Ovarian cystectomy and oophorectomy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ovarian cystectomy and oophorectomy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
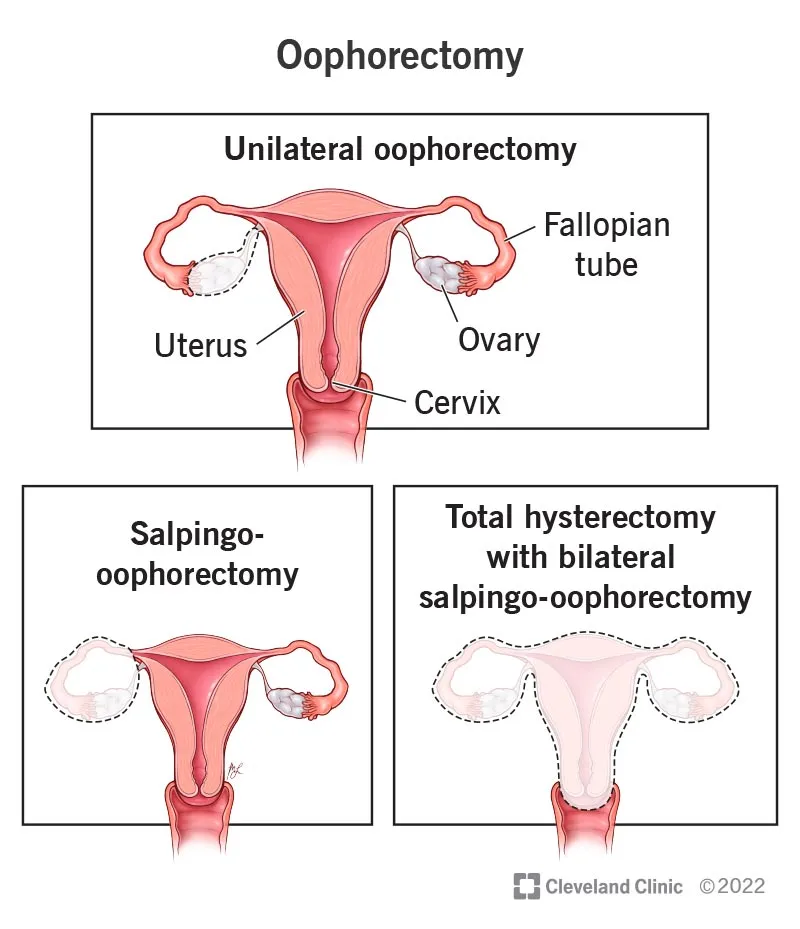
Ovarian cystectomy and oophorectomy US Medical PG Question 1: A 33-year-old woman comes to the emergency department because of a 1-hour history of severe pelvic pain and nausea. She was diagnosed with a follicular cyst in the left ovary 3 months ago. The cyst was found incidentally during a fertility evaluation. A pelvic ultrasound with Doppler flow shows an enlarged, edematous left ovary with no blood flow. Laparoscopic evaluation shows necrosis of the left ovary, and a left oophorectomy is performed. During the procedure, blunt dissection of the left infundibulopelvic ligament is performed. Which of the following structures is most at risk of injury during this step of the surgery?
- A. Bladder trigone
- B. Uterine artery
- C. Kidney
- D. Ureter (Correct Answer)
Ovarian cystectomy and oophorectomy Explanation: ***Ureter***
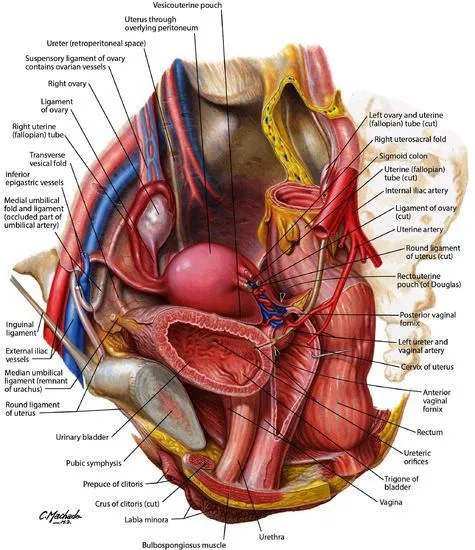
- The **infundibulopelvic ligament** (also known as the suspensory ligament of the ovary) contains the **ovarian artery and vein** and is in close proximity to the ureter as it crosses the pelvic brim.
