Stress urinary incontinence procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Stress urinary incontinence procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Stress urinary incontinence procedures US Medical PG Question 1: A 53-year-old multiparous woman is scheduled to undergo elective sling surgery for treatment of stress incontinence. She has frequent loss of small amounts of urine when she coughs or laughs, despite attempts at conservative treatment. The physician inserts trocars in the obturator foramen bilaterally to make the incision and passes a mesh around the pubic bones and underneath the urethra to form a sling. During the procedure, the physician accidentally injures a nerve in the obturator foramen. The function of which of the following muscles is most likely to be affected following the procedure?
- A. Obturator internus
- B. Tensor fascia latae
- C. Adductor longus (Correct Answer)
- D. Semitendinosus
- E. Transversus abdominis
Stress urinary incontinence procedures Explanation: ***Adductor longus***
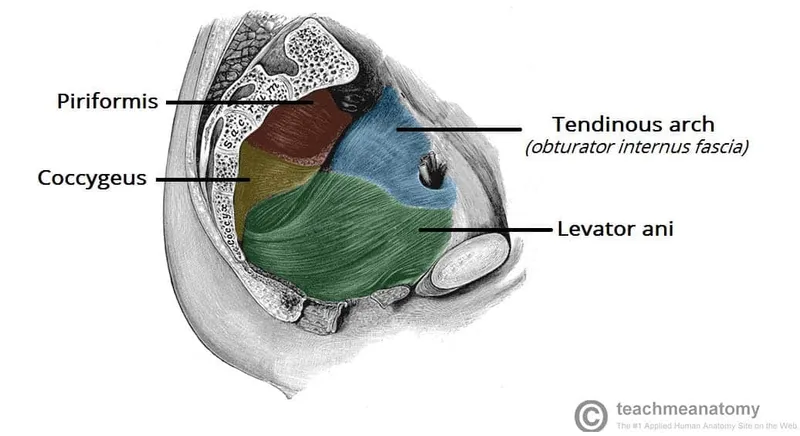
- The **obturator nerve** passes through the obturator foramen and innervates the **adductor muscles** of the thigh, including the **adductor longus**.
- Injury to the obturator nerve would therefore directly affect the function of the adductor longus, leading to impaired thigh adduction.
*Obturator internus*
- The **obturator internus** muscle is innervated by the **nerve to obturator internus**, which arises from the sacral plexus (L5-S2).
- This nerve does not pass through the obturator foramen, making injury to this muscle unlikely in this specific scenario.
*Tensor fascia latae*
- The **tensor fascia latae** is innervated by the **superior gluteal nerve** (L4-S1).
- The superior gluteal nerve is located deeper in the gluteal region and does not traverse the obturator foramen.
*Semitendinosus*
- The **semitendinosus** is one of the hamstring muscles and is innervated by the **tibial division of the sciatic nerve** (L5-S2).
- The sciatic nerve is located posteriorly in the thigh and does not pass through the obturator foramen.
*Transversus abdominis*
- The **transversus abdominis** muscle is innervated by the **thoracoabdominal nerves** (T7-T11) and the **subcostal nerve** (T12).
- These nerves supply the abdominal wall and are anatomically distant from the obturator foramen, hence injury is not expected.
Stress urinary incontinence procedures US Medical PG Question 2: A 75-year-old woman presents to the physician with a complaint of a frequent need to void at nighttime, which has been disrupting her sleep. She notes embarrassingly that she is often unable to reach the bathroom in time, and experiences urinary leakage throughout the night as well as during the day. The patient undergoes urodynamic testing and a urinalysis is obtained which is normal. She is instructed by the physician to perform behavioral training to improve her bladder control. Which of the following is the most likely diagnosis contributing to this patient’s symptoms?
- A. Urinary tract infection
- B. Stress incontinence
- C. Urge incontinence (Correct Answer)
- D. Overflow incontinence
- E. Total incontinence
Stress urinary incontinence procedures Explanation: ***Urge incontinence***
- The patient's symptoms of a **frequent need to void**, inability to reach the bathroom in time (urgency), and **nocturnal leakage** (nocturia with incontinence) are classic for urge incontinence.
- This condition is characterized by **detrusor overactivity**, leading to sudden, strong urges to urinate that are difficult to defer.
*Urinary tract infection*
- While UTIs can cause urgency and frequency, the patient's **normal urinalysis** rules out an active infection as the cause of her symptoms.
