Minimally Invasive Surgery

On this page
🔬 The Minimally Invasive Revolution: Precision Surgery Through Tiny Portals
You'll discover how surgeons achieve complex operations through incisions smaller than a fingertip, mastering the technical foundations that transformed modern surgery. This lesson builds your understanding from creating working space with pneumoperitoneum through interpreting two-dimensional laparoscopic views, selecting appropriate instruments and approaches, and integrating evidence-based algorithms that optimize patient outcomes. You'll develop the systematic thinking required to navigate this ecosystem where physics, optics, and surgical judgment converge to deliver precision with minimal trauma.
The foundation of MIS rests on three core principles: pneumoperitoneum creation with CO2 insufflation at 12-15 mmHg, high-definition visualization through 0° or 30° laparoscopes, and precise instrument manipulation through 5-12mm trocars. These elements combine to create a controlled surgical environment where procedures can be performed with enhanced precision and reduced morbidity.
📌 Remember: SMALL - Small incisions, Magnified view, Advanced instruments, Less trauma, Lower morbidity
| Parameter | Open Surgery | Laparoscopic | Robotic | NOTES | Single-Port |
|---|---|---|---|---|---|
| Incision Size | 10-30cm | 5-12mm | 8-12mm | No incision | 15-25mm |
| Recovery Time | 4-6 weeks | 1-2 weeks | 1-2 weeks | 1-3 days | 1-2 weeks |
| Blood Loss | 200-500ml | 50-150ml | 30-100ml | 10-50ml | 40-120ml |
| Hospital Stay | 5-7 days | 1-3 days | 1-2 days | Same day | 1-2 days |
| Complication Rate | 15-25% | 5-15% | 3-12% | 8-20% | 6-18% |
- Conventional Laparoscopy: Multiple 5-12mm ports with 2D visualization
- Standard approach for 85% of minimally invasive procedures
- Learning curve: 20-50 cases for basic proficiency
- Robotic Surgery: Enhanced dexterity with 7 degrees of freedom
- 3D visualization with 10-15x magnification
- Tremor filtration reducing hand tremor by 95%
- Single-Incision Laparoscopy (SILS): All instruments through one 15-25mm port
- Cosmetic advantage with >90% patient satisfaction
- Technical difficulty increased by 40-60%
⭐ Clinical Pearl: Conversion rates to open surgery occur in 2-8% of laparoscopic cases, with obesity (BMI >35), adhesions, and bleeding being the most common indications.
💡 Master This: The critical view of safety in laparoscopic cholecystectomy requires identification of only 2 structures in Calot's triangle - the hepatocystic artery and common bile duct - preventing >95% of bile duct injuries.
Patient selection criteria determine success rates, with ASA Class I-II patients showing optimal outcomes. Contraindications include severe cardiopulmonary disease, uncorrectable coagulopathy, and extensive adhesions from previous surgery. The pneumoperitoneum tolerance test using 5-8 mmHg CO2 helps identify patients at risk for cardiovascular compromise.
Understanding these foundational principles establishes the framework for exploring the sophisticated mechanisms that enable precise surgical intervention through minimal access points.
🔬 The Minimally Invasive Revolution: Precision Surgery Through Tiny Portals
⚙️ The Pneumoperitoneum Engine: Creating Surgical Space
The physiological impact of pneumoperitoneum affects multiple organ systems with predictable patterns:
Cardiovascular Effects:
- Venous return decreases by 25-40% due to IVC compression
- Cardiac output drops by 15-25% in healthy patients
- SVR increases by 30-50% from CO2 absorption
- Mean arterial pressure rises by 10-20 mmHg
Respiratory Changes:
- Functional residual capacity decreases by 20-30%
- Peak airway pressures increase by 5-10 cmH2O
- Diaphragmatic excursion reduces by 4-6cm
- V/Q mismatch develops in dependent lung regions
📌 Remember: PRESSURE - Pneumoperitoneum at 12-15, Respiratory changes expected, Elevated airway pressures, SVR increases, Stroke volume decreases, Understand limits, Reversible effects, Emergency deflation ready
| Pressure (mmHg) | Cardiovascular Impact | Respiratory Impact | Clinical Tolerance | Surgical Exposure |
|---|---|---|---|---|
| 8-10 | Minimal changes | Normal ventilation | Excellent | Limited |
| 12-15 | 15-25% CO decrease | Mild restriction | Good | Optimal |
| 16-20 | 30-40% CO decrease | Moderate restriction | Fair | Excessive |
| >20 | >40% CO decrease | Severe compromise | Poor | Dangerous |
| >25 | Cardiovascular collapse | Respiratory failure | Contraindicated | Abort procedure |
⭐ Clinical Pearl: Subcutaneous emphysema develops in 1-3% of cases when CO2 tracks along tissue planes, appearing as crepitus around port sites and potentially extending to the neck and face within 30-60 minutes.