- During dissection or clamping of this ligament, especially in an emergency setting or when anatomy is distorted (e.g., by an enlarged ovary or edema), the **ureter** is highly susceptible to injury.
*Bladder trigone*
- The **bladder trigone** is the smooth triangular region at the base of the bladder, formed by the openings of the ureters and the internal urethral orifice.
- It is not directly adjacent to the infundibulopelvic ligament and is therefore at a comparably lower risk of injury during dissection of this ligament.
*Uterine artery*
- The **uterine artery** travels within the cardinal ligament and supplies the uterus; it is located more medially and inferiorly within the broad ligament.
- While important in pelvic surgery, it is not in the immediate vicinity of the infundibulopelvic ligament dissection itself.
*Kidney*
- The **kidneys** are retroperitoneal organs located much higher in the abdominal cavity, far superior to the pelvis.
- They are not at risk of direct injury during pelvic surgery involving the infundibulopelvic ligament.
Ovarian cystectomy and oophorectomy US Medical PG Question 2: A 47-year-old woman presents with abnormal vaginal bleeding. She reports that she has had heavy, irregular periods for the past 6 months. Her periods, which normally occur every 28 days, are sometimes now only 2-3 weeks apart, last 7-10 days, and has spotting in between menses. Additionally, her breasts feel enlarged and tender. She denies abdominal pain, dysuria, dyspareunia, constipation, or abnormal vaginal discharge. The patient has a history of depression and hyperlipidemia. She takes fluoxetine and atorvastatin. She is a widow and has 2 healthy children. She works as an accountant. The patient says she drinks a half bottle of wine every night to help her calm down after work and to help her sleep. She denies tobacco or illicit drug use. She is not currently sexually active. Physical examination reveals spider angiomata and mild ascites. The left ovary is palpable but non-tender. A thickened endometrial stripe and a left ovarian mass are noted on ultrasound. A mammogram, chest radiograph, and CT abdomen/pelvis are pending. Which of the following tumor markers is associated with the patient’s most likely diagnosis?
- A. Alpha-fetoprotein
- B. Estrogen
- C. Testosterone
- D. Carcinoembryonic antigen
- E. Cancer antigen-125 (Correct Answer)
Ovarian cystectomy and oophorectomy Explanation: ***Cancer antigen-125***
- The patient's presentation with **abnormal vaginal bleeding**, **breast tenderness**, **spider angiomata**, and **ascites** suggests a gynecological malignancy, possibly **ovarian cancer** with liver involvement due to chronic alcohol use. **CA-125** is the most widely used tumor marker for epithelial ovarian cancer.
- While not diagnostic on its own, elevated CA-125 levels, especially in the context of a **palpable ovarian mass** and **ascites**, strongly support the diagnosis of ovarian cancer, and it is also used for monitoring treatment response and recurrence.
*Alpha-fetoprotein*
- **Alpha-fetoprotein (AFP)** is primarily associated with **germ cell tumors**, such as **yolk sac tumors** of the ovary, and **hepatocellular carcinoma**.
- While an ovarian mass is present, the clinical picture with prominent signs of **estrogen excess** (abnormal bleeding, breast tenderness, thickened endometrial stripe) and **liver disease** (spider angiomata, ascites) does not strongly point to an AFP-secreting tumor or primary hepatocellular carcinoma without further evidence.
*Estrogen*
- Although the patient's symptoms (abnormal bleeding, breast tenderness, thickened endometrial stripe) are consistent with **estrogen excess**, estrogen itself is a **hormone**, not a tumor marker used to diagnose ovarian cancer.
- Some ovarian tumors, particularly **granulosa cell tumors**, produce estrogen, which would be reflected in elevated serum estrogen levels, but "estrogen" is not the tumor marker itself.