- UTIs typically present with dysuria, hematuria, or suprapubic pain, which are not mentioned.
*Stress incontinence*
- This type of incontinence is characterized by **involuntary urine leakage with increased intra-abdominal pressure**, such as coughing, sneezing, or laughing.
- The patient's description of sudden urges and inability to reach the bathroom in time does not align with stress incontinence.
*Overflow incontinence*
- This condition is due to **incomplete bladder emptying**, leading to a constantly full bladder and continuous leakage.
- It often presents with weak stream, hesitancy, and a feeling of incomplete voiding, which are not described here.
*Total incontinence*
- Total incontinence involves the **continuous and unpredictable leakage** of urine, day and night, without any discernible pattern.
- While the patient experiences significant leakage, her symptoms point more specifically to the urge component rather than a complete absence of bladder control.
Stress urinary incontinence procedures US Medical PG Question 3: A 60-year-old, multiparous, woman comes to the physician because of urinary leakage for the past 4 months. She involuntarily loses a small amount of urine after experiencing a sudden, painful sensation in the bladder. She wakes up at night several times to urinate, and she sometimes cannot make it to the bathroom in time. She has diabetes mellitus type 2 controlled with insulin and a history of pelvic organ prolapse, for which she underwent surgical treatment 5 years ago. Menopause was 11 years ago. She drinks 4-5 cups of coffee daily. Pelvic examination shows no abnormalities, and a Q-tip test is negative. Ultrasound of the bladder shows a normal postvoid residual urine. Which of the following is the underlying cause of this patient's urinary incontinence?
- A. Decreased estrogen levels
- B. Decreased pelvic floor muscle tone
- C. Increased urine bladder volumes
- D. Increased detrusor muscle activity (Correct Answer)
- E. Recurrent pelvic organ prolapse
Stress urinary incontinence procedures Explanation: ***Increased detrusor muscle activity***
- The symptoms of **sudden, painful sensation** in the bladder, involuntary loss of urine, **nocturia**, and inability to reach the bathroom in time (urgency) are all classic signs of **urge incontinence**.
- **Urge incontinence** is primarily caused by **uninhibited contractions of the detrusor muscle**, often seen in conditions like **detrusor overactivity**.
*Decreased estrogen levels*
- While **estrogen deficiency** can contribute to **atrophic changes** in the genitourinary tract and predispose to urgency and incontinence, it's a general factor rather than the direct underlying cause of the *specific pattern* of uncontrolled detrusor contractions.
- The primary mechanism of urge incontinence is detrusor overactivity, not simply tissue changes due to estrogen loss, although estrogen can exacerbate symptoms.
*Decreased pelvic floor muscle tone*
- This is the primary cause of **stress urinary incontinence**, characterized by urine leakage with physical activity that increases intra-abdominal pressure (e.g., coughing, sneezing, lifting).
- The patient's symptoms do not align with stress incontinence, as her leakage is associated with a sudden urge, not physical exertion, and her **Q-tip test is negative**, ruling out significant urethral hypermobility.
*Increased urine bladder volumes*
- High bladder volumes can lead to **overflow incontinence** (leakage due to an overdistended bladder) or exacerbate urge symptoms, but the **normal postvoid residual urine** here indicates the bladder is emptying adequately and not chronically overfilled, ruling out overflow as the primary cause.
- Urge incontinence is characterized by frequency and urgency even at lower bladder volumes, due to the detrusor muscle's heightened responsiveness.
*Recurrent pelvic organ prolapse*
- The patient has a history of **pelvic organ prolapse (POP)** repaired 5 years ago, and the current **pelvic examination shows no abnormalities**, making recurrent prolapse unlikely to be the cause of her current symptoms.
- While POP can sometimes be associated with urinary symptoms (including urge incontinence via bladder neck kinking or trigone irritation), the absence of current prolapse on examination rules this out as the underlying cause.
Stress urinary incontinence procedures US Medical PG Question 4: A 63-year-old woman visits her family physician because she has been experiencing difficulty to get her urine stream started in the past 8 months with many occasions needing extra effort to pass the urine. She describes the stream as intermittent and slow, and comments that she needs to go to the restroom again immediately after urinating. Her personal medical history is negative for malignancies, and all of her cytologies have been reported as normal. The only medication she takes is an angiotensin receptor blocker to treat essential hypertension diagnosed 5 years ago. Physical examination is unremarkable except for herniation of the anterior wall of the vagina that goes beyond the hymen. Which of the following types of incontinence is affecting the patient?
