Gynecologic Surgery

On this page
🔬 The Gynecologic Surgeon's Operating Theater: Precision Medicine in Action
Gynecologic surgery demands more than technical skill-it requires strategic thinking that integrates anatomy, pathology, and patient-centered decision-making into every incision. You'll learn to recognize surgical signatures that distinguish emergencies from elective cases, master the evidence-based algorithms that guide intervention versus observation, and understand how gynecologic conditions interconnect with broader systemic health. This lesson builds your clinical reasoning from initial assessment through operative planning, equipping you to approach surgical problems with both precision and perspective.
📌 Remember: CLOSE for pelvic surgical anatomy - Cervix (transformation zone), Ligaments (cardinal, uterosacral), Ovaries (vascular pedicles), Supports (levator ani), Endopelvic fascia (integrity planes)
The surgical approach determines outcomes across 6 major categories: minimally invasive laparoscopy (85% of benign cases), robotic assistance (40% growth annually), vaginal procedures (60% prolapse repairs), abdominal approaches (25% complex cases), hysteroscopic interventions (90% intrauterine pathology), and emergency procedures (15% of all gynecologic surgeries).
- Laparoscopic Advantages
- Reduced hospital stay: 1-2 days vs 3-5 days open
- Faster recovery: 2-3 weeks vs 6-8 weeks
- Return to work: 7-10 days earlier
- Cosmetic outcomes: 5mm incisions vs 15cm laparotomy
- Robotic Precision
- Tremor elimination: 6-7 degrees of freedom
- Magnification: 10-15x visualization
- Suturing accuracy: 90% improvement in confined spaces
- Learning curve: 20-50 cases for proficiency
| Surgical Approach | Hospital Stay | Recovery Time | Complication Rate | Cost Factor | Fertility Impact |
|---|---|---|---|---|---|
| Laparoscopic | 1-2 days | 2-3 weeks | 5-8% | 1.2x | Minimal |
| Robotic | 1-2 days | 2-3 weeks | 4-6% | 2.5x | Minimal |
| Vaginal | 1-3 days | 3-4 weeks | 8-12% | 0.8x | Variable |
| Abdominal | 3-5 days | 6-8 weeks | 12-18% | 1.0x | Moderate |
| Hysteroscopic | Same day | 1-2 weeks | 2-4% | 0.6x | Preserved |
💡 Master This: Surgical success depends on anatomical plane recognition - the avascular spaces between organs that allow safe dissection. The vesicouterine fold, rectovaginal space, and pararectal spaces contain <2% major vessel density, making them ideal surgical corridors.
Understanding tissue handling principles prevents complications: electrocautery settings at 30-40 watts for cutting, 20-25 watts for coagulation, pneumoperitoneum pressure maintained at 12-15 mmHg, and CO2 insufflation rates of 2-4 L/min to prevent gas embolism risk (<0.1% incidence with proper technique).
🔬 The Gynecologic Surgeon's Operating Theater: Precision Medicine in Action
⚙️ The Surgical Decision Matrix: When Scalpels Meet Strategy
📌 Remember: SURGICAL indications framework - Symptom severity (quality of life impact), Uterine size (>12-14 weeks), Refractory to medical therapy (6+ months), Growth rate (rapid enlargement), Infertility impact, Cancer risk, Anatomic distortion, Location accessibility
Pre-operative optimization reduces complications by 40-60%: hemoglobin >10 g/dL (iron supplementation 4-6 weeks), BMI <35 (weight loss 5-10% improves outcomes), smoking cessation (4+ weeks reduces wound complications 50%), and medical comorbidity stabilization (diabetes HbA1c <7%, hypertension <140/90 mmHg).