*Testosterone*
- **Testosterone** is primarily associated with **androgen-secreting tumors**, such as **Sertoli-Leydig cell tumors** of the ovary, which would typically present with signs of **virilization** (e.g., hirsutism, deepening voice, clitoromegaly).
- The patient's symptoms of **estrogen excess** (abnormal uterine bleeding, breast tenderness) are contrary to a testosterone-secreting tumor.
*Carcinoembryonic antigen*
- **Carcinoembryonic antigen (CEA)** is a tumor marker primarily associated with **colorectal cancer**, but it can also be elevated in other adenocarcinomas, such as those of the **breast, lung, and gastrointestinal tract**.
- While general malignancy is considered, CEA is not the primary marker for ovarian cancer, and the constellation of symptoms (especially those related to estrogen excess and possible liver involvement) points more specifically towards an ovarian origin.
Ovarian cystectomy and oophorectomy US Medical PG Question 3: Patient 1 – A 26-year-old woman presents to her primary care physician for an annual exam. She currently does not have any acute concerns and says her health has been generally well. Medical history is significant for asthma, which is managed with an albuterol inhaler. Her last pap smear was unremarkable. She is currently sexually active with one male and consistently uses condoms. She occasionally smokes marijuana and drinks wine once per week. Her mother recently passed away from advanced ovarian cancer. Her sister is 37-years-old and was recently diagnosed with breast cancer and ovarian cancer. Physical examination is remarkable for a mildly anxious woman.
Patient 2 – A 27-year-old woman presents to her primary care physician for an annual exam. She says that she would like to be screened for breast cancer since two of her close friends were recently diagnosed. She noticed she has a small and mobile mass on her left breast, which increases in size and becomes tender around her time of menses. Family history is remarkable for hypertension in the father. The physical exam is significant for a small, well-defined, and mobile mass on her left breast that is not tender to palpation.
Which of the following is the best next step in management for patient 1 and 2?
- A. Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam
- B. Patient 1 – Reassurance. Patient 2 – Breast ultrasound
- C. Patient 1 – CA-125 testing. Patient 2 – BRCA testing
- D. Patient 1 – BRCA testing. Patient 2 – Breast ultrasound (Correct Answer)
- E. Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography
Ovarian cystectomy and oophorectomy Explanation: ***Patient 1 – BRCA testing. Patient 2 – Breast ultrasound***
- Patient 1 has a strong family history of early-onset **breast and ovarian cancer** (**mother and sister**), suggesting a high probability of an inherited genetic mutation, such as **BRCA1/2**, which warrants genetic testing.
- Patient 2 presents with a **small, mobile, well-defined breast mass** that is likely benign, and a **breast ultrasound** is the appropriate initial imaging for further characterization in a young woman.
*Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam*
- Patient 1's primary concern is genetic predisposition due to family history, an **ultrasound** is not the initial or primary screening method for future cancer risk.
- Patient 2 has a palpable mass; waiting 3 months for a **clinical breast exam** without initial imaging (ultrasound) is not appropriate for evaluating a new breast lump.
*Patient 1 – Reassurance. Patient 2 – Breast ultrasound*
- Patient 1's family history of **early-onset breast and ovarian cancer** is a significant risk factor; therefore, simple **reassurance** without further investigation is inappropriate.
- While a **breast ultrasound** is appropriate for Patient 2, the recommendation for Patient 1 is incorrect.
*Patient 1 – CA-125 testing. Patient 2 – BRCA testing*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer treatment or recurrence, not for initial screening in asymptomatic individuals, especially in a young woman with no active symptoms.
- **BRCA testing** is indicated for Patient 1 due to family history, but not for Patient 2 who has a likely benign breast mass and no significant family history.
*Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography*
- Regular **breast and ovarian ultrasounds** are not recommended as primary screening tools for genetic risk in asymptomatic high-risk individuals like Patient 1.
- **Mammography** is less sensitive in young women (under 30) due to higher breast tissue density, making **ultrasound** the preferred initial imaging for Patient 2.
