Endometriosis surgical management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Endometriosis surgical management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Endometriosis surgical management US Medical PG Question 1: A 32-year-old woman visits her family physician for a routine health check-up. During the consult, she complains about recent-onset constipation, painful defecation, and occasional pain with micturition for the past few months. Her menstrual cycles have always been regular with moderate pelvic pain during menses, which is relieved with pain medication. However, in the last 6 months, she has noticed that her menses are “heavier” with severe lower abdominal cramps that linger for 4–5 days after the last day of menstruation. She and her husband are trying to conceive a second child, but lately, she has been unable to have sexual intercourse due to pain during sexual intercourse. During the physical examination, she has tenderness in the lower abdomen with no palpable mass. Pelvic examination reveals a left-deviated tender cervix, a tender retroverted uterus, and a left adnexal mass. During the rectovaginal examination, nodules are noted. What is the most likely diagnosis for this patient?
- A. Endometriosis (Correct Answer)
- B. Ovarian cyst
- C. Pelvic inflammatory disease (PID)
- D. Diverticulitis
- E. Irritable bowel syndrome (IBS)
Endometriosis surgical management Explanation: ***Endometriosis***
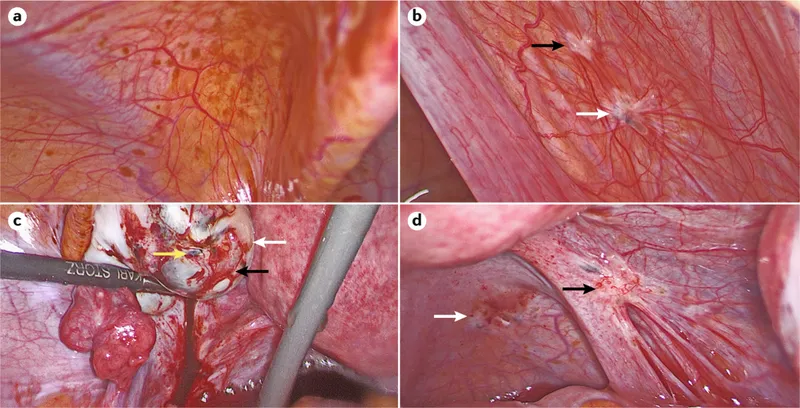
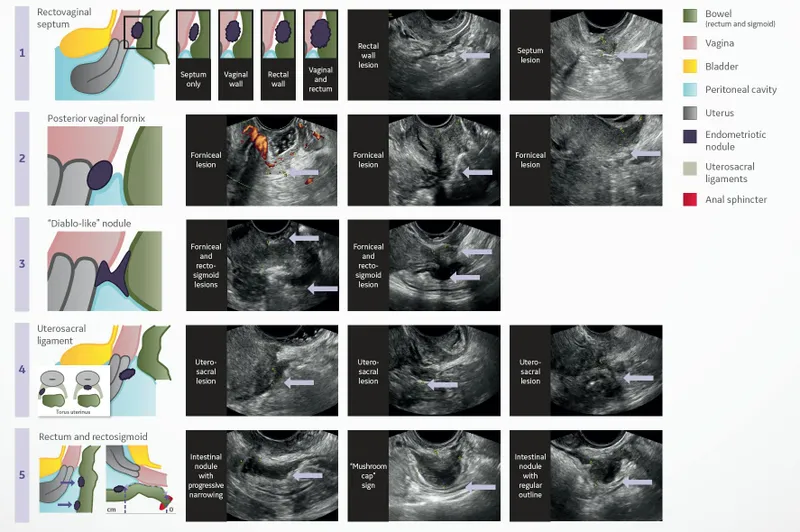
- The constellation of **dysmenorrhea** (severe lower abdominal cramps, heavy menses), **dyspareunia** (pain with sexual intercourse), and **dyschezia** (painful defecation) with rectovaginal nodularity suggests endometriosis.
- The physical examination findings of a **left-deviated tender cervix**, **tender retroverted uterus**, and a **left adnexal mass** further support the diagnosis of endometriosis, as implants can cause retroversion of the uterus and form endometriomas.
*Ovarian cyst*
- While an **adnexal mass** is present, an ovarian cyst typically does not explain the full spectrum of symptoms like severe dysmenorrhea, dyspareunia, dyschezia, or rectovaginal nodules.