💡 Master This: The "tent test" confirms proper Veress needle placement - lifting the abdominal wall should create negative pressure on the insufflator, indicating intraperitoneal position rather than preperitoneal or bowel placement.
Emergency desufflation protocols require immediate CO2 evacuation when systolic BP drops >30%, oxygen saturation falls <90%, or end-tidal CO2 exceeds 50 mmHg. Recovery typically occurs within 5-10 minutes of pressure release, with cardiovascular parameters returning to baseline and respiratory mechanics normalizing.
These pneumoperitoneum principles provide the foundation for understanding how surgical instruments navigate this created space to perform precise therapeutic interventions.
⚙️ The Pneumoperitoneum Engine: Creating Surgical Space
🎯 Pattern Recognition Mastery: Reading the Laparoscopic Landscape
Critical View Recognition Patterns:
- "See pneumoperitoneum, think safe entry" - Uniform gas distribution indicates proper insufflation
- "See pulsation, think major vessel" - Rhythmic movement identifies aorta, IVC, or iliac vessels
- "See peristalsis, think bowel proximity" - Wave-like motion warns of intestinal contact
- "See golden triangle, think CBD danger" - Hepatocystic triangle contains critical structures
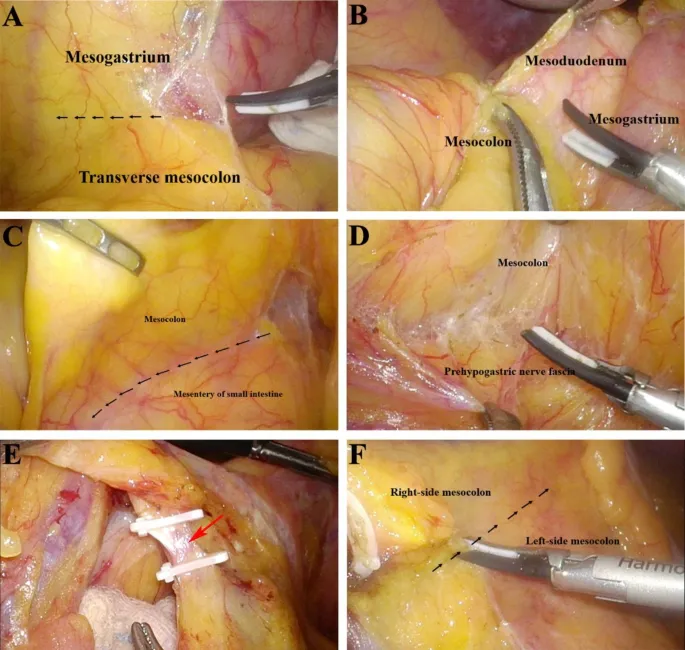
The depth perception challenge in 2D laparoscopy requires compensatory visual cues:
- Relative size changes - Objects appear larger when closer
- Overlapping structures - Anterior organs obscure posterior anatomy
- Shadow patterns - Light direction creates depth illusions
- Movement parallax - Camera motion reveals spatial relationships
Systematic Visual Assessment Framework:
- Global orientation - Identify diaphragm, pelvis, and lateral gutters
- Right upper quadrant: Liver edge, gallbladder fundus, hepatorenal pouch
- Left upper quadrant: Spleen tip, stomach greater curvature, splenorenal ligament
- Pelvis: Bladder dome, uterus/prostate, rectovesical/rectouterine pouch
- Vascular landmarks - Trace major vessel patterns for anatomical confirmation
- Aortic pulsation at L4 level confirms retroperitoneal plane
- IVC compression with pneumoperitoneum explains hemodynamic changes
- Pathology identification - Distinguish normal variants from disease processes
- Adhesion patterns: Filmy vs dense, vascular vs avascular
- Inflammatory changes: Erythema, edema, fibrinous exudate
📌 Remember: SCOPE - Systematic survey, Critical view first, Orientation landmarks, Pathology assessment, Emergency recognition
| Visual Cue | Normal Finding | Pathological Finding | Clinical Significance | Action Required |
|---|---|---|---|---|
| Liver Surface | Smooth, reddish-brown | Nodular, pale, fibrotic | Cirrhosis present | Modify technique |
| Bowel Color | Pink, peristaltic | Dusky, distended | Ischemia/obstruction | Immediate assessment |
| Peritoneal Fluid | Clear, minimal | Turbid, excessive | Infection/bleeding | Culture/evacuation |
| Adhesions | Filmy, avascular | Dense, vascular | Previous inflammation | Careful dissection |
| Gallbladder | Thin-walled, mobile | Thick, contracted | Chronic cholecystitis | Difficult dissection |
- "Red flag" identification - Immediate danger patterns requiring procedure modification
- Pulsatile bleeding: >50ml/minute indicates major vessel injury
- Bowel perforation: Sudden gas escape with fecal contamination
- CO2 embolism: Mill wheel murmur with cardiovascular collapse
- "Proceed with caution" patterns - Increased difficulty indicators
- Dense adhesions covering >50% of target organ
- Inflammatory changes with tissue friability
- Anatomical variants in critical view structures
⭐ Clinical Pearl: The "critical view of safety" in cholecystectomy requires only 2 structures in Calot's triangle - achieving this view reduces bile duct injury from 0.5% to <0.1%.