- A. Overflow incontinence (Correct Answer)
- B. Functional incontinence
- C. Mixed incontinence
- D. Stress incontinence
- E. Urgency incontinence
Stress urinary incontinence procedures Explanation: ***Overflow incontinence***
- The patient's symptoms of **difficulty initiating a urine stream**, **intermittent and slow stream**, **needing extra effort to pass urine**, and **feeling the need to urinate again immediately after** are classic signs of **urinary retention** and **overflow incontinence**.
- The presence of an **anterior vaginal wall herniation beyond the hymen** suggests a significant cystocele, which can obstruct the bladder outlet, leading to chronic incomplete bladder emptying and overflow.
*Functional incontinence*
- This type of incontinence occurs when a person has **normal bladder control** but is unable to reach the toilet in time due to **physical or cognitive impairments**, such as mobility issues, dementia, or severe depression.
- The patient's presentation does not describe any such physical or cognitive limitations preventing her from accessing the toilet.
*Mixed incontinence*
- Mixed incontinence is characterized by the presence of **both stress and urgency incontinence symptoms**.
- While it's a common type, the patient's primary symptoms are more indicative of outlet obstruction and incomplete emptying, rather than involuntary leakage with exertion or a sudden, strong urge.
*Stress incontinence*
- **Stress incontinence** is defined by involuntary urine leakage that occurs with **physical exertion** such as coughing, sneezing, laughing, or lifting.
- The patient's symptoms are primarily related to difficulty voiding and incomplete emptying, not leakage during physical activity.
*Urgency incontinence*
- **Urgency incontinence** is characterized by a **sudden, strong, and uncontrollable urge to urinate** that leads to involuntary urine leakage.
- While the patient mentions needing to go to the restroom again, her main symptoms revolve around obstructive voiding and incomplete emptying, rather than uncontrollable urges.
Stress urinary incontinence procedures US Medical PG Question 5: A 19-year-old man is brought to the emergency department following a high-speed motor vehicle collision in which he was a restrained passenger. He complains of pelvic pain and urinary retention with overflow incontinence, along with associated lower extremity weakness. Examination shows perineal bruising and there is pain with manual compression of the pelvis. Injury to which of the following structures is most likely responsible for this patient's urinary incontinence?
- A. Ilioinguinal nerve
- B. Obturator nerve
- C. Genitofemoral nerve
- D. Pelvic splanchnic nerves (Correct Answer)
- E. Superior gluteal nerve
Stress urinary incontinence procedures Explanation: ***Pelvic splanchnic nerves***
- Urinary retention with overflow incontinence and lower extremity weakness following a pelvic trauma suggests damage to the **sacral spinal segments** or the **pelvic splanchnic nerves**.
- These nerves carry **parasympathetic fibers** that stimulate bladder contraction (detrusor muscle) and relaxation of the internal urethral sphincter, which are crucial for normal micturition.
*Ilioinguinal nerve*
- This nerve supplies sensory innervation to the **genitalia** and part of the inner thigh, and motor innervation to the internal oblique and transversus abdominis muscles.
- Damage to this nerve would primarily cause sensory deficits or abdominal muscle weakness, not urinary retention or lower extremity weakness.
*Obturator nerve*
- The obturator nerve primarily innervates the **adductor muscles of the thigh** and provides sensory innervation to the medial thigh.
- Injury would result in difficulty with hip adduction and sensory loss in the medial thigh, not bladder dysfunction or diffuse lower extremity weakness.
*Genitofemoral nerve*
- This nerve provides sensory innervation to the **anterior compartment of the thigh** and the external genitalia, and motor innervation to the cremaster muscle.
- Damage would typically manifest as altered sensation in these areas or an absent cremasteric reflex, without directly affecting bladder function.
*Superior gluteal nerve*
- The superior gluteal nerve innervates the **gluteus medius, gluteus minimus, and tensor fasciae latae muscles**, which are crucial for hip abduction and stabilization during walking.
- Injury would lead to a characteristic **Trendelenburg gait**, but would not directly cause urinary incontinence or retention.
