Gynecologic cancer staging procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gynecologic cancer staging procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gynecologic cancer staging procedures US Medical PG Question 1: A 33-year-old woman comes to the emergency department because of a 1-hour history of severe pelvic pain and nausea. She was diagnosed with a follicular cyst in the left ovary 3 months ago. The cyst was found incidentally during a fertility evaluation. A pelvic ultrasound with Doppler flow shows an enlarged, edematous left ovary with no blood flow. Laparoscopic evaluation shows necrosis of the left ovary, and a left oophorectomy is performed. During the procedure, blunt dissection of the left infundibulopelvic ligament is performed. Which of the following structures is most at risk of injury during this step of the surgery?
- A. Bladder trigone
- B. Uterine artery
- C. Kidney
- D. Ureter (Correct Answer)
Gynecologic cancer staging procedures Explanation: ***Ureter***
- The **infundibulopelvic ligament** (also known as the suspensory ligament of the ovary) contains the **ovarian artery and vein** and is in close proximity to the ureter as it crosses the pelvic brim.
- During dissection or clamping of this ligament, especially in an emergency setting or when anatomy is distorted (e.g., by an enlarged ovary or edema), the **ureter** is highly susceptible to injury.
*Bladder trigone*
- The **bladder trigone** is the smooth triangular region at the base of the bladder, formed by the openings of the ureters and the internal urethral orifice.
- It is not directly adjacent to the infundibulopelvic ligament and is therefore at a comparably lower risk of injury during dissection of this ligament.
*Uterine artery*
- The **uterine artery** travels within the cardinal ligament and supplies the uterus; it is located more medially and inferiorly within the broad ligament.
- While important in pelvic surgery, it is not in the immediate vicinity of the infundibulopelvic ligament dissection itself.
*Kidney*
- The **kidneys** are retroperitoneal organs located much higher in the abdominal cavity, far superior to the pelvis.
- They are not at risk of direct injury during pelvic surgery involving the infundibulopelvic ligament.
Gynecologic cancer staging procedures US Medical PG Question 2: A 64-year-old woman presents to the surgical oncology clinic as a new patient for evaluation of recently diagnosed breast cancer. She has a medical history of type 2 diabetes mellitus for which she takes metformin. Her surgical history is a total knee arthroplasty 7 years ago. Her family history is insignificant. Physical examination is notable for an irregular nodule near the surface of her right breast. Her primary concern today is which surgical approach will be chosen to remove her breast cancer. Which of the following procedures involves the removal of a portion of a breast?
- A. Arthroplasty
- B. Lumpectomy (Correct Answer)
- C. Vasectomy
- D. Mastectomy
- E. Laminectomy
Gynecologic cancer staging procedures Explanation: ***Lumpectomy***
- A **lumpectomy** is a surgical procedure that removes the **breast cancer tumor** and a small margin of surrounding healthy tissue, preserving most of the breast.
- This procedure is a common treatment for early-stage breast cancer and is often followed by radiation therapy.
*Arthroplasty*
- **Arthroplasty** is a surgical procedure to **repair or replace a joint**, typically due to arthritis or injury.
- The patient's history of a total knee arthroplasty indicates this procedure was performed on her knee, not her breast.
*Vasectomy*
- A **vasectomy** is a surgical procedure for **male sterilization**, involving the cutting and sealing of the vas deferens.
- This procedure is unrelated to breast cancer treatment or breast surgery.
*Mastectomy*
- A **mastectomy** involves the **complete surgical removal of the entire breast**, often including the nipple and areola.
- While it is a breast surgery, it removes the *entire* breast, not just a portion.
*Laminectomy*
- A **laminectomy** is a surgical procedure that removes a portion of the **vertebra (lamina)** to relieve pressure on the spinal cord or nerves.
- This procedure is for spinal conditions and is entirely unrelated to breast cancer surgery.
