ (99.3℉), and oxygen saturation of 95% on room air. His lungs are clear on auscultation. The cardiac exam is significant for a narrow pulse pressure. Abdominal examination reveals a large bruise over the epigastric and periumbilical regions. The abdomen is distended and there is diffuse tenderness to palpation with rebound and guarding, worst in the epigastric region. There is hyperresonance to percussion in the epigastric region and absence of hepatic dullness in the right upper quadrant. Aspiration of the nasogastric tube reveals bloody contents. Focused assessment with sonography for trauma (FAST) shows free fluid in the pelvic region. Evaluation of the perisplenic and perihepatic regions is impossible due to the presence of free air. Aggressive intravenous fluid resuscitation is administered but fails to improve upon the patient’s hemodynamics. Which of the following is the next best step in management?
- A. Emergency laparoscopy
- B. Abdominal ultrasound
- C. Diagnostic peritoneal lavage (DPL)
- D. Emergency laparotomy (Correct Answer)
- E. CT scan
CO2 insufflation physiology Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** unresponsive to fluid resuscitation, coupled with clear signs of **perforation** (hyperresonance, absent hepatic dullness, free air on FAST limited view). This clinical picture is a direct indication for immediate surgical intervention.
- The presence of bloody nasogastric tube contents, diffuse tenderness with rebound and guarding, and a history of significant blunt trauma further support the need for urgent exploratory **laparotomy** to identify and repair the source of injury.
*Emergency laparoscopy*
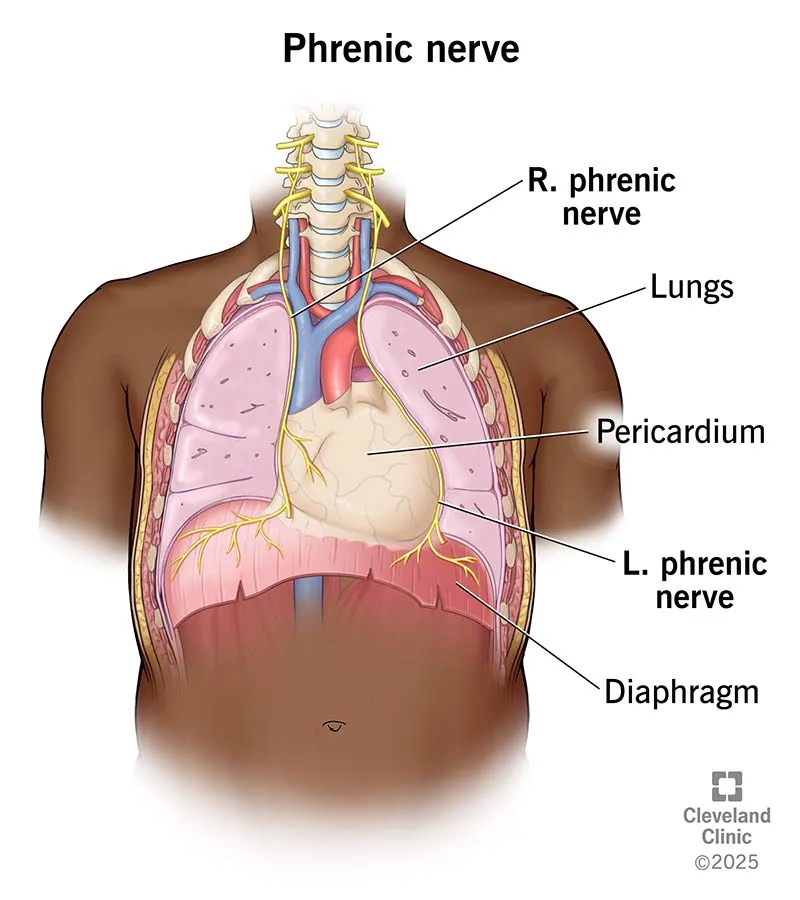
- While laparoscopy can be used for abdominal exploration, it is **contraindicated in hemodynamically unstable patients** due to the need for pneumoperitoneum, which can further compromise cardiovascular stability.