- Timing Considerations
- Menstrual cycle: follicular phase (days 1-10) optimal
- Endometrial thickness: <5mm for hysteroscopy
- GnRH agonist pretreatment: 2-3 months for large fibroids
- Hormonal suppression: reduces vascularity 30-40%
- Risk Stratification
- ASA classification: I-II outpatient, III-IV inpatient monitoring
- Surgical complexity: simple (<2 hours), intermediate (2-4 hours), complex (>4 hours)
- Blood loss prediction: simple <200mL, complex >500mL
- Conversion risk: laparoscopic to open 2-5% benign, 8-12% malignant
| Risk Factor | Low Risk | Moderate Risk | High Risk | Intervention Required |
|---|---|---|---|---|
| Age | <50 years | 50-70 years | >70 years | Cardiac clearance |
| BMI | <30 | 30-35 | >35 | Weight optimization |
| Prior Surgery | None | 1-2 procedures | >3 procedures | Adhesion planning |
| Uterine Size | <12 weeks | 12-16 weeks | >16 weeks | Morcellation plan |
| Hemoglobin | >12 g/dL | 10-12 g/dL | <10 g/dL | Iron/EPO therapy |
💡 Master This: Patient counseling must include specific success rates - myomectomy fertility improvement 40-60%, endometriosis surgery pregnancy rates 30-50%, prolapse repair satisfaction 85-90%, and recurrence risks varying by procedure type (5-15% mesh repairs vs 15-30% native tissue).
Informed consent addresses procedure-specific risks: bleeding (2-5% transfusion risk), infection (3-8% depending on approach), organ injury (bladder 1-2%, bowel 0.1-0.5%, ureter 0.2-1%), conversion to laparotomy (2-8%), and fertility impact (adhesion formation 10-30%, ovarian reserve reduction 5-15% with ovarian surgery).
⚙️ The Surgical Decision Matrix: When Scalpels Meet Strategy
🎯 The Pattern Recognition Playbook: Surgical Signatures in Action
Visual pattern recognition during surgery follows systematic assessment protocols. Normal anatomy landmarks include uterosacral ligament insertion at S2-S4, ovarian vessels crossing ureter at pelvic brim, and cardinal ligament containing uterine artery at cervical level. Deviation from these patterns signals anatomical variants (15-20% population) or pathologic distortion.
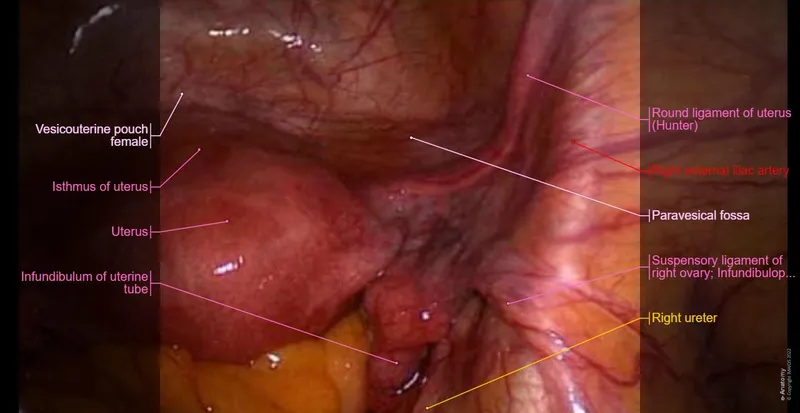
📌 Remember: OVARIES for adnexal assessment - Ovarian size (3-5cm normal), Vascular pattern (avoid infundibulopelvic ligament), Adhesions (endometriosis clue), Relation to ureter (2cm safety margin), Internal architecture (cystic vs solid), Endometriomas (chocolate cyst appearance), Surface irregularities (malignancy concern)
Endometriosis recognition requires systematic peritoneal survey: powder-burn lesions (black/blue deposits), red flame-like implants (active disease), white scarred areas (chronic fibrosis), chocolate cysts (ovarian endometriomas), and deep infiltrating nodules (>5mm depth). Severity staging follows rASRM classification: Stage I (1-5 points), Stage II (6-15 points), Stage III (16-40 points), Stage IV (>40 points).