Ovarian cystectomy and oophorectomy US Medical PG Question 4: A 32-year-old man visits his primary care physician for a routine health maintenance examination. During the examination, he expresses concerns about not wanting to become a father. He has been sexually active and monogamous with his wife for the past 5 years, and they inconsistently use condoms for contraception. He tells the physician that he would like to undergo vasectomy. His wife is also a patient under the care of the physician and during her last appointment, she expressed concerns over being prescribed any drugs that could affect her fertility because she would like to conceive soon. Which of the following is the most appropriate action by the physician regarding this patient's wish to undergo vasectomy?
- A. Explain the procedure's benefits, alternatives, and potential complications (Correct Answer)
- B. Refer the patient to a psychotherapist to discuss his reluctance to have children
- C. Discourage the patient from undergoing the procedure because his wife wants children
- D. Insist that the patient returns with his wife to discuss the risks and benefits of the procedure together
- E. Call the patient's wife to obtain her consent for the procedure
Ovarian cystectomy and oophorectomy Explanation: ***Explain the procedure's benefits, alternatives, and potential complications***
- The physician's primary ethical obligation is to the individual patient, ensuring informed consent for any medical procedure. Providing comprehensive information about **vasectomy benefits, alternatives, and risks** allows the patient to make an autonomous decision.
- While patient-physician confidentiality generally prohibits disclosing specific details of one spouse's medical history to the other, the general knowledge that his wife desires children creates an important backdrop for the discussion. It is the patient's responsibility to consider this and convey this information to his wife.
*Refer the patient to a psychotherapist to discuss his reluctance to have children*
- It is **not appropriate** to assume the patient has a psychological issue solely based on his desire for a vasectomy, even with his wife's conflicting wishes. This action could be seen as judgmental and dismissive of the patient's autonomy.
- A patient's preference for sterilization, even if contrary to a partner's desires, does not inherently indicate a need for psychiatric evaluation unless there are other concerning psychological symptoms.
*Discourage the patient from undergoing the procedure because his wife wants children*
- **Discouraging** the patient based on his wife's wishes infringes upon the patient's **autonomy and reproductive rights**. The physician's role is to provide information and support the patient's informed decisions, not to act as a relationship counselor or impose personal values.
- Medical decisions, especially concerning fertility, are deeply personal, and a physician should not pressure a patient into a decision they do not want based on a partner's separate, yet relevant, wishes.
*Insist that the patient returns with his wife to discuss the risks and benefits of the procedure together*
- While open communication between spouses about reproductive decisions is beneficial, **insisting** on the wife's presence for the consultation undermines the patient's **confidentiality and individual autonomy**. The patient has the right to make medical decisions independently.
- The physician should encourage the patient to discuss this with his wife, but it is ultimately the patient's decision whether to involve her in the consultation for his procedure.
*Call the patient's wife to obtain her consent for the procedure*
- This action would be a **breach of patient confidentiality**. The physician cannot disclose information about the patient's decision or medical discussions with a third party, even a spouse, without the patient's explicit consent.
- A spouse's consent is **not legally or ethically required** for an individual to undergo a vasectomy in most jurisdictions, as it is a decision pertaining to the individual's body and reproductive rights.
Ovarian cystectomy and oophorectomy US Medical PG Question 5: A 37-year-old G2P1 woman presents to the clinic complaining of amenorrhea. She reports that she has not had a period for 2 months. A urine pregnancy test that she performed yesterday was negative. She is sexually active with her husband and uses regular contraception. Her past medical history is significant for diabetes and a dilation and curettage procedure 4 months ago for an unviable pregnancy. She denies any discharge, abnormal odor, abnormal bleeding, dysmenorrhea, or pain but endorses a 10-pound intentional weight loss over the past 3 months. A pelvic examination is unremarkable. What is the most likely explanation for this patient’s presentation?