Gynecologic cancer staging procedures US Medical PG Question 3: A 62-year-old woman presents to the clinic for postmenopausal bleeding for the past month. She reports that the bleeding often occurs after intercourse with her husband. The patient denies fever, weight loss, chills, chest pain, abdominal pain, or shortness of breath but endorses mild dyspareunia and vaginal discharge. Her past medical history is significant for human papilloma virus and cervical cancer that was treated with surgical resection and radiation 5 years ago. Physical examination is unremarkable except for an irregular mass protruding from the vaginal wall. What is the most likely explanation for this patient’s condition?
- A. Metastasis of cervical cancer via direct extension (Correct Answer)
- B. Primary malignancy of endometrial cells
- C. Atrophy of vaginal tissues secondary to old age
- D. Metastasis of cervical cancer via hematogenous spread
- E. Primary malignancy of vaginal squamous cells
Gynecologic cancer staging procedures Explanation: ***Metastasis of cervical cancer via direct extension***
- The patient has a history of **cervical cancer** and now presents with an **irregular mass protruding from the vaginal wall**, along with postmenopausal bleeding and dyspareunia. This clinical picture is highly suggestive of **local recurrence or direct extension** of the cervical cancer to the vagina.
- Cervical cancer commonly spreads to adjacent structures like the vagina, which would explain the symptoms of **postmenopausal bleeding, dyspareunia, and an irregular mass** in the vaginal wall.
*Primary malignancy of endometrial cells*
- While postmenopausal bleeding is a classic symptom of **endometrial cancer**, the presence of an **irregular mass protruding from the vaginal wall** makes this diagnosis less likely as the primary cause.
- Endometrial cancer usually causes bleeding directly from the uterus and typically presents with a uterine mass or thickening, not a visible vaginal mass unless it has already broadly metastasized.
*Atrophy of vaginal tissues secondary to old age*
- **Vaginal atrophy** can cause postmenopausal bleeding and dyspareunia, but it typically presents as **thin, pale, and dry vaginal tissues**, not an **irregular mass**.
- The presence of a palpable mass strongly points away from atrophy as the sole explanation.
*Metastasis of cervical cancer via hematogenous spread*
- While cervical cancer can metastasize hematogenously, **hematogenous spread** typically leads to distant metastases in organs like the lungs, liver, or bones, not usually to a localized, protruding vaginal mass.
- The presentation of a mass directly in the vagina points more towards **local extension** rather than distant hematogenous spread to a new primary site.
*Primary malignancy of vaginal squamous cells*
- Primary vaginal cancer is a possibility given the symptoms and a history of HPV, but the patient's prior diagnosis and treatment for **cervical cancer** 5 years ago make **recurrent or metastatic cervical cancer** a more likely explanation for a vaginal mass presenting in this manner.
- It is reasonable to assume a connection between the previous cervical cancer and the current vaginal lesion given the proximity and timing, suggesting recurrence or metastasis rather than a de novo primary vaginal cancer.
Gynecologic cancer staging procedures US Medical PG Question 4: Patient 1 – A 26-year-old woman presents to her primary care physician for an annual exam. She currently does not have any acute concerns and says her health has been generally well. Medical history is significant for asthma, which is managed with an albuterol inhaler. Her last pap smear was unremarkable. She is currently sexually active with one male and consistently uses condoms. She occasionally smokes marijuana and drinks wine once per week. Her mother recently passed away from advanced ovarian cancer. Her sister is 37-years-old and was recently diagnosed with breast cancer and ovarian cancer. Physical examination is remarkable for a mildly anxious woman.
Patient 2 – A 27-year-old woman presents to her primary care physician for an annual exam. She says that she would like to be screened for breast cancer since two of her close friends were recently diagnosed. She noticed she has a small and mobile mass on her left breast, which increases in size and becomes tender around her time of menses. Family history is remarkable for hypertension in the father. The physical exam is significant for a small, well-defined, and mobile mass on her left breast that is not tender to palpation.
Which of the following is the best next step in management for patient 1 and 2?