- Fibroid Classification Patterns
- Submucosal (Type 0-2): hysteroscopic approach 95% success
- Intramural (Type 3-4): laparoscopic myomectomy preferred
- Size limits: <10cm laparoscopic, >10cm consider open
- Number limits: <5 fibroids laparoscopic feasibility
- Ovarian Mass Characteristics
- Simple cysts: <5cm observe, >5cm consider removal
- Complex cysts: septations, solid components, vascularity
- Malignancy risk: RMI score >200 high suspicion
- CA-125 levels: >35 U/mL concerning in postmenopausal
| Pathology Type | Visual Signature | Size Threshold | Surgical Approach | Success Rate |
|---|---|---|---|---|
| Endometriosis | Black/red lesions | Any size | Excision vs ablation | 70-85% |
| Fibroids | Well-circumscribed | <10cm lap, >10cm open | Myomectomy | 85-95% |
| Ovarian cysts | Smooth/complex | >5cm intervention | Cystectomy | 90-95% |
| Adhesions | Filmy/dense bands | Severity graded | Adhesiolysis | 60-80% |
| Prolapse | Anatomic descent | Stage 2+ symptoms | Repair choice | 80-90% |
Intraoperative decision-making follows "see-think-do" protocols: assess anatomy (normal vs distorted), identify pathology (extent and severity), plan approach (conservative vs aggressive), execute technique (energy source selection), and verify hemostasis (<50mL blood loss goal for benign cases).
💡 Master This: Complication recognition requires immediate pattern identification - ureteral injury shows lack of peristalsis and dye extravasation, bladder injury presents gas bubbles in Foley bag, bowel injury demonstrates content spillage or serosal tears, and vascular injury causes rapid blood loss with hemodynamic changes.
Energy source selection follows tissue-specific protocols: monopolar electrocautery for cutting (pure cut 40-50 watts), bipolar for hemostasis (25-35 watts), ultrasonic for vessel sealing (<7mm diameter), advanced bipolar for larger vessels (<7mm LigaSure), and laser for precision excision (endometriosis treatment).
🎯 The Pattern Recognition Playbook: Surgical Signatures in Action
🔍 The Differential Diagnosis Decoder: Surgical vs Conservative Management
Acute vs chronic presentations guide surgical urgency decisions. Ovarian torsion presents with sudden onset severe pain (8-10/10), nausea/vomiting (90% cases), and adnexal mass on imaging, requiring emergency surgery within 6-8 hours to preserve ovarian function. Chronic pelvic pain from endometriosis develops over months-years, responds partially to NSAIDs (40-60% relief), and allows planned surgical intervention.
📌 Remember: TWISTED for ovarian torsion diagnosis - Timing (sudden onset), Whirl sign (vascular pedicle), Intense pain (>8/10), Size increase (>5cm mass), Tenderness (severe), Edema (ovarian enlargement), Doppler (absent/decreased flow)
Malignant vs benign differentiation determines surgical approach and extent. Benign characteristics include smooth surfaces, mobile masses, normal CA-125 (<35 U/mL premenopausal), simple cystic appearance, and unilateral presentation. Malignant features show irregular surfaces, fixed masses, elevated tumor markers, solid components with vascularity, and bilateral involvement (40-50% ovarian cancers).
- Imaging Discrimination Criteria
- Ultrasound findings: simple cysts (anechoic, thin walls) vs complex masses (septations, solid areas)
- MRI characteristics: T1/T2 signal patterns distinguish endometriomas vs malignancy
- Endometriomas: high T1, shading on T2
- Malignancy: heterogeneous enhancement, ascites
- Tumor Marker Interpretation
- CA-125: >35 U/mL concerning, >200 U/mL high suspicion
- HE4: <70 pmol/L premenopausal, <140 pmol/L postmenopausal
- ROMA index: combines CA-125 and HE4 for risk stratification
- Sensitivity: 85-90% for epithelial ovarian cancer
| Clinical Feature | Benign Condition | Malignant Condition | Surgical Urgency | Approach |
|---|---|---|---|---|
| Pain onset | Gradual/cyclic | Progressive/constant | Planned | Conservative |
| Mass mobility | Mobile | Fixed/adherent | Urgent | Oncologic |
| Tumor markers | Normal | Elevated | Immediate | Staging |
| Imaging | Simple/cystic | Complex/solid | Emergency | Debulking |
| Age factor | Reproductive | Postmenopausal | Planned | Fertility-sparing |
Fertility preservation decisions require age-specific considerations: <35 years prioritize conservative surgery (myomectomy over hysterectomy, cystectomy over oophorectomy), 35-40 years balance symptom relief with reproductive goals, and >40 years may favor definitive procedures if family complete.