- A. Polycystic ovarian syndrome
- B. Pregnancy
- C. Intrauterine adhesions (Correct Answer)
- D. Premature menopause
- E. Extreme weight loss
Ovarian cystectomy and oophorectomy Explanation: ***Intrauterine adhesions***
- The recent history of a **dilation and curettage (D&C)** procedure and subsequent amenorrhea strongly suggest **intrauterine adhesions (Asherman's syndrome)**. The D&C can cause damage to the endometrial lining, leading to scar tissue formation.
- The absence of other menstrual symptoms like pain, discharge, or abnormal bleeding, combined with amenorrhea, aligns with this diagnosis, as the scarred uterine cavity prevents normal menstrual shedding.
*Polycystic ovarian syndrome*
- While PCOS can cause amenorrhea, it is usually associated with other symptoms like **hirsutism**, acne, or obesity, none of which are mentioned here.
- The patient's recent D&C and the acute onset of amenorrhea are more direct clues for intrauterine adhesions.
*Pregnancy*
- The patient's **negative urine pregnancy test** performed yesterday effectively rules out pregnancy as the cause of her amenorrhea.
- Although she uses contraception, a negative test is a strong indicator against pregnancy.
*Premature menopause*
- Premature menopause typically occurs before age 40 and is associated with symptoms like **hot flashes**, night sweats, or vaginal dryness, which are absent in this case.
- While the patient is 37, making her within the age range for premature menopause, the recent D&C provides a more plausible and acute explanation for her amenorrhea.
*Extreme weight loss*
- While **significant weight loss** can cause hypothalamic amenorrhea, the patient's 10-pound intentional weight loss over 3 months is not typically considered "extreme" enough to induce amenorrhea in a healthy individual without other contributing factors.
- Her prior D&C is a more direct and significant risk factor for the current symptoms.
Ovarian cystectomy and oophorectomy US Medical PG Question 6: A 62-year-old woman presents to her primary care physician for a routine physical exam. The patient has no specific complaints but does comment on some mild weight gain. She reports that she recently retired from her job as a math teacher and has taken up hiking. Despite the increase in activity, she believes her pants have become "tighter." She denies headaches, urinary symptoms, or joint pains. She has a history of hypertension, type 2 diabetes, and rheumatoid arthritis. Her medications include aspirin, lisinopril, rovastatin, metformin, and methotrexate. She takes her medications as prescribed and is up to date with her vaccinations. A colonoscopy two years ago and a routine mammography last year were both normal. The patient’s last menstrual period was 10 years ago. The patient has a father who died of colon cancer at 71 years of age and a mother who has breast cancer. Her temperature is 98.7°F (37°C), blood pressure is 132/86 mmHg, pulse is 86/min, respirations are 14/min and oxygen saturation is 98% on room air. Physical exam is notable for a mildly distended abdomen and a firm and non-mobile right adnexal mass. What is the next step in the management of this patient?
- A. Pelvic ultrasound (Correct Answer)
- B. Abdominal MRI
- C. PET-CT
- D. Exploratory laparotomy and debulking
- E. CA-125 level
Ovarian cystectomy and oophorectomy Explanation: ***Pelvic ultrasound***
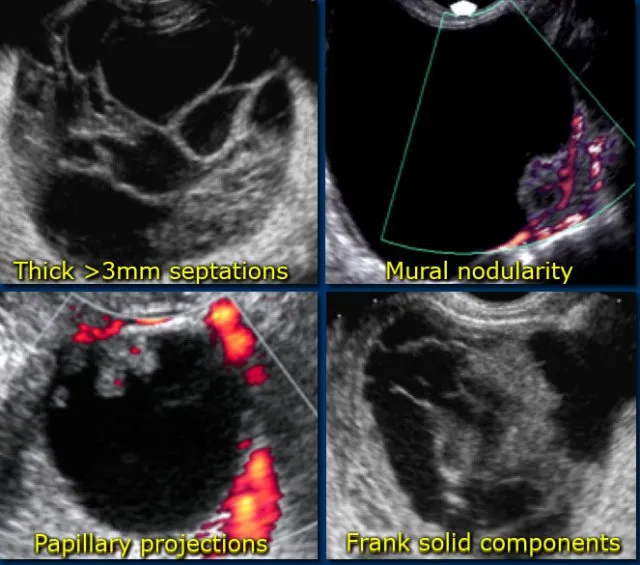
- A **non-mobile right adnexal mass** in a postmenopausal woman, along with vague symptoms like **abdominal distension** and **weight gain**, raises suspicion for **ovarian cancer**.