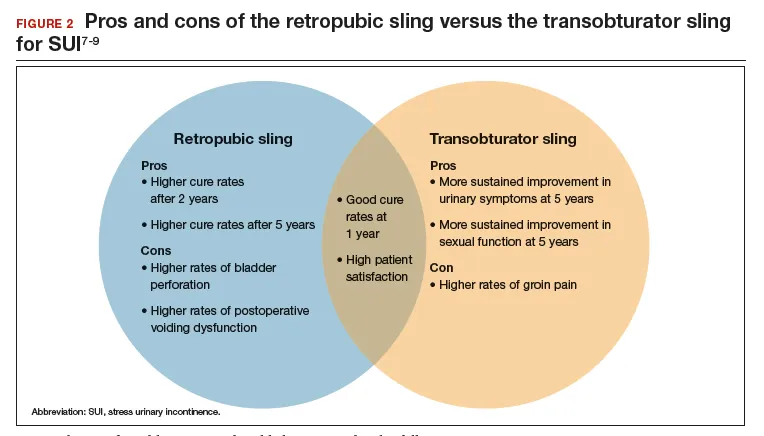
Stress urinary incontinence procedures US Medical PG Question 6: A 40-year-old gravida 4 para 2 woman presents with urinary incontinence requesting definitive treatment. She started experiencing urinary incontinence when coughing, laughing, or exercising about three months ago. Symptoms have not improved with behavioral changes or Kegel exercises. Past medical history is significant for her last pregnancy which was complicated by an arrest of descent and a grade 3 episiotomy. She currently takes no medications. A review of systems is significant for constipation for the last few months. Rectal and vaginal exams are normal. Which of the following is the mechanism that underlies the best course of treatment for this patient?
- A. Anatomic elevation of the urethra (Correct Answer)
- B. Oral estrogen therapy
- C. Reduction of detrusor muscle tone
- D. Dilation of a urethral or ureteral stricture
- E. Inhibition of DNA gyrase and topoisomerase
Stress urinary incontinence procedures Explanation: ***Anatomic elevation of the urethra***
- This patient presents with symptoms highly suggestive of **stress urinary incontinence (SUI)**, characterized by leakage with coughing, laughing, or exercise, which is often caused by urethral hypermobility and **pelvic floor weakness** following childbirth trauma.
- SUI that is refractory to conservative management (behavioral changes, Kegel exercises) often requires surgical intervention, such as a **mid-urethral sling**, which functions by providing sub-urethral support and elevating the urethra to prevent leakage.
*Oral estrogen therapy*
- **Estrogen therapy** is primarily used to treat atrophic vaginitis, which can contribute to urgency and frequency, but it is not a definitive treatment for **stress urinary incontinence** caused by anatomical defects.
- It works by restoring the health of the vaginal and urethral mucosa, but does not address the lack of structural support in SUI.
*Reduction of detrusor muscle tone*
- **Reduction of detrusor tone** with anticholinergic medications or beta-3 agonists is the primary treatment for **urge urinary incontinence (UUI)**, which involves involuntary bladder contractions.
- The patient's symptoms (leakage with exertion) are classic for SUI, not UUI.
*Dilation of a urethral or ureteral stricture*
- **Urethral strictures** cause obstructive voiding symptoms such as weak stream, straining, and incomplete emptying, rather than stress incontinence.
- While urinary tract symptoms could mimic incontinence, dilation is not an effective treatment for the type of incontinence described.
*Inhibition of DNA gyrase and topoisomerase*
- **Inhibition of DNA gyrase and topoisomerase** is the mechanism of action for **fluoroquinolone antibiotics**, which are used to treat bacterial infections.
- This mechanism is completely unrelated to the treatment of urinary incontinence, which is a structural and functional issue of the bladder and urethra, not an infection.