- A. Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam
- B. Patient 1 – Reassurance. Patient 2 – Breast ultrasound
- C. Patient 1 – CA-125 testing. Patient 2 – BRCA testing
- D. Patient 1 – BRCA testing. Patient 2 – Breast ultrasound (Correct Answer)
- E. Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography
Gynecologic cancer staging procedures Explanation: ***Patient 1 – BRCA testing. Patient 2 – Breast ultrasound***
- Patient 1 has a strong family history of early-onset **breast and ovarian cancer** (**mother and sister**), suggesting a high probability of an inherited genetic mutation, such as **BRCA1/2**, which warrants genetic testing.
- Patient 2 presents with a **small, mobile, well-defined breast mass** that is likely benign, and a **breast ultrasound** is the appropriate initial imaging for further characterization in a young woman.
*Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam*
- Patient 1's primary concern is genetic predisposition due to family history, an **ultrasound** is not the initial or primary screening method for future cancer risk.
- Patient 2 has a palpable mass; waiting 3 months for a **clinical breast exam** without initial imaging (ultrasound) is not appropriate for evaluating a new breast lump.
*Patient 1 – Reassurance. Patient 2 – Breast ultrasound*
- Patient 1's family history of **early-onset breast and ovarian cancer** is a significant risk factor; therefore, simple **reassurance** without further investigation is inappropriate.
- While a **breast ultrasound** is appropriate for Patient 2, the recommendation for Patient 1 is incorrect.
*Patient 1 – CA-125 testing. Patient 2 – BRCA testing*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer treatment or recurrence, not for initial screening in asymptomatic individuals, especially in a young woman with no active symptoms.
- **BRCA testing** is indicated for Patient 1 due to family history, but not for Patient 2 who has a likely benign breast mass and no significant family history.
*Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography*
- Regular **breast and ovarian ultrasounds** are not recommended as primary screening tools for genetic risk in asymptomatic high-risk individuals like Patient 1.
- **Mammography** is less sensitive in young women (under 30) due to higher breast tissue density, making **ultrasound** the preferred initial imaging for Patient 2.
Gynecologic cancer staging procedures US Medical PG Question 5: A 31-year-old female presents to her gynecologist for a routine Pap smear. Her last Pap smear was three years ago and was normal. On the current Pap smear, she is found to have atypical squamous cells of unknown significance (ASCUS). Reflex HPV testing is positive. What is the best next step?
- A. Colposcopy (Correct Answer)
- B. Repeat Pap smear and HPV testing in 5 years
- C. Repeat Pap smear in 3 years
- D. Repeat Pap smear in 1 year
- E. Loop electrosurgical excision procedure (LEEP)
Gynecologic cancer staging procedures Explanation: ***Colposcopy***
- A **colposcopy** is indicated for a patient over 25 with **atypical squamous cells of undetermined significance (ASCUS)** and a **positive high-risk human papillomavirus (HPV) test** to evaluate for cervical intraepithelial neoplasia (CIN).
- The positive HPV test suggests a higher risk of underlying cervical disease requiring direct visualization and potentially biopsy of abnormal areas.
*Repeat Pap smear and HPV testing in 5 years*
- This option is incorrect because a **positive HPV test** along with ASCUS indicates a need for more immediate and invasive evaluation than routine screening.
- Waiting five years could allow progression of potential **cervical dysplasia** without intervention.
*Repeat Pap smear in 3 years*
- This timeframe is typically for women aged 21-29 with a normal Pap smear and negative HPV, or for follow-up after low-grade abnormalities, not for ASCUS with positive HPV.
- The presence of **high-risk HPV** mandates a more aggressive follow-up strategy.
*Repeat Pap smear in 1 year*
- This might be an option for ASCUS with a **negative HPV test** or for adolescents, but it is insufficient when high-risk HPV is positive.
- A **high-risk HPV infection** following an ASCUS result requires colposcopy to rule out significant cervical lesions.
*Loop electrosurgical excision procedure (LEEP)*
- A **LEEP** is a therapeutic procedure used to remove abnormal cervical tissue, usually performed after a colposcopy and biopsy confirms a high-grade lesion (CIN 2 or 3).