- In cases of suspected visceral perforation with extensive free air and massive bleeding, **laparoscopy may be technically challenging** and less efficient than open laparotomy for rapid control of hemorrhage and contamination.
*Abdominal ultrasound*
- An abdominal ultrasound (**FAST exam**) has already been partially performed, revealing free fluid and raising suspicion of free air, making further ultrasound redundant.
- While useful for initial trauma assessment, an ultrasound **cannot definitively rule out all abdominal injuries**, especially hollow viscus perforations or retroperitoneal hematomas, and is insufficient for unstable patients with clear signs of peritonitis.
*Diagnostic peritoneal lavage (DPL)*
- **DPL is largely replaced by FAST and CT scans** in most trauma centers, especially given the availability of imaging.
- Although it can detect intraperitoneal bleeding or perforation, it is an **invasive procedure** with potential complications and would only confirm what is already strongly suspected clinically; it does not address the need for immediate therapeutic intervention in an unstable patient.
*CT scan*
- A CT scan would be the imaging modality of choice for a **hemodynamically stable** patient with blunt abdominal trauma.
- However, performing a CT scan on an **unstable patient** would unnecessarily delay definitive surgical management, which is critical given the signs of ongoing internal bleeding and likely perforation.
CO2 insufflation physiology US Medical PG Question 2: A 34-year-old woman is recovering in the post-operative unit following a laparoscopic procedure for chronic endometriosis. She had initially presented with complaints of painful menstrual cramps that kept her bedridden most of the day. She also mentioned to her gynecologist that she had been diagnosed with endometriosis 4 years ago, and she could not find a medication or alternative therapeutic measure that helped. Her medical history was significant for surgery she had 6 years ago to remove tumors she had above her kidneys, after which she was prescribed hydrocortisone. An hour after the laparoscopic procedure, she calls the nurse because she is having difficulty breathing. The nurse records her vital signs include: blood pressure 85/55 mm Hg, respirations 20/min, and pulse 115/min. The patient suddenly loses consciousness. Intravenous fluids are started immediately. She gains consciousness, but her blood pressure is unchanged. Which of the following is the most likely cause of the hypotension?
- A. Bleeding profusely through the surgical site
- B. Improper supplementation of steroids (Correct Answer)
- C. Infection involving the suture line
- D. High doses of anesthetic drugs
- E. Loss of fluids during the procedure
CO2 insufflation physiology Explanation: ***Improper supplementation of steroids***
- The patient's history of **bilateral adrenalectomy (tumors above kidneys)** for which she was prescribed **hydrocortisone** indicates **adrenal insufficiency**. Stressful events like surgery require an increased dose of steroids, and improper supplementation can lead to an **adrenal crisis**.
- The symptoms of **hypotension, tachycardia, and loss of consciousness** are characteristic of an **adrenal crisis (acute adrenal insufficiency)**, which occurs when the body lacks sufficient cortisol during stress.
*Bleeding profusely through the surgical site*
- While **hemorrhage** can cause hypotension and tachycardia, the patient regained consciousness with IV fluids but her **blood pressure remained unchanged**, which is less typical for isolated blood loss if volume is restored without addressing the underlying cause.
- There is no direct mention of visible bleeding, the prompt only states the patient lost consciousness and her blood pressure is unchanged.
*Infection involving the suture line*
- **Surgical site infections** typically manifest several days post-op, presenting with **fever, erythema, and purulent drainage**, not acute hypotension and loss of consciousness an hour after surgery.
- The immediate post-operative timeline and systemic symptoms are not consistent with a localized wound infection as the primary cause of this acute decline.
*High doses of anesthetic drugs*
- Anesthetic drugs can cause **vasodilation and hypotension**. However, their effects are usually transient and would likely resolve more completely with IV fluids, especially an hour after a laparoscopic procedure.