💡 Master This: Surgical complexity scoring predicts operative time and complication risk - simple procedures (<2 hours, <5% complications) include diagnostic laparoscopy and simple cystectomy, while complex cases (>4 hours, >15% complications) involve extensive endometriosis, large fibroids (>10cm), or suspected malignancy.
Conservative management success rates vary by condition: hormonal therapy for endometriosis (60-70% pain relief), GnRH agonists for fibroids (30-50% size reduction), pelvic floor therapy for prolapse (40-60% symptom improvement), and medical management for abnormal bleeding (70-80% response rates with progestins or tranexamic acid).
🔍 The Differential Diagnosis Decoder: Surgical vs Conservative Management
⚖️ The Treatment Algorithm Arsenal: Evidence-Based Surgical Protocols
Surgical technique selection follows evidence-based algorithms that consider patient factors, pathology characteristics, and surgeon expertise. Laparoscopic myomectomy achieves 85-95% symptom relief with 40-60% fertility improvement, while hysteroscopic resection of submucosal fibroids shows 90-95% success rates for menorrhagia control.
📌 Remember: TECHNIQUE selection criteria - Tissue type (fibrous vs cystic), Experience level (surgeon proficiency), Complexity score (simple vs advanced), Hemostasis needs (bleeding risk), Navigate anatomy (distorted planes), Instrumentation (available technology), Quality outcomes (success rates), Urgency factors (emergency vs elective), Equipment access (robotic availability)
Endometriosis surgical management follows severity-based protocols: Stage I-II disease responds to ablation or excision with 70-80% pain relief, Stage III-IV requires complete excision of deep infiltrating lesions achieving 80-90% symptom improvement. Fertility outcomes show pregnancy rates of 30-50% post-surgery depending on disease severity and patient age.
- Energy Source Protocols
- Monopolar electrocautery: cutting 40-50W, coagulation 30-40W
- Bipolar energy: vessel sealing 25-35W, tissue desiccation
- Ultrasonic devices: <7mm vessels, minimal thermal spread
- Advanced bipolar: LigaSure <7mm, Enseal <7mm diameter
- Hemostasis Techniques
- Suture ligation: permanent hemostasis, large vessel control
- Topical agents: Surgicel, Floseal for oozing surfaces
- Argon beam: superficial coagulation, liver/spleen surfaces
- Hemostatic matrix: Gelfoam with thrombin for raw surfaces
| Procedure Type | Success Rate | Complication Rate | Recovery Time | Fertility Impact |
|---|---|---|---|---|
| Hysteroscopic resection | 90-95% | 2-5% | 1-2 weeks | Preserved |
| Laparoscopic myomectomy | 85-90% | 5-10% | 2-4 weeks | Improved 40-60% |
| Endometriosis excision | 80-90% | 8-15% | 3-6 weeks | Improved 30-50% |
| Ovarian cystectomy | 90-95% | 3-8% | 2-3 weeks | Preserved 85-90% |
| Prolapse repair | 85-90% | 10-15% | 4-6 weeks | Variable |
Post-operative management follows standardized protocols: pain control with multimodal analgesia (NSAIDs + acetaminophen + opioids PRN), early mobilization within 6-12 hours, diet advancement as tolerated, and discharge criteria including stable vital signs, adequate pain control (<4/10), and return of bowel function.
💡 Master This: Complication management requires immediate recognition and protocol-driven responses - bleeding (>500mL or hemodynamic instability) needs surgical exploration, infection (fever >38.5°C, elevated WBC) requires antibiotic therapy, and organ injury demands immediate repair or specialist consultation.