- Performing a LEEP immediately without a preceding colposcopy and biopsy would be **premature** as the diagnosis of the severity of cervical changes is not yet confirmed.
Gynecologic cancer staging procedures US Medical PG Question 6: A 24-year-old woman comes to the physician for a routine pelvic examination. She feels well. Menses occur at 30-day intervals and last 7 days. Her last menstrual period was 6 days ago. She has no history of abnormal Pap smears; her last Pap smear was 13 months ago. She is sexually active with three male partners and uses condoms consistently. She has never been tested for sexually transmitted infections. Her 54-year-old mother has breast cancer. She is up-to-date on her Tdap, MMR, and varicella vaccinations. Her temperature is 37.1°C (98.8°F), pulse is 68/min, and blood pressure is 108/68 mm Hg. Physical examination shows no abnormalities. In addition to HIV, gonorrhea, and chlamydia testing, which of the following is the most appropriate recommendation at this time?
- A. HPV vaccination (Correct Answer)
- B. Mammography
- C. HPV testing
- D. Pregnancy test
- E. Syphilis testing
Gynecologic cancer staging procedures Explanation: ***HPV vaccination***
- This patient is 24 years old, which is within the recommended age range for **HPV vaccination** (**up to age 26** for catch-up vaccination).
- Her multiple sexual partners and consistent condom use do not eliminate the risk of HPV infection, making vaccination a crucial preventive measure against **cervical cancer** and other HPV-related conditions.
*Mammography*
- **Mammography screening** is typically recommended starting at age 40 or 50, although earlier screening may be considered for high-risk individuals.
- While her mother has breast cancer, the patient's young age of 24 makes mammography generally **not indicated** at this time, as the risk-benefit profile does not favor early screening without other significant risk factors or symptoms.
*HPV testing*
- **HPV testing** is typically recommended as part of cervical cancer screening for women **aged 30 and older**, either alone or co-tested with a Pap smear.
- At age 24, a Pap smear alone is generally sufficient if recommended, and HPV testing is not routinely performed unless the Pap smear results are abnormal.
*Pregnancy test*
- The patient reports regular menses at 30-day intervals, with her last menstrual period occurring 6 days ago, indicating she is currently **menstruating or recently finished** her period.
- There are no symptoms suggestive of pregnancy, making a pregnancy test **unnecessary** at this routine visit.
*Syphilis testing*
- While the patient is sexually active with multiple partners, increasing her risk for STIs, **syphilis testing** was not explicitly mentioned as a recommended additional test in the question's premise.
- The question asks for the *most appropriate additional recommendation* beyond HIV, gonorrhea, and chlamydia testing, implying a focus on broad preventative health or screening not already covered.
Gynecologic cancer staging procedures US Medical PG Question 7: A 47-year-old woman comes to the physician for a mass in her left breast she noticed 2 days ago during breast self-examination. She has hypothyroidism treated with levothyroxine. There is no family history of breast cancer. Examination shows large, moderately ptotic breasts. The mass in her left breast is small (approximately 1 cm x 0.5 cm), firm, mobile, and painless. It is located 4 cm from her nipple-areolar complex at the 7 o'clock position. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. No masses are palpable in her right breast. A urine pregnancy test is negative. Mammogram showed a soft tissue mass with poorly defined margins. Core needle biopsy confirms a low-grade infiltrating ductal carcinoma. The pathological specimen is positive for estrogen receptors and negative for progesterone and human epidermal growth factor receptor 2 (HER2) receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate next step in management?
- A. Lumpectomy with sentinel lymph node biopsy followed by hormone therapy
- B. Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy
- C. Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy
- D. Radical mastectomy followed by hormone therapy
- E. Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy (Correct Answer)
Gynecologic cancer staging procedures Explanation: **Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy**
- The patient has **early-stage (T1N0M0) estrogen receptor (ER)-positive, HER2-negative invasive ductal carcinoma** suitable for **breast-conserving surgery (lumpectomy)**.