- A **pelvic ultrasound** is the initial, non-invasive, and cost-effective imaging modality to characterize adnexal masses, assessing size, morphology, and vascularity.
*Abdominal MRI*
- While **MRI** offers excellent soft tissue contrast, it is typically used as a **secondary imaging modality** for further characterization of adnexal masses when ultrasound findings are inconclusive or for surgical planning, not as the initial step.
- Its higher cost and longer scan time make it less suitable for initial screening compared to ultrasound.
*PET-CT*
- **PET-CT** is primarily used for **staging malignancies** and detecting metastatic disease, or in cases of unknown primary, and is not the initial diagnostic test for an adnexal mass.
- It involves radiation exposure and is generally reserved for situations where malignancy is already highly suspected or confirmed.
*Exploratory laparotomy and debulking*
- **Exploratory laparotomy** and **debulking** are surgical procedures performed for the definitive diagnosis, staging, and treatment of ovarian cancer, but only *after* a thorough initial workup has been completed.
- It is an invasive procedure and should not be the first step in the investigation of an adnexal mass.
*CA-125 level*
- Measuring **CA-125** levels is useful as a **tumor marker** in the workup of suspected ovarian cancer, particularly in symptomatic postmenopausal women, and for monitoring treatment response.
- However, it has **low specificity** (can be elevated in benign conditions) and should be ordered in conjunction with imaging, not as the sole initial diagnostic step.
Ovarian cystectomy and oophorectomy US Medical PG Question 7: A 15-year-old girl comes to the physician because of a 2-year history of irregular menstrual bleeding. Menses have occurred at irregular 45- to 60-day intervals since menarche at the age of 13 years. Her last menstrual period was 5 weeks ago and lasted for 7 days with heavy flow and no cramping. She is not sexually active. She is 171 cm (5 ft 7 in) tall and weighs 58 kg (128 lb); BMI is 20 kg/m2. Her temperature is 36.6°C (97.8°F), pulse is 80/min, and blood pressure is 110/60 mm Hg. Pelvic examination shows a normal-appearing vagina and cervix. Bimanual examination shows a normal-sized uterus and no palpable adnexal masses. The remainder of the physical examination shows no abnormalities. A urine pregnancy test is negative. Which of the following is the most likely explanation for this patient's symptoms?
- A. Endometriosis
- B. Polycystic ovary syndrome
- C. Pituitary adenoma
- D. Anovulation (Correct Answer)
- E. Ovarian insufficiency
Ovarian cystectomy and oophorectomy Explanation: ***Anovulation***
- Irregular menses, especially in the context of adolescence, are commonly due to **immature hypothalamic-pituitary-ovarian axis**, leading to anovulatory cycles.
- In anovulatory bleeding, the **endometrium proliferates unopposed by progesterone**, leading to irregular shedding and heavy flow.
*Endometriosis*
- Characterized by **pelvic pain** and **dysmenorrhea**, which are absent in this patient.
- Endometriosis typically causes dysfunctional uterine bleeding rather than irregular menses starting at menarche.
*Polycystic ovary syndrome*
- Often presents with **hirsutism**, **acne**, and/or **obesity**, none of which are noted in this patient.
- While it causes irregular menses due to anovulation, the absence of other classic symptoms makes it less likely given the age and presentation.
*Pituitary adenoma*
- Can cause irregular menses via **hyperprolactinemia**, but this would typically present with **galactorrhea** or **visual field defects**, which are not mentioned.
- The patient's otherwise normal examination and lack of symptoms of mass effect or hormonal excess make a pituitary adenoma unlikely.
*Ovarian insufficiency*
- Implies premature ovarian failure, which is rare at this age and would typically present with symptoms of **estrogen deficiency**, like hot flashes, and ultimately **amenorrhea**.
