Hysterectomy techniques and indications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hysterectomy techniques and indications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hysterectomy techniques and indications US Medical PG Question 1: A 33-year-old woman comes to the emergency department because of a 1-hour history of severe pelvic pain and nausea. She was diagnosed with a follicular cyst in the left ovary 3 months ago. The cyst was found incidentally during a fertility evaluation. A pelvic ultrasound with Doppler flow shows an enlarged, edematous left ovary with no blood flow. Laparoscopic evaluation shows necrosis of the left ovary, and a left oophorectomy is performed. During the procedure, blunt dissection of the left infundibulopelvic ligament is performed. Which of the following structures is most at risk of injury during this step of the surgery?
- A. Bladder trigone
- B. Uterine artery
- C. Kidney
- D. Ureter (Correct Answer)
Hysterectomy techniques and indications Explanation: ***Ureter***
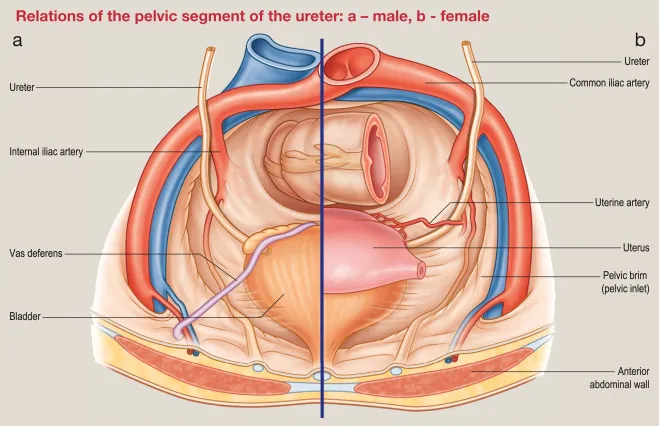
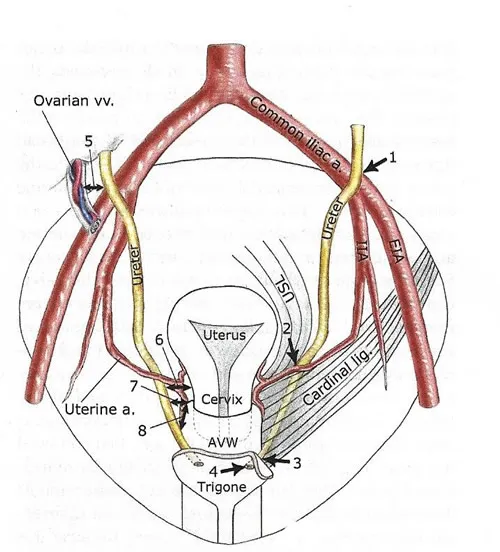
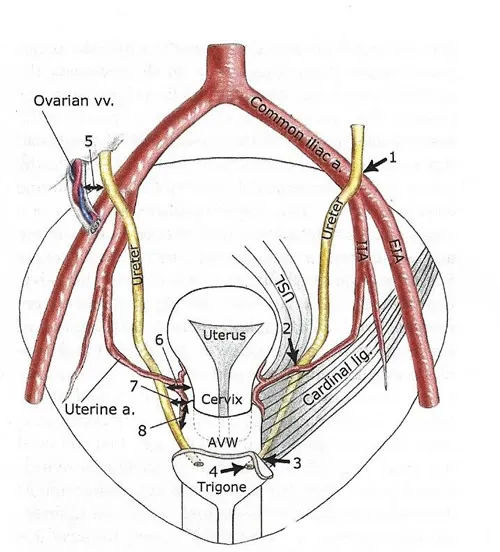
- The **infundibulopelvic ligament** (also known as the suspensory ligament of the ovary) contains the **ovarian artery and vein** and is in close proximity to the ureter as it crosses the pelvic brim.
- During dissection or clamping of this ligament, especially in an emergency setting or when anatomy is distorted (e.g., by an enlarged ovary or edema), the **ureter** is highly susceptible to injury.
*Bladder trigone*
- The **bladder trigone** is the smooth triangular region at the base of the bladder, formed by the openings of the ureters and the internal urethral orifice.
- It is not directly adjacent to the infundibulopelvic ligament and is therefore at a comparably lower risk of injury during dissection of this ligament.
*Uterine artery*
- The **uterine artery** travels within the cardinal ligament and supplies the uterus; it is located more medially and inferiorly within the broad ligament.