- **Lumpectomy** must be followed by **radiation therapy** to the remaining breast tissue to reduce the risk of local recurrence, and **endocrine therapy** (due to ER positivity) is indicated to reduce systemic recurrence risk.
- **Sentinel lymph node biopsy** is performed to stage the axilla; if positive, an axillary lymph node dissection may be indicated. However, in this case, the mass is small, and there is no palpable axillary adenopathy, making sentinel lymph node biopsy the appropriate initial step.
*Lumpectomy with sentinel lymph node biopsy followed by hormone therapy*
- While **lumpectomy with sentinel lymph node biopsy** and **hormone therapy** are part of the appropriate management, **radiation therapy** to the conserved breast is a critical component that is missing from this option.
- Omitting **radiation therapy** after lumpectomy for invasive breast cancer significantly increases the risk of local recurrence.
*Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy*
- A **nipple-sparing mastectomy** is a more aggressive surgical approach than typically required for a **small, early-stage tumor** like this, which is amenable to breast-conserving surgery.
- **Axillary lymph node dissection** is usually reserved for cases with clinically positive lymph nodes or a positive sentinel lymph node biopsy, not as an initial step when there is no palpable axillary adenopathy.
*Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy*
- This option involves an **unnecessarily extensive surgical procedure (nipple-sparing mastectomy with axillary lymph node dissection)** for a **small (1cm x 0.5cm) early-stage tumor** that can be managed with breast-conserving therapy.
- While radiation and hormone therapy are relevant, the initial surgical choice is too aggressive given the clinical presentation.
*Radical mastectomy followed by hormone therapy*
- **Radical mastectomy** (which includes removal of the breast, underlying chest muscle, and axillary lymph nodes) is rarely performed today due to its significant morbidity and is not indicated for this **early-stage tumor**.
- **Modified radical mastectomy**, which removes the breast and axillary lymph nodes while preserving the chest muscle, is typically only considered if breast-conserving surgery is not feasible or desired, and **hormone therapy** would be indicated, but **radiation** may also be needed depending on other factors.
Gynecologic cancer staging procedures US Medical PG Question 8: A 13-year-old boy is brought to the emergency department by his mother because of vomiting and severe testicular pain for 3 hours. The boy has had 4–5 episodes of vomiting during this period. He has never had a similar episode in the past and takes no medications. His father died of testicular cancer at the age of 50. His immunizations are up-to-date. He appears anxious and uncomfortable. His temperature is 37°C (98.6°F), pulse is 90/min, respirations are 14/min, and blood pressure is 100/60 mm Hg. Cardiopulmonary examination shows no abnormalities The abdomen is soft and nondistended. The left scrotum is firm, erythematous, and swollen. There is severe tenderness on palpation of the scrotum that persists on elevation of the testes. Stroking the inner side of the left thigh fails to elicit elevation of the scrotum. Which of the following is the most appropriate next step in management?
- A. Urine dipstick
- B. Ceftriaxone and doxycycline therapy
- C. Close observation
- D. CT scan of the abdomen and pelvis
- E. Surgical exploration of the scrotum (Correct Answer)
Gynecologic cancer staging procedures Explanation: ***Surgical exploration of the scrotum***
- The sudden onset of severe testicular pain, vomiting, an **absent cremasteric reflex**, and testicular tenderness that **persists on elevation (negative Prehn's sign)** are highly suggestive of **testicular torsion**.
- **Testicular torsion** is a surgical emergency requiring immediate exploration to salvage the testis; delaying surgery beyond 6-8 hours significantly increases the risk of **testicular ischemia** and necrosis.
*Urine dipstick*
- While a **urine dipstick** can help rule out a **urinary tract infection** or **epididymitis**, these conditions typically present with more gradual pain and often have associated urinary symptoms, which are not the primary concern here.
- Delaying definitive treatment for a suspected **testicular torsion** by performing non-urgent diagnostic tests can lead to irreversible damage to the testis.