- Most ovarian cysts are asymptomatic or cause only localized pain; they do not typically cause progressive **dysmenorrhea** or **deep dyspareunia**.
*Pelvic inflammatory disease (PID)*
- PID is characterized by **acute pelvic pain**, fever, and cervical motion tenderness, often following a sexually transmitted infection.
- This patient presents with chronic symptoms, no fever, and a history more consistent with **endometriosis implants** causing pain rather than infection.
*Diverticulitis*
- Diverticulitis typically presents with **left lower quadrant abdominal pain**, fever, and changes in bowel habits, but usually not with severe dysmenorrhea or dyspareunia.
- The rectovaginal nodules and ovarian mass are not typical findings for **diverticulitis**.
*Irritable bowel syndrome (IBS)*
- While **constipation**, abdominal pain, and painful defecation can be symptoms of IBS, it does not explain the severe dysmenorrhea, dyspareunia, or the physical examination findings such as the adnexal mass, tender cervix, or rectovaginal nodules.
- IBS is a **functional bowel disorder** and usually lacks the structural abnormalities found on examination here.
Endometriosis surgical management US Medical PG Question 2: A 31-year-old female presents to her gynecologist with spotting between periods. She reports that her menses began at age 11, and she has never had spotting prior to the three months ago. Her medical history is significant for estrogen-receptor positive intraductal carcinoma of the breast, which was treated with tamoxifen. An endometrial biopsy is performed, which shows endometrial hyperplasia with atypia. She reports that she and her husband are currently trying to have children. What is the next best step?
- A. Start progestin-only therapy (Correct Answer)
- B. Partial, cervix-sparing hysterectomy
- C. Observation with annual endometrial biopsies
- D. Start combination estrogen and progestin therapy
- E. Total abdominal hysterectomy with bilateral salpingo-oophorectomy
Endometriosis surgical management Explanation: ***Start progestin-only therapy***
- This patient has **endometrial hyperplasia with atypia**, which carries a high risk of progression to **endometrial cancer**, especially when associated with **tamoxifen use**.
- Given her desire for **fertility preservation**, **high-dose progestin therapy** (e.g., megestrol acetate, medroxyprogesterone acetate) is the **first-line treatment** to reverse the hyperplasia while allowing for potential conception.
*Partial, cervix-sparing hysterectomy*
- This procedure treats the uterus but would still preclude future pregnancies and is typically reserved for cases where definitive surgical management is required but the patient wishes to preserve vaginal function.
- It would be too aggressive for a patient desiring fertility who has not failed medical therapy, and it does not remove the at-risk endometrium effectively.
*Observation with annual endometrial biopsies*
- **Endometrial hyperplasia with atypia** has a significant risk of progressing to **endometrial carcinoma**, estimated at 29% over 20 years.
- Simply observing without intervention is **inappropriate** given this high risk, even with regular monitoring.
*Start combination estrogen and progestin therapy*
- The patient's endometrial hyperplasia is likely due to the **unopposed estrogenic effect of tamoxifen** on the endometrium, which acts as a selective estrogen receptor modulator (SERM).
- Adding **estrogen** would exacerbate the problem and increase the risk of endometrial cancer, making this an unsafe and inappropriate treatment.
*Total abdominal hysterectomy with bilateral salpingo-oophorectomy*
- This is a definitive surgical treatment for endometrial hyperplasia with atypia and endometrial cancer, and would effectively remove the affected tissue.
- However, this option would render the patient **infertile**, which contradicts her expressed desire to have children. It would be considered if progestin therapy fails or if fertility is not a concern.
Endometriosis surgical management US Medical PG Question 3: A 19-year-old woman presents to her gynecologist for evaluation of amenorrhea and occasional dull right-sided lower abdominal pain that radiates to the rectum. She had menarche at 11 years of age and had regular 28-day cycles by 13 years of age. She developed menstrual cycle irregularity approximately 2 years ago and has not had a menses for 6 months. She is not sexually active. She does not take any medications. Her weight is 94 kg (207.2 lb) and her height is 166 cm (5.4 ft). Her vital signs are within normal limits. The physical examination shows a normal hair growth pattern. No hair loss or acne are noted. There is black discoloration of the skin in the axillae and posterior neck. Palpation of the abdomen reveals slight tenderness in the right lower quadrant, but no masses are appreciated. The gynecologic examination reveals no abnormalities. The hymen is intact. The rectal examination reveals a non-tender, mobile, right-sided adnexal mass. Which of the following management plans would be best for this patient?