- While important in pelvic surgery, it is not in the immediate vicinity of the infundibulopelvic ligament dissection itself.
*Kidney*
- The **kidneys** are retroperitoneal organs located much higher in the abdominal cavity, far superior to the pelvis.
- They are not at risk of direct injury during pelvic surgery involving the infundibulopelvic ligament.
Hysterectomy techniques and indications US Medical PG Question 2: A 36-year-old woman comes to the physician for a 2-month history of urinary incontinence and a vaginal mass. She has a history of five full-term normal vaginal deliveries. She gave birth to a healthy newborn 2-months ago. Since then she has felt a sensation of vaginal fullness and a firm mass in the lower vagina. She has loss of urine when she coughs, sneezes, or exercises. Pelvic examination shows an irreducible pink globular mass protruding out of the vagina. A loss of integrity of which of the following ligaments is most likely involved in this patient's condition?
- A. Infundibulopelvic ligament
- B. Broad ligament of the uterus
- C. Cardinal ligament of the uterus (Correct Answer)
- D. Round ligament of uterus
- E. Uterosacral ligament
Hysterectomy techniques and indications Explanation: ***Cardinal ligament of the uterus***
- The patient's symptoms, including **vaginal mass**, **urinary incontinence** with coughing/sneezing, and history of **multiple vaginal deliveries**, strongly suggest **uterine prolapse**.
- The cardinal ligaments are crucial in providing **lateral cervical support** and are often damaged during childbirth, leading to uterine descent.
*Infundibulopelvic ligament*
- This ligament primarily supports the **ovaries** and contains the **ovarian artery** and vein.
- Damage to this ligament is associated with ovarian prolapse or complications during oophorectomy, not uterine prolapse.
*Broad ligament of the uterus*
- The broad ligament is a **peritoneal fold** that drapes over the uterus, fallopian tubes, and ovaries.
- While it helps to hold these structures in place, its primary role is not in preventing uterine prolapse; it mainly provides a medium for neurovascular structures.
*Round ligament of uterus*
- The round ligament extends from the uterus to the **labia majora** and primarily helps maintain **anteversion** of the uterus.
- It plays a minor role in uterine support and its laxity is not a primary cause of uterine prolapse.
*Uterosacral ligament*
- The uterosacral ligaments provide **posterior support** to the uterus, particularly by anchoring the cervix to the sacrum.
- While damage to these ligaments contributes to **apical prolapse**, the cardinal ligaments are more critical for lateral support and more commonly implicated in overall uterine prolapse following childbirth.
Hysterectomy techniques and indications US Medical PG Question 3: A 31-year-old female presents to her gynecologist with spotting between periods. She reports that her menses began at age 11, and she has never had spotting prior to the three months ago. Her medical history is significant for estrogen-receptor positive intraductal carcinoma of the breast, which was treated with tamoxifen. An endometrial biopsy is performed, which shows endometrial hyperplasia with atypia. She reports that she and her husband are currently trying to have children. What is the next best step?
- A. Start progestin-only therapy (Correct Answer)
- B. Partial, cervix-sparing hysterectomy
- C. Observation with annual endometrial biopsies
- D. Start combination estrogen and progestin therapy
- E. Total abdominal hysterectomy with bilateral salpingo-oophorectomy
Hysterectomy techniques and indications Explanation: ***Start progestin-only therapy***
- This patient has **endometrial hyperplasia with atypia**, which carries a high risk of progression to **endometrial cancer**, especially when associated with **tamoxifen use**.
- Given her desire for **fertility preservation**, **high-dose progestin therapy** (e.g., megestrol acetate, medroxyprogesterone acetate) is the **first-line treatment** to reverse the hyperplasia while allowing for potential conception.
*Partial, cervix-sparing hysterectomy*
- This procedure treats the uterus but would still preclude future pregnancies and is typically reserved for cases where definitive surgical management is required but the patient wishes to preserve vaginal function.
- It would be too aggressive for a patient desiring fertility who has not failed medical therapy, and it does not remove the at-risk endometrium effectively.
*Observation with annual endometrial biopsies*
- **Endometrial hyperplasia with atypia** has a significant risk of progressing to **endometrial carcinoma**, estimated at 29% over 20 years.
- Simply observing without intervention is **inappropriate** given this high risk, even with regular monitoring.