Stress urinary incontinence procedures US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Stress urinary incontinence procedures Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Stress urinary incontinence procedures US Medical PG Question 8: Four hours after undergoing an abdominal hysterectomy, a 43-year-old woman is evaluated in the post-anesthesia care unit because she has only had a urine output of 5 mL of blue-tinged urine since surgery. The operation went smoothly and ureter patency was checked via retrograde injection of methylene blue dye mixed with saline through the Foley catheter. She received 2.4 L of crystalloid fluids intraoperatively and urine output was 1.2 L. She had a history of fibroids with painful and heavy menses. She is otherwise healthy. She underwent 2 cesarean sections 8 and 5 years ago, respectively. Her temperature is 37.4°C (99.3°F), pulse is 75/min, respirations are 16/min, and blood pressure is 122/76 mm Hg. She appears comfortable. Cardiopulmonary examination shows no abnormalities. There is a midline surgical incision with clean and dry dressings. Her abdomen is soft and mildly distended in the lower quadrants. Her bladder is slightly palpable. Extremities are warm and well perfused, and capillary refill is brisk. Laboratory studies show:
Leukocyte count 8,300/mm3
Hemoglobin 10.3 g/dL
Hematocrit 31%
Platelet count 250,000/mm3
Serum
_Na+ 140 mEq/L
_K+ 4.2 mEq/L
_HCO3+ 26 mEq/L
_Urea nitrogen 26 mg/dL
_Creatinine 1.0 mg/dL
Urine
_Blood 1+
_WBC none
_Protein negative
_RBC none
_RBC casts none
A bladder scan shows 250 mL of retained urine. Which of the following is the next best step in the evaluation of this patient?
- A. Check the Foley catheter (Correct Answer)
- B. Return to the operating room for emergency surgery
- C. Perform ultrasound of the kidneys
- D. Administer 20 mg of IV furosemide
- E. Administer bolus 500 mL of Lactated Ringers
Stress urinary incontinence procedures Explanation: ***Check the Foley catheter***
- This patient presents with signs of **urinary retention** (low urine output, palpable bladder, retained urine on bladder scan) despite methylene blue injection confirming ureter patency. The most common and easily reversible cause of low urine output post-hysterectomy is a **kinked or obstructed Foley catheter**.
- Given the smooth intraoperative course and adequate urine output during surgery, a quick check and potential **repositioning or flushing of the catheter** is the immediate and most appropriate first step before considering more invasive interventions.
*Return to the operating room for emergency surgery*
- This is a drastic step and is not indicated at this stage. There is no evidence of a **surgical complication** requiring emergency intervention, such as a ureteral injury (which was checked intraoperatively) or active hemorrhage.
- The patient's vital signs are stable, and she appears comfortable, which makes an emergency surgical re-exploration highly unlikely as the initial best step.
*Perform ultrasound of the kidneys*
- While a renal ultrasound can assess for **hydronephrosis** or other kidney abnormalities, it is a delayed step. Given the clear evidence of bladder retention and the possibility of a simple catheter malfunction, performing an ultrasound without first addressing the catheter would be premature.
- The patient's **creatinine is normal**, making acute kidney injury due to obstruction less likely as an immediate concern.
*Administer 20 mg of IV furosemide*
- Furosemide is a **loop diuretic** that increases urine production. However, it would be ineffective and potentially harmful if the issue is a mechanical obstruction of urine outflow, as appears to be the case here.
- Administering a diuretic without addressing the outflow problem would only worsen bladder distension and potentially stress the renal system without resolving the underlying issue.
*Administer bolus 500 mL of Lactated Ringers*
- This patient has already received 2.4 L of crystalloid fluids intraoperatively and has stable vital signs, indicating she is likely **euvolemic**.
- Giving another fluid bolus would not address the observed urinary retention and could lead to **fluid overload** if the urine outflow obstruction persists.
Stress urinary incontinence procedures US Medical PG Question 9: A 56-year-old man is brought to the emergency department 25 minutes after he was involved in a high-speed motor vehicle collision where he was the unrestrained passenger. He has severe lower abdominal and pelvic pain. On arrival, he is alert and oriented. His pulse is 95/min, respirations are 22/min, and blood pressure is 106/62 mm Hg. Examination shows severe tenderness to palpation over the lower abdomen and over the left anterior superior iliac spine. There is no limb length discrepancy. Application of downward pressure over the pelvis shows no springy resistance or instability. Rectal examination is unremarkable. A focused assessment with sonography shows no free fluid in the abdomen. There is no blood at the urethral meatus. Placement of a Foley catheter shows gross hematuria. An x-ray of the pelvis shows a fracture of the left pelvic edge. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. External fixation of the pelvis
- C. Cystoscopy
- D. Retrograde urethrography
- E. Retrograde cystography (Correct Answer)
Stress urinary incontinence procedures Explanation: ***Retrograde cystography***
- The presence of **gross hematuria** in a patient with a **pelvic fracture** necessitates ruling out **bladder injury**. A retrograde cystography directly visualizes the bladder and can detect extravasation of contrast if a bladder rupture is present.