- A. Pelvic MRI should be the first-line imaging since both transvaginal and transabdominal ultrasound are inappropriate for this virginal, obese patient
- B. Clinical examination is sufficient for diagnosis since the adnexal mass was clearly palpable on rectal examination, making imaging unnecessary
- C. Transabdominal ultrasound is the appropriate first-line imaging for this virginal patient, despite reduced sensitivity due to her obesity, as transvaginal ultrasound would be inappropriate given her intact hymen
- D. The patient's obesity will not significantly affect transabdominal ultrasound quality, so transvaginal ultrasound is unnecessary even though she is virginal
- E. Transvaginal ultrasound should be performed first as it provides superior resolution for adnexal masses, regardless of the patient's sexual history or hymenal status (Correct Answer)
Endometriosis surgical management Explanation: ***Transvaginal ultrasound should be performed first as it provides superior resolution for adnexal masses, regardless of the patient's sexual history or hymenal status***
- **Transvaginal ultrasound (TVUS)** offers superior resolution for evaluating adnexal masses compared to transabdominal ultrasound due to its proximity to pelvic organs.
- While patient comfort and sexual history are important, an intact hymen is **not an absolute contraindication** to TVUS; it can often be performed carefully with a smaller probe or with patient cooperation.
*Pelvic MRI should be the first-line imaging since both transvaginal and transabdominal ultrasound are inappropriate for this virginal, obese patient*
- **Pelvic MRI** is a valuable diagnostic tool but is typically reserved as a **second-line imaging modality** when ultrasound findings are inconclusive or more detailed tissue characterization is needed.
- While obesity can reduce the quality of transabdominal ultrasound, and the patient is virginal, TVUS remains the **preferred initial imaging** due to its accessibility and high resolution.
*Transabdominal ultrasound is the appropriate first-line imaging for this virginal patient, despite reduced sensitivity due to her obesity, as transvaginal ultrasound would be inappropriate given her intact hymen*
- **Transabdominal ultrasound (TAUS)** would be challenging due to the patient's **obesity**, significantly limiting its sensitivity and resolution for adnexal structures.
- While TVUS may seem challenging with an intact hymen, it is **not strictly contraindicated** and offers far better diagnostic yield than a suboptimal TAUS in this scenario.
*Clinical examination is sufficient for diagnosis since the adnexal mass was clearly palpable on rectal examination, making imaging unnecessary*
- A palpable **adnexal mass** on clinical examination, while an important finding, is **not sufficient for diagnosis** without imaging.
- Imaging is essential to characterize the mass (e.g., solid, cystic, complex), size, location, and relationship to surrounding structures to guide appropriate management.
*The patient's obesity will not significantly affect transabdominal ultrasound quality, so transvaginal ultrasound is unnecessary even though she is virginal*
- **Obesity significantly impairs** the quality and penetration of transabdominal ultrasound, making it difficult to visualize pelvic organs and adnexal masses clearly.
- Therefore, transabdominal ultrasound is unlikely to provide sufficient diagnostic information in this obese patient, making the higher resolution of TVUS (even with an intact hymen) clinically advantageous.
Endometriosis surgical management US Medical PG Question 4: A 36-year-old African American G1P0010 presents to her gynecologist for an annual visit. She has a medical history of hypertension, for which she takes hydrochlorothiazide. The patient’s mother had breast cancer at age 68, and her sister has endometriosis. At this visit, the patient’s temperature is 98.6°F (37.0°C), blood pressure is 138/74 mmHg, pulse is 80/min, and respirations are 13/min. Her BMI is 32.4 kg/m^2. Pelvic exam reveals a nontender, 16-week sized uterus with an irregular contour. A transvaginal ultrasound is performed and demonstrates a submucosal leiomyoma. This patient is at most increased risk of which of the following complications?
- A. Endometrial cancer
- B. Miscarriage
- C. Infertility
- D. Uterine prolapse
- E. Iron deficiency anemia (Correct Answer)
Endometriosis surgical management Explanation: ***Iron deficiency anemia***
- Submucosal leiomyomas (fibroids) can cause significantly **heavy and prolonged menstrual bleeding**, known as menometrorrhagia, leading to chronic blood loss.
- This chronic blood loss depletes iron stores in the body, resulting in **iron deficiency anemia**.
