Pelvic organ prolapse repair US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pelvic organ prolapse repair. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pelvic organ prolapse repair US Medical PG Question 1: A 57-year-old, multiparous, woman comes to the physician because of urinary leakage for the past 6 months. She involuntarily loses a small amount of urine after experiencing a sudden, painful sensation in the bladder. She has difficulty making it to the bathroom in time, and feels nervous when there is no bathroom nearby. She also started having to urinate at night. She does not have hematuria, abdominal pain, or pelvic pain. She has insulin-dependent diabetes mellitus type 2, and underwent surgical treatment for symptomatic pelvic organ prolapse 3 years ago. Menopause was 6 years ago, and she is not on hormone replacement therapy. She works as an administrative manager, and drinks 3–4 cups of coffee daily at work. On physical examination, there is no suprapubic tenderness. Pelvic examination shows no abnormalities and Q-tip test was negative. Ultrasound of the bladder shows a normal post-void residual urine. Which of the following is the primary underlying etiology for this patient's urinary incontinence?
- A. Increased urine bladder volumes
- B. Increased detrusor muscle activity (Correct Answer)
- C. Recurrent pelvic organ prolapse
- D. Trauma to urinary tract
- E. Decreased pelvic floor muscle tone
Pelvic organ prolapse repair Explanation: ***Increased detrusor muscle activity***
- The patient's symptoms of **sudden, painful sensation in the bladder**, involuntary urine loss, difficulty making it to the bathroom ("** बाथरूम-hopping**"), and **nocturia** are classic for **urge incontinence**.
- **Urge incontinence** is primarily caused by **uninhibited contractions of the detrusor muscle**, often due to **detrusor overactivity**. Her caffeine intake and history of diabetes can exacerbate this condition.
*Increased urine bladder volumes*
- While increased urine volume can exacerbate incontinence, it's typically associated with **overflow incontinence** (constant dribbling due to an overfilled bladder) or **polyuria** (excessive urine production), neither of which are suggested as the primary cause of her specific symptoms.
- The post-void residual urine is normal, ruling out significant retention that would lead to chronically increased bladder volumes from incomplete emptying.
*Recurrent pelvic organ prolapse*
- Pelvic organ prolapse can contribute to **stress incontinence** or **obstructive symptoms**, but her current pelvic exam shows no abnormalities, and she recently underwent surgery for this, making it less likely to be the primary cause of her current symptoms.
- Her symptoms of **urgency and nocturia** are not typical presentations of prolapse-related incontinence.
*Trauma to urinary tract*
- Trauma to the urinary tract would typically present with symptoms such as **hematuria**, **pain**, or difficulty voiding, none of which are reported in this case.
- There is no history of recent trauma or procedures that would directly lead to her current symptoms of urge incontinence.
*Decreased pelvic floor muscle tone*
- **Decreased pelvic floor muscle tone** is the primary cause of **stress incontinence**, characterized by urine leakage with increased intra-abdominal pressure (e.g., coughing, sneezing).
- Her symptoms are of **urgency and involuntary loss of urine** after a sudden sensation, which is distinct from stress incontinence, and her negative Q-tip test suggests good urethral support.
Pelvic organ prolapse repair US Medical PG Question 2: A 37-year-old woman presents with an inability to void in the hours after giving birth to her first child via vaginal delivery. Her delivery involved the use of epidural anesthesia as well as pelvic trauma from the use of forceps. She is currently experiencing urinary leakage and complains of increased lower abdominal pressure. Which of the following is the most appropriate treatment for this patient’s condition?
- A. Pessary insertion
- B. Pelvic floor muscle strengthening
- C. Antimuscarinic drugs
- D. Midurethral sling
- E. Urethral catheterization (Correct Answer)
Pelvic organ prolapse repair Explanation: ***Urethral catheterization***
- The patient is experiencing **postpartum urinary retention** (inability to void) and **overflow incontinence** (urinary leakage due to bladder overdistension), alongside increased lower abdominal pressure, all indicative of an overfilled bladder.
- **Urethral catheterization** is the most appropriate immediate treatment to relieve bladder distension, prevent kidney damage, and allow bladder recovery.
*Pessary insertion*
- **Pessaries** are used for pelvic organ prolapse or stress urinary incontinence, not for acute postpartum urinary retention.
- They provide structural support but do not address the inability to void in an overdistended bladder.