Quality metrics track surgical outcomes: conversion rates (<5% for benign disease), complication rates (<10% major complications), readmission rates (<5% within 30 days), patient satisfaction (>90% would recommend**), and functional outcomes (symptom resolution >80%).
⚖️ The Treatment Algorithm Arsenal: Evidence-Based Surgical Protocols
🔗 The Multi-System Integration Matrix: Surgical Interconnections
Pelvic floor integration demonstrates complex system interactions: levator ani muscle provides structural support for uterus, bladder, and rectum, while endopelvic fascia creates tissue planes that guide surgical dissection. Prolapse repair must address all three compartments - anterior (cystocele), posterior (rectocele), and apical (uterovaginal) - to achieve durable outcomes (85-90% success with comprehensive repair).
📌 Remember: SUPPORT for pelvic floor anatomy - Sacral attachments (S2-S4 nerve roots), Uterosacral ligaments (cardinal support), Pubocervical fascia (anterior compartment), Peritoneum (pouch of Douglas), Obturator internus (lateral walls), Rectovaginal fascia (posterior compartment), Tendinous arch (fascial condensation)
Neurovascular preservation requires understanding anatomical relationships: hypogastric nerve (sympathetic T12-L2) controls bladder function, pelvic splanchnic nerves (parasympathetic S2-S4) manage bowel/bladder coordination, and pudendal nerve (S2-S4) innervates external anal sphincter and clitoris. Nerve-sparing techniques during radical surgery preserve sexual function (70-80% vs 40-50% with nerve sacrifice).
- Vascular Territory Management
- Uterine artery: branches at cervix, ascending/descending divisions
- Ovarian vessels: cross ureter at pelvic brim, anastomose with uterine
- Internal iliac system: anterior/posterior divisions, visceral branches
- Venous drainage: pampiniform plexus, ovarian veins (right to IVC, left to renal)
- Urologic Integration
- Ureter course: "water under bridge" - under uterine artery
- Bladder innervation: hypogastric (storage), pelvic (voiding)
- Injury prevention: lateral dissection, identify ureter before vessel ligation
- Cystoscopy: routine for complex cases, ureteral patency confirmation
| System Integration | Anatomical Relationship | Surgical Consideration | Preservation Technique | Success Rate |
|---|---|---|---|---|
| Reproductive-Urologic | Ureter crosses uterine vessels | Identify before ligation | Lateral dissection | 98-99% |
| Pelvic Floor-GI | Rectovaginal fascia | Posterior repair integrity | Layer closure | 85-90% |
| Vascular-Neural | Hypogastric nerve plexus | Bladder function | Nerve-sparing | 70-80% |
| Ovarian-Vascular | Infundibulopelvic ligament | Vessel control | Bipolar coagulation | 95-98% |
| Uterine-Cervical | Parametrial tissues | Radical resection | Systematic approach | 90-95% |
Hormonal system integration affects surgical outcomes: estrogen deficiency post-oophorectomy increases cardiovascular risk (2-3x), bone loss (2-3% annually), and sexual dysfunction (60-70% cases). Hormone replacement therapy initiated immediately post-surgery prevents vasomotor symptoms (80-90% effective) and maintains bone density.
💡 Master This: Fertility preservation requires ovarian reserve assessment - AMH levels (>1.0 ng/mL adequate reserve), antral follicle count (>5-7 per ovary), and age considerations (<35 years optimal outcomes). Ovarian tissue cryopreservation offers future fertility options when bilateral oophorectomy necessary in young patients.
Oncologic integration demands multidisciplinary coordination: gynecologic oncologist for surgical staging, medical oncologist for chemotherapy protocols, radiation oncologist for adjuvant therapy, and genetic counselor for hereditary cancer syndromes (BRCA1/2, Lynch syndrome). Survival outcomes improve 20-30% with specialized care at high-volume centers.