*Endometrial cancer*
- While obesity is a risk factor for endometrial cancer, **leiomyomas themselves are not directly premalignant** or associated with an increased risk of endometrial carcinoma.
- The patient's irregular uterus is consistent with fibroids, not necessarily endometrial hyperplasia or cancer.
*Miscarriage*
- **Large or submucosal fibroids** can increase the risk of miscarriage by disrupting endometrial blood supply or distorting the uterine cavity.
- However, the most immediate and common complication of fibroids, particularly submucosal ones, is heavy bleeding leading to anemia.
*Infertility*
- Submucosal leiomyomas can interfere with **implantation** or **sperm transport**, thus contributing to infertility.
- However, for a G1P0010 patient, the most *likely* immediate complication associated with significant bleeding from a submucosal fibroid is anemia, before issues with future conception are explicitly addressed.
*Uterine prolapse*
- Uterine prolapse is typically due to **weakening of pelvic floor support structures**, often associated with parity, age, and conditions increasing intra-abdominal pressure.
- While a large uterus from fibroids could theoretically contribute, it is not the primary or most common complication of fibroids; heavy bleeding is much more direct and frequent.
Endometriosis surgical management US Medical PG Question 5: A 66-year-old woman presents to her primary care physician for a wellness exam. She noticed mild spotting a few days prior to presentation. Her last menstrual period was when she was 53 years of age, and she denies any trauma to the area. She is sexually active with one male partner and does not use condoms. Medical history is significant for type II diabetes mellitus and hypertension. She is currently taking metformin and lisinopril. Her last pap smear was normal. She is 5 ft 5 in (165.1 cm), weighs 185 lbs (84 kg), and BMI is 30.8 kg/m2. Her blood pressure is 115/70 mmHg, pulse is 85/min, and respirations are 15/min. Pelvic examination demonstrates a normal sized uterus with no adnexal masses. There are no vulvar, vaginal, or cervical lesions. Stool testing for blood is negative and an endometrial biopsy is performed, which demonstrates simple endometrial hyperplasia without atypia. Which of the following is the best next step in management?
- A. Anastrozole
- B. Megestrol acetate (Correct Answer)
- C. Nafarelin
- D. Estrogen-progestin contraceptives
- E. Hysterectomy
Endometriosis surgical management Explanation: ***Megestrol acetate***
- This patient has **simple endometrial hyperplasia without atypia**, which is effectively treated with **progestin therapy**.
- **Megestrol acetate** is a progestin often used for this condition, aiming to induce regression of the hyperplastic tissue.
*Anastrozole*
- **Anastrozole** is an **aromatase inhibitor** primarily used in the treatment of hormone-sensitive breast cancer.
- It works by reducing estrogen production but is not the first-line treatment for simple endometrial hyperplasia.
*Nafarelin*
- **Nafarelin** is a **GnRH agonist** mainly used for conditions like endometriosis and uterine fibroids.
- It suppresses ovarian function but is not the standard treatment for simple endometrial hyperplasia.
*Estrogen-progestin contraceptives*
- While containing progestin, **estrogen-progestin contraceptives** are generally contraindicated in postmenopausal women with abnormal uterine bleeding due to the estrogen component, which can worsen hyperplasia.
- The goal in treating endometrial hyperplasia is to provide progestin while avoiding exogenous estrogen.
*Hysterectomy*
- **Hysterectomy** is a surgical option reserved for more severe forms of endometrial hyperplasia, such as **atypical hyperplasia**, or in cases where progestin therapy fails.
- It is an overly aggressive approach for simple endometrial hyperplasia without atypia.
Endometriosis surgical management US Medical PG Question 6: A 25-year-old nulliparous woman presents to her gynecologist complaining of recurrent menstrual pain. She reports a 4-month history of pelvic pain that occurs during her periods. It is more severe than her typical menstrual cramps and sometimes occurs when she is not on her period. She also complains of pain during intercourse. Her periods occur every 28-30 days. Her past medical history is notable for kyphoscoliosis requiring spinal fusion and severe acne rosacea. She takes tretinoin and has a copper intra-uterine device. Her family history is notable for ovarian cancer in her mother and endometrial cancer in her paternal grandmother. Her temperature is 99°F (37.2°C), blood pressure is 120/85 mmHg, pulse is 90/min, and respirations are 16/min. On exam, she appears healthy and is in no acute distress. A bimanual examination demonstrates a normal sized uterus and a tender right adnexal mass. Her intrauterine device is well-positioned. What is the underlying cause of this patient's condition?