*Pelvic floor muscle strengthening*
- **Pelvic floor exercises** are beneficial for stress incontinence or mild degrees of prolapse.
- They are contraindicated in acute urinary retention as they may worsen the inability to void if the issue is a failure of bladder contractility or urethral relaxation.
*Antimuscarinic drugs*
- **Antimuscarinics** relax the detrusor muscle and are used to treat overactive bladder symptoms (e.g., urgency, frequency).
- They would worsen bladder emptying in a patient with urinary retention.
*Midurethral sling*
- A **midurethral sling** is a surgical procedure for stress urinary incontinence.
- It is an invasive treatment for a chronic condition and is not appropriate for acute postpartum urinary retention.
Pelvic organ prolapse repair US Medical PG Question 3: A 36-year-old woman comes to the physician for a 2-month history of urinary incontinence and a vaginal mass. She has a history of five full-term normal vaginal deliveries. She gave birth to a healthy newborn 2-months ago. Since then she has felt a sensation of vaginal fullness and a firm mass in the lower vagina. She has loss of urine when she coughs, sneezes, or exercises. Pelvic examination shows an irreducible pink globular mass protruding out of the vagina. A loss of integrity of which of the following ligaments is most likely involved in this patient's condition?
- A. Infundibulopelvic ligament
- B. Broad ligament of the uterus
- C. Cardinal ligament of the uterus (Correct Answer)
- D. Round ligament of uterus
- E. Uterosacral ligament
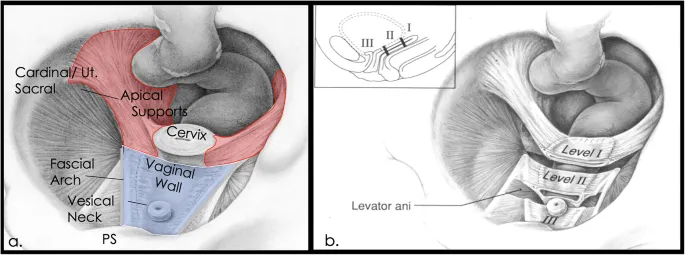
Pelvic organ prolapse repair Explanation: ***Cardinal ligament of the uterus***
- The patient's symptoms, including **vaginal mass**, **urinary incontinence** with coughing/sneezing, and history of **multiple vaginal deliveries**, strongly suggest **uterine prolapse**.
- The cardinal ligaments are crucial in providing **lateral cervical support** and are often damaged during childbirth, leading to uterine descent.
*Infundibulopelvic ligament*
- This ligament primarily supports the **ovaries** and contains the **ovarian artery** and vein.
- Damage to this ligament is associated with ovarian prolapse or complications during oophorectomy, not uterine prolapse.
*Broad ligament of the uterus*
- The broad ligament is a **peritoneal fold** that drapes over the uterus, fallopian tubes, and ovaries.
- While it helps to hold these structures in place, its primary role is not in preventing uterine prolapse; it mainly provides a medium for neurovascular structures.
*Round ligament of uterus*
- The round ligament extends from the uterus to the **labia majora** and primarily helps maintain **anteversion** of the uterus.
- It plays a minor role in uterine support and its laxity is not a primary cause of uterine prolapse.
*Uterosacral ligament*
- The uterosacral ligaments provide **posterior support** to the uterus, particularly by anchoring the cervix to the sacrum.
- While damage to these ligaments contributes to **apical prolapse**, the cardinal ligaments are more critical for lateral support and more commonly implicated in overall uterine prolapse following childbirth.
Pelvic organ prolapse repair US Medical PG Question 4: A 61-year-old G4P3 presents with a 5-year history of involuntary urine loss on coughing, sneezing, and physical exertion. She denies urine leakage at night. She has been menopausal since 51 years of age. She is otherwise healthy and is not on any medications, including hormone replacement therapy. The weight is 78 kg (172 lb) and the height is 156 cm (5.1 ft). The vital signs are within normal limits. The physical examination shows no costovertebral angle tenderness. The neurologic examination is unremarkable. The gynecologic examination revealed pale and thin vulvar and vaginal mucosa. The external urethral opening appears normal; there is urine leakage when the patient is asked to cough. The Q-tip test is positive. The bimanual exam reveals painless bulging of the anterior vaginal wall. Which of the following findings are most likely to be revealed by cystometry?