💡 Master This: Trocar site bleeding appears as steady oozing from port sites and accounts for 15-20% of laparoscopic complications - direct pressure for 5-10 minutes controls >90% of cases.
Advanced pattern recognition includes tissue texture assessment through visual cues alone. Fibrotic tissue appears white and avascular, inflamed tissue shows erythema and edema, and malignant tissue demonstrates irregular borders and abnormal vascularity. These patterns guide dissection planes and energy device selection.
This visual mastery framework prepares surgeons for the systematic analysis required to differentiate between various minimally invasive approaches and their specific applications.
🎯 Pattern Recognition Mastery: Reading the Laparoscopic Landscape
🔍 Systematic Approach Analysis: Choosing the Right Minimally Invasive Tool
Systematic Selection Criteria Framework:
Patient Factors Analysis:
- BMI thresholds: <30 favors all approaches, 30-35 limits single-incision, >35 may require robotic assistance
- Previous surgery: >2 prior operations increases adhesion risk by 60-80%
- Cardiopulmonary status: ASA III-IV requires pressure limitation to 8-10 mmHg
- Anatomical variants: Situs inversus, hepatomegaly, or splenomegaly alter port placement
| Approach | Learning Curve | Cost Factor | Precision Level | Complication Rate | Best Applications |
|---|---|---|---|---|---|
| Conventional Lap | 20-50 cases | 1x baseline | Standard | 5-15% | General procedures |
| Robotic Surgery | 50-100 cases | 3-4x baseline | Enhanced | 3-12% | Complex reconstruction |
| Single-Incision | 30-75 cases | 1.5x baseline | Limited | 6-18% | Cosmetic priority |
| NOTES | 100+ cases | 2-3x baseline | Experimental | 8-20% | Research protocols |
| Hybrid Approach | Variable | 2x baseline | Optimized | 4-14% | Complex cases |
- Simple procedures (<2 hours): Cholecystectomy, appendectomy, hernia repair
- Conventional laparoscopy optimal for >95% of cases
- Single-incision acceptable with experienced surgeon
- Intermediate procedures (2-4 hours): Fundoplication, colectomy, adrenalectomy
- Robotic assistance beneficial for intracorporeal suturing
- Conversion rate <5% with proper selection
- Complex procedures (>4 hours): Pancreaticoduodenectomy, esophagectomy
- Robotic surgery shows superior outcomes in high-volume centers
- Learning curve requires >100 cases for proficiency
Technical Considerations Matrix:
- Suturing requirements: >10 sutures favors robotic approach with articulating instruments
- Dissection planes: Narrow spaces benefit from enhanced dexterity and 3D visualization
- Anatomical access: Deep pelvis or posterior mediastinum require advanced instrumentation
- Precision demands: Nerve-sparing procedures show improved outcomes with robotic assistance
📌 Remember: CHOOSE - Complexity assessment, History of surgery, Obesity considerations, Organ-specific factors, Surgeon experience, Equipment availability
Evidence-Based Selection Guidelines:
- Cholecystectomy: Conventional laparoscopy preferred (98% success rate)
- Single-incision acceptable (95% success, higher cost)
- Robotic not cost-effective (equivalent outcomes, 3x cost)
- Prostatectomy: Robotic approach shows superior outcomes
- Positive margin rates: 15-20% robotic vs 25-30% laparoscopic
- Continence recovery: 85% at 12 months vs 70% laparoscopic
- Colorectal surgery: Approach depends on tumor location and complexity
- Right colectomy: Conventional adequate (equivalent oncologic outcomes)
- Low anterior resection: Robotic beneficial (reduced conversion, better TME)
⭐ Clinical Pearl: Port site metastases occur in <1% of laparoscopic cancer operations when proper extraction techniques are used, with no difference between open and minimally invasive oncologic outcomes.