- A. Endometrial glands and stroma within the uterine myometrium
- B. Excess androgen production
- C. Endometrial glands and stroma within the peritoneal cavity (Correct Answer)
- D. Benign proliferation of uterine myometrium
- E. Chronic inflammation of the uterine endometrium
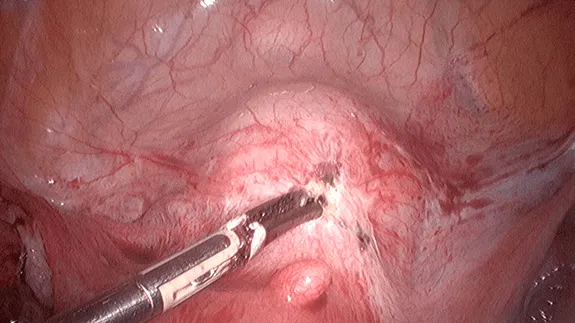
Endometriosis surgical management Explanation: ***Endometrial glands and stroma within the peritoneal cavity***
- This describes **endometriosis**, characterized by **dysmenorrhea, dyspareunia, and chronic pelvic pain** which are all present in this patient.
- The presence of a **tender adnexal mass** further supports endometriosis, likely an **endometrioma** (chocolate cyst).
*Endometrial glands and stroma within the uterine myometrium*
- This condition is known as **adenomyosis**, and typically presents with **symmetrical, boggy, enlarged uterus** and heavy menstrual bleeding.
- This patient's uterus is described as **normal sized**, making adenomyosis less likely.
*Excess androgen production*
- This is characteristic of **Polycystic Ovarian Syndrome (PCOS)**, which presents with hirsutism, acne, irregular periods, and infertility.
- The patient's symptoms of regular but painful periods, dyspareunia, and chronic pelvic pain are not typical for PCOS.
*Benign proliferation of uterine myometrium*
- This describes **uterine fibroids (leiomyomas)**, which are common and can cause heavy menstrual bleeding, pelvic pressure, and infertility.
- While they can cause pain, the clinical picture of dysmenorrhea, dyspareunia, and a tender adnexal mass is more consistent with endometriosis.
*Chronic inflammation of the uterine endometrium*
- This is known as **chronic endometritis**, often caused by infection and leading to intermenstrual bleeding, pelvic pain, and infertility.
- While pelvic pain is a symptom, the other characteristic symptoms and the presence of a tender adnexal mass make endometriosis a more fitting diagnosis.
Endometriosis surgical management US Medical PG Question 7: A previously healthy 25-year-old woman is brought to the emergency department because of a 1-hour history of sudden severe lower abdominal pain. The pain started shortly after having sexual intercourse. The pain is worse with movement and urination. The patient had several urinary tract infections as a child. She is sexually active with her boyfriend and uses condoms inconsistently. She cannot remember when her last menstrual period was. She appears uncomfortable and pale. Her temperature is 37.5°C (99.5°F), pulse is 110/min, and blood pressure is 90/60 mm Hg. Abdominal examination shows a palpable, tender right adnexal mass. Her hemoglobin concentration is 10 g/dL and her hematocrit is 30%. A urine pregnancy test is negative. Pelvic ultrasound shows a 5 x 3-cm right ovarian sac-like structure with surrounding echogenic fluid around the structure and the uterus. Which of the following is the most appropriate management for this patient's condition?
- A. Intravenous methotrexate administration
- B. Uterine artery embolization
- C. Emergency exploratory laparotomy (Correct Answer)
- D. Oral doxycycline and metronidazole administration
- E. CT scan of the abdomen
Endometriosis surgical management Explanation: ***Emergency exploratory laparotomy***
- The patient presents with **sudden severe lower abdominal pain**, **hypotension (90/60 mm Hg)**, **tachycardia (110/min)**, **palpable tender right adnexal mass**, and signs of **anemia (Hb 10 g/dL, Hct 30%)**, along with **free fluid** on ultrasound, indicating **hemorrhagic shock due to a ruptured ectopic pregnancy or ovarian cyst**. This is a surgical emergency.
- An **exploratory laparotomy** is immediately indicated to identify the source of bleeding, control hemorrhage, and remove the ruptured structure, especially given her unstable vital signs.