🔗 The Multi-System Integration Matrix: Surgical Interconnections
🎯 The Surgical Mastery Toolkit: Essential Clinical Arsenal
Essential instrument mastery includes laparoscopic fundamentals: 5mm graspers for tissue manipulation, monopolar hook for cutting/coagulation, bipolar forceps for hemostasis, scissors for precise dissection, and clip appliers for vessel control. Advanced instruments include ultrasonic devices (Harmonic), advanced bipolar (LigaSure), and robotic platforms (da Vinci) with tremor elimination and 7 degrees of freedom.
📌 Remember: INSTRUMENTS for laparoscopic setup - Insufflation (CO2 12-15 mmHg), Needle (Veress 90-degree angle), Scope (0-degree diagnostic, 30-degree operative), Trocars (5-12mm sizes), Retractors (atraumatic graspers), Ultrasonic (vessel sealing <7mm), Monopolar (cutting 40-50W), Energy (bipolar 25-35W), Needle holders (suturing), Tissue bags (specimen removal), Suction (irrigation/aspiration)
Suturing techniques determine tissue healing and long-term outcomes: interrupted sutures for hemostasis and tension-free closure, running sutures for speed and watertight seals, figure-of-eight for vessel control, and purse-string for circular closures. Suture materials include absorbable (Vicryl 2-4 weeks, PDS 6-8 weeks) and permanent (silk, nylon) based on tissue requirements.
- Energy Source Mastery
- Monopolar settings: pure cut 40-50W, blend 30-40W, coag 25-30W
- Bipolar parameters: vessel sealing 25-35W, desiccation 15-20W
- Ultrasonic advantages: minimal smoke, precise cutting, <2mm thermal spread
- Advanced bipolar: tissue sensing, automatic shutoff, consistent sealing
- Complication Recognition
- Bleeding patterns: arterial (pulsatile, bright red), venous (steady, dark red)
- Organ injury signs: gas bubbles (bladder), content spillage (bowel), hematuria (ureter)
- Immediate management: pressure control, suture repair, specialist consultation
- Prevention strategies: proper visualization, adequate exposure, systematic approach
| Surgical Skill | Proficiency Marker | Practice Requirement | Complication Rate | Mastery Indicator |
|---|---|---|---|---|
| Port placement | <2 min setup | 50+ cases | <2% injury | Consistent positioning |
| Tissue handling | Atraumatic technique | 100+ cases | <5% damage | Gentle manipulation |
| Suturing | <5 min/suture | 200+ sutures | <3% dehiscence | Smooth technique |
| Energy use | Appropriate settings | 150+ cases | <1% thermal injury | Precise application |
| Complication management | <30 sec recognition | Variable | <10% conversion | Immediate response |
Quality improvement metrics track surgical performance: operative time (benchmark comparisons), blood loss (<200mL benign cases), conversion rates (<5% planned laparoscopy), complication rates (<10% major**), readmission rates (<5% within 30 days), and patient satisfaction (>90% recommend surgeon**).
💡 Master This: Continuous improvement requires case log analysis, complication review, outcome tracking, and technique refinement. Simulation training improves technical skills (20-30% faster learning), team-based training reduces communication errors (40-50%), and mentorship programs accelerate competency development (6-12 months faster progression).
Emergency preparedness includes hemorrhage control (pressure, suture, energy), organ injury repair (immediate vs delayed), conversion criteria (safety first), and team communication (clear, concise, actionable). Crisis resource management principles ensure optimal outcomes during unexpected complications through leadership, communication, situational awareness, and decision-making protocols.
🎯 The Surgical Mastery Toolkit: Essential Clinical Arsenal
Practice Questions: Gynecologic Surgery
Test your understanding with these related questions
A 33-year-old woman comes to the emergency department because of a 1-hour history of severe pelvic pain and nausea. She was diagnosed with a follicular cyst in the left ovary 3 months ago. The cyst was found incidentally during a fertility evaluation. A pelvic ultrasound with Doppler flow shows an enlarged, edematous left ovary with no blood flow. Laparoscopic evaluation shows necrosis of the left ovary, and a left oophorectomy is performed. During the procedure, blunt dissection of the left infundibulopelvic ligament is performed. Which of the following structures is most at risk of injury during this step of the surgery?