- If it was due to anesthetic drugs, the patient's blood pressure would likely normalize with fluid administration once the effects of the anesthetic began to wear off, which is not the case here.
*Loss of fluids during the procedure*
- **Fluid loss** during surgery can cause hypotension, but intravenous fluids were administered, and the patient regained consciousness.
- If fluid loss were the sole cause, resolving consciousness and maintaining low blood pressure typically indicates the fluid loss was not completely compensated, but the primary cause for the persistent hypotension is not just volume.
CO2 insufflation physiology US Medical PG Question 3: A 27-year-old man is brought to the emergency department 30 minutes after being shot in the abdomen during a violent altercation. His temperature is 36.5°C (97.7°F), pulse is 118/min and regular, and blood pressure is 88/65 mm Hg. Examination shows cool extremities. Abdominal examination shows a 2.5-cm entrance wound in the left upper quadrant at the midclavicular line, below the left costal margin. Focused ultrasound shows free fluid in the left upper quadrant. Which of the following sets of hemodynamic changes is most likely in this patient?
Cardiac output (CO) | Pulmonary capillary wedge pressure (PCWP) | Systemic vascular resistance (SVR) | Central venous pressure (CVP)
- A. ↑ ↓ ↓ ↓
- B. ↓ ↓ ↑ ↑
- C. ↓ ↓ ↓ ↓
- D. ↓ ↓ ↑ ↓ (Correct Answer)
- E. ↓ ↑ ↑ ↑
CO2 insufflation physiology Explanation: ***↓ ↓ ↑ ↓***
- This patient is in **hypovolemic shock** due to hemorrhage, leading to decreased **cardiac output (CO)** and **pulmonary capillary wedge pressure (PCWP)** due to reduced preload.
- The body compensates for hypovolemia by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, while **central venous pressure (CVP)** decreases due to the depleted blood volume.
*↑ ↓ ↓ ↓*
- An increased **cardiac output** is inconsistent with hypovolemic shock, where the heart's ability to pump blood is compromised by a lack of circulating volume.
- While **PCWP**, **SVR**, and **CVP** decreasing could be seen in some forms of shock, the elevated CO rules out hypovolemic shock.
*↓ ↓ ↑ ↑*
- An elevated **central venous pressure (CVP)** is inconsistent with hypovolemic shock, as CVP reflects right atrial pressure and would be low due to decreased blood volume.
- While other parameters such as **CO** and **PCWP** decreasing and **SVR** increasing can be seen in hypovolemic shock, the increased CVP suggests a different hemodynamic state, like cardiogenic shock.
*↓ ↓ ↓ ↓*
- A decrease in **systemic vascular resistance (SVR)** is characteristic of **distributive shock** (e.g., septic or neurogenic shock), not hypovolemic shock, where compensatory vasoconstriction would lead to increased SVR.
- While **CO**, **PCWP**, and **CVP** would decrease due to overall poor perfusion, the SVR response differentiates it from hypovolemic shock.
*↓ ↑ ↑ ↑*
- An elevated **pulmonary capillary wedge pressure (PCWP)** and **central venous pressure (CVP)** indicate increased fluid volume or cardiac dysfunction, which is contrary to the reduced preload seen in hypovolemic shock.
- While **cardiac output (CO)** may decrease in cardiogenic shock, the other elevated pressures point away from a primary hypovolemic cause.
CO2 insufflation physiology US Medical PG Question 4: Five days after undergoing a pancreaticoduodenectomy for pancreatic cancer, a 46-year-old woman has 2 episodes of non-bilious vomiting and mild epigastric pain. She has a patient-controlled analgesia pump. She has a history of hypertension. She has smoked one pack of cigarettes daily for 25 years. She drinks 3–4 beers daily. Prior to admission to the hospital, her only medications were amlodipine and hydrochlorothiazide. Her temperature is 37.8°C (100°F), pulse is 98/min, and blood pressure is 116/82 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Examination shows a midline surgical incision over the abdomen with minimal serous discharge and no erythema. The abdomen is soft with mild tenderness to palpation in the epigastrium. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 11.6 g/dL
Leukocyte count 16,000/mm3
Serum
Na+ 133 mEq/L
K+ 3.4 mEq/L
Cl- 115 mEq/L
Glucose 77 mg/dL
Creatinine 1.2 mg/dL
Arterial blood gas on room air shows:
pH 7.20
pCO2 23 mm Hg
pO2 91 mm Hg
HCO3- 10 mEq/L
Which of the following is the most likely cause of this patient's acid-base status?