- A. Increased residual volume, involuntary detrusor contractions on maximal bladder filling
- B. Normal residual volume, no involuntary detrusor contractions (Correct Answer)
- C. Normal residual volume, involuntary detrusor contractions on minimal bladder filling
- D. Normal residual volume, involuntary detrusor contractions on maximal bladder filling
- E. Increased residual volume, no involuntary detrusor contractions
Pelvic organ prolapse repair Explanation: ***Normal residual volume, no involuntary detrusor contractions***
- The patient's symptoms (involuntary urine loss on coughing, sneezing, and physical exertion, denial of nocturnal leakage) are classic for **stress urinary incontinence (SUI)**. SUI is due to **urethral hypermobility** or intrinsic sphincter deficiency, not detrusor overactivity, hence *no involuntary detrusor contractions*.
- **Normal residual volume** is expected in SUI as the bladder empties appropriately; the issue is with urethral support during increased intra-abdominal pressure.
*Increased residual volume, involuntary detrusor contractions on maximal bladder filling*
- **Increased residual volume** is not typical in pure SUI and might suggest bladder outlet obstruction or an underactive detrusor.
- **Involuntary detrusor contractions** indicate **urge incontinence** or overactive bladder, which is inconsistent with the patient's presentation of leakage only with exertion and no nocturnal symptoms.
*Normal residual volume, involuntary detrusor contractions on minimal bladder filling*
- While **normal residual volume** is consistent, **involuntary detrusor contractions** at *minimal* bladder filling are characteristic of a severely overactive bladder or neurogenic bladder, which is not suggested by the patient's symptoms (leakage only with exertion).
*Normal residual volume, involuntary detrusor contractions on maximal bladder filling*
- **Involuntary detrusor contractions**, even at maximal filling, are a feature of **detrusor overactivity**, leading to **urge incontinence**. This pattern of leakage is unrelated to the patient's reported stress-related symptoms.
*Increased residual volume, no involuntary detrusor contractions*
- **Increased residual volume** without involuntary detrusor contractions could point towards **bladder outlet obstruction** or **detrusor underactivity**. Neither of these conditions typically presents with urine leakage exclusively upon coughing, sneezing, or exertion.
Pelvic organ prolapse repair US Medical PG Question 5: A 63-year-old woman visits her family physician because she has been experiencing difficulty to get her urine stream started in the past 8 months with many occasions needing extra effort to pass the urine. She describes the stream as intermittent and slow, and comments that she needs to go to the restroom again immediately after urinating. Her personal medical history is negative for malignancies, and all of her cytologies have been reported as normal. The only medication she takes is an angiotensin receptor blocker to treat essential hypertension diagnosed 5 years ago. Physical examination is unremarkable except for herniation of the anterior wall of the vagina that goes beyond the hymen. Which of the following types of incontinence is affecting the patient?
- A. Overflow incontinence (Correct Answer)
- B. Functional incontinence
- C. Mixed incontinence
- D. Stress incontinence
- E. Urgency incontinence
Pelvic organ prolapse repair Explanation: ***Overflow incontinence***
- The patient's symptoms of **difficulty initiating a urine stream**, **intermittent and slow stream**, **needing extra effort to pass urine**, and **feeling the need to urinate again immediately after** are classic signs of **urinary retention** and **overflow incontinence**.
- The presence of an **anterior vaginal wall herniation beyond the hymen** suggests a significant cystocele, which can obstruct the bladder outlet, leading to chronic incomplete bladder emptying and overflow.
*Functional incontinence*
- This type of incontinence occurs when a person has **normal bladder control** but is unable to reach the toilet in time due to **physical or cognitive impairments**, such as mobility issues, dementia, or severe depression.
- The patient's presentation does not describe any such physical or cognitive limitations preventing her from accessing the toilet.
*Mixed incontinence*
- Mixed incontinence is characterized by the presence of **both stress and urgency incontinence symptoms**.
- While it's a common type, the patient's primary symptoms are more indicative of outlet obstruction and incomplete emptying, rather than involuntary leakage with exertion or a sudden, strong urge.
*Stress incontinence*
- **Stress incontinence** is defined by involuntary urine leakage that occurs with **physical exertion** such as coughing, sneezing, laughing, or lifting.
- The patient's symptoms are primarily related to difficulty voiding and incomplete emptying, not leakage during physical activity.