- This imaging study specifically investigates the bladder using retrograde contrast filling, which is crucial for diagnosing **intraperitoneal** or **extraperitoneal bladder rupture**.
*Intravenous pyelography*
- This study evaluates the **kidneys** and **ureters** for injury, but the primary concern with gross hematuria and pelvic fracture is the bladder.
- An IV pyelogram provides less detailed imaging of the bladder compared to a retrograde cystogram and is less effective for detecting bladder rupture.
*External fixation of the pelvis*
- While the patient has a pelvic fracture, the immediate priority in a hemodynamically stable patient with gross hematuria is to identify and manage potential **life-threatening urologic injuries** before definitive orthopedic repair.
- **Pelvic external fixation** is primarily indicated for **unstable pelvic fractures** or those causing significant hemorrhage, neither of which is explicitly described as an immediate concern requiring intervention before urologic evaluation.
*Cystoscopy*
- **Cystoscopy** is an endoscopic procedure that allows direct visualization of the bladder's interior. While it can identify bladder injuries, it is generally considered after imaging studies like **retrograde cystography** to confirm findings or address specific issues like clot evacuation or stent placement.
- The initial diagnostic step should focus on assessing for rupture via contrast study, which is often less invasive than a direct endoscopic procedure in the acute trauma setting.
*Retrograde urethrography*
- **Retrograde urethrography (RUG)** is used to evaluate for **urethral injury**, especially when there is blood at the urethral meatus, a high-riding prostate, or an inability to pass a Foley catheter.
- The patient's Foley catheter was successfully placed, and there was **no blood at the urethral meatus**, making urethral injury less likely and thus RUG a lower priority as the initial step compared to assessing for bladder injury.
Stress urinary incontinence procedures US Medical PG Question 10: A 22-year-old man is rushed to the emergency department after a motor vehicle accident. The patient states that he feels weakness and numbness in both of his legs. He also reports pain in his lower back. His airway, breathing, and circulation is intact, and he is conversational. Neurologic exam is significant for bilateral lower extremity flaccid paralysis and impaired pain and temperature sensation up to T10-T11 with normal vibration sense. A computerized tomography scan of the spine is performed which shows a vertebral burst fracture of the vertebral body at the level of T11. Which of the following findings is most likely present in this patient?
- A. Intact vibration sense
- B. Bowel incontinence (Correct Answer)
- C. Flaccid paralysis at the level of the lesion
- D. Spasticity below the lesion
- E. Impaired proprioception sense
Stress urinary incontinence procedures Explanation: ***Bowel incontinence***
- The presented symptoms of acute **bilateral lower extremity flaccid paralysis**, **impaired pain and temperature sensation**, and a T11 **vertebral burst fracture** are highly indicative of **anterior cord syndrome**.
- **Anterior cord syndrome** characteristically involves damage to the **anterior two-thirds of the spinal cord**, affecting the **corticospinal tracts** (motor control), **spinothalamic tracts** (pain and temperature sensation), and the **autonomic fibers** that control bladder and bowel function, leading to **bowel and bladder dysfunction**.
*Intact vibration sense*
- The sensation of **vibration** and **proprioception** is carried by the **dorsal columns** (posterior part of the spinal cord), which are typically **spared** in **anterior cord syndrome**.
- Therefore, **intact vibration sense** is an expected finding, but the question asks for the **most likely finding** that represents a significant complication of the syndrome.
*Flaccid paralysis at the level of the lesion*
- While **flaccid paralysis** is present in the lower extremities, it occurs **below the level of the lesion** due to damage to the descending motor tracts (corticospinal tracts).
- Flaccid paralysis *at* the level of the lesion would typically involve damage to the **lower motor neurons** at that specific segment, which is not the primary feature described for a burst fracture causing **anterior cord syndrome**.
*Spasticity below the lesion*
- **Spasticity** typically develops much **later** in spinal cord injuries, after the initial phase of **spinal shock** resolves (usually weeks to months).
- In the acute phase following a significant spinal cord injury, **flaccid paralysis** is the more common finding below the lesion, reflecting spinal shock.
*Impaired proprioception sense*
- Similar to vibration sense, **proprioception** is primarily mediated by the **dorsal columns**, which are generally **spared** in **anterior cord syndrome**.
- Therefore, **proprioception** would likely be **intact**, not impaired, in this specific type of spinal cord injury.
More Stress urinary incontinence procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.