*Start combination estrogen and progestin therapy*
- The patient's endometrial hyperplasia is likely due to the **unopposed estrogenic effect of tamoxifen** on the endometrium, which acts as a selective estrogen receptor modulator (SERM).
- Adding **estrogen** would exacerbate the problem and increase the risk of endometrial cancer, making this an unsafe and inappropriate treatment.
*Total abdominal hysterectomy with bilateral salpingo-oophorectomy*
- This is a definitive surgical treatment for endometrial hyperplasia with atypia and endometrial cancer, and would effectively remove the affected tissue.
- However, this option would render the patient **infertile**, which contradicts her expressed desire to have children. It would be considered if progestin therapy fails or if fertility is not a concern.
Hysterectomy techniques and indications US Medical PG Question 4: A 55-year-old woman is being managed on the surgical floor after having a total abdominal hysterectomy as a definitive treatment for endometriosis. On day 1 after the operation, the patient complains of fevers. She has no other complaints other than aches and pains from lying in bed as she has not moved since the procedure. She is currently receiving ondansetron, acetaminophen, and morphine. Her temperature is 101°F (38.3°C), blood pressure is 127/68 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 94% on room air. Her abdominal exam is within normal limits and cardiopulmonary exam is only notable for mild crackles. Which of the following is the most likely etiology of this patient’s fever?
- A. Deep vein thrombosis
- B. Abscess formation
- C. Inflammatory stimulus of surgery (Correct Answer)
- D. Urinary tract infection
- E. Wound infection
Hysterectomy techniques and indications Explanation: ***Inflammatory stimulus of surgery***
- Postoperative fever occurring within the first 24-48 hours after surgery, especially a major abdominal procedure, is most commonly due to the **systemic inflammatory response** to tissue trauma and stress from the surgery itself.
- The temperature of 101°F (38.3°C) is a common reactive fever. In this timeframe, **atelectasis** (part of the inflammatory response to surgery) is the classic cause, supported by the patient's **immobility since surgery** and **mild crackles** on exam.
- The patient has no other specific signs of infection, making this the most likely cause.
*Deep vein thrombosis*
- While DVT is a concern post-surgery, it typically presents with **leg pain, swelling, and tenderness**, not primarily as fever alone on day 1.
- A fever from DVT would usually indicate a more advanced complication like pulmonary embolism, which is inconsistent with the mild crackles and stable oxygen saturation.
*Abscess formation*
- Abscesses usually take several days to form and present with significant fevers, localized pain, and possibly purulent drainage, not typically within the first **24 hours post-op**.
- The abdominal exam is noted as within normal limits, making an abscess unlikely at this early stage.
*Urinary tract infection*
- UTIs are common post-op, especially with catheterization, but typically present with **dysuria, frequency, urgency**, and sometimes suprapubic pain, which are absent here.
- While fever can be a symptom, the lack of urinary complaints makes it a less likely primary diagnosis on day 1.
*Wound infection*
- Wound infections rarely develop within the first **24-48 hours** post-surgery, as bacteria require time to proliferate and cause inflammatory signs.
- Typical signs include **erythema, warmth, tenderness, and purulent drainage** at the incision site, which are not mentioned.
Hysterectomy techniques and indications US Medical PG Question 5: A 56-year-old woman is one week status post abdominal hysterectomy when she develops a fever of 101.4°F (38.6°C). Her past medical history is significant for type II diabetes mellitus and a prior history of alcohol abuse. The operative report and intraoperative cystoscopy indicate that the surgery was uncomplicated. The nurse reports that since the surgery, the patient has also complained of worsening lower abdominal pain. She has given the patient the appropriate pain medications with little improvement. The patient has tolerated an oral diet well and denies nausea, vomiting, or abdominal distension. Her blood pressure is 110/62 mmHg, pulse is 122/min, and respirations are 14/min. Since being given 1000 mL of intravenous fluids yesterday, the patient has excreted 800 mL of urine. On physical exam, she is uncomfortable, shivering, and sweating. The surgical site is intact, but the surrounding skin appears red. No drainage is appreciated. The abdominal examination reveals tenderness to palpation and hypoactive bowel sounds. Labs and a clean catch urine specimen are obtained as shown below:
Leukocyte count and differential:
Leukocyte count: 18,000/mm^3
Segmented neutrophils: 80%
Bands: 10%
Eosinophils: 1%
Basophils: < 1%
Lymphocytes: 5%
Monocytes: 4%
Platelet count: 300,000/mm^3
Hemoglobin: 12.5 g/dL
Hematocrit: 42%
Urine:
Epithelial cells: 15/hpf
Glucose: positive
RBC: 1/hpf
WBC: 2/hpf
Bacteria: 50 cfu/mL
Ketones: none
Nitrites: negative
Leukocyte esterase: negative
Which of the following is most likely the cause of this patient’s symptoms?