*Intravenous methotrexate administration*
- **Methotrexate** is used for **unruptured ectopic pregnancies** with specific criteria (e.g., small size, stable patient, declining hCG levels), but it is contraindicated in cases of rupture due to the risk of hemorrhage.
- The patient's **hypotension** and **anemia** indicate active bleeding and hemodynamic instability, making medical management inappropriate and delaying critical surgical intervention.
*Uterine artery embolization*
- **Uterine artery embolization** is primarily used for conditions like **uterine fibroids** or **postpartum hemorrhage**.
- It is not the appropriate first-line emergency treatment for acute rupture of an ectopic pregnancy or ovarian cyst with hypovolemic shock.
*Oral doxycycline and metronidazole administration*
- **Doxycycline** and **metronidazole** are antibiotics used to treat **pelvic inflammatory disease (PID)**, which presents with symptoms like fever, vaginal discharge, and lower abdominal pain, but typically not acute hemorrhagic shock.
- This patient's presentation is an acute surgical emergency with signs of hemorrhage, not an infection requiring only antibiotic therapy.
*CT scan of the abdomen*
- While a **CT scan** could provide more detailed imaging, the patient's **hemodynamic instability** (hypotension, tachycardia) requires immediate intervention.
- Delaying definitive treatment for further imaging in acute hemorrhagic shock is not appropriate and could worsen her condition.
Endometriosis surgical management US Medical PG Question 8: A 31 year-old-man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. Rectal examination reveals a small amount of bright red blood. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, and respiratory rate 14/min. Colonoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate treatment to induce remission in this patient?
- A. Azathioprine
- B. Mesalamine
- C. Total proctocolectomy
- D. Sulfasalazine
- E. Systemic corticosteroids (Correct Answer)
Endometriosis surgical management Explanation: ***Systemic corticosteroids***
- The patient presents with classic symptoms of an acute **ulcerative colitis flare**, including bloody diarrhea, abdominal pain, and colonoscopy findings of extensive inflammation from the rectum to the splenic flexure (consistent with **left-sided colitis**).
- **Systemic corticosteroids** such as prednisone or methylprednisolone are the **most appropriate treatment to induce remission** during active flares of moderate to severe ulcerative colitis due to their potent **anti-inflammatory effects** and rapid onset of action.
- This patient has moderate to severe disease based on extent and symptom severity, warranting systemic corticosteroids rather than topical or aminosalicylate therapy alone.
*Azathioprine*
- **Azathioprine** is an **immunomodulator** used for maintaining remission in inflammatory bowel disease, not for acute flare treatment.
- Its onset of action is slow (weeks to months), making it unsuitable for immediate symptom control in an acute flare.
*Mesalamine*
- **Mesalamine** (an aminosalicylate) is a **first-line therapy** for inducing and maintaining remission in **mild to moderate** ulcerative colitis, particularly for proctitis or left-sided colitis.
- However, for extensive disease with significant symptoms as seen in this patient, **systemic corticosteroids** are preferred due to greater potency and more rapid induction of remission in moderate to severe flares.
*Total proctocolectomy*
- **Total proctocolectomy** is a surgical procedure that provides a **definitive cure** for ulcerative colitis by removing the entire colon and rectum.
- However, surgery is reserved for cases of **refractory disease** (failure of medical therapy), severe complications (e.g., toxic megacolon, perforation, severe hemorrhage), or high risk of dysplasia/cancer.
- This patient is presenting with an acute flare and should be managed medically first; surgery is not the initial treatment approach.
*Sulfasalazine*
- **Sulfasalazine** is an aminosalicylate similar to mesalamine, used for inducing and maintaining remission in mild to moderate ulcerative colitis.
- While effective for mild disease, systemic corticosteroids are preferred for moderate to severe acute flares due to their stronger and more rapid anti-inflammatory action when the disease is extensive and symptomatic.
Endometriosis surgical management US Medical PG Question 9: An 8-year-old boy and his 26-year-old babysitter are brought into the emergency department with severe injuries caused by a motor vehicle accident. The child is wheeled to the pediatric intensive care unit with a severe injury to his right arm, as well as other external and internal injuries. He is hemorrhaging and found to be hemodynamically unstable. He subsequently requires transfusion and surgery, and he is currently unconscious. The pediatric trauma surgeon evaluates the child’s arm and realizes it will need to be amputated at the elbow. Which of the following is the most appropriate course of action to take with regards to the amputation?