*Ceftriaxone and doxycycline therapy*
- This antibiotic regimen is typically used to treat **epididymitis** or **orchitis**, especially in sexually active adolescents, or cases suspected of bacterial infection.
- The acute, severe nature of the pain and the absence of fever or urinary symptoms make **bacterial epididymitis** less likely, and administering antibiotics would delay the critical intervention needed for **testicular torsion**.
*Close observation*
- **Close observation** is inappropriate given the highly suspicious symptoms of **testicular torsion**, which is a time-sensitive emergency.
- Delaying intervention can result in irreversible **ischemic damage** to the testicle, leading to its loss.
*CT scan of the abdomen and pelvis*
- A **CT scan** is not the appropriate initial diagnostic step for acute scrotal pain; it exposes the patient to radiation and would delay definitive diagnosis and treatment.
- While it could identify other sources of abdominal pain, the clinical presentation is characteristic of a local scrotal pathology, and **ultrasound with Doppler** is preferred if imaging is needed to confirm **testicular torsion**, though clinical suspicion often warrants direct surgical exploration.
Gynecologic cancer staging procedures US Medical PG Question 9: A 27-year-old man is brought to the emergency department by ambulance following a motor vehicle accident 1 hour prior. He appears agitated. His blood pressure is 85/60 mm Hg, the pulse is 110/min, and the respiratory rate is 19/min. Physical examination shows bruising of the left flank and fracture of the left lower thoracic bones. Strict bed rest and monitoring with intravenous fluids is initiated. Urinalysis shows numerous RBCs. A contrast-enhanced CT scan shows normal enhancement of the right kidney. The left renal artery is only visible in the proximal section with a small amount of extravasated blood around the left kidney. The left kidney shows no enhancement. Imaging of the spleen shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Immediate surgical exploration (Correct Answer)
- B. Observation with delayed repair
- C. Conservative management
- D. Renal artery embolization
- E. Renal artery embolization with delayed nephrectomy
Gynecologic cancer staging procedures Explanation: ***Immediate surgical exploration***
- The patient presents with signs of **hemodynamic instability** (BP 85/60, pulse 110/min, agitation) and imaging findings consistent with **left renal artery avulsion** and devascularization (no enhancement of the left kidney, visible only proximally, extravasated blood). These findings necessitate immediate surgical intervention to control hemorrhage and assess kidney viability.
- The goal is to revascularize the kidney if possible, perform a nephrectomy if the kidney is unsalvageable, and manage hemorrhage to stabilize the patient.
*Observation with delayed repair*
- This approach is typically reserved for **hemodynamically stable** patients with renal injuries, especially lower-grade injuries that do not involve complete vessel avulsion or ongoing significant hemorrhage.
- Delaying intervention in a hemodynamically unstable patient with a presumed renal artery avulsion can lead to further decompensation, irreversible kidney damage, and increased mortality.
*Conservative management*
- **Conservative management** is appropriate for hemodynamically stable patients with minor renal injuries, such as contusions or small lacerations, or for very selected cases of more severe injuries that have spontaneously tamponaded and are not causing significant clinical compromise.
- The patient's **hemodynamic instability** and direct evidence of renal artery injury preclude conservative management in this case.
*Renal artery embolization*
- **Renal artery embolization** is a highly effective, minimally invasive technique for controlling bleeding from renal injuries. However, it is primarily indicated for **hemodynamically stable patients** with contained hemorrhage or specific pseudoaneurysms/AV fistulas.
- In a hemodynamically unstable patient with a complete renal artery avulsion and non-perfused kidney, embolization is unlikely to revascularize the kidney and may even hinder subsequent surgical repair if revascularization is deemed possible. Furthermore, it might not be sufficient to control diffuse or extensive bleeding associated with avulsion.
*Renal artery embolization with delayed nephrectomy*
- While embolization can precede nephrectomy in certain scenarios for better hemorrhage control, it is not the primary immediate step in a **hemodynamically unstable** patient with renal artery avulsion and a non-enhancing kidney.