- A. Surgical error
- B. Post-operative ileus
- C. Wound infection (Correct Answer)
- D. Alcohol withdrawal
- E. Urinary tract infection
Hysterectomy techniques and indications Explanation: ***Wound infection***
- The patient presents with **fever**, worsening **lower abdominal pain**, **tachycardia**, and **local signs of inflammation** (redness around the surgical site, tenderness) one week post-hysterectomy, with a **leukocytosis and left shift** (elevated neutrophils and bands). These findings are highly characteristic of a common **post-surgical wound infection**.
- The lack of significant drainage initially does not rule out infection, and the symptoms are localized to the surgical area.
*Surgical error*
- The operative report and intraoperative cystoscopy indicated the surgery was **uncomplicated**, making an immediate post-operative surgical error less likely to be the primary cause of these symptoms.
- While complications can arise later, the current presentation points more directly to an infectious process rather than an unnoted immediate surgical complication.
*Post-operative ileus*
- Although bowel sounds are hypoactive, the patient is **tolerating an oral diet well** and denies nausea, vomiting, or abdominal distension, which are key symptoms of a clinically significant ileus.
- Her primary complaint is localized pain and systemic signs of infection, rather than generalized abdominal distension and inability to pass flatus or stool.
*Alcohol withdrawal*
- While the patient has a history of alcohol abuse, the primary symptoms (fever, localized abdominal pain, redness around the incision, leukocytosis) are more indicative of an **infectious process** than alcohol withdrawal.
- Alcohol withdrawal typically presents with tremors, agitation, hallucinations, and autonomic instability, and while some overlap (tachycardia) exists, the overall clinical picture doesn't fit.
*Urinary tract infection*
- The urine analysis shows **negative nitrites and leukocyte esterase**, with only 2 WBC/hpf, which makes a **urinary tract infection (UTI) highly unlikely** despite the presence of some bacteria (50 cfu/mL, which is often considered contamination in a clean catch).
- The patient's symptoms are also predominantly localized to the surgical wound area rather than dysuria, frequency, or urgency.
Hysterectomy techniques and indications US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Hysterectomy techniques and indications Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Hysterectomy techniques and indications US Medical PG Question 7: Thirty minutes after normal vaginal delivery of twins, a 35-year-old woman, gravida 5, para 4, has heavy vaginal bleeding with clots. Physical examination shows a soft, enlarged, and boggy uterus. Despite bimanual uterine massage, administration of uterotonic drugs, and placement of an intrauterine balloon for tamponade, the bleeding continues. A hysterectomy is performed. Vessels running through which of the following structures must be ligated during the surgery to achieve hemostasis?
- A. Suspensory ligament
- B. Round ligament
- C. Ovarian ligament
- D. Uterosacral ligament
- E. Cardinal ligament (Correct Answer)
Hysterectomy techniques and indications Explanation: ***Cardinal ligament***
- The **uterine artery** and **uterine vein**, which supply the uterus, run through the **cardinal ligament** (also known as the transverse cervical ligament).
- Ligation of these vessels is crucial during a hysterectomy to control bleeding from the uterus.
*Suspensory ligament*
- The **suspensory ligament of the ovary** contains the **ovarian artery** and vein, which primarily supply the ovaries and fallopian tubes.
- While these may be ligated during a hysterectomy if the ovaries are removed, they are not the primary vessels causing uterine bleeding in postpartum hemorrhage.
*Round ligament*
- The **round ligament of the uterus** extends from the uterus to the labia majora and contains relatively small vessels, primarily contributing to uterine support.
- Ligation of this ligament alone would not effectively control heavy uterine bleeding.
*Ovarian ligament*
- The **ovarian ligament** connects the ovary to the uterus and contains small vessels that mainly supply the ovary.
- It does not house the major blood supply to the uterus itself.
*Uterosacral ligament*
- The **uterosacral ligaments** primarily provide support to the uterus by connecting it to the sacrum and contain small nerves and vessels.
- Ligation of these ligaments would not control the main arterial supply to the uterus.