*Urgency incontinence*
- **Urgency incontinence** is characterized by a **sudden, strong, and uncontrollable urge to urinate** that leads to involuntary urine leakage.
- While the patient mentions needing to go to the restroom again, her main symptoms revolve around obstructive voiding and incomplete emptying, rather than uncontrollable urges.
Pelvic organ prolapse repair US Medical PG Question 6: A 66-year-old G3P3 presents with an 8-year-history of back pain, perineal discomfort, difficulty urinating, recurrent malaise, and low-grade fevers. These symptoms have recurred regularly for the past 5–6 years. She also says that there are times when she experiences a feeling of having a foreign body in her vagina. With the onset of symptoms, she was evaluated by a physician who prescribed her medications after a thorough examination and recommended a vaginal pessary, but she was non-compliant. She had 3 vaginal deliveries She has been menopausal since 51 years of age. She does not have a history of malignancies or cardiovascular disease. She has type 2 diabetes mellitus that is controlled with diet and metformin. Her vital signs include: blood pressure 110/60 mm Hg, heart rate 91/min, respiratory rate 13/min, and temperature 37.4℃ (99.3℉). On physical examination, there is bilateral costovertebral angle tenderness. The urinary bladder is non-palpable. The gynecologic examination reveals descent of the cervix to the level of the introitus. A Valsalva maneuver elicits uterine procidentia. Which pathology is most likely to be revealed by imaging in this patient?
- A. Renal cyst
- B. Urinary bladder polyp
- C. Renal tumor
- D. Hydronephrosis (Correct Answer)
- E. Renal calculi
Pelvic organ prolapse repair Explanation: ***Hydronephrosis***
- The patient's **uterine procidentia** (third-degree uterine prolapse) can lead to **ureteral kinking** or compression, causing obstruction of urine flow.
- This obstruction, combined with recurrent back pain, malaise, low-grade fevers, and CVA tenderness, strongly suggests **hydronephrosis** due to urinary stasis and potential recurrent UTIs.
*Renal cyst*
- While common, renal cysts are typically **asymptomatic** and do not explain the recurrent fevers, malaise, and CVA tenderness.
- They are generally **not associated with urinary obstruction** leading to such systemic symptoms.
*Urinary bladder polyp*
- Bladder polyps can cause hematuria or urinary frequency but are **unlikely to cause bilateral CVA tenderness**, back pain, or systemic symptoms like fever and malaise.
- They do not typically lead to **ureteral obstruction** or hydronephrosis.
*Renal tumor*
- A renal tumor could explain systemic symptoms like malaise and low-grade fevers, but the recurrent nature over 5-6 years and the strong association with **uterine prolapse-induced obstruction** make it less likely.
- While it can cause back pain, **bilateral CVA tenderness** and difficulty urinating are not classic presenting features.
*Renal calculi*
- Renal calculi cause **severe, colicky flank pain** that radiates, and while they can cause urinary obstruction and recurrent UTIs, the patient's long-standing, constant back pain and the context of significant **uterine prolapse** make hydronephrosis a more direct consequence.
- The symptoms described are more indicative of **chronic obstruction** rather than acute stone passage.
Pelvic organ prolapse repair US Medical PG Question 7: A 45-year-old man undergoes elective vasectomy for permanent contraception. The procedure is performed under local anesthesia. There are no intra-operative complications and he is discharged home with ibuprofen for post-operative pain. This patient is at increased risk for which of the following complications?
- A. Prostatitis
- B. Seminoma
- C. Testicular torsion
- D. Sperm granuloma (Correct Answer)
- E. Inguinal hernia
Pelvic organ prolapse repair Explanation: **Sperm granuloma**
- A **sperm granuloma** can occur after vasectomy due to the extravasation of sperm from the severed vas deferens, leading to a foreign body granulomatous reaction.
- This complication presents as a **palpable, tender nodule** at the vasectomy site and is a relatively common long-term issue.
*Prostatitis*
- **Prostatitis** is an inflammation of the prostate gland, and there is no direct mechanistic link or increased risk following a vasectomy.
- It is typically caused by bacterial infection or non-infectious inflammatory processes, unrelated to the **vas deferens** ligation.
*Seminoma*
- **Seminoma** is a type of testicular germ cell tumor, and extensive research has shown no increased risk of developing testicular cancer after vasectomy.