- A. Obtain an emergency court order from a judge to obtain consent to amputate the child’s arm
- B. Find the child’s parents to obtain consent to amputate the child’s arm
- C. Amputate the child’s arm at the elbow joint (Correct Answer)
- D. Wait for the child’s babysitter to recover from her injuries to obtain her consent to amputate the child’s arm
- E. Wait for the child to gain consciousness to obtain his consent to amputate his arm
Endometriosis surgical management Explanation: ***Amputate the child’s arm at the elbow joint***
- In an emergency situation where a child's life is at risk and a procedure is immediately necessary to save their life or prevent significant harm, **implied consent** allows for medical intervention without explicit parental consent. The child's **hemodynamic instability** and **severe hemorrhage** indicate an immediate threat to life.
- The decision to amputate to save the child's life is a **medically necessary emergency intervention**. Waiting for consent would cause a dangerous delay.
*Obtain an emergency court order from a judge to obtain consent to amputate the child’s arm*
- While court orders can be used in cases of parental refusal or unavailability for non-emergency procedures, the **urgent nature** of this life-threatening situation precludes waiting for a court order.
- The delay in obtaining a court order could significantly worsen the child's prognosis or lead to death.
*Find the child’s parents to obtain consent to amputate the child’s arm*
- Although parental consent is generally required for minors, the child's **critical condition** and **hemodynamic instability** mean delaying life-saving treatment to locate parents would be medically irresponsible.
- The principle of **beneficence** (acting in the best interest of the patient) and avoiding harm takes precedence in this emergency.
*Wait for the child’s babysitter to recover from her injuries to obtain her consent to amputate the child’s arm*
- A babysitter is generally not legally authorized to provide consent for major medical procedures for a child, especially an amputation.
- Even if the babysitter had some form of temporary custody, her own injury makes her an unreliable source of consent, and the delay would be critical.
*Wait for the child to gain consciousness to obtain his consent to amputate his arm*
- An 8-year-old child is generally not considered mature enough to provide **informed consent** for such a major medical decision.
- The child is **unconscious and hemodynamically unstable**, making it impossible to obtain consent and dangerously delaying a life-saving procedure.
Endometriosis surgical management US Medical PG Question 10: A 34-year-old woman is brought into the emergency department by emergency medical services after an electrical fire in her apartment. She is coughing with an O2 saturation of 98%, on 2L of nasal cannula. The patient's physical exam is significant for a burn on her right forearm that appears to be dry, white, and leathery in texture. Her pulses and sensations are intact in all extremities. The patient's vitals are HR 110, BP 110/80, T 99.2, RR 20. She has no evidence of soot in her mouth and admits to leaving the room as soon as the fire started. Which of the following is the best treatment for this patient?
- A. Excision and grafting (Correct Answer)
- B. Bacitracin
- C. Amputation
- D. Mafenide acetate
- E. Pain relievers
Endometriosis surgical management Explanation: ***Excision and grafting***
* The burn is described as **dry, white, and leathery**, which are classic features of a **full-thickness (third-degree) burn**.
* Full-thickness burns destroy all skin layers including the dermis, and typically have **loss of sensation** at the burn site due to nerve ending destruction.
* **Excision and grafting** is the definitive treatment for full-thickness burns, involving removal of necrotic tissue and skin grafting to promote healing and prevent infection.
* The patient has intact pulses and sensations in all extremities (indicating no compartment syndrome or vascular compromise), making her a good candidate for this procedure.
*Bacitracin*
* **Bacitracin** is an antibiotic ointment used for **superficial (first-degree) or minor partial-thickness burns**.
* It is insufficient for a **full-thickness burn**, which requires surgical debridement and grafting for proper healing.
*Amputation*
* **Amputation** is reserved for cases of **irreversible tissue damage** with compromised vascularity, extensive non-viable tissue, or severe crush injuries.
* This patient has **intact pulses and sensations in all extremities**, indicating the limb is viable and perfused, making amputation inappropriate.
*Mafenide acetate*
* **Mafenide acetate** is a topical antimicrobial agent that penetrates eschar and can be used for deep burns to prevent infection.
* While useful as adjunctive therapy, it does **not replace the need for surgical excision and grafting**, which is the definitive treatment for full-thickness burns.
*Pain relievers*
* **Pain relievers** are important supportive care for burn patients but are **not definitive treatment**.
* They manage symptoms but do not address the underlying need for debridement and wound closure through grafting.
More Endometriosis surgical management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.