- A. Excessive alcohol intake
- B. Adrenal insufficiency
- C. Rhabdomyolysis
- D. Adverse effect of medication
- E. Fistula (Correct Answer)
CO2 insufflation physiology Explanation: ***Fistula***
- The patient's **metabolic acidosis** (pH 7.20, HCO3- 10 mEq/L) with normal anion gap (Na+ - (Cl- + HCO3-) = 133 - (115 + 10) = 8 mEq/L) suggests **bicarbonate loss**.
- A pancreaticoduodenectomy (Whipple procedure) involves multiple anastomoses, making **fistula formation** (e.g., pancreatic, biliary, or enteric) a significant complication that can lead to large volume losses of electrolyte-rich fluids, including bicarbonate.
*Excessive alcohol intake*
- While chronic alcohol intake can cause various metabolic derangements, an acute episode of acidosis due to alcohol typically presents as **alcoholic ketoacidosis** (high anion gap) or lactic acidosis.
- The patient's presentation of a normal anion gap metabolic acidosis does not align with the typical acid-base disturbances directly caused by acute alcohol intoxication or withdrawal.
*Adrenal insufficiency*
- Adrenal insufficiency can cause **hyponatremia**, hyperkalemia, and sometimes **non-anion gap metabolic acidosis** due to impaired aldosterone function leading to decreased H+ secretion and bicarbonate reabsorption.
- However, the patient's **potassium (3.4 mEq/L)** is within the normal range to slightly low, and the clinical picture following recent major surgery points more directly to surgical complications.
*Rhabdomyolysis*
- Rhabdomyolysis typically causes a **high anion gap metabolic acidosis** due to the release of phosphorous and other organic acids from damaged muscle cells, as well as potential acute kidney injury.
- This patient has a **normal anion gap acidosis**, and there are no clinical signs (e.g., muscle pain, elevated creatine kinase) pointing towards rhabdomyolysis.
*Adverse effect of medication*
- The patient's medications, amlodipine and hydrochlorothiazide, are not typically associated with a severe normal anion gap metabolic acidosis in this context.
- While **thiazide diuretics** can rarely cause mild metabolic alkalosis due to volume contraction, they would not cause this degree of acidosis, especially with a normal anion gap, and are not known to directly cause bicarbonate loss associated with a fistula.
CO2 insufflation physiology US Medical PG Question 5: A 32-year-old woman comes to the physician for a screening health examination that is required for scuba diving certification. The physician asks her to perform a breathing technique: following deep inspiration, she is instructed to forcefully exhale against a closed airway and contract her abdominal muscles while different cardiovascular parameters are evaluated. Which of the following effects is most likely after 10 seconds in this position?
- A. Decreased intra-abdominal pressure
- B. Decreased left ventricular stroke volume (Correct Answer)
- C. Decreased pulse rate
- D. Decreased systemic vascular resistance
- E. Increased venous return to left atrium
CO2 insufflation physiology Explanation: ***Decreased left ventricular stroke volume***
- After 10 seconds of performing the **Valsalva maneuver**, the increased intrathoracic pressure significantly reduces **venous return** to the heart.
- Reduced venous return leads to decreased **ventricular filling** (preload), which in turn diminishes **left ventricular stroke volume** and cardiac output.
*Decreased intra-abdominal pressure*
- The instruction to "contract her abdominal muscles" during forceful exhalation against a closed airway (Valsalva maneuver) directly leads to an **increase** in **intra-abdominal pressure**, not a decrease.