- The primary concern is the patient's instability, which requires immediate surgical control, and delaying nephrectomy after embolization often isn't feasible if the kidney is completely devascularized and the patient is unstable. The decision for nephrectomy typically occurs during the initial surgical exploration.
Gynecologic cancer staging procedures US Medical PG Question 10: A 67-year-old woman with endometrial cancer undergoes robotic-assisted staging surgery. Final pathology reveals grade 2 endometrioid adenocarcinoma with 60% myometrial invasion, positive pelvic lymph nodes (2/15), negative para-aortic nodes (0/8), and lymphovascular space invasion. No cervical or adnexal involvement. The tumor care team debates adjuvant treatment. Evaluate which combination of pathologic features most significantly impacts treatment recommendations?
- A. Grade 2 histology and depth of myometrial invasion
- B. Number of positive nodes and total nodes removed
- C. Lymphovascular space invasion and myometrial invasion depth
- D. Positive pelvic nodes and negative para-aortic nodes (Correct Answer)
- E. Absence of cervical involvement and patient age
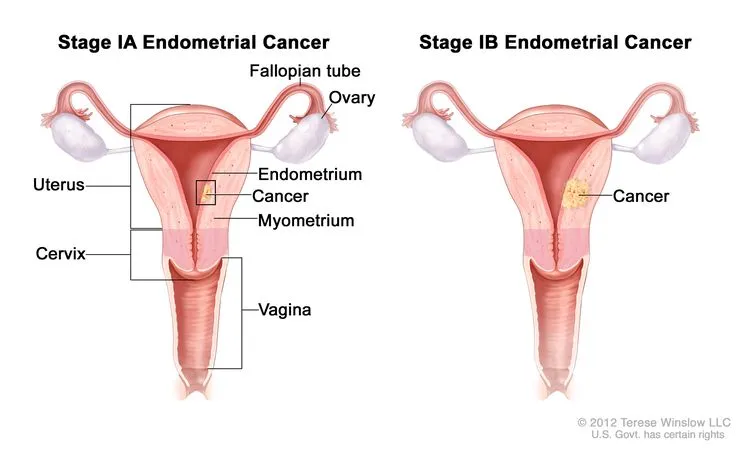
Gynecologic cancer staging procedures Explanation: ***Positive pelvic nodes and negative para-aortic nodes***
- The presence of positive pelvic lymph nodes classifies this as **FIGO Stage IIIC1** disease, which is the primary driver for recommending **systemic chemotherapy**.
- The negative para-aortic nodes help delineate the **radiation field**, focusing treatment on the pelvis rather than extended-field radiation, thus making this combination critical for the management plan.
*Grade 2 histology and depth of myometrial invasion*
- While these factors contribute to the **GOG-99** or **PORTEC** risk criteria for early-stage disease, they are superseded by the presence of **nodal metastasis** (Stage IIIC).
- Myometrial invasion (>50%) and Grade 2 are baseline risk factors, but they do not dictate the switch from local to **systemic therapy** once nodes are positive.
*Number of positive nodes and total nodes removed*
- The **lymph node count** (2/15) confirms the stage but does not change the treatment algorithm as much as the **anatomical location** (pelvic vs. para-aortic) of those nodes.
- While a low total node count might suggest staging inadequacy, Stage IIIC status is already established here, making the **distribution** more clinically significant for therapy planning.
*Lymphovascular space invasion and myometrial invasion depth*
- **Lymphovascular space invasion (LVSI)** is a strong prognostic indicator for recurrence, but it is often a precursor to the nodal involvement already identified in this patient.
- These features are used to justify **adjuvant therapy** in early-stage (Stage I) patients, but nodal status is a more powerful determinant in Stage III disease.
*Absence of cervical involvement and patient age*
- The lack of **cervical stromal invasion** means the patient is not Stage II, but this is less impactful than the upgrade to **Stage IIIC** due to positive nodes.
- **Patient age** is a clinical factor used in risk-stratification models like **GOG-99**, but it does not outweigh the pathological finding of **metastasized disease** in treatment selection.
More Gynecologic cancer staging procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.