Hysterectomy techniques and indications US Medical PG Question 8: An 18-year-old woman presents to the emergency department with severe right lower quadrant discomfort and stomach pain for the past day. She has no significant past medical history. She states that she is sexually active and uses oral contraceptive pills for birth control. Her vital signs include: blood pressure 127/81 mm Hg, pulse 101/min, respiratory rate 19/min, and temperature 39.0°C (102.2°F). Abdominal examination is significant for focal tenderness and guarding in the right lower quadrant. Blood is drawn for lab tests which reveal the following:
Hb% 13 gm/dL
Total count (WBC) 15,400 /mm3
Differential count
Neutrophils:
Segmented 70%
Band Form 5%
Lymphocytes 20%
Monocytes 5%
What is the next best step in the management of this patient?
- A. Upper gastrointestinal series
- B. Pelvic exam
- C. Ultrasound of the appendix
- D. Upper gastrointestinal endoscopy
- E. Ultrasound of the pelvis (Correct Answer)
Hysterectomy techniques and indications Explanation: ***Ultrasound of the pelvis***
- In a young woman presenting with **right lower quadrant pain, fever, leukocytosis with left shift, and peritoneal signs (guarding)**, the next best step is **pelvic ultrasound**.
- This imaging modality can evaluate **both surgical and gynecological causes** of acute abdomen, including **appendicitis, ovarian torsion, tubo-ovarian abscess, ectopic pregnancy**, and **ruptured ovarian cyst**.
- **Pelvic ultrasound is the first-line imaging** for RLQ pain in women of reproductive age because it avoids radiation and provides comprehensive evaluation of pelvic structures.
- The clinical picture (high fever 39°C, significant leukocytosis 15,400 with left shift, guarding) suggests **acute appendicitis** as the most likely diagnosis, but gynecological emergencies must also be excluded.
*Pelvic exam*
- While important in evaluating gynecological causes, a **pelvic exam should not precede imaging** in a patient with peritoneal signs (guarding) and high suspicion for surgical emergency.
- In the setting of acute abdomen with fever and leukocytosis, **imaging takes priority** to identify the source and guide management.
- Pelvic exam would be appropriate **after imaging** if gynecological pathology is identified or if there are specific findings suggesting PID (bilateral pain, cervical discharge).
- The presentation is more consistent with **appendicitis than PID**, which typically causes bilateral lower abdominal pain and cervical motion tenderness.
*Upper gastrointestinal series*
- An **upper GI series** uses X-rays and contrast to visualize the esophagus, stomach, and duodenum.
- It is indicated for evaluating **GERD, peptic ulcer disease, or dysphagia**, which are not suggested by this patient's acute RLQ pain and fever.
- This would be inappropriate for acute abdominal pain with peritoneal signs.
*Upper gastrointestinal endoscopy*
- This procedure directly visualizes the upper GI tract to diagnose **esophagitis, gastric ulcers, or malignancy**.
- It has no role in the evaluation of acute **lower quadrant pain** with systemic inflammatory signs.
- This would delay appropriate diagnosis and treatment of a surgical emergency.
*Ultrasound of the appendix*
- While **ultrasound can visualize the appendix**, a **pelvic ultrasound** is preferred because it provides a **comprehensive evaluation** of both the appendix and gynecological structures.
- In women of reproductive age with RLQ pain, gynecological causes must be excluded, making **pelvic ultrasound more appropriate** than focusing solely on the appendix.
- If pelvic ultrasound is inconclusive for appendicitis, **CT abdomen/pelvis with contrast** would be the next step.
Hysterectomy techniques and indications US Medical PG Question 9: A 67-year-old woman with endometrial cancer undergoes robotic-assisted staging surgery. Final pathology reveals grade 2 endometrioid adenocarcinoma with 60% myometrial invasion, positive pelvic lymph nodes (2/15), negative para-aortic nodes (0/8), and lymphovascular space invasion. No cervical or adnexal involvement. The tumor care team debates adjuvant treatment. Evaluate which combination of pathologic features most significantly impacts treatment recommendations?
- A. Grade 2 histology and depth of myometrial invasion
- B. Number of positive nodes and total nodes removed
- C. Lymphovascular space invasion and myometrial invasion depth
- D. Positive pelvic nodes and negative para-aortic nodes (Correct Answer)
- E. Absence of cervical involvement and patient age
Hysterectomy techniques and indications Explanation: ***Positive pelvic nodes and negative para-aortic nodes***
- The presence of positive pelvic lymph nodes classifies this as **FIGO Stage IIIC1** disease, which is the primary driver for recommending **systemic chemotherapy**.