- This increase in intra-abdominal pressure further impedes venous return from the lower extremities to the heart.
*Decreased pulse rate*
- In the initial phase of the Valsalva maneuver (first 5-10 seconds), the decrease in cardiac output triggers a **reflex tachycardia** to maintain blood pressure, leading to an **increased pulse rate**.
- A decrease in pulse rate (bradycardia) is more characteristic of the release phase, not during the sustained strain.
*Decreased systemic vascular resistance*
- During the Valsalva maneuver, the body attempts to compensate for the drop in cardiac output and blood pressure by increasing **sympathetic tone**, which causes **vasoconstriction** and thus **increases systemic vascular resistance**.
- A decrease in systemic vascular resistance would further drop blood pressure and is not the physiological response during this phase.
*Increased venous return to left atrium*
- The Valsalva maneuver dramatically **reduces venous return** to both the right and left atria due to the high intrathoracic pressure compressing the great veins.
- This decreased venous return is the primary mechanism leading to the subsequent fall in cardiac output during the maneuver.
CO2 insufflation physiology US Medical PG Question 6: Three days after undergoing laparoscopic colectomy, a 67-year-old man reports swelling and pain in his right leg. He was diagnosed with colon cancer 1 month ago. His temperature is 38.5°C (101.3°F). Physical examination shows swelling of the right leg from the ankle to the thigh. There is no erythema or rash. Which of the following is likely to be most helpful in establishing the diagnosis?
- A. D-dimer level
- B. Compression ultrasonography (Correct Answer)
- C. CT pulmonary angiography
- D. Transthoracic echocardiography
- E. Blood cultures
CO2 insufflation physiology Explanation: ***Compression ultrasonography***
- This patient's presentation with **unilateral leg swelling and pain** after surgery, especially given his recent **colon cancer diagnosis** (a hypercoagulable state), is highly suspicious for a **deep vein thrombosis (DVT)**.
- **Compression ultrasonography** is the gold standard, non-invasive imaging modality for diagnosing DVT, allowing direct visualization of thrombi and assessing venous compressibility.
*D-dimer level*
- While a **positive D-dimer** indicates recent or ongoing clot formation, it is **non-specific** and can be elevated in many conditions, including surgery, cancer, and infection.
- A normal D-dimer can rule out DVT in low-probability patients, but a high D-dimer in a high-probability patient (like this case) requires further imaging for confirmation, making it less definitive than ultrasound.
*CT pulmonary angiography*
- This imaging is used to diagnose a **pulmonary embolism (PE)**, which is a complication of DVT, but the primary symptoms here are localized to the leg.
- While PE is a concern, diagnosing the source (DVT) in the leg is the immediate priority for treatment and prevention of future complications.
*Transthoracic echocardiography*
- **Echocardiography** evaluates cardiac structure and function and can sometimes detect large clots in the right heart leading to PE, but it is not the primary diagnostic tool for DVT in the leg.
- It would be done if signs of cardiac strain or shunting associated with acute PE were prominent, which is not the case here.
*Blood cultures*
- **Blood cultures** are used to diagnose **bacteremia or sepsis**, which might explain a fever, but the prominent, unilateral leg swelling and pain are not typical for a primary infectious cause in the leg without local signs of cellulitis or abscess.
- While a low-grade fever is present, the absence of erythema or rash makes a primary infectious etiology less likely than DVT given the risk factors.
CO2 insufflation physiology US Medical PG Question 7: A 32-year-old man is brought to the emergency department after a skiing accident. The patient had been skiing down the mountain when he collided with another skier who had stopped suddenly in front of him. He is alert but complaining of pain in his chest and abdomen. He has a past medical history of intravenous drug use and peptic ulcer disease. He is a current smoker. His temperature is 97.4°F (36.3°C), blood pressure is 77/53 mmHg, pulse is 127/min, and respirations are 13/min. He has a GCS of 15 and bilateral shallow breath sounds. His abdomen is soft and distended with bruising over the epigastrium. He is moving all four extremities and has scattered lacerations on his face. His skin is cool and delayed capillary refill is present. Two large-bore IVs are placed in his antecubital fossa, and he is given 2L of normal saline. His FAST exam reveals fluid in Morison's pouch. Following the 2L normal saline, his temperature is 97.5°F (36.4°C), blood pressure is 97/62 mmHg, pulse is 115/min, and respirations are 12/min.