- Ovarian insufficiency is characterized by **elevated gonadotropin levels**, which are not indicated by the patient's presentation.
Ovarian cystectomy and oophorectomy US Medical PG Question 8: Four hours after undergoing an abdominal hysterectomy, a 43-year-old woman is evaluated in the post-anesthesia care unit because she has only had a urine output of 5 mL of blue-tinged urine since surgery. The operation went smoothly and ureter patency was checked via retrograde injection of methylene blue dye mixed with saline through the Foley catheter. She received 2.4 L of crystalloid fluids intraoperatively and urine output was 1.2 L. She had a history of fibroids with painful and heavy menses. She is otherwise healthy. She underwent 2 cesarean sections 8 and 5 years ago, respectively. Her temperature is 37.4°C (99.3°F), pulse is 75/min, respirations are 16/min, and blood pressure is 122/76 mm Hg. She appears comfortable. Cardiopulmonary examination shows no abnormalities. There is a midline surgical incision with clean and dry dressings. Her abdomen is soft and mildly distended in the lower quadrants. Her bladder is slightly palpable. Extremities are warm and well perfused, and capillary refill is brisk. Laboratory studies show:
Leukocyte count 8,300/mm3
Hemoglobin 10.3 g/dL
Hematocrit 31%
Platelet count 250,000/mm3
Serum
_Na+ 140 mEq/L
_K+ 4.2 mEq/L
_HCO3+ 26 mEq/L
_Urea nitrogen 26 mg/dL
_Creatinine 1.0 mg/dL
Urine
_Blood 1+
_WBC none
_Protein negative
_RBC none
_RBC casts none
A bladder scan shows 250 mL of retained urine. Which of the following is the next best step in the evaluation of this patient?
- A. Check the Foley catheter (Correct Answer)
- B. Return to the operating room for emergency surgery
- C. Perform ultrasound of the kidneys
- D. Administer 20 mg of IV furosemide
- E. Administer bolus 500 mL of Lactated Ringers
Ovarian cystectomy and oophorectomy Explanation: ***Check the Foley catheter***
- This patient presents with signs of **urinary retention** (low urine output, palpable bladder, retained urine on bladder scan) despite methylene blue injection confirming ureter patency. The most common and easily reversible cause of low urine output post-hysterectomy is a **kinked or obstructed Foley catheter**.
- Given the smooth intraoperative course and adequate urine output during surgery, a quick check and potential **repositioning or flushing of the catheter** is the immediate and most appropriate first step before considering more invasive interventions.
*Return to the operating room for emergency surgery*
- This is a drastic step and is not indicated at this stage. There is no evidence of a **surgical complication** requiring emergency intervention, such as a ureteral injury (which was checked intraoperatively) or active hemorrhage.
- The patient's vital signs are stable, and she appears comfortable, which makes an emergency surgical re-exploration highly unlikely as the initial best step.
*Perform ultrasound of the kidneys*
- While a renal ultrasound can assess for **hydronephrosis** or other kidney abnormalities, it is a delayed step. Given the clear evidence of bladder retention and the possibility of a simple catheter malfunction, performing an ultrasound without first addressing the catheter would be premature.
- The patient's **creatinine is normal**, making acute kidney injury due to obstruction less likely as an immediate concern.
*Administer 20 mg of IV furosemide*
- Furosemide is a **loop diuretic** that increases urine production. However, it would be ineffective and potentially harmful if the issue is a mechanical obstruction of urine outflow, as appears to be the case here.
- Administering a diuretic without addressing the outflow problem would only worsen bladder distension and potentially stress the renal system without resolving the underlying issue.
*Administer bolus 500 mL of Lactated Ringers*
- This patient has already received 2.4 L of crystalloid fluids intraoperatively and has stable vital signs, indicating she is likely **euvolemic**.
- Giving another fluid bolus would not address the observed urinary retention and could lead to **fluid overload** if the urine outflow obstruction persists.