- The procedure does not alter the cellular processes or environment within the testicles that predispose to germ cell tumor formation.
*Testicular torsion*
- **Testicular torsion** is a urological emergency involving the twisting of the spermatic cord, which cuts off blood supply to the testis.
- This condition is not associated with vasectomy; it typically occurs due to an anatomical abnormality (e.g., **bell-clapper deformity**) or trauma.
*Inguinal hernia*
- An **inguinal hernia** is a protrusion of abdominal contents through a weakness in the abdominal wall, specifically in the inguinal canal.
- Vasectomy is a superficial procedure that does not involve manipulating or weakening the abdominal wall in a way that would increase the risk of an inguinal hernia.
Pelvic organ prolapse repair US Medical PG Question 8: A previously healthy 20-year-old woman comes to her physician because of pain during sexual intercourse. She recently became sexually active with her boyfriend. She has had no other sexual partners. She is frustrated because she has consistently been experiencing a severe, sharp vaginal pain on penetration. She has tried lubricants without significant relief. She has not been able to use tampons in the past due to similar pain with tampon insertion. External vulvar examination shows no abnormalities. She is unable to undergo a bimanual or speculum exam due to intracoital pain with attempted digit or speculum insertion. Testing for Chlamydia trachomatis and Neisseria gonorrhoeae is negative. Which of the following is the best next step in management?
- A. Sex psychotherapy
- B. Lorazepam
- C. Vaginal estrogen cream
- D. Vaginal Botox injections
- E. Pelvic floor physical therapy (Correct Answer)
Pelvic organ prolapse repair Explanation: ***Pelvic floor physical therapy***
- This patient's symptoms of **severe, sharp vaginal pain on penetration (dyspareunia)**, inability to use tampons, and pain during attempted gynecological exams are classic for **vaginismus**, a type of **genito-pelvic pain/penetration disorder**.
- **Pelvic floor physical therapy** is the **first-line treatment** for vaginismus, as it aims to relax and desensitize the hypertonic and painful pelvic floor muscles.
*Sex psychotherapy*
- While psychological factors often contribute to and are exacerbated by vaginismus, **psychotherapy alone is typically not sufficient** as a primary treatment for the physical muscular spasm and pain.
- It may be a useful adjunct to address anxiety, fear, or relationship issues, but it does not directly treat the **hypertonicity of the pelvic floor muscles**.
*Lorazepam*
- **Lorazepam is an anxiolytic** and could potentially help with anxiety related to sexual activity, but it does not directly address the **localized muscular spasm** causing vaginismus.
- Using systemic sedatives for localized pain is **not a targeted or appropriate primary treatment** for this condition.
*Vaginal estrogen cream*
- **Vaginal estrogen cream** is used to treat **atrophic vaginitis**, which is characterized by vaginal dryness, thinning of vaginal tissue, and pain, typically in **postmenopausal women** or those with estrogen deficiency.
- This young, previously healthy 20-year-old woman is unlikely to have **vaginal atrophy**, and her symptoms of pain with tampon insertion predate sexual activity.
*Vaginal Botox injections*
- **Botox (botulinum toxin)** injections into the pelvic floor muscles can be used in **refractory cases of vaginismus** after failure of conservative treatments like physical therapy.
- It is an **invasive and second-line option**, not the best initial step for a newly diagnosed case.
Pelvic organ prolapse repair US Medical PG Question 9: A 63-year-old woman presents to her primary care doctor with increased urinary frequency. She has noticed that over the past 6 months, she has had to urinate more often than usual. Several times per day, she develops a rapid-onset need to urinate and has occasionally been unable to reach the restroom. These symptoms have caused her a lot of distress and impacted her work as a grocery store clerk. She has tried pelvic floor exercises, decreasing her caffeine consumption, and has intentionally lost 20 pounds in an effort to alleviate her symptoms. She denies urinary hesitancy or hematuria. Her past medical history is notable for rheumatoid arthritis for which she takes methotrexate. She does not smoke or drink alcohol. Her temperature is 98.8°F (37.1°C), blood pressure is 124/68 mmHg, pulse is 89/min, and respirations are 19/min. She is well-appearing and in no acute distress. Which of the following interventions would be most appropriate in this patient?