Which of the following is the best next step in management?
- A. Diagnostic peritoneal lavage
- B. Emergency laparotomy (Correct Answer)
- C. Upper gastrointestinal endoscopy
- D. Close observation
- E. Diagnostic laparoscopy
CO2 insufflation physiology Explanation: ***Emergency laparotomy***
- The patient remains **hemodynamically unstable** (BP 97/62 mmHg, HR 115/min after 2L IV fluids) with evidence of **intra-abdominal fluid on FAST exam** (fluid in Morison's pouch).
- This clinical picture indicates active intra-abdominal hemorrhage requiring **immediate surgical intervention** to identify and control the source of bleeding.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has largely been replaced by the focused abdominal sonography for trauma (FAST) exam and CT scans.
- While it can detect intra-abdominal bleeding, it is **invasive** and would delay definitive treatment in a hemodynamically unstable patient with positive FAST.
*Upper gastrointestinal endoscopy*
- This procedure is primarily for diagnosing and treating **upper gastrointestinal bleeding** or mucosal abnormalities.
- It is **not indicated** for evaluating traumatic intra-abdominal hemorrhage or hemodynamic instability following blunt abdominal trauma.
*Close observation*
- Close observation is appropriate for **hemodynamically stable patients** with blunt abdominal trauma and minor injuries or equivocal findings.
- This patient's persistent hypotension, tachycardia, and positive FAST findings rule out observation as a safe or appropriate next step.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a minimally invasive surgical procedure used to evaluate the abdominal cavity.
- While it can be diagnostic, it is generally **contraindicated in hemodynamically unstable patients** as it can prolong the time to definitive hemorrhage control if a major injury is found.
CO2 insufflation physiology US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
CO2 insufflation physiology Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
CO2 insufflation physiology US Medical PG Question 9: A 63-year-old man is brought to the emergency department, 30 minutes after being involved in a high-speed motor vehicle collision. He is obtunded on arrival. He is intubated and mechanical ventilation is begun. The ventilator is set at a FiO2 of 60%, tidal volume of 440 mL, and positive end-expiratory pressure of 4 cm H2O. On the third day of intubation, his temperature is 37.3°C (99.1°F), pulse is 91/min, and blood pressure is 103/60 mm Hg. There are decreased breath sounds over the left lung base. Cardiac examination shows no abnormalities. The abdomen is soft and not distended. Arterial blood gas analysis shows:
pH 7.49
pCO2 29 mm Hg
pO2 73 mm Hg
HCO3- 20 mEq/L
O2 saturation 89%
Monitoring shows a sudden increase in the plateau airway pressure. An x-ray of the chest shows deepening of the costophrenic angle on the left side. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Administer levofloxacin
- C. Close observation
- D. Increase the PEEP
- E. Insertion of a chest tube (Correct Answer)
CO2 insufflation physiology Explanation: ***Insertion of a chest tube***
- The sudden increase in **plateau airway pressure**, decreased breath sounds over the left lung base, worsening hypoxemia (O2 sat 89%) despite high FiO2, and **deepening of the costophrenic angle on the left side** indicate a **traumatic hemothorax**.
- Deepening of the costophrenic angle on chest X-ray is a classic sign of **pleural fluid accumulation** (hemothorax or pleural effusion), not pneumothorax.
- In a trauma patient (high-speed motor vehicle collision) on day 3 of mechanical ventilation, this represents a **delayed hemothorax** requiring immediate drainage.