Ovarian cystectomy and oophorectomy US Medical PG Question 9: A 39-year-old man presents with painless swelling of the right testis and a sensation of heaviness. The physical examination revealed an intra-testicular solid mass that could not be felt separately from the testis. After a thorough evaluation, he was diagnosed with testicular seminoma. Which of the following group of lymph nodes are most likely involved?
- A. Superficial inguinal lymph nodes (lateral group)
- B. Deep inguinal lymph nodes
- C. Superficial inguinal lymph nodes (medial group)
- D. Para-rectal lymph nodes
- E. Para-aortic lymph nodes (Correct Answer)
Ovarian cystectomy and oophorectomy Explanation: ***Para-aortic lymph nodes***
- The **testes** develop in the abdomen and descend into the scrotum, retaining their original lymphatic drainage. Therefore, **testicular cancer** typically metastasizes to the **para-aortic** (or retroperitoneal) lymph nodes, which are located near the renal veins at the level of L1-L2.
- This is the primary lymphatic drainage pathway for the testes.
*Superficial inguinal lymph nodes (lateral group)*
- These lymph nodes primarily drain the skin of the **scrotum**, perineum, and lower limbs, but not the **testes** themselves.
- Involvement would suggest spread to the scrotal skin or compromised lymphatic flow due to prior scrotal surgery or infection, which is not indicated here.
*Deep inguinal lymph nodes*
- **Deep inguinal lymph nodes** drain structures deeper in the leg and gluteal region, as well as receiving efferent vessels from the superficial inguinal nodes.
- They are not the primary drainage site for the **testes**.
*Superficial inguinal lymph nodes (medial group)*
- Similar to the lateral group, the **medial superficial inguinal lymph nodes** primarily drain the external genitalia (excluding the testes), perineum, and lower abdominal wall.
- They are not the direct drainage route for **testicular cancer**.
*Para-rectal lymph nodes*
- **Para-rectal lymph nodes** are located near the rectum and are involved in the drainage of the rectum and lower sigmoid colon.
- They have no direct connection to the lymphatic drainage of the **testes**.
Ovarian cystectomy and oophorectomy US Medical PG Question 10: A 54-year-old male carpenter accidentally amputated his right thumb while working in his workshop 30 minutes ago. He reports that he was cutting a piece of wood, and his hand became caught up in the machinery. He is calling the emergency physician for advice on how to transport his thumb and if it is necessary. Which of the following is the best information for this patient?
- A. Place thumb in cup of cold milk
- B. Wrap thumb in saline-moistened, sterile gauze and place in sterile bag (Correct Answer)
- C. Wrap thumb in sterile gauze and submerge in a cup of saline
- D. There is no need to save the thumb
- E. Place thumb directly into cooler of ice
Ovarian cystectomy and oophorectomy Explanation: ***Wrap thumb in saline-moistened, sterile gauze and place in sterile bag***
- This method provides a **moist, sterile environment** for the amputated part, which is crucial for preserving tissue viability.
- The use of a sterile bag helps prevent contamination and allows the part to be placed inside a cooler without direct ice contact, preventing **frostbite**.
*Place thumb in cup of cold milk*
- While cold milk might offer some cooling, it is **not sterile** and could introduce bacteria, increasing the risk of infection.
- Milk's composition is **not ideal for cell preservation** compared to saline, which is more isotonic.
*Wrap thumb in sterile gauze and submerge in a cup of saline*
- Submerging the amputated part directly in saline, even with sterile gauze, can lead to **tissue maceration** due to overhydration.
- This method also makes it more difficult to prevent contamination during transportation if the cup is not sealed.
*There is no need to save the thumb*
- **Replantation surgery** is often possible and highly desirable for thumb amputations due to its critical functional role.
- Dismissing the amputated part would deprive the patient of a chance to restore function, especially given the short time since amputation.
*Place thumb directly into cooler of ice*
- Direct contact with ice can cause **frostbite** and **tissue damage**, compromising the viability of the amputated part.
- The preferred method is to keep the amputated part cool, but not frozen, usually by placing it in a sealed bag within an ice-filled container.
More Ovarian cystectomy and oophorectomy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.