- The negative para-aortic nodes help delineate the **radiation field**, focusing treatment on the pelvis rather than extended-field radiation, thus making this combination critical for the management plan.
*Grade 2 histology and depth of myometrial invasion*
- While these factors contribute to the **GOG-99** or **PORTEC** risk criteria for early-stage disease, they are superseded by the presence of **nodal metastasis** (Stage IIIC).
- Myometrial invasion (>50%) and Grade 2 are baseline risk factors, but they do not dictate the switch from local to **systemic therapy** once nodes are positive.
*Number of positive nodes and total nodes removed*
- The **lymph node count** (2/15) confirms the stage but does not change the treatment algorithm as much as the **anatomical location** (pelvic vs. para-aortic) of those nodes.
- While a low total node count might suggest staging inadequacy, Stage IIIC status is already established here, making the **distribution** more clinically significant for therapy planning.
*Lymphovascular space invasion and myometrial invasion depth*
- **Lymphovascular space invasion (LVSI)** is a strong prognostic indicator for recurrence, but it is often a precursor to the nodal involvement already identified in this patient.
- These features are used to justify **adjuvant therapy** in early-stage (Stage I) patients, but nodal status is a more powerful determinant in Stage III disease.
*Absence of cervical involvement and patient age*
- The lack of **cervical stromal invasion** means the patient is not Stage II, but this is less impactful than the upgrade to **Stage IIIC** due to positive nodes.
- **Patient age** is a clinical factor used in risk-stratification models like **GOG-99**, but it does not outweigh the pathological finding of **metastasized disease** in treatment selection.
Hysterectomy techniques and indications US Medical PG Question 10: A 29-year-old woman with stage IA1 cervical cancer (3 mm invasion, no LVSI) desires fertility preservation. She has one child and wants more children. Cone biopsy margins are positive. Imaging shows no lymph node involvement. Her oncologist recommends radical hysterectomy, while a fertility specialist suggests radical trachelectomy. The patient strongly desires future pregnancy. Evaluate the optimal management strategy balancing oncologic and reproductive outcomes.
- A. Repeat cone biopsy followed by close surveillance (Correct Answer)
- B. Radical hysterectomy given positive margins
- C. Simple trachelectomy with sentinel lymph node biopsy
- D. Radical trachelectomy with pelvic lymphadenectomy
- E. Neoadjuvant chemotherapy followed by conservative surgery
Hysterectomy techniques and indications Explanation: ***Repeat cone biopsy followed by close surveillance***
- In **Stage IA1** cervical cancer without **lymphovascular space invasion (LVSI)**, achieving **negative margins** via a repeat conization is standard to ensure all microscopic disease is removed while preserving the uterus.
- This approach is the most conservative and effective strategy for **fertility preservation**, as the risk of **lymph node metastasis** is less than 1% in this specific pathological subgroup.
*Radical hysterectomy given positive margins*
- This procedure provides definitive oncologic treatment but results in **permanent infertility**, which violates the patient's strong preference for **fertility preservation**.
- Radical surgery is considered **overtreatment** for Stage IA1 disease without LVSI, provided that negative margins can be achieved through additional local excision.
*Simple trachelectomy with sentinel lymph node biopsy*
- While a trachelectomy preserves fertility, a **simple trachelectomy** would still leave the positive margins from the initial cone biopsy untreated if not mapped correctly.
- **Sentinel lymph node biopsy** is generally not required for Stage IA1 disease lacking LVSI because the risk of nodal involvement is extremely low.
*Radical trachelectomy with pelvic lymphadenectomy*
- This is an extensive procedure typically reserved for **Stage IA2 to IB1** disease or Stage IA1 with **positive LVSI**, making it too aggressive for this patient's diagnosis.
- It carries higher risks of surgical morbidity and **obstetric complications**, such as preterm labor and cervical insufficiency, compared to a repeat cone biopsy.
*Neoadjuvant chemotherapy followed by conservative surgery*
- **Neoadjuvant chemotherapy (NACT)** is not an indicated or standard treatment for early-stage (IA1) cervical cancer with minimal stromal invasion.
- NACT is typically explored in research settings for **bulky Stage IB** tumors to shrink them prior to performing **fertility-sparing surgery**, which does not apply here.
More Hysterectomy techniques and indications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.