- **Chest tube insertion** is the definitive management to evacuate blood, re-expand the lung, and improve ventilation and oxygenation.
*CT scan of the chest*
- While CT scan would provide detailed anatomical information, the clinical presentation with sudden respiratory decompensation and clear chest X-ray findings of hemothorax requires **immediate intervention**.
- Delaying treatment to obtain CT imaging in an unstable ventilated patient could worsen hypoxemia and lead to cardiovascular compromise.
- CT scan may be obtained later if needed to evaluate for ongoing bleeding or other injuries.
*Administer levofloxacin*
- Antibiotics would be appropriate for **pneumonia or empyema**, but the patient has no clear signs of infection (afebrile at 37.3°C, acute presentation over hours not days).
- The primary problem is **mechanical compression** from pleural fluid accumulation, not infection.
- Antibiotics do not address the life-threatening respiratory compromise from hemothorax.
*Close observation*
- Close observation is inappropriate given the acute deterioration with increased plateau pressures and worsening hypoxemia.
- The patient requires urgent intervention to prevent further respiratory failure and potential cardiovascular collapse.
- Expectant management would be negligent in this clinical scenario.
*Increase the PEEP*
- Increasing **Positive End-Expiratory Pressure (PEEP)** would worsen the situation by increasing intrathoracic pressure against an already compressed lung.
- Higher PEEP could impair venous return, decrease cardiac output, and potentially convert a simple hemothorax to a tension physiology.
- PEEP adjustments do not address the underlying problem of pleural space fluid accumulation requiring drainage.
CO2 insufflation physiology US Medical PG Question 10: A 37-year-old woman is brought to the emergency department 15 minutes after falling down a flight of stairs. On arrival, she has shortness of breath, right-sided chest pain, right upper quadrant abdominal pain, and right shoulder pain. She is otherwise healthy. She takes no medications. She appears pale. Her temperature is 37°C (98.6°F), pulse is 115/min, respirations are 20/min, and blood pressure is 85/45 mm Hg. Examination shows several ecchymoses over the right chest. There is tenderness to palpation over the right chest wall and right upper quadrant of the abdomen. Bowel sounds are normal. Cardiopulmonary examination shows no abnormalities. Neck veins are flat. Which of the following is the most likely diagnosis?
- A. Splenic laceration
- B. Liver hematoma (Correct Answer)
- C. Pneumothorax
- D. Duodenal hematoma
- E. Small bowel perforation
CO2 insufflation physiology Explanation: ***Liver hematoma***
- The patient's presentation with **right upper quadrant abdominal pain**, **right shoulder pain** (referred pain from diaphragmatic irritation), and **hypotension** following a fall points strongly to **liver injury**.
- The liver is the **most commonly injured organ** in blunt abdominal trauma due to its size and position.
*Splenic laceration*
- While splenic laceration can cause hypovolemic shock, pain is typically localized to the **left upper quadrant** and left shoulder (**Kehr's sign**), not the right.
- The ecchymoses and tenderness are predominantly on the **right side** of the chest and abdomen.
*Pneumothorax*
- A pneumothorax would typically present with **unilateral diminished breath sounds**, **hyperresonance to percussion**, and potentially **tracheal deviation**, none of which are mentioned.
- The patient's **blood pressure is low**, which is more suggestive of significant hemorrhage than an isolated pneumothorax, especially with **flat neck veins**.
*Duodenal hematoma*
- A duodenal hematoma typically presents with **epigastric pain**, **vomiting**, and symptoms of **gastric outlet obstruction**, often days after the injury.
- It does not typically cause **referred shoulder pain** or immediate **hypovolemic shock** as seen here.
*Small bowel perforation*
- Small bowel perforation would present with signs of **peritonitis**, such as **rebound tenderness**, **guarding**, and absent or diminished bowel sounds due to inflammation from bowel contents.
- While there is abdominal pain, the **bowel sounds are normal**, and the primary symptoms align more with **hemorrhage**.
More CO2 insufflation physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.