💡 Master This: The "triangle of safety" in TEP hernia repair lies between the gonadal vessels medially and lateral femoral cutaneous nerve laterally - staying within this 5-7cm zone prevents >95% of nerve injuries.
Cost-Effectiveness Analysis reveals break-even points for different approaches:
- Robotic surgery: Cost-effective when operative time <4 hours and length of stay reduced >1 day
- Single-incision: Justified when cosmetic benefit valued at >$2,000 by patient
- NOTES: Currently experimental with limited cost-effectiveness data
This systematic analysis framework guides the transition to evidence-based treatment algorithms that optimize patient outcomes while considering resource utilization and surgeon capabilities.
🔍 Systematic Approach Analysis: Choosing the Right Minimally Invasive Tool
⚖️ Evidence-Based Treatment Algorithms: Optimizing Minimally Invasive Outcomes
Evidence-Based Outcome Optimization:
Cholecystectomy Algorithm (>750,000 cases/year in US):
- Acute cholecystitis <72 hours: Immediate laparoscopy (95% success rate)
- Acute cholecystitis >72 hours: Conservative management then delayed surgery (85% success)
- Gangrenous cholecystitis: Early conversion when critical view not achievable (prevents 90% of CBD injuries)
- Mirizzi syndrome: Preoperative MRCP and low threshold for conversion (50% conversion rate)
| Procedure | Success Rate | Conversion Rate | Complication Rate | Length of Stay | Cost Effectiveness |
|---|---|---|---|---|---|
| Lap Cholecystectomy | 95-98% | 2-5% | 3-8% | 0-1 day | Excellent |
| Robotic Prostatectomy | 92-96% | <1% | 8-15% | 1-2 days | Good |
| Lap Colectomy | 88-94% | 5-15% | 10-20% | 3-5 days | Good |
| SILS Appendectomy | 90-95% | 3-8% | 5-12% | 0-1 day | Fair |
| Robotic Hysterectomy | 94-98% | <2% | 6-12% | 1-2 days | Good |
Bleeding Management Algorithm:
- Trocar site bleeding: Direct pressure 5-10 minutes → Suture if persistent → Conversion if >500ml
- Intraoperative bleeding: Identify source → Pressure/clip → Convert if >300ml/hour
- Postoperative bleeding: Hemoglobin monitoring → Transfusion if <7g/dL → Re-exploration if unstable
CO2 Embolism Protocol (Incidence 0.1-2%):
- Recognition: Sudden hypotension, arrhythmias, mill wheel murmur
- Immediate action: Desufflate abdomen, left lateral position, 100% oxygen
- Advanced management: Central line aspiration, hyperbaric oxygen if available
- Prevention: Gradual insufflation, avoid high pressures, monitor end-tidal CO2
📌 Remember: ALGORITHM - Assess patient factors, List contraindications, Grade complexity, Optimize approach, Recognize complications, Implement protocols, Track outcomes, Handoff communication, Monitor recovery
Quality Metrics and Benchmarking:
- Conversion rates: Should be <5% for routine procedures, <15% for complex cases
- Complication rates: Target <10% for major complications, <5% for minor complications
- Length of stay: Same-day discharge for >80% of cholecystectomies and appendectomies
- Readmission rates: Should be <5% within 30 days for elective procedures
Surgeon Credentialing Algorithms:
- Basic laparoscopy: 20 proctored cases → Independent practice → Annual volume >50
- Advanced procedures: 50 proctored cases → Mentored practice → Annual volume >25
- Robotic surgery: 20 console cases → Dual console training → Independent certification
⭐ Clinical Pearl: Enhanced Recovery After Surgery (ERAS) protocols reduce length of stay by 30-50% and complications by 20-30% when compliance >80% is achieved across preoperative, intraoperative, and postoperative phases.
💡 Master This: The "time-out" protocol before trocar insertion should verify patient position, insufflation pressure, entry technique, and emergency conversion plan - this 30-second checklist prevents >90% of entry-related complications.