- A. Intermittent catheterization
- B. Tamsulosin
- C. Topical estrogen
- D. Pessary placement
- E. Oxybutynin (Correct Answer)
Pelvic organ prolapse repair Explanation: ***Oxybutynin***
- The patient presents with classic symptoms of **overactive bladder**, including increased urinary frequency, urgency, and urge incontinence, which have not responded to behavioral modifications. Oxybutynin is an **antimuscarinic medication** that relaxes the detrusor muscle, reducing bladder spasms and urgency.
- This medication is a **first-line pharmacological treatment** for overactive bladder syndrome after conservative therapies have failed, making it the most appropriate intervention given her symptoms and history.
*Intermittent catheterization*
- This intervention is primarily used for **urinary retention** or significant **post-void residual volume**, which are not indicated by the patient's symptoms (she denies urinary hesitancy).
- Her symptoms are consistent with bladder overactivity, not an inability to empty her bladder, so catheterization would be inappropriate and potentially harmful.
*Tamsulosin*
- Tamsulosin is an **alpha-1 adrenergic blocker** typically used to treat symptoms of **benign prostatic hyperplasia (BPH)** in men by relaxing smooth muscle in the prostate and bladder neck.
- It is not indicated for overactive bladder in women and would not address her primary symptoms of frequency and urgency.
*Topical estrogen*
- Topical estrogen can be beneficial for **urogenital atrophy** in postmenopausal women, which can contribute to urinary symptoms, particularly stress incontinence or dysuria.
- While she is a 63-year-old woman, her symptoms are clearly indicative of **urge incontinence** and overactive bladder, which are less likely to be solely improved by estrogen, especially given the severity and associated urgency.
*Pessary placement*
- Pessaries are used for **pelvic organ prolapse** or **stress urinary incontinence** to provide structural support or compress the urethra.
- The patient's primary complaint is **urge incontinence** and overactive bladder symptoms, not prolapse or stress incontinence, making a pessary an unsuitable intervention.
Pelvic organ prolapse repair US Medical PG Question 10: A 77-year-old woman, gravida 2, para 2, is brought to the physician by staff of the nursing home where she resides because of involuntary loss of urine and increased frequency of urination over the past 2 weeks. She reports that she has very little time to get to the bathroom after feeling the urge to urinate. “Accidents” have occurred 4–6 times a day during this period. She has never had urinary incontinence before. She has also been more tired than usual. She drinks 3 cups of coffee daily. Her last menstrual period was 15 years ago. She takes no medications. Vital signs are within normal limits. The abdomen is soft and nontender. Pelvic examination shows a normal-appearing vagina and cervix; uterus and adnexa are small. Which of the following is the most appropriate next step in management?
- A. Vaginal estrogen cream
- B. Urinalysis and culture (Correct Answer)
- C. Pad test
- D. MRI of the pelvis
- E. Caffeine abstinence
Pelvic organ prolapse repair Explanation: **Urinalysis and culture**
- The sudden onset of **urinary incontinence** and **increased frequency** in an elderly woman, especially without prior history, strongly suggests a **urinary tract infection (UTI)**.
- UTIs are common in elderly individuals and can present atypically with incontinence, confusion, or increased fatigue, requiring **urinalysis** to detect infection and **culture** for pathogen identification and antibiotic susceptibility.
*Vaginal estrogen cream*
- This treatment is primarily for **atrophic vaginitis** and associated **urge or stress incontinence** due to estrogen deficiency, which develops gradually over time.
- The patient's symptoms are of **acute onset**, which makes **atrophy** less likely to be the primary cause of this sudden change.
*Pad test*
- A pad test quantifies the amount of urine leakage over a specific period and is used to assess the **severity of incontinence**.
- While it helps in characterizing incontinence, it does not identify the **underlying cause** of new-onset symptoms, particularly in the context of possible infection.
*MRI of the pelvis*
- This imaging study would be considered for evaluating **structural abnormalities** or **neurological causes** of incontinence, such as masses or nerve compression.
- Given the acute onset of symptoms suggestive of infection, a less invasive and more direct diagnostic approach, like urinalysis, is warranted first.
*Caffeine abstinence*
- **Caffeine** is a **bladder irritant** and **diuretic** that can worsen existing urinary incontinence or frequency.
- While reducing caffeine intake might help manage symptoms in the long term, it is not the appropriate **first step** to diagnose the acute onset of severe symptoms that likely point to an infection.
More Pelvic organ prolapse repair US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.