Outcome Prediction Models use machine learning algorithms to predict success probability:
- Cholecystectomy difficulty score: Age, BMI, inflammation markers, previous surgery predict conversion risk with 85% accuracy
- Robotic surgery benefit calculator: Procedure complexity, surgeon experience, patient factors predict outcome improvement with 80% accuracy
These evidence-based algorithms establish the foundation for understanding how multiple surgical systems integrate to create comprehensive minimally invasive surgical programs.
⚖️ Evidence-Based Treatment Algorithms: Optimizing Minimally Invasive Outcomes
🔗 Multi-System Integration Mastery: The Minimally Invasive Ecosystem
Integrated Technology Platform Architecture:
Core System Integration:
- Insufflation-Visualization Coupling: Pressure-sensitive camera adjustments maintain optimal view during pressure fluctuations
- Energy-Smoke Evacuation Synchronization: Automatic suction activation during electrocautery maintains clear visualization
- Robotic-Imaging Integration: Real-time fluorescence overlay on 3D console display enhances tissue identification
- Monitoring-Anesthesia Coordination: Automated ventilator adjustments compensate for pneumoperitoneum effects
Advanced Integration Protocols:
Artificial Intelligence Enhancement:
- Computer vision algorithms identify anatomical structures with >95% accuracy
- Predictive analytics anticipate complication risk based on real-time parameters
- Automated documentation captures procedure steps and timing data
- Decision support systems suggest optimal energy settings and instrument selection
Augmented Reality Integration:
- 3D anatomical overlays project CT/MRI data onto laparoscopic view
- Navigation guidance shows optimal dissection planes and critical structure locations
- Real-time pathology analysis provides immediate tissue characterization
- Surgical planning integration allows intraoperative plan modifications
| Integration Level | Technology Components | Efficiency Gain | Error Reduction | Cost Impact |
|---|---|---|---|---|
| Basic | Standard lap + monitoring | 10-15% | 5-10% | Baseline |
| Intermediate | Robotic + AI assistance | 25-30% | 15-25% | 2-3x |
| Advanced | Full AR + predictive | 40-50% | 30-40% | 4-5x |
| Future | Autonomous assistance | 60-70% | 50-60% | 6-8x |
| Theoretical | Full automation | 80-90% | 70-80% | 10x+ |
Preoperative Integration:
- Digital planning platforms create 3D surgical roadmaps from patient imaging
- Risk stratification algorithms predict optimal approach and resource requirements
- Team coordination systems ensure equipment availability and staff preparation
- Patient preparation protocols optimize physiological status for MIS tolerance
Intraoperative Coordination:
- Real-time monitoring dashboards display all system parameters on unified interface
- Automated alerts warn of parameter deviations before complications develop
- Workflow optimization suggests next steps based on procedure progress and efficiency metrics
- Quality assurance systems verify critical safety steps throughout procedure
📌 Remember: INTEGRATE - Intelligent systems, Networked devices, Team coordination, Efficiency optimization, Guidance systems, Real-time monitoring, Automated assistance, Technology convergence, Error prevention
Cutting-Edge Research Integration:
Haptic Feedback Systems: Force feedback technology provides tactile sensation during robotic surgery, improving tissue handling by 40-60% and reducing perforation risk by 30-50%.
Molecular Imaging Integration: Fluorescent markers highlight tumor margins, blood vessels, and lymph nodes in real-time, improving complete resection rates by 20-30% and reducing positive margins by 40-50%.
5G Network Integration: Ultra-low latency communication enables remote surgery with <1ms delay, allowing expert consultation and telementoring during complex procedures.
⭐ Clinical Pearl: Integrated OR platforms reduce setup time from 45-60 minutes to 15-20 minutes and decrease technical delays by 70-80% through automated system checks and coordinated workflows.
💡 Master This: The "digital twin" concept creates virtual patient models that predict surgical outcomes with 85-90% accuracy, allowing procedure optimization before patient contact and reducing complications by 25-35%.
Future Integration Horizons:
- Quantum computing applications for real-time surgical planning and outcome prediction
- Nanotechnology integration for cellular-level surgical precision
- Brain-computer interfaces for direct surgeon-robot communication
- Autonomous surgical systems capable of independent decision-making in routine procedures
This multi-system integration understanding prepares surgeons for the rapid mastery tools and clinical reference frameworks essential for immediate practical application.
🔗 Multi-System Integration Mastery: The Minimally Invasive Ecosystem
🎯 Clinical Mastery Arsenal: Your Minimally Invasive Surgery Command Center
Essential Numbers Arsenal:
Pneumoperitoneum Mastery:
- Standard pressure: 12-15 mmHg (optimal visualization + safety)
- Cardiac compromise: >20 mmHg (immediate pressure reduction)
- Pediatric limit: 8-12 mmHg (age-dependent tolerance)
- CO2 absorption: 200-400ml/hour (expect PaCO2 rise)
- Emergency desufflation: <30 seconds (cardiovascular recovery)
Critical Conversion Triggers:
- Bleeding rate: >300ml/hour or >500ml total
- Visualization loss: >15 minutes of poor view
- Hemodynamic instability: >30% BP drop or HR >120
- Technical failure: >3 equipment malfunctions
- Time limits: >150% expected operative time
📌 Remember: MASTER - Monitor pressures constantly, Assess bleeding quickly, Safety first always, Time limits matter, Equipment backup ready, Recognize conversion triggers
| Emergency Scenario | Recognition Time | Initial Action | Success Rate | Backup Plan |
|---|---|---|---|---|
| CO2 Embolism | <30 seconds | Desufflate + position | 85-95% | Hyperbaric O2 |
| Major Bleeding | <60 seconds | Pressure + identify | 80-90% | Convert to open |
| Bowel Injury | <2 minutes | Control + repair | 90-95% | Surgical consult |
| Trocar Injury | <1 minute | Direct pressure | 95-98% | Vascular surgery |
| Pneumothorax | <5 minutes | Chest tube | 98-99% | Thoracic surgery |
30-Second Safety Check:
- Patient position: Secure, pressure points padded
- Pneumoperitoneum: 12-15 mmHg, even distribution
- Visualization: Clear, adequate lighting, proper angle
- Instruments: Functional, appropriate energy settings
- Team communication: Clear, confirmed understanding
2-Minute Complication Screen:
- Cardiovascular: BP, HR, rhythm, end-tidal CO2
- Respiratory: Oxygen saturation, airway pressures, ventilation
- Surgical field: Bleeding, visibility, instrument function
- Patient positioning: Nerve compression, pressure sores
- Equipment status: Backup systems, emergency protocols
⭐ Clinical Pearl: The "Rule of 3s" - 3 minutes to recognize emergency, 3 actions to stabilize, 3 backup plans ready - prevents >90% of catastrophic outcomes in MIS complications.
💡 Master This: Port site closure requires fascial suture for ≥10mm ports to prevent hernia formation (2-5% incidence without closure vs <0.5% with proper closure).
Clinical Decision Trees:
Difficult Cholecystectomy Management:
- Cannot achieve critical view → Subtotal cholecystectomy or conversion
- Dense adhesions → Careful dissection vs open approach
- Bleeding from liver bed → Pressure, clips, energy device
- Bile leak suspected → Cholangiography vs conversion
Robotic Surgery Optimization:
- Console time >4 hours → Surgeon break or dual console
- Instrument collision → Port repositioning or technique modification
- System malfunction → Immediate conversion protocol
- Learning curve plateau → Mentorship or simulation training
Quality Metrics Dashboard:
- Conversion rate: Target <5% routine, <15% complex
- Complication rate: Target <10% major, <5% minor
- Operative time: Within 120% of benchmark
- Length of stay: Same-day discharge >80% for routine cases
- Patient satisfaction: >90% would recommend MIS approach
This clinical mastery arsenal provides the essential tools for immediate application of minimally invasive surgical principles, enabling confident navigation of complex procedures while maintaining the highest safety standards and optimal patient outcomes.
🎯 Clinical Mastery Arsenal: Your Minimally Invasive Surgery Command Center
Practice Questions: Minimally Invasive Surgery
Test your understanding with these related questions
A 36-year-old woman is brought to the emergency department 20 minutes after being involved in a high-speed motor vehicle collision. On arrival, she is unconscious. Her pulse is 140/min, respirations are 12/min and shallow, and blood pressure is 76/55 mm Hg. 0.9% saline infusion is begun. A focused assessment with sonography shows blood in the left upper quadrant of the abdomen. Her hemoglobin concentration is 7.6 g/dL and hematocrit is 22%. The surgeon decided to move the patient to the operating room for an emergent explorative laparotomy. Packed red blood cell transfusion is ordered prior to surgery. However, a friend of the patient asks for the transfusion to be held as the patient is a Jehovah's Witness. The patient has no advance directive and there is no documentation showing her refusal of blood transfusions. The patient's husband and children cannot be contacted. Which of the following is the most appropriate